Neurofibromatosis (NF) is an inherited autosomal disorder that affects the nervous system and skin. Tumors, both benign and malignant, are reported to occur four times more often in patients with NF when compared to the general population matched for age and gender.1 A variety of endocrine tumors are frequently reported in these patients. The commonest one is pheochromocytoma, which occurs in 0.1% to 5.7% of patients.2 We report a case of hyperparathyroidism and bilateral pheochromocytoma occurring in a patient with familial peripheral neurofibromatosis. The combination of pheochromocytoma and hyperparathyroidism suggest MEN2A (multiple endocrine neoplasia, type II) syndrome in this patient. On the other hand pheochromocytoma is part of the spectrum of disorders associated with neurofibromatosis type 1 (NF1). There are 14 reported cases of hyperparathyroidism occurring in patients with NF, making a genuine association between these two uncommon conditions likely. These differentials are discussed and diagnosis is confirmed based on genetic analysis.
Case
This 65-year-old man was referred to our hospital for adrenalectomy. He was known to have familial peripheral neurofibromatosis type1 (Von Recklinghausen’s disease) for many years, which also affected his two children and his brother. Recently he was admitted to a peripheral hospital for repair of bilateral inguinal hernia. During routine preoperative examination he was incidentally found to have hypertension and gave a history of 2 years of headache.
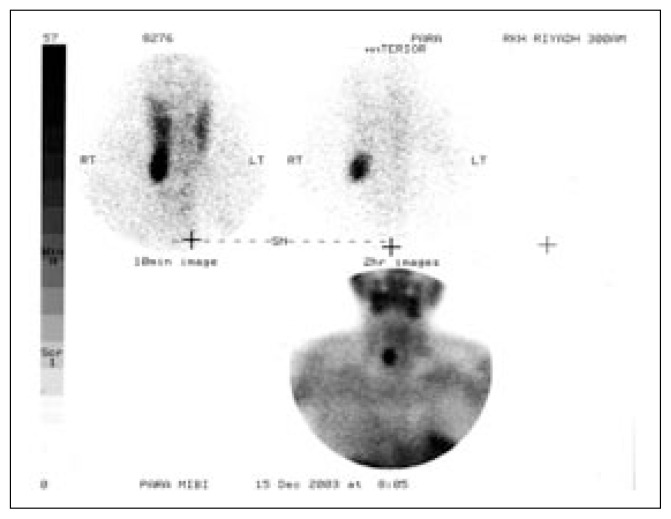
Since the association of NF and pheochromocytoma is well established, a proper evaluation to exclude pheochromocytoma was planned. Both metabolic and radiological investigations confirmed the likely diagnosis. CT of the abdomen revealed the typical appearance of a large right-sided adrenal mass plus a probable smaller one in the left adrenal gland. The patient was started on labetolol, then referred to us for adrenalectomy. Examination revealed multiple pedunculated neurofibromas on his chest, back and neck. His BP was 145/86. The patient had many (>15) “cafe-au-lait” spots, which were larger than 2 cm in diameter and located mainly on his chest, abdomen and back. His condition fit the diagnosis of NF1 according to the diagnostic criteria of the national NF foundation.1 Investigations for pheochromocytoma showed high 24 hour-urinary free catecholamines with an adrenaline level of 1029 nmol/L (normal, <230) and noradrenalin of 1041 nmol/L (normal, <900). MIBG scan showed bilateral uptake in both adrenal glands, but mainly in the right one. Serum calcium was 2.96 mmol/L, and PTH was 153 ng/L (normal, 7–53). The 24 hour-urinary calcium was normal. US of the neck and MIBI scan (Figure 1) showed a normal thyroid and a single parathyroid adenoma on the right lower aspect. The combination of hyperparathyroidism and pheochromocytoma suggested MEN2A,1 which was characterized by medullary thyroid cancer, pheochromocytoma and parathyroid adenoma or hyperplasia in this patient although he had a negative family history for both conditions. The pentagastrin stimulation test was negative. In the molecular genetic analysis for MEN2A,1 direct mutation analysis showed that he was not a carrier of a mutation in exon 11, which includes codon 634 of the RET proto-oncogene. In addition, single-strand conformation variant analysis (SSCP) of exon 10, which includes codons 609, 611, 618, and 620, and MS-PCR analysis of codon 768 detected normal band patterns.
Figure 1.
MIBI scan showing right lower parathyroid adenoma.
He underwent a right adrenalectomy. Histopathological exam of the gland revealed pheochromocytoma. Since the MIBG scan showed minimal uptake, the plan was to avoid removing the other gland unless there was clear evidence that it was abnormal. A bilateral adrenalectomy would leave the patient dependent on oral steroids for the rest of his life, and expose him to the risk of adrenal crisis, considering that he was not very compliant to his medications previously. Hyperparathyroidism was managed by excision of the parathyroid adenoma (right lower gland). The other glands were found to be normal by palpation and biopsy.
Discussion
Neurufibromatosis is an autosomal dominant genetic disorder that affects the nervous system and skin. It has been classified into two distinct types: NF1 and NF2. NF1, also known as Von Recklinghausen NF, manifests as skin neurofibromas and multiple caféau-lait spots. Other associations are optic gliomas, scoliosis, precocious puberty, learning disabilities and malignancies (e.g. pheochromocytoma, somatostatinoma). NF2, also known as bilateral acoustic NF (BAN), is more rare. It is characterized by multiple tumors on the cranial and spinal nerves plus bilateral acoustic nerve tumors, which are the hallmark of the disease. Tumors, both benign and malignant, are reported to occur four times more often in patients with NF when compared to the general population matched for age and gender.2
Pheochromocytoma is known to occur in a small but defined number of patients with NF, affecting 0.1% to 5.7% of patients. Of the 148 patients with NF1 and pheochromocytoma reviewed by Walther,3 84% had solitary adrenal tumors, 9.6% had bilateral adrenal disease and 6.1% had ectopic pheochromocytoma. The pheochromocytoma in MEN1 can be unilateral or bilateral, affecting more than half of individuals. If a tumor is present in one adrenal gland, hyperplasia is likely in the other gland.
Data from the international RET consortium3 indicates that the preponderance of MEN2A mutations are in codon 634. In 20 cases from 74 families, 97% had RET mutations with 87% having a mutation at codon 634, 6.4% at codon 918, 3.5% at codon 618, 2.1% at codon 611 and 0% at codon 918. Three percent had no RET mutation. The genetic analysis in our patient indicated that his chance of having MEN2 was less than 0.5%. What makes this case unique is the finding of bilateral pheochromocytoma and hyperparathyroidism raising the possibility of MEN2A. Also the finding of both hyperparathyroidism and NF, both being rare diseases, suggest a possible link between the two disorders, which is supported by previous case reports of a similar association.
The association between peripheral NF and hyperparathyroidism was first reported in 1953 in a patient with ostietis fibrosa cystica, NF and liposarcoma. Since then there have been about 14 case reports5–14 of this association and they were almost always due to parathyroid adenoma rather hyperplasia. Also, many patients (40–50%) with NF can develop skeletal lesions, which may be related to neurofibroma of bone, ostietis fibrosa cystica or osteomalacia. The latter is characterized by renal phosphate wasting of unknown etiology similar to humoral hypercalcemia of malignancy (HHM). The similarity of the bone lesions seen in NF1 and hyperparathyroidism strongly suggests a genetic link between these two pathologies or at least a common underlying pathology.
Cases of hyperparathyroidism due to parathyroid hyperplasia plus hypophosphatemic osteomalacia occurring in patients with NF1 have been reported. In those case, it was difficult to determine if the hyperparathyroid was primary or tertiary.9 In our patient MEN2(A) was unlikely since he had no family history. Also his genetic screening was negative for the MEN2(A) gene mutation. Apart from hyperparathyroidism there is another bony disorder shared by both NF1 and MEN2. Fibrous bony dysplasia (FD) is a developmental abnormality of bone mesenchyma presenting as expansible fibrous lesions of the skeleton that may result in pathological fractures. In this disorder the absorbed bone is replaced by a fibrosseous tissue instead of by normal bone. As the mass of fibrous tissue proliferates, it erodes the cortical bone from within, while the periosteum lays down a thin shell of bone outside and hence the bone expands. The precise nature of FD remains controversial. Cosegregations of FD and NF1 have been reported, and it has been surmised that FD is associated with the NF1 gene.12 NF has been also linked in many reports to somatostatinoma.15–17 In the literature, duodenal somatostatinoma is associated with von Recklinghausen’s disease in 50% of cases.17 This linkage of neurofibromatosis, phaeochromocytoma, and duodenal carcinoid could represent a specific multiple endocrine neoplasia syndrome.
Based on these data, do we have enough evidence to reclassify NF1 as one of the MEN syndromes due to the increasing awareness of its collective endocrine abnormalities? It seems that hyperparathyroidism should be looked for in all patients affected with NF1 to find out its true incidence in these patients, and as part of research to uncover any hidden association between the two conditions. Also, research is needed to find out if correction of hypercalcemia and hyperparathyroidism in these patients can reverse the bony abnormalities of NF1 mentioned above.
References
- 1.National NF foundation. www.nf.org.
- 2.Madeleinr ET, Zoller, Rembeck Brigitta. Malignant and benign tumors in patients with neurofibromatosis type1 in a defined Swedish population. Cancer. 1997 Jun 1;79(11):2125–2131. [PubMed] [Google Scholar]
- 3.Walther MM, et al. Von Recklinghausen disease and pheochromocytoma. Journal of Urology. 1999 Nov;162(5):1582–6. [PubMed] [Google Scholar]
- 4.Mulligan LM, et al. Genotype-phenotype correlation in multiple endocrine neoplasia type 2: report of the international RET mutation consortium. J Int Medicine. 238:343–346. doi: 10.1111/j.1365-2796.1995.tb01208.x. [DOI] [PubMed] [Google Scholar]
- 5.Moiton MP, Bijou F, Vargas F, Valentino R. Association of type 1 neurofibromatosis and primary hyperparathyroidism. Presse Medicale. 2002 Oct 19;31(34):1604–5. [PubMed] [Google Scholar]
- 6.Abdel-Wanis ME, Kawahara N, Tomita K. The association of neurofibromatosis 1 and spinal deformity with primary hyperparathyroidism and osteomalacia: might melatonin have a role? Journal of Orthopaedic Science. 2001;6(2):193–8. doi: 10.1007/s007760100071. [DOI] [PubMed] [Google Scholar]
- 7.Duquenne M, Klein M, Duriez T. Hyperparathyroidism in a patient with neurofibromatosis associated with Steinert’s disease. Annales de Medecine Interne. 1994;145(7):505–7. [PubMed] [Google Scholar]
- 8.van Damme PA, Mooren RE. Differentiation of multiple giant cell lesions, Noonan-like syndrome, and (occult) hyperparathyroidism. Case report and review of the literature. International Journal of Oral & Maxillofacial Surgery. 1994 Feb;23(1):32–6. doi: 10.1016/s0901-5027(05)80323-6. [DOI] [PubMed] [Google Scholar]
- 9.Weinstein RS, Harris RL. Hypercalcemic hyperparathyroidism and hypophosphatemic osteomalacia complicating neurofibromatosis. Calcified Tissue International. 1990 Jun;46(6):361–6. doi: 10.1007/BF02554965. [DOI] [PubMed] [Google Scholar]
- 10.Rosenberg NL, Diliberti JH, Andrews AM, Buist NR. Myotonic dystrophy and hyperparathyroidism: association with neurofibromatosis and multiple endocrine adenomatosis type 2A. Journal of Neurology, Neurosurgery & Psychiatry. 1988 Dec;51(12):1578–80. doi: 10.1136/jnnp.51.12.1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoppe LB, Collicott PE, Stivrins TJ. Von Recklinghausen’s neurofibromatosis and primary hyperparathyroidism: a case report and literature review. Nebraska Medical Journal. 1986 Dec;71(12):435–7. [PubMed] [Google Scholar]
- 12.Freimanis MG, Rodgers RW, Samaan NA. Neurofibromatosis and primary hyperparathyroidism. Southern Medical Journal. 1984 Jun;77(6):794–5. doi: 10.1097/00007611-198406000-00039. [DOI] [PubMed] [Google Scholar]
- 13.Chakrabarti S, Murugesan A, Arida EJ. The association of neurofibromatosis and hyperparathyroidism. American Journal of Surgery. 1979 Mar;137(3):417–20. doi: 10.1016/0002-9610(79)90079-5. [DOI] [PubMed] [Google Scholar]
- 14.Cinamon U, Avinoch I, Harell M. Neurofibromatosis type1, Hyperparathyroidism and Osteosarcoma: interplay? Eur Arch Otorhinolaryngol. 2002 Nov;259(10):540–2. doi: 10.1007/s00405-002-0497-3. [DOI] [PubMed] [Google Scholar]
- 15.Reichardt M, Rexroth W, Hasslacher C. Von Recklinghausen type I neurofibromatosis and neuroendocrine tumor (somatostatinoma) in a 50-year-old woman. Medizinische Klinik. 1998 Sep 15;93(9):550–3. doi: 10.1007/BF03042665. [DOI] [PubMed] [Google Scholar]
- 16.Sakamoto A, Oda Y, Oshiro Y, Tamiya S, Iwamoto Y, Tsuneyoshi M. immunoexpression of neurofibromin, S-100 protein, and leu-7 and mutation analysis of the NF1 gene at codon 1423 in osteofibrous dysplasia. Human Pathology. 2001 Nov;32(11):1245–51. doi: 10.1053/hupa.2001.28954. [DOI] [PubMed] [Google Scholar]
- 17.Blaser A, Vajda P, Rosset P. Duodenal somatostatinomas associated with von Recklinghausen disease. Schweizerische Medizinische Wochenschrift. Journal Suisse de Medecine. 1998 Dec 12;128(50):1984–7. [PubMed] [Google Scholar]