Abstract
BACKGROUND
Accidental needlestick injuries sustained by health care workers are a common occupational hazard in health care settings. The aim of this study was to review the epidemiology of needlestick injuries in Buraidah Central Hospital, a 212-bed secondary care hospital in Buraidah, Saudi Arabia.
METHODS
We conducted a retrospective survey of all self-reported documents related to needlestick injuries, for the period January 2002 through December 2003. The data was analyzed to determine the age, sex and job category of the health care worker suffering the injury as well as the risk factors responsible for needlestick injuries.
RESULTS
During the 2-year period, employees reported 73 injuries from needles and other sharp objects. Nurses were involved in 66% of instances, physicians in 19%, technicians in 10%, and nonclinical support staff in 5.5%. The majority (53.4%) of the injuries occurred after use and before disposal of the objects. Syringe needles were responsible for 63% of all injuries. Most injuries occurred during recapping of used needles (29%), during surgery (19%), and by collision with sharps (14%). Disposal-related (11%) causes as well as injuries by concealed sharps (5%) occurred while handling linens or trash containing improperly disposed needles.
CONCLUSION
This data emphasizes the importance of increased awareness, training and education of health care workers for reporting and prevention of needlestick injuries.
Needlestick injuries (NSIs), also referred to as sharps injuries, percutaneous injuries and sharps exposures, represent accidental breaks in the skin with needles, scalpels or other sharp objects that have been in contact with a source patient’s blood or body fluids.1 Blood borne infections have been recognised as an occupational hazard for nearly 50 years.2 However, it is only in the last 20 years that there has been a widespread recognition of the specific risk posed to health care workers (HCWs) by blood borne viruses such as hepatitis B, C and human immunodeficiency virus (HIV). While as many as twenty blood borne pathogens can be transmitted through accidental needlesticks,3 the potentially life threatening are HIV, hepatitis B virus (HBV) and hepatitis C virus (HCV).4 A health care worker’s chance of contracting HIV after an HIV-infected accidental needlestick is one in 250,5 while the chance of contracting HBV after an accidental needlestick is one in 20.4 The chances of contracting HCV after an HCV-contaminated accidental needlestick average 3.5 in 100.6
There is lack of information about the various factors that cause accidents with needles. Surveillance programs that provide in-depth analysis of needlestick accidents are an important tool for obtaining this information.7 The analysis of the data collected is a vital component of the surveillance program, and can provide useful information for designing effective prevention strategies. The purpose of this study was to analyze self-reported cases of needlestick injuries in health care workers in Buraidah Central Hospital. The incidence of injuries as well as the nature and circumstances under which they occurred, were explored.
Methods
Buraidah Central Hospital Buraidah is a 212-bed secondary care hospital with a nursing staff of 215 (158 female nurses, 57 male nurses) and 108 physicians. The hospital provides medical services to the general population.
The objectives of this study were to determine the incidence of needlestick injuries in health care workers, investigate the factors that cause these injuries and identify the areas in which the prevention program needs improvement. Needlestick injuries are recorded as a part of the ongoing surveillance program of the infection control department at the hospital. A retrospective review of the infection control department records of needlestick injuries between January 2002 and December 2003 was conducted. These included percutaneous injuries from hypodermic and suturing needles and stylets of intravenous canulae as well as other sharp objects. Recorded data included the age, sex, job category and place of work of the health care worker suffering the injury and the details of the incident, which included the type of pricking agent and the circumstances under which the injury occurred. The data was analyzed in the statistical package SPSS 10.0 for Windows.
Results
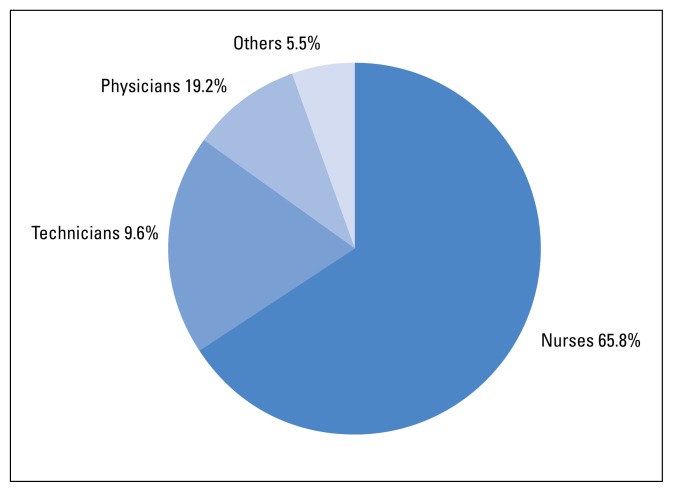
A total of 73 NSIs were reported to the infection control department during the 2-year period of 2002–2003. There were 34 (46.57%) injuries in 2002 and 39 (53.43%) injuries in 2003. Of the 73 HCWs who were injured by needlesticks, 44 (60.3%) were female and 29 (39.7%) male. The mean age of individuals was 32.5±8.1 years, with a minimum age of 20 years and a maximum of 55 years. The nurses (n=48) were the most commonly injured group of workers, which constituted 65.8% of all incidences reported. Fourteen (19.2%) of the incidents were reported by doctors and 7 (9.6%) by technicians. Non-clinical support staff such as cleaners and ward attendants accounted for 4 (5.5%) injuries (Figure 1). The incidence of needlestick injuries, for nurses and doctors, was 0.11 needlesticks per nurse per year and 0.06 needlesticks per doctor per year, respectively.
Figure 1.
Job category of persons with needlestick injuries.
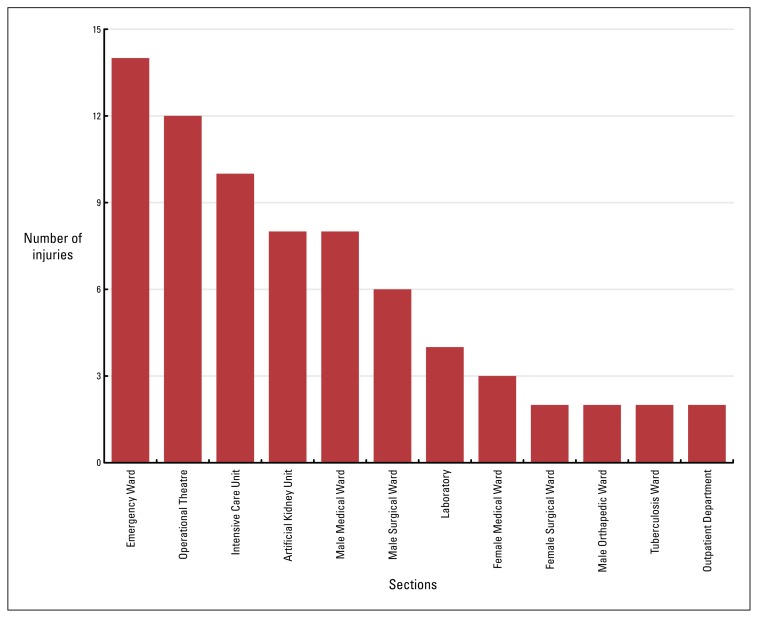
Thirty-one of 73 injuries (42.5%) occurred in hospital wards, 14 (19.2%) in the accident and emergency department, 12 (16.4%) in the operation theatre, 10 (13.7%) in the intensive care unit, 4 (5.5%) in the lab and 2 (2.7%) incidents were reported from the outpatient department (Figure 2). Twenty-nine (39.7%) of the reported injuries occurred during use of needlesticks and sharp objects, while 44 (60.3%) of the injuries occurred after use. Twenty-nine (39.7%) occurred during a clinical procedure (during surgery, IV-line-related, restless patient and handling/passing device), 39 (53.4%) occurred after a clinical procedure but before disposal (recapping, collision with sharp and disposal related), and 5 (6.8%) occurred after disposal (concealed sharps). There were 21 (29%) needlestick injuries due to recapping of used syringes, the most common group. Fourteen (19%) of the injuries were reported while doing surgical procedures. The other major group was collision with sharps, which involves incidences like transferring blood from the syringe to the vial and missing the target. Eight (11%) of these incidents are disposal related, which includes incidences like segregating surgical instruments from the used needles and syringes, for disposal (Table 1).
Figure 2.
Incidence of needlestick injuries in different sections of Buraidah Central Hospital.
Table 1.
Breakdown of needlestick injuries by procedure in Buraidah Central Hospital, Buraidah (2002–2003)
| Procedure | Number | Percentage |
|---|---|---|
| Recapping | 21 | 29% |
| During Surgery | 14 | 19% |
| Collision with Sharp | 10 | 14% |
| Disposal related | 8 | 11% |
| IV line related | 6 | 8% |
| Restless patient | 6 | 8% |
| Concealed Sharps | 5 | 7% |
| Handling/Passing Device | 3 | 4% |
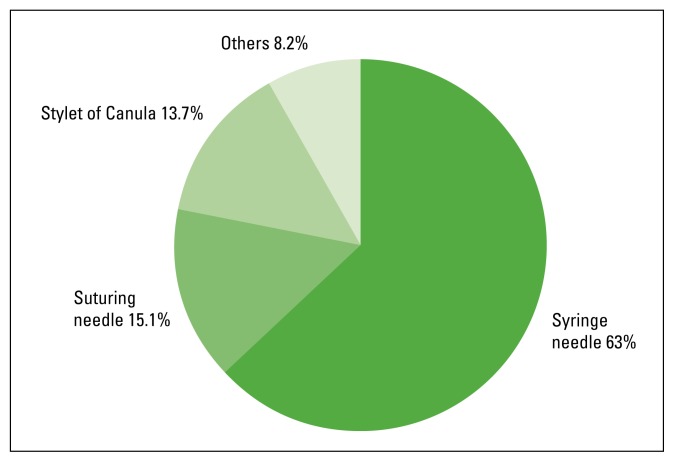
The most common procedure reported to cause such injury in each of the job categories also varied. Among physicians, most of the injuries occurred while suturing or doing a surgical procedure. Nurses sustained a needlestick while recapping a needle, disposing of a used needle, injecting medicine, or drawing blood. Sanitary staff had NSIs while disposing of garbage in the majority of cases. The syringe needles were responsible for 46 (63%) of the injuries, stylet of canula for 10 (13.7%), suturing needles for 11 (15.1%) and 6 (8.2%) of the injuries were caused by other sharps like k-wire, fistula needle and surgical blades (Figure 3).
Figure 3.
Pricking agents responsible for needlestick injuries.
Discussion
Needlestick injuries present the single greatest occupational hazard to medical personnel.8 In well-designed studies, injuries from contaminated needles and other sharp devices used in health care settings have been associated with transmission of more than 20 different blood borne pathogens to health care workers.9
Several studies on needlestick and sharp injuries among health care workers have been reported from the Kingdom of Saudi Arabia10–14 as well as all around the world (Table 2). In this study, the rates for needle-stick injuries for nurses (0.11 Needlestick/nurse/year) and doctors (0.06 Needlesticks/doctor/year) was much lower when compared to the studies by Stotka et al and Aiken et al. This difference may be explained on the basis that these were prospective surveys in which cases of NSIs were actively sought, while the present study was a retrospective analysis of self-reported cases. Another factor, which may be responsible for lower number of cases in this study, is underreporting, as needlestick injuries have historically been underreported. The percentage of underreporting in published studies has ranged from 40% to 80%.22–28
Table 2.
Results of Some Studies of Needlestick injuries in Health care workers
| Reference | Results |
|---|---|
| Menish et al, 2002, Saudi Arabia14 | 364 injuries in a period of 4 years in 600 bed tertiary care hospital with 2800 employees |
| Abu-Gad & Al-Turki, 2001 Saudi Arabia13 | 282 injuries in 11 of 38 hospitals of eastern province with a reporting system |
| Stotka et al, 1991 USA15 | 0.57 Needlesticks per doctor per year and 0.83 Needlesticks per nurse per year in General medical wards of two Virginia acute care hospitals |
| Armstrong SE, 199116 | 4.27 to 12.4 per 100 registered nurses |
| Neurberger JS et al, 199117 | 43.5 per 1,000 employees over a 12-month-period in University Teaching Hospital |
| Whitby M et al, 199118 | 6.9 per 100 full-time nursing staff per year before intervention to 15.4 per 100 full-time nursing staff per year after intervention |
| Aiken LH et al, 199719 | 0.8 per nurse per year |
| Ruben FL et al, 198320 | 579 incidents over a period of 4 years in a 450 bed hospital |
| Mc Cormick et al, 1981 USA21 | 316 Needlestick injuries over a period of 47 months |
The preponderance of injuries occurring in nursing staff is a common feature of studies around the world.13,29,30 In two major state funded teaching hospitals in USA, nurses accounted for 40% of victims of needlestick injuries and physicians for 28%. Laboratory workers, technicians and housekeeping staff comprised another major portion (17%) of needlestick injuries.31 In another study published by Ruben et al, nurses were involved in 66% of instances.20
In our study the percentage of reported incidents involving doctors (19.2%) is lower than other studies, which which varied from 10% to 28%. Anecdotal evidence suggests that this group is inclined to self-assess and not report such injuries, contributing to the apparent lower incidence.32 Of reported incidents, 8% involved ancillary staff and others, including porters and cleaners who invariably sustained needlestick injuries due to the careless disposal of sharps by clinical staff.
According to the results of our study, 45.1% of the injuries occurred in the wards, while 16.9% occurred in the operation theatre. This is comparable to the data from the National Health Services (NHS) in Scotland where 53% of injuries occurred in hospital wards, while 16% occurred in the operation theatre. However only 3% of the injuries were reported in the accident and emergency department in NHS Scotland data, as compared to a high rate of 19.2% in our study.32
The percentage of injuries occurring during clinical use (39.7%) is comparable to the data from National Surveillance System for Hospital Health Care Workers (NaSH), which shows that approximately 38% of percutaneous injuries occur during use.33 In the most recent report of EPINet data, 32% of sharps injuries occurred during use of the sharp, and 26% after use but before disposal, while approximately 11% were related to disposal of the sharps.34 In our study the risk for sustaining a needlestick injury was more after a procedure (53.4%). This fact highlights the need for clinical HCWs to stay alert to the possibility of injury until the procedure is completed and the “sharp” disposed of.
The most common pricking agent in our study was the syringe needle (55%), a frequency similar to other studies.13,35 Data from an EPINet study of 77 hospitals showed that by far the largest number of sharps injuries are caused by disposable syringes.36 Of nearly 5 000 percutaneous injuries reported by hospitals participating in National Surveillance System for Hospital Health Care Workers (NaSH) between June 1995 and July 1999, 62% were associated with hollow-bore needles-primarily hypodermic needles attached to disposable syringes (29%) and winged-steel (butterfly-type) needles (13%).33 The study conducted by Shiao et al in 2002 and Puro et al, in 2001 showed hollow-bore needles responsible for 64% and 65% of the NSIs respectively,37,38 while in the study of McGeer et al, the injuries with hollow-bore needles were as high as 98%.37
Understanding the epidemiology of NSIs in the target population is critical to implementing control measures. This study allowed identification of the major activities leading to these injuries. The study shows that recapping of used syringes is responsible for 29% of the injuries. Past studies of needlestick injuries have shown that 10% to 25% occurred when recapping a used needle.20,21,38,39,40
A significant portion of needlestick injuries occur when manipulating IV lines or administering IV and IM injections as well as after use and before disposal.3 Similar findings in our study, in which 30% of the injuries occurred when manipulating IV lines or administering injections in restless patients or in collisions with sharps immediately after these procedures (Table 1).
Needlestick injuries are an important and continuing cause of exposure to serious and fatal diseases among health care workers. Clearly, not every needlestick injury is preventable, but research has shown that almost 83% of injuries from hollow bore needles can be prevented.35
This study also concludes that for prevention of needlestick injuries, awareness amongst health care workers should be increased. Continuing education and training programs for hospital staff are recommended to keep them up to date and aware of new needlestick policies, practices and procedures.
References
- 1.Haiduven Donna. Prevention of Sharps Injuries in Healthcare Workers. [Accessed 2004 July 18]. http://www.bbriefings.com/pdf/14/ACF795E.PDF.
- 2.Grosheide P, Van Damme P. Communicable Disease Series. World Health Organisation; Copenhagen: 1996. Prevention and control of hepatitis B in the community; pp. 9–25. [Google Scholar]
- 3.Jagger J, Hunt EH, Brand-Elnaggar J, Pearson RD. Rates of needlestick injury caused by various devices in a university hospital. N Engl J Med. 1988;319:284–288. doi: 10.1056/NEJM198808043190506. [DOI] [PubMed] [Google Scholar]
- 4.De Laune S. Risk reduction through testing, screening, and infection control precautions—with special emphasis on needlestick injuries. Infect Control Hosp Epidemiol. 1990;11(10):563–565. [PubMed] [Google Scholar]
- 5.Jagger J, Pearson RD. Universal precautions: Still missing the point on needlesticks. Infect Control Hosp Epidemiol. 1991;12(4):211–213. doi: 10.1086/646326. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control. Risk of acquiring hepatitis C for health care workers and recommendations for prophylaxis and follow-up after occupational exposure. Hepatitis Surveillance Report. 1996;56:3–6. [Google Scholar]
- 7.Any one interested in Info on needlestick Injuries. [Accessed 2004 June 29]. http://www.ofaaa.bc.ca/wwwboard/messages/415.html.
- 8.Kelen GD, Fritz SF, Qaqish B. Unrecognized HIV infection in emergency Department patients. N Engl J Med. 1998;38:1645–1650. doi: 10.1056/NEJM198806233182503. [DOI] [PubMed] [Google Scholar]
- 9.Chiarello LA. Selection of Safer Needle Devices: A Conceptual Framework for Approaching Product Evaluation. Am J Infect Control. 1995;23(6):386–395. doi: 10.1016/0196-6553(95)90271-6. [DOI] [PubMed] [Google Scholar]
- 10.Shanks NJ, Al-kalai D. Occupation risk of needlestick injuries among health care personnel in Saudi Arabia. J Hosp Infect. 1995 Mar;29(3):221–226. doi: 10.1016/0195-6701(95)90332-1. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy M, O’Reilly D, Mah MW. The use of a quality-improvement approach to reduce needlestick injuries in a Saudi Arabian hospital. Clin Perform Qual Health Care. 1998;6(2):79–83. [PubMed] [Google Scholar]
- 12.Paul T. Self-reported needlestick injuries in dental health care workers at Armed Forces Hospital Riyadh, Saudi Arabia. Mil Med. 2000;165(3):208–210. [PubMed] [Google Scholar]
- 13.Abu-Gad HA, Al-Turki KA. Some epidemiological aspects of needlestick injuries among the hospital health care workers: Eastern province, Saudi Arabia. Eur J Epidemiol. 2001;17(5):401–407. doi: 10.1023/a:1013793301772. [DOI] [PubMed] [Google Scholar]
- 14.Memish ZA, Almuneef M, Dillon J. Epidemiology of needlestick and sharps injuries in a tertiary care center in Saudi Arabia. Am J Infect Control. 2002;30(4):234–241. doi: 10.1067/mic.2002.118841. [DOI] [PubMed] [Google Scholar]
- 15.Stotka JL, et al. An analysis of blood and body fluid exposures sustained by house officers, medical students, and nursing personnel on acute-care general medical wards: a prospective study. Infect Control Hosp Epidemiol. 1991;12:583–590. doi: 10.1086/646246. [DOI] [PubMed] [Google Scholar]
- 16.Armstrong SE. The cost of needle-stick injuries. Reprinted from The impact of safer medical devices. Nursing Economics. 1991;9(6):426–433. [PubMed] [Google Scholar]
- 17.Neuberger JS, Harris J, Kundin WD, et al. Incidence of needlestick injuries in hospital personnel: Implications for prevention. Am J Infect Control. 1991;12(3):171–175. doi: 10.1016/0196-6553(84)90094-4. (1984) [DOI] [PubMed] [Google Scholar]
- 18.Whitby M, Stead P, Najman JM. Needlestick injury: Impact of a recapping device and an associated education program. Infect Control Hosp Epidemiol. 1991;12:220–225. doi: 10.1086/646328. (1991) [DOI] [PubMed] [Google Scholar]
- 19.Aiken LH, Sloane DM, Klocinski J. Hospital nurse’s occupational exposure to blood: Prospective, retrospective and institutional reports. Am J Public Health. 1997;87(1):103. doi: 10.2105/ajph.87.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruben FL, Norden CW, Rockwell K, Hruska E. Epidemiology of accidental needle puncture wounds in hospital workers. Am J Med Sci. 1983 Jul-Aug;286(1):26–30. doi: 10.1097/00000441-198307000-00004. [DOI] [PubMed] [Google Scholar]
- 21.McCormick RD, Maki DG. Epidemiology of needlestick injuries in hospital personnel. Am J Med. 1981 Apr;70(4):928–32. doi: 10.1016/0002-9343(81)90558-1. [DOI] [PubMed] [Google Scholar]
- 22.Hamory BH. Underreporting of needlestick Injuries in a University Hospital. Am J Infect Control. 1983;11:174–177. doi: 10.1016/0196-6553(83)90077-9. [DOI] [PubMed] [Google Scholar]
- 23.Roy E, Robillard P. Underreporting of Accidental Exposures to Blood and Other Body Fluids in Health Care Settings:An Alarming Situation (abstract) Adv Exposure Prev. 1995;1(4):11. [Google Scholar]
- 24.Mangione CM. Occupational Exposure to HIV: Frequency and Rates of Underreporting of Percutaneous and Mucocutaneous Exposures by Medical House Staff. Am J Med. 1991;90:85–90. doi: 10.1016/0002-9343(91)90510-5. [DOI] [PubMed] [Google Scholar]
- 25.Haiduven D, Simpkins S, Phillips E, Stevens DA. Percutaneous/Mucocutaneous Injury Reporting in a PublicTeaching Hospital. J Hosp Inf. 1999;41:151–154. doi: 10.1016/s0195-6701(99)90053-1. [DOI] [PubMed] [Google Scholar]
- 26.Osborn EHS, Papadakis MA, Gerberding JL. Occupational exposures to body fluids among medical students. A seven-year longitudinal study. Ann Intern Med. 1999;130(1):45–51. doi: 10.7326/0003-4819-130-1-199901050-00009. [DOI] [PubMed] [Google Scholar]
- 27.CDC (Centers for Disease Control and Prevention) Evaluation of safety devices for preventing percutaneous injuries among health-care workers during phlebotomy procedures. Minneapolis-St.Paul, New York City, and San Francisco, 1993–1995. MMWR. 1997a;46(2):21–25. [PubMed] [Google Scholar]
- 28.EPINet. Exposure prevention information network data reports. University of Virginia: International Health Care Worker Safety Center; 1999. [Accessed 2004 June 26]. http://www.healthsystem.virginia.edu/internet/epinet/soi99.cfm. 1.1.1. [Google Scholar]
- 29.US Department of Health and Human Services. National Institute for Occupational Safety and Health (NIOSH) NIOSH ALERT Preventing Needlestick Injuries in Health Care Settings. 2000. [Accessed 2004 June 16]. Publication No. 2000–108. http://www.cdc.gov/niosh/2000-108.html.
- 30.Lymer UB, Schutz AA, Isaksson B. A descriptive study of blood exposure incidents among health care workers in a university hospital in Sweden. J Hosp Inf. 1997;35:223–235. doi: 10.1016/s0195-6701(97)90210-3. [DOI] [PubMed] [Google Scholar]
- 31.Needlestick Injuries among health care workers in Washington State 1996–2000. [Accessed 2004 June 01]. http://www.lni.wa.gov/Safety/Research/files/NeedleStick.pdf.
- 32.Needlestick injuries: sharpen your awareness. [Accessed 2004 July 18]. http://www.show.scot.nhs.uk/sehd/publications/nisa/nisa-04.htm.
- 33.Preventing needlestick injuries in health care settings. [Accessed 2004 June 16]. www.cdc.gov/niosh/2000-108.html.
- 34.Perry J, Parker G, Jagger J. EPINet Report: 2001 Percutaneous Injury Rates. Adv Exposure Prev. 2003;6(3):32–36. [Google Scholar]
- 35.Ippolito G, Puro V, Petrosillo N, Pugliese G, Wispelwey B, Tereskerz PM, Bentley M, Jagger J. Prevention, Management, and Chemoprophylaxis of Occupational Exposure to HIV. Charlottesville, VA: Advances in Exposure Prevention, International Health Care Worker Safety Center; 1997. [Google Scholar]
- 36.International Health Care Worker Safety Center. Exposure Prevention Information Network. Uniform Needlestick and Sharp Object Injury Report 77 Hospitals, 1993–1995 [February 1998] 1995. [Accessed 2004 June 6]. www.dir.ca.gov/OSHSB/sharps2.HTML.
- 37.McGeer A, et al. Epidemiology of needlestick injuries in house officers. J Infect Dis. 1990;162:961–964. doi: 10.1093/infdis/162.4.961. [DOI] [PubMed] [Google Scholar]
- 38.McCormick RD, et al. Epidemiology of hospital sharps injuries: a 14-year prospective study in the pre-AIDs and AIDs eras. Am J Med. 1991;91:301S–307S. doi: 10.1016/0002-9343(91)90386-c. [DOI] [PubMed] [Google Scholar]
- 39.Krasinski K, LaCouture R, Holzman RS. Effect of changing needle disposal systems on needle puncture injuries. Infect Control. 1987;8(2):59–62. doi: 10.1017/s0195941700067084. [DOI] [PubMed] [Google Scholar]
- 40.Yassi A, McGill M. Determinants of blood and body fluid exposure in a large teaching hospital: hazards of the intermittent intravenous procedure. Am J Infect Control. 1991;19(3):129–135. doi: 10.1016/0196-6553(91)90018-8. 1991. [DOI] [PubMed] [Google Scholar]