Abstract
BACKGROUND
Recurrent and complex bilateral inguinal hernias are associated with a high recurrence rate. Giant prosthetic reinforcement of the visceral sac (GPRVS) is popular in America and Europe, but there are no prospective data from Iran.
PATIENTS AND METHODS
From 20 March 1995 to 20 March 2003, 234 patients (227 men and 7 women) with 420 inguinal hernias (186 bilateral and 48 unilateral) underwent repair using a large polyester mesh based on Stoppa’s preperitoneal technique. Mean age was 60 years (range 25 to 88) and 44.8% had one or more comorbid conditions. In 154 instances, the relapsed hernia had already been operated once or twice for recurrence.
RESULTS
Mean hospital stay after surgery was 2.2 days (range 1–13 days). The mean operative time was 45 minutes (range 30–75 minutes). General complications were one case of upper gastrointestinal bleeding, one case of ileus and one case of atelectasis. Local complications consisted of three local seroma formations. In no instance was postoperative neuralgia, chronic pain or testicular atrophy, mesh infection or death reported. Follow-up was obtained in all patients. The recurrence rate was 0.71% (3 of 420) per inguinal repaired or 0.85% (2 of 234) per patient. Factors predicating a high risk for recurrence included large hernia size (>5 cm), failure of one or more previous repairs (65.8%, 154 of 234), chronic cough and associated lower abdominal hernias.
CONCLUSION
GPRVS is anatomic, sutureless, tension-free and the absolute weapon to eliminate all type of groin hernias. No other technique produces better results for the repair of recurrent and re-recurrent groin hernias.
Recurrent and complex inguinal hernias are associated with a high risk of recurrence. A recent review indicates that first-time recurrent hernia repair fail in 1% to 30% of cases, that second-time recurrent repairs do so at the rate of 3% to 35%, and third-time or more repairs fail in 50% of cases.1 Reasons for these dismal results include failure to identify the patients and factors affecting recurrence such as chronic obstructive pulmonary disease, large size and weak fascial structures. In addition, the use of anterior repair for recurrences requires extensive dissection, often including the enlargement of an already large defect and the use of scarred and devascularized tissue under tension for the repair.
Stoppa et al2,3 first described a technique aimed at eliminating hernias of the groin by reinforcing the peritoneum with a giant polyester mesh. With this giant prosthetic reinforcement of the visceral sac (GPRVS), the mesh acts as an artificial endoabdominal fascia and prevents visceral sac extension through the myopectineal orifice where all groin hernias begin.2
There is consensus on the use of a prosthetic mesh for the surgical treatment of recurrent groin hernia, bilateral groin hernia, complex hernias and connective tissue disease with groin hernia. This article is a prospective evaluation of 234 consecutive GPRVS used to repair recurrent or complex bilateral inguinal hernias.
Patients and Methods
We prospectively evaluated patients undergoing bilateral or unilateral Stoppa groin hernia repair over the period from 20 March 1995 to 20 March 2003 with particular reference to indications, postoperative hospital stay, complications, and recurrence. The criteria for selection were recurrent and re-recurrent hernias (unilateral or bilateral) or primary bilateral hernia with associated risk factors for recurrence, including chronic cough, connective tissue disease, or other lower abdominal hernias. The repairs were performed at Sina hospital, Tabriz University of Medical Sciences, Tabriz, Iran. Follow-up was obtained by examination at clinic. Follow-up examination was scheduled in all patients from 0 to 96 months.
Surgical Technique
The technique developed by Stoppa was used with some minor modifications.2–6 A urinary catheter was positioned before surgery in all patients. Prophylactic intravenous antibiotics (cephazolin 1 gram every 6 hours) were administered in all patients before, during, and after the procedure, until the drains were removed.
The procedure is performed under general anesthesia or spinal anesthesia. A midline incision extends from 2 cm below the umbilicus to 1 cm above the symphysis pubis. The preperitoneal space is entered with blunt dissection aided by sharp dissection when the peritoneum is scarred from prior operations (appendectomy, herniorrhaphy, prostatectomy or lower abdominal laparotomy). The dissection includes the retropubic space of Retzius and Bogros, and continues laterally, dissecting the posterior portion of the rectus abdominis muscle on the far side of the operator, proceeding behind the epigastric vessels, progressing to the retroinguinal space and further exposing the iliopsoas muscle. Direct hernias are identified and reduced. Indirect defects can be divided and the proximal peritoneum oversewn, leaving the distal peritoneum in place un-dissected and attached to the cord. In sliding indirect hernias, the sac is dissected from the cord structures. The spermatic cord and the gonadal vessels are parietalized by dissecting them from their peritoneal attachment to allow them to lay tension-free in the posterior pelvis. This step averts the need for mesh splitting. The polyester mesh (Mersilene, Ethicon) is fashioned as a chevron, and placed in the preperitoneal space with long clamps. The size of the prosthesis is measured on the patient. The width equals the distance between the anterior superior iliac spines, and vertically measures the distance between the umbilicus and the symphysis pubis plus 6 cm. In obese patients, the mesh should be several centimeters wider than the interspinous dimensions. The mesh is held in place without the need for fixation since the intra-abdominal pressure forces the mesh to lay flat between the peritoneum and the fascial layers. The mesh is oriented so that it stretches transversally. The assistant retracts the parietal wall while the surgeon depresses the peritoneal sac with the left hand, pulling toward him or her to open the parietoperitoneal space. The patient is in the Trendelenburg position to facilitate exposure. First, the inferior midline clamp is placed in the space between the pubis and bladder (Retzius space), then the inferior lateral clamp, and then the lateral angel clamp (over the iliac vessels). Finally, the upper lateral clamp extends the length as far as possible to unfold the prosthesis laterally. Each time a clamp is inserted, the assistant immobilizes it until the operator releases the visceral sac, abdominal wall retractor, and the clamp is removed. The process is repeated on the opposite side. The patient is placed in the reversed Trendelenburg position, and the clamps are removed. The mid-portion of the superior border of the prosthesis is then sutured with a single stitch of absorbable suture to the posterior rectus sheath. None of the hernial defects were repaired. Closed suction drainage was positioned in all patients and was removed after 24 to 48 hours. Eight hours following the procedure, patients received clear liquids and were advanced to regular diet as tolerated. Patients without comorbid conditions were discharged after 24 hours of observation if they could void and tolerate liquids. Closed suction drainage eliminates seromas and hematomas and is not necessarily an indication for hospital admission. Patients return for follow-up one week postoperatively. Following the procedure, patients were not restricted in their activity but were encouraged to return to their previous lifestyle without limitation as soon as pain or discomfort permits.
Results
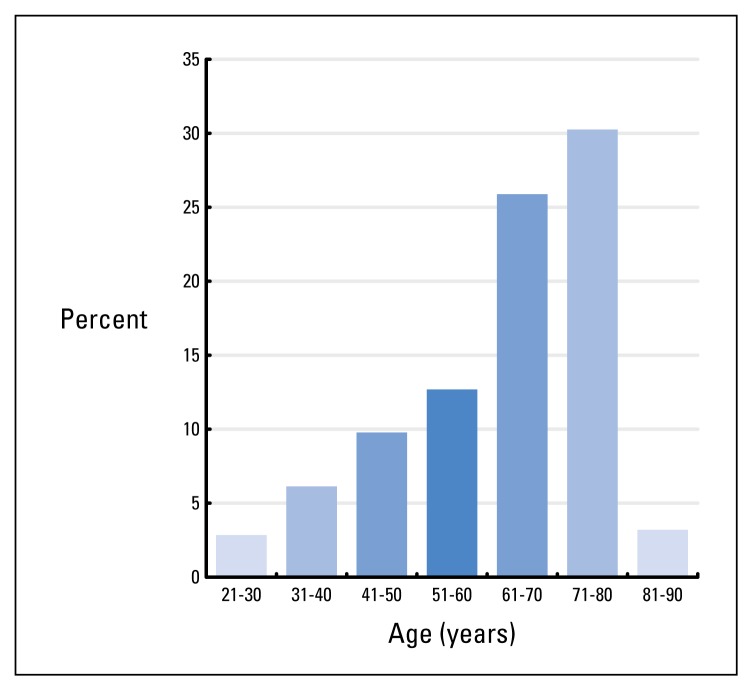
A total of 420 inguinal hernias (186 bilateral, 48 unilateral) were repaired in 234 patients (Table 1). There were 227 men (97%) and 7 women (3%). The mean age of patients was 60 years (range, 25 to 88). One hundred thirty-seven patients were older than 60 years, including seven older than 80 years (Figure 1). Concomitant medical problems were observed in 105 patients (44.8%). Cardiovascular diseases were the most frequent (65 cases), followed by urologic diseases (mainly benign prostatic hypertrophy, 20 cases) and pulmonary diseases (20 cases including bronchectasis, chronic obstructive pulmonary disease, asthma, chronic cough and tuberculosis). Risk factors predicating a high risk for recurrence included a large hernia size (>5 cm) in 34% (80 of 234), failure of one or more previous repairs in 65.8% (154 of 234), and associated lower abdominal hernia in 9.8% (23 of 234). In the 234 patients with 420 groin hernias, 80 hernias were primary, 143 were recurrent and eleven re-recurrent.
Table 1.
Type of groin hernias in 234 patients with Stoppa groin hernia repair.
| Type of groin hernias | Number |
|---|---|
| Bilateral indirect inguinal hernia | 55 |
| Bilateral direct inguinal hernia | 93 |
| Bilateral inguinal hernia (right: direct, left: indirect) | 16 |
| Bilateral inguinal hernia (right: indirect, left: direct) | 22 |
| Unilateral hernia | 48 |
Figure 1.
Age distribution in 234 patients who underwent Stoppa groin hernia repair.
GPRVS was completed in all 234 patients, and no patient required conversion to another technique. Bilateral GPRVS was used in 186 patients to repair 372 hernias, of which 212 were recurrent and 160 primary groin hernias. Unilateral GPRVS via a subumbilical incision has been used to manage 48 complex and recurrent hernias of the groin. General anesthesia was used in 51 patients, and spinal anesthesia in 183 cases. The mean operative time was 45 minutes (range 30–75), and there was no complication related to anesthesia (Table 2). There were 216 right-sided hernias and 204 left-sided hernias. No anterior counterincision was required. All patients were repaired with polyester mesh (Mersillene, Ethicon).
Table 2.
Mean operative time and postoperative complications in 234 patients with Stoppa groin hernia repair.
| Number | |
|---|---|
| Mean operative time | |
| 30 minutes | 92 |
| 45 minutes | 71 |
| 60 minutes | 50 |
| 75 minutes | 21 |
| Postoperative complications | |
| Ileus | 1 |
| Upper gastrointestinal bleeding | 1 |
| Atelectasis | 1 |
| Seroma | 3 |
| Recurrence | 2 |
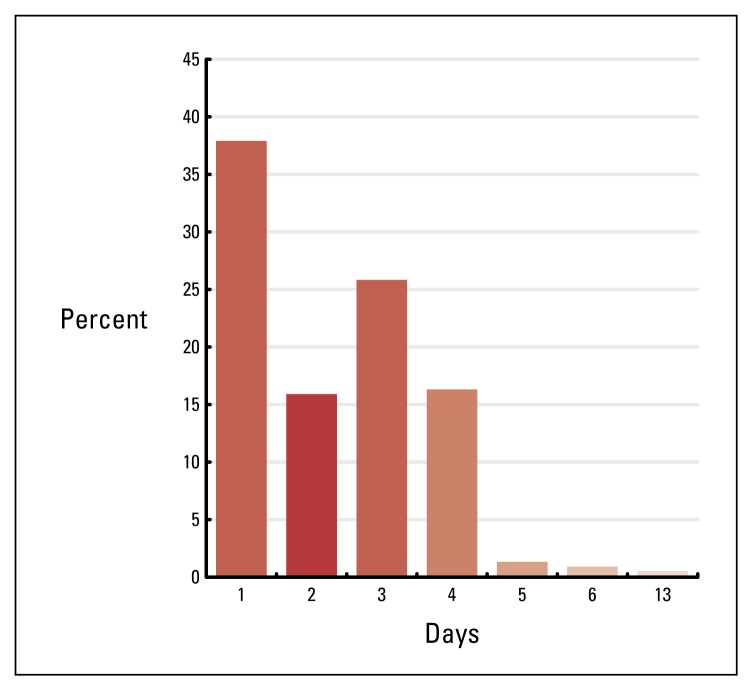
The mean length of hospital stay was 2.2 days (range, 1–13 days). Ninety-seven patients without comorbid conditions were discharged 24 hours after the operation (Figure 2). Upper gastrointestinal bleeding from peptic ulcer, which required several blood transfusions and a prolonged hospital stay (13 days), occurred in one patient. There was one case of ileus and one case atelectasis. Local complications consisted of three cases of seromas in the dead space of the hernia sac, which were resolved with needle aspiration without delaying recovery or discharge (Table 2).
Figure 2.
Postoperative hospital stays in 234 patients.
No neuropathies, chronic pain or testicular atrophies occurred. No deep infections occurred in the patients who had polyester prosthesis implanted, and no polyester prosthesis had to be removed. The recurrence rate was 0.71% (3 of 420) per inguinal repaired or 0.85% (2 of 234) per patient. The latter two recurrences occurred 6 and 4 months after repair, respectively. Mean time off from work after surgery was 2 weeks (range 1–3 weeks).
Discussion
The risk of recurrent herniation must be balanced against the risks, the complexity and the magnitude of the hernioplasty. Some patients do not want general anesthesia and others do not want mesh.10,18,19,20,21 For primary inguinal hernias of all types, anterior inguinal hernioplasty with the aid of local anesthesia and without prosthetic reinforcement will remain the first choice of surgeons and patients because it is simple and safe and produces acceptable results. It can be done in an ambulatory surgical center in selected patients, and can be successfully performed in even the most debilitated patient, if necessary.
More recently, primary as well as recurrent hernias have been successfully repaired using prosthetic material with the safe utilization of open or laparoscopic approaches. In recent commentary, Rutkow stated that the recurrence rate has been the major, if not sole, criterion on which the efficacy of any herniorrhaphy is judged despite the fact that over the last half century, recurrence rates have been similar regardless of which technique is used. In addition to recurrence rates, socioeconomic factors, technical difficulty, complication rates, short and long-term postoperative discomfort, time of return to daily activities should also play a role in the equation.
Nyhus12 points out that modern hernia surgery should individualize the repair to each clinical situation, and some would add, to each social and economic circumstance. In this study, the GPRVS was mostly used in a group of older patients, with multiple medical problems as well as recurrent or complex bilateral hernias. Miller13 and colleagues demonstrated that the simultaneous repair of bilateral inguinal hernias is safe and does not result in an increased recurrence rate.
The posterior approach allows a bilateral approach through a single incision and reduces the risk of nerve injury, neuralgia, ischemic orchitis, testicular atrophy and chronic pain. In this study, the choice of GPRVS for primary bilateral inguinal hernias was individualized. Primary bilateral hernias were considered as complex if they were associated with factors predicating a high risk for recurrence such as multiplicity, large size or were associated with comorbid aggravating factors (e.g., COPD) based on the recurrence rate reported after traditional hernia repair. The GPRVS takes advantage of the unique properties of the polyester mesh: (1) it does not encapsulate, thus minimizing the formation of fluid collections; (2) it has no plastic memory and adapts to the endopelvis; and (3) it induces fibrous ingrowth preventing migration. The same material (polyester) has a long track record of safety, and has been used for many years in vascular surgery to replace major vessels.
The GPRVS was evaluated prospectively because even though this technique is popular in America and Europe, there are no prospective data from Iran. The complication rate of 3% per patient repaired (one major, 0.43% and 6 minor, 2.56%) is comparable with other reports.2,15,21 There were no mesh or superficial wound infections. The mean length of stay (2.2 days) reflects the large population of elderly patients with complex medical and social situations. In comparison, 97 of 234 patients without comorbid conditions were discharged after 24 hours of the operation. Overall, the patients were very satisfied with the procedure. The absence of limitation in the level of activity postoperatively allowed all patients, including industrial and agriculture workers, to return early to full activity. This lack of restriction in activity is based on the safety provided by the wide tension-free mesh prosthesis, which evenly distributes the intra-abdominal forces against the lower abdominal wall (Pascal’s hydrostatic principle). Large prostheses are kept in place by intra-abdominal pressure; they need not be fixed or associated with a repair of the hernial orifice.
Recently, with the advent of laparoscopic repair,8,12 the armamentarium of the surgeon has increased and so has the confusion as to which technique is best to use. In patients presenting with large chronic or recurrent hernias, laparoscopy is often technically challenging because the difficulties associated with reduction of the hernia or adhesions, especially in cases where mesh has been previously used. Prior abdominal interventions (e.g. appendectomy) often complicate laparoscopic dissection of the retroperitoneum. Laparoscopy uses smaller prostheses and requires mesh fixation with the attendant risk of nerve injury. The technique of GPRVS with large polyester mesh cannot be readily transferred to laparoscopy because of the reduced size of the operative field and limited exposure, and the need for parietalization of the cord structures.
In our series, the 0.85% (2 of 234) recurrence rate is lower than other studies using the GPRVS technique7,11,14,15,16,17,18 and compares well with recurrence rates reported with other techniques. In the experience of Stoppa et al,2 others, and our study with GPRVS, all recurrences occurred within 6 months and were ascribed to technical failures. In GPRVS, the replacement of the endoabdominal fascia seals the inguinal, femoral, and obturator canals as well as all other potential sites of weakness in the lower abdomen. For this reason, late recurrences are not reported. In contrast, recurrences after anterior techniques accumulate over time, and long-term follow-up is mandatory. In our study, 93% of patients were followed up for 6 months or more, and late recurrences in these patients were unlikely. Early in the experience, the two recurrences occurred 6 and 4 months after the procedure and were due to technical error.
In theory, recurrences after GPRVS are inconceivable.21 Nevertheless, they occur. Although other factors may be at play, most recurrences can be attributed to technical errors, most often related to the size and placement of the mesh. No other hernioplasty produces better results for recurrent and especially re-recurrent groin hernias. For excellent results, the mesh must be polyester that is correctly sized, shaped and placed. Finally, the operation is easy and the dissection pleasing to all surgeons. Exceptional skill and extensive experience do not appear necessary for good results. The GPRVS is a safe and effective way to treat selected patients with recurrent unilateral or complex bilateral inguinal hernias.
References
- 1.Schumpelick V, Zinner M, editors. Atlas of hernia surgery. Toronto, Philadelphia: BC Decker; 1990. p. 209. [Google Scholar]
- 2.Stoppa RE. The preperitoneal approach and prosthetic repair of groin hernia. In: Nyhus LM, Condon RE, editors. Hernia. ed 4. Philadelphia: JB Lippincott; 1995. [Google Scholar]
- 3.Alexandre JH, Bouillot JL. Recurrent inguinal hernia: surgical repair with a sheet of Dacron mesh the inguinal route. Eurg J Surg. 1996;162:29–33. [PubMed] [Google Scholar]
- 4.Stoppa RE. The treatment of complicated groin and incisional hernias. World J Surg. 1989;13:5445. doi: 10.1007/BF01658869. [DOI] [PubMed] [Google Scholar]
- 5.Stoppa RE, Rives JL. The use of Dacron in the repair of hernias of the groin. Surg Clin North Am. 1984;64(269) doi: 10.1016/s0039-6109(16)43284-6. [DOI] [PubMed] [Google Scholar]
- 6.Lerut JP, Luder PJ. Giant prosthetic reinforcement of the visceral sac in inguinal hernia repair: Stoppa operation. In: Maddern GJ, Hiatt JR, Phillips EH, editors. Hernia repair open vs laparoscopic approach. New York: Churchill Livingstone; 1997. pp. 133–144. [Google Scholar]
- 7.Beets GL, van Seldere D, Baeten CG. Longterm results of giant prosthetic reinforcement of the visceral sac for complex recurrent inguinal hernia. Br J Surg. 1996;83:203. [PubMed] [Google Scholar]
- 8.Felix EL, Michas CA, Mcknight RL. Laparoscopic repair of recurrent hernias. Surg Endos. 1995;9:135–139. doi: 10.1007/BF00191953. [DOI] [PubMed] [Google Scholar]
- 9.Mathonnet M, Cubertafond P, Gainant A. Bilateral inguinal hernias: Giant prosthetic reinforcement of the visceral sac. Hernia. 1988;1:93. [Google Scholar]
- 10.Mozingo DW, Walters MJ, Otchy DP, Rosenthal D. Preperitoneal synthetic mesh repair of recurrent inguinal hernias. Surg Gynecol Obstet. 1992;174:33–35. [PubMed] [Google Scholar]
- 11.Nyhus LM. The recurrent groin hernia: therapeutic solution. World J Surg. 1989;13:541–544. doi: 10.1007/BF01658868. [DOI] [PubMed] [Google Scholar]
- 12.Nyhus LM. Individualization of hernia repair: a new era. 1993;114:1–2. [PubMed] [Google Scholar]
- 13.Miller AR, van Heerden JA, Naessens JM, O’Brien PC. Simultaneous bilateral hernia repair. A case against conventional wisdom. Ann Surg. 1991;213:272–276. doi: 10.1097/00000658-199103000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rignault DP. preperitoneal prosthetic inguinal hernioplasty through a Pfannenstiel approach. Surg Gynecol Obestet. 1987;173:465. [PubMed] [Google Scholar]
- 15.Shulman AG, Amid PK, Lichtenstein IL. The safety of mesh repair for primary inguinal hernia: results of 3,019 operations from five diverse surgical sources. Am Surg. 1992;58:255–257. [PubMed] [Google Scholar]
- 16.Schaap HM, van de Pavoordt HDWM, Bast TJ. The preperitoneal approach in the repair of recurrent inguinal hernias. Surg Gynecol Obstet. 1992;174:460–464. [PubMed] [Google Scholar]
- 17.Van Damme JP. A preperitoneal approach in the prosthetic repair of inguinal hernia. Int Surg. 1985;70:223. [PubMed] [Google Scholar]
- 18.Wantz GE. Giant prosthetic reinforcement of the visceral sac. Surg Gynecol Obstet. 1989;169:408. [PubMed] [Google Scholar]
- 19.Wantz GE. preperitoneal hernioplasty with mersilene: unilateral giant prosthetic reinforcement of the nvisceral sac. In: schumpelick V, Wantz GE, editors. inguinal hernia repair. Karger; Basel: 1995. [Google Scholar]
- 20.Wantz GE. the technique of giant prosthetic reinforcement of the visceral sac performed through an anterior groin incision. Surg Gynecol Obstet. 1993;177:497. [PubMed] [Google Scholar]
- 21.Wantz GE. Giant prosthetic reinforcement of the visceral sac. Surg Clin North Am. 1998;78:1075. doi: 10.1016/S0039-6109(05)70370-4. [DOI] [PubMed] [Google Scholar]
- 22.Vogt DM, Curet MJ, Pitcher DE. Preliminary results of a prospective randomized trial of laparoscopic onlay versus conventional inguinal herniorrhaphy. Am J Surg. 1995;169:84–90. doi: 10.1016/s0002-9610(99)80114-7. [DOI] [PubMed] [Google Scholar]