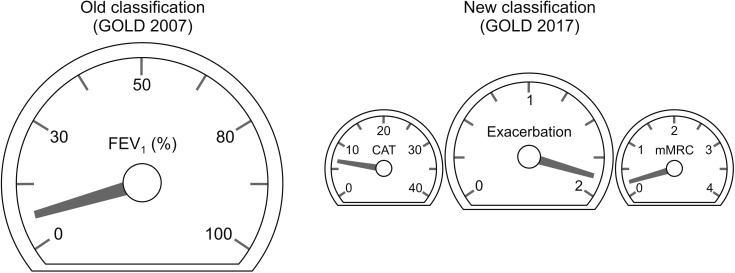
Chronic obstructive pulmonary disease (COPD) is a preventable and treatable disease which is characterized by respiratory symptoms and airflow limitation1. It is a leading cause of death in worldwide. Classification of COPD is very important since treatment is recommended by classification. Old COPD classification is based on spirometry result. In Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2007 document2, post bronchodilator forced expiratory volume in 1 second (FEV1) measured by spirometry was used to classify COPD. FEV1 is easy to measure and result is quite consistent. Moreover, measurement of FEV1 is standardized worldwide. There is no room for bias in measuring FEV1. GOLD 2007 classified COPD as stage I to IV based on post bronchodilator FEV1(%).
In 2011, GOLD committee changed classification of COPD from I–IV to ABCD. Main reason for this change is that there was some discrepancy between lung function and quality of life3. Moreover, history of exacerbation is more powerful predictor for future exacerbation than FEV1 (%)4. Later in 2017, FEV1 (%) was removed from criteria for classification between high and low risk groups1. Spirometry result is still mandatory when diagnose of COPD. However, it is no longer considered when classifying COPD patients (Figure 1).
Figure 1. Comparison between Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2007 and 2017 classification. FEV1: forced expiratory volume in 1 second; CAT: Chronic Obstructive Pulmonary Disease Assessment Test; mMRC: modified Medical Research Council.
Since the release 2017 GOLD documents, there have been debates whether GOLD 2017 classification is better than old spirometric classification. Gedebjerg et al.5 showed that GOLD 2017 classification does not predict mortality more accurately than 2007. Data from PLATINO study showed that GOLD 2007 classification shows more stability over time compared with GOLD 2013.6 Recently, Candemir et al.7 investigated whether there was a difference between GOLD 2017 classification and 2007 in clinical variables in patients with COPD. Interestingly, similar values of FEV1 were found between group A and C. Also, mean FEV1 was not different at all between B and D. Moreover, group A and C showed similar result of incremental shuttle walk test (ISWT). On the contrary, GOLD 2007 classification was well correlated with many clinically important variables such as dyspnea, quality of life, anxiety scores, body mass index, fat free mass index, and ISWT.
These previous results showed that still FEV1 (%) is good and useful markers for classification of COPD. It is not yet concluded whether removal of FEV1 in GOLD 2017 was good decision or not. However, as the Candemir et al.7 mentioned, GOLD 2017 classification might not represent the severity of COPD sufficiently well. Probably the combination of both spirometric stage and combined assessment of GOLD 2017 is important, especially for estimating clinical variables.
Footnotes
Conflicts of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, et al. Global strategy for the diagnosis, management, and prevention of Chronic Obstructive Lung Disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195:557–582. doi: 10.1164/rccm.201701-0218PP. [DOI] [PubMed] [Google Scholar]
- 2.Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176:532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 3.Agusti A, Calverley PM, Celli B, Coxson HO, Edwards LD, Lomas DA, et al. Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:122. doi: 10.1186/1465-9921-11-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hurst JR, Vestbo J, Anzueto A, Locantore N, Mullerova H, Tal-Singer R, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363:1128–1138. doi: 10.1056/NEJMoa0909883. [DOI] [PubMed] [Google Scholar]
- 5.Gedebjerg A, Szepligeti SK, Wackerhausen LH, Horvath-Puho E, Dahl R, Hansen JG, et al. Prediction of mortality in patients with chronic obstructive pulmonary disease with the new Global Initiative for Chronic Obstructive Lung Disease 2017 classification: a cohort study. Lancet Respir Med. 2018;6:204–212. doi: 10.1016/S2213-2600(18)30002-X. [DOI] [PubMed] [Google Scholar]
- 6.Menezes AM, Wehrmeister FC, Perez-Padilla R, Viana KP, Soares C, Mullerova H, et al. The PLATINO study: description of the distribution, stability, and mortality according to the Global Initiative for Chronic Obstructive Lung Disease classification from 2007 to 2017. Int J Chron Obstruct Pulmon Dis. 2017;12:1491–1501. doi: 10.2147/COPD.S136023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Candemir I, Ergun P, Kaymaz D, Tasdemir F, Egesel N. The comparison of clinical variables in two classifications: GOLD 2017 combined assessment and spirometric stage of chronic obstructive pulmonary disease. Tuberc Respir Dis. 2018;81:281–288. doi: 10.4046/trd.2017.0114. [DOI] [PMC free article] [PubMed] [Google Scholar]