Summary
Osteoarthritis (OA) is a chronic prevalent condition that affects the synovial joints and can lead to disability. There is no single treatment that is known to cure OA. Most treatments have aimed at reducing symptoms or slowing the progression of the disease and its consequences. Exercise therapy is a common intervention in treating OA, with primary aims of improving functional movement and managing the problems associated with abnormal functional movement. We review the underlying process of exercise treatment and its importance for OA disability. A brief description of OA disease and an OA disability model are introduced, and then the importance of exercise and trends in prescribing exercises for OA are discussed. Finally, future directions and suggestions for research in this field are described.
Osteoarthritis (OA) is a chronic prevalent condition that affects the synovial joints and can lead to disability. In 1995, nearly 40 million people had OA in the USA, and by the year 2020 almost 60 million (18.2% of population) Americans will be affected by arthritis.1 In Canada, 10% of adults reported a long-term health problem due to OA.2 In Arabic countries there are not enough data to report the prevalence of OA. However, there is no reason to expect that OA is less prevalent in Arabic countries.
Exercise therapy is a common intervention used in treating OA, with the primary aims of improving functional movement and managing the problems associated with abnormal functional movement. The purpose of this article is to review the underlying process of exercise treatment and its importance for OA disability. The review uses the knee joint as an example but there are implications for other joints.
Osteoarthritis pathogenics and disability
Osteoarthritis is not an inflammatory disease, as implied by the name, but a degenerative joint disease.3 Studies have shown that OA involves more than just simple mechanical wear and tear; it involves mechanical, chemical, immunological, hormonal and/or genetic factors (Table 1).3–6 Although the pathological etiology of OA is not fully understood, it is not difficult to describe. OA disease causes pain, swelling, and loss of motion of the joint due to the bones under the cartilage rubbing together. The worst pain occurs due to bone-to-bone weight-bearing or due to pieces of bone or cartilage breaking off and floating inside the joint space.3,6 In chronic cases, the joint may lose its normal shape by losing the cartilage and forming osteophytes that grow on the edge of the joint.
Table 1.
Summary of the clinical, pathophysiologic, biochemical and biomechanical changes that characterize OA. Table contents extracted from text definition of OA by Flores et al5.
| Changes | Characteristics |
|---|---|
| Clinical | Joint pain, tenderness, limitation of movement, crepitus, occasional effusion, swelling, and local (but not systemic) inflammation |
| Pathological | Irregularly distributed loss of cartilage more frequently in areas of increased load, sclerosis of subchondral bone, subchondral cyst, marginal osteophytes, increased metaphyseal blood flow, and variable synovial inflammation |
| Histological | Early fragmentation of the cartilage surface, cloning of chondrocytes, vertical cleft in cartilage, variable crystal deposition, remodeling and eventual violation of tidemark by blood vessels |
| Biochemical | Reduction in the proteoglycan concentration, alteration in collagen fibril size and weave, and increased synthesis and degradation of matrix macromolecules |
| Biomechanical | Alterations of the tensile, compressive, shear proprieties, and hydraulic permeability of the cartilage. Increased stiffness of the subchondral bone. |
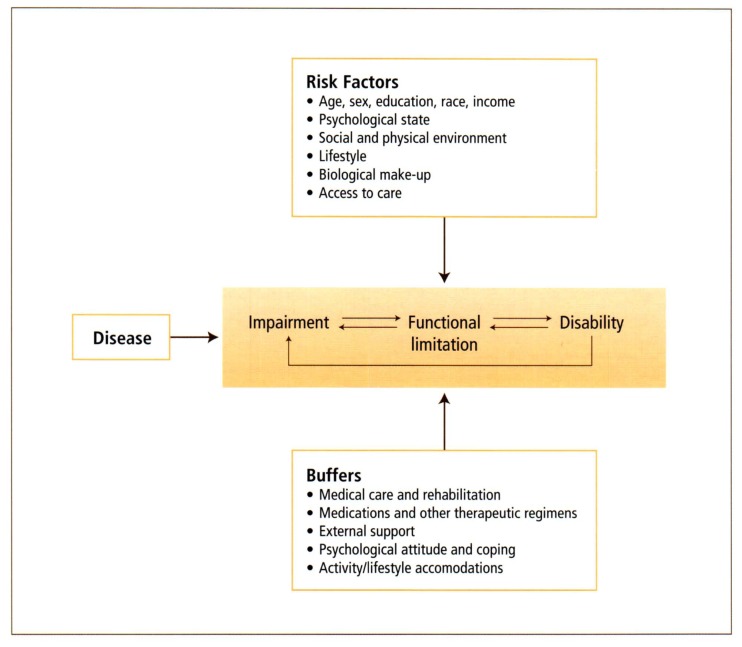
A common disability model that explains the relation between the disease and its role in disability was developed by Nagi.7 Based on that model, Jette8 explained the OA disability process by viewing it as a cyclical process with possible relevant risk factors and buffers (Figure 1). The OA disability model describes exercise intervention as a preventive measure, primary prevention when its target is to prevent the occurrence of the disease, secondary prevention when its target is to prevent the occurrence of functional limitation, and tertiary prevention when its target is to prevent further disability8,9
Figure 1.
Model of osteoarthritis disability cycle and its relation to risk factors and buffers that affect progression of osteoarthritis disease.8
Exercise treatment of osteoarthritis
Currently there are no treatments available that cure the underlying process of OA disease.10 Treatment of OA is mainly directed toward decreasing the symptoms of the condition and slowing or preventing the progress of the condition.9 Therapeutic exercise is a form of physical activity that is provided under the supervision of appropriate health professionals for specific treatment goals. Regular physical activity is associated with lower mortality rates for both older and younger adults. Moreover, it is associated with a decreasing risk for a wide range of diseases and conditions, such as cardiovascular disease, osteoporosis, falling, cancer, diabetes, blood pressure and osteoarthritis.11
Patients with knee OA have a significant decrease in knee muscle strength and control as well as a decrease in velocity during gait in comparison to normal older subjects.12–13 Pain is strongly associated with decreased quadriceps strength even in very early joint degeneration. It has been suggested that quadriceps weakness is a risk factor for OA.17 The main reasons for prescribing exercises in general include (1) achieving therapeutic goals, (2) improving general health and reducing secondary disability, and (3) modifying possible risk factors in disease progression.9,14,15 Minor14 summarized the potential benefits of physical activity and exercise on OA as follows:
Minimizes or slows the pathological process that takes place in the OA joint. Exercise helps in increasing cartilage nutrition and remodeling, increases the synovial blood flow, decreases swelling, and improves muscle strength. Thus, the pathological effect of exercise may include slowing the cartilage degeneration process, decreasing bone stiffness, decreasing joint effusion and improving muscle strength.
Decreases impairments that occur from OA by reducing the main impairment factors. Exercise helps in decreasing pain, improving strength and endurance, and improving range of motion and connective tissue elasticity.
Decreases functional limitation by improving walking speed, gait, and physical activity and decreasing depression and anxiety. Fatigue, reductions in daily activity, poor sleep and depression are common factors associated with the OA condition.
Osteoarthritis may be associated with several disability problems such as decreased social activity, decreased quality of life, increased health risk of inactivity and decreased employment. Improving health status, physical fitness, and quality of life can minimize these disability problems.
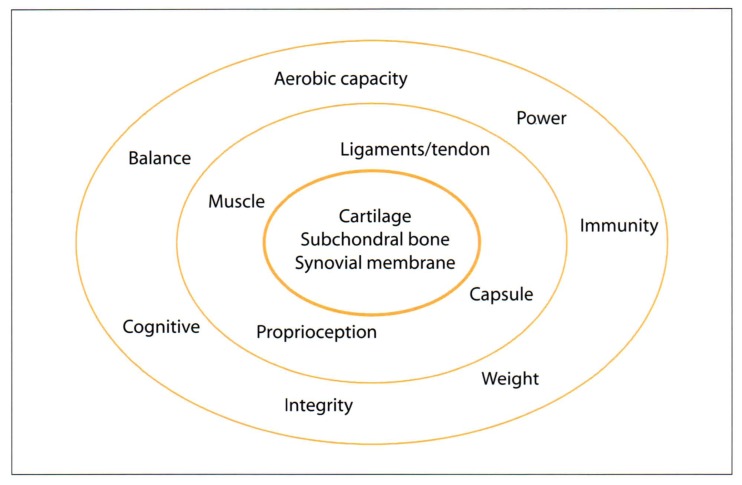
Clinicians used to recommend that subjects with OA rest or avoid exercise based on the supposition that cartilage does not heal or repair itself and that OA is simply a condition of excessive wear and tear.10,16 The emphasis on rest and not doing exercise in OA has been reversed as a preponderance of studies have shown that (1) OA is more than a simple wear and tear condition; its consequences can lead to physical limitation and disability beyond the affected joint; and (2) articular cartilage can heal or repair itself, despite the fact that the repair is only a mix of hyaline and fibro-cartilage.10,14–16 As a result of these observations, we suggest that exercise benefits be viewed in a comprehensive manner at the following three levels: first, at the micro level or inner part of the joint that includes cartilage, synovial tissue, and subchondral bones; second, at the functional level of the joint, in which the joint is considered a functional unit that includes functional structures such as surrounding muscles, ligaments, tendons, capsule, proprioceptors, etc; and third, at a whole body system level from the point of view of the cardiovascular, musculoskeletal, neurophysiological, immunological and/or psychological systems (Figure 2). Inside the joint, weight-bearing exercise can increase the pumping action which helps in increasing intra-articular nutrient diffusion and stimulates cartilage healing or repair.15 Defining the joint as functional unit means including surrounding functional structures such as muscles, ligaments, tendons, capsule, and proprioceptors as part of a joint.10 It has been shown that exercise is very beneficial in improving muscle strength, joint range of motion, proprioception, and feedback.10,14–17 By knowing that persons with arthritis tend to be less active and less fit than their unaffected peers, exercise benefits should be viewed from a broader perspective that includes cardiovascular and musculoskeletal prospectives.18
Figure 2.
Structural levels where exercise might cause changes. The inner circle represents the microstructure of the joint, the middle circle the joint as a functional unit, and the outer circle the whole body system.
The benefits of exercise intervention in OA have been shown in many clinical studies that compared exercise treatment to placebo or non-exercise treatments.17–27 Kover et al18 conducted a controlled trial consisting of eight weeks of a supervised walking program and found significant improvement in timed walking distance and self-reported pain and functional status after the intervention compared to the control group. Moreover, the control group demonstrated a decrease in walking distance over the same period. Ettinger et al19 conducted a single blind clinical trial to study the effects of structured exercise programs on self-reported disability in 439 older subjects with knee OA. The results showed that both the group receiving aerobic exercise and the group receiving resisted exercise made greater gains in self-reported pain and disability scores after the exercise interventions than the group receiving health education. Functional capacity (walking, lifting and carrying, stair climbing and the time needed to get in and out of a car) was improved significantly for those who participated in the aerobic exercise group. Moderate aerobic and resisted exercises did not increase the severity of the knee OA, based on x-ray diagnosis. Chamberlain et al23 evaluated the effects of a 4-week exercise program that was designed to increase the strength and endurance of knee OA muscles and reported decreased pain and increased strength, endurance and function. Borjesson et al24 evaluated the effect of two 4-week exercise programs involving individual weight-bearing exercises and supervised group therapy consisting of non-weight-bearing exercises. Patients in both exercise groups experienced an overall improvement compared to the control group. van Baar et al22 performed a systematic review of 11 randomized clinical trials that studied the effectiveness of exercise therapy in patients with osteoarthritis of the hip and knee. The study concluded that exercise therapy is beneficial for knee OA patients.
Despite discrepancies in study criteria and outcomes, the above research attests to a positive effect of exercise treatment for OA. It is not clear whether positive functional outcomes were due to direct changes in the joint structure, changes in the surrounding tissue, in the cardiovascular capacity, and/or in participants’ subjective opinion of change, or a combination of these. The effectiveness of exercise on improving function and reducing pain can be viewed in three ways. First, exercise can reduce the load across painful areas within the joint and cause biomechanical changes.26 Second, exercise can modify the neurological and/or psychological perception of pain.13,26 Third, exercise can alter physiological, metabolic or structural properties of the joint.16 However, these possibilities have not been explored in detail. To understand the underlying effects of exercise those effects at the different levels explained in Figure 2 need to be investigated. There is also a need to study the relationships among biomechanical, physiological, cognitive, and functional changes that occur due to intervention for OA.
Exercise prescriptions for osteoarthritis patients
Several factors have to be considered when selecting or prescribing exercise for OA patients. Ettinger et al10 posed the following questions:
- Does exercise exacerbate the disease?
- What type of exercise is the most beneficial?
- What is the most cost-effective method of screening?
- What are the optimal frequency, intensity and duration of exercise?
- Should exercise programs be facility-based or home-based?
Despite the promising results of many studies that recommend exercise for OA, there is no consensus on the answers to these questions about exercise programs for OA. One of the major concerns in exercise intervention for OA is the possibility that weight-bearing activity might not be recommended for OA joints because it involves wear and tear of joint cartilage which might accelerate disease progression. Advocates of the notion that weight bearing harms the OA knee joint have supported the use of open kinetic chain strengthening exercises (non-weight-bearing exercises such as knee isokinetic exercises, knee extension and flexion exercises from a sitting position, straight leg raising exercises, and knee curl exercises.) The specificity of such exercises is geared toward pure strengthening instead of improving a specific functional activity. However, issues relating to exercise extend beyond simple consideration of cartilage wear and tear. Exercise potentially involves considerations of joint stability, joint motion, joint effusion, synovial fluid level, position sense, balance, and conduct of daily activities. Focusing only on open chain exercises compromises the specificity and selectivity principles of training, which state that optimal gains in a motor activity are made when the exercise most closely resembles the activity.28,30,31 Improvements in daily function would be best served by exercise resembling the daily activity. Thus, the trend in rehabilitation exercise for OA is to emphasize functional types of exercises that include weight-bearing activity. The term “functional” relates to those activities that most closely resemble day-to-day activities, such as rising to stand, ascending and descending stairs, stepping, walking, squatting and lunging. Functional exercises (some might refer to them as closed kinetic chain exercises) have been shown to have many benefits over open chain exercises: they provide axial loading to the joint, exercise more than one joint at the same time, involve both concentric and eccentric muscle contraction, simulate daily activity, enhance muscle contraction and minimize the shear forces at the knee joint.32–34 Other proposed benefits include increased proprioception and coordination of the lower extremity and increased carry over to functional activities, including a quicker return to daily activities and advanced physical activities such as sports activities.35
Prescribing the proper exercises for a specific condition and for a specific person requires a melding of the knowledge of disease and injury, exercise physiology, exercise biomechanics, and exercise behavior in an accessible, enjoyable and affordable setting. To design an exercise program for OA, the essential components that have to be taken into account are the mode(s), the intensity, the duration, the frequency and the progression of exercises. The American College of Sports Medicine (ACSM) recommends a framework of exercise sessions that include a warm-up, a core activity and a cool-down component.21 Most of the studies that have dealt with exercise interventions for OA disease introduced exercise programs that ranged in duration from 30 to 45 minutes per session, 2 to 3 times per week, with an intensity of heart rate of 50% to 80% of HR maximum.17,24,27,33 These parameter ranges agreed with the ACSM guidelines, which recommend that exercise sessions should include a 10 minute warm-up, 20 to 60 minutes of endurance activities and 5 to 10 minutes of cooling-down.33 However, this formula is dependent on the mode of exercise, the objectives of the program and the type of subjects. Stretching exercises are better suited to the warm-up and cool-down phases and take the form of slow static stretches that are sustained for 10 to 30 seconds with a minimum of 4 repetitions for each exercise. The duration of aerobic exercises needs to be 30 minutes or longer at a moderate intensity to produce the appropriate aerobic fitness level. The resistance training should be performed at least twice a week, no more than 30 minutes for each session, with at least 48 hours of rest between sessions, at an intensity that elicits a fairly hard exertion rate (perceived exertion rating of a 12–13). Moreover, resistance exercises should achieve an overload initially by increasing the number of repetitions, and then by increasing resistance. The ACSM guidelines suggest that exercise intensity for elderly subjects with orthopedic conditions should start at a low level and progress according to the tolerance and preferences of the subject, with training sessions not longer than 60 minutes, to maintain the appropriate adherence to exercises.33 Based on the ACSM guideline and previous study in this area, we recommend a mixed type of exercise—aerobic and strength—for a period of 8 weeks, 3 times per week. Caution is needed when prescribing exercises for knee OA to avoid over stretching and hypermobility, specifically avoiding carrying loads over 10% of body weight, avoiding vigorous impact load exercises such as jumping, hopping or running up and down stairs and observing signs of overtraining or systematic changes such as joint redness, swelling, etc. An instructor should always be ready to modify or change exercise type as needed.
Future directions
It is clear that exercise intervention is beneficial in reducing pain and disability in subjects with knee OA. The following may account for reported changes in pain and function following exercise: first, exercise can reduce the load across painful areas within the joint and cause biomechanical changes;28 second, exercise can modify the neurological and/or psychological perception of pain;28 third, exercise can alter physiological, metabolic or structural properties of the joint.16 Despite evidence of change, none of these underlying processes have been understood. Moreover, the optimal exercise program for treating OA disease has not been defined. As such, we believe that future studies about exercise intervention for OA should explore (1) the relationship among cognitive, biomechanical, physiological, and functional outcomes of exercise; (2) the optimal type of exercise intervention for OA at different stages of the disease, and (3) the long-term effectiveness of exercise for subjects with knee OA.
Conclusion
The main purpose of this article was to discuss the concept of exercise intervention for OA disease. Studies suggest that the exercise effect should be examined at three levels, namely at the level of the joint, at the joint as a functional unit and at the level of whole body systems. The literature on exercise in OA concludes that exercise is beneficial in reducing pain, improving strength, improving function and reducing disabilities associated with OA. A mix of aerobic, functional, strengthening and stretching training is more beneficial than single modes of activity such as knee strengthening exercises. The specific nature and causes of changes in pain and function after exercise interventions for OA are an area that needs to be explored in future studies. The optimal type, mode, and length of exercise programs and the long-term effect of such exercise are issues that also need to be explored.
References
- 1.Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthr Rheum. 1998;41(5):778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 2.The Arthritis Society (Canada) 2002. www.arthritis.ca.
- 3.Martin DA. Pathomechanics of knee osteoarthritis. Medicine and Science in Sports and Exercise. 1994;26(12):1429–1434. [PubMed] [Google Scholar]
- 4.Hutton CW. Osteoarthritis: The cause not the result of joint failure. Ann Rheum Dis. 1989;48:958. doi: 10.1136/ard.48.11.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flores RH, Hochberg MC. Definition and classification of osteoarthritis. In: Brandt KD, Doherty M, Lohmander LS, editors. Osteoarthritis. Oxford: Oxford Medical Publication; 1998. pp. 13–22. [Google Scholar]
- 6.Felson DT. Epidemiology of osteoarthritis. In: Brandt KD, Doherty M, Lohmander LS, editors. Osteoarthritis. Oxford: Oxford Medical Publication; 1998. pp. 23–41. [Google Scholar]
- 7.Creamer P, Hochberg MC. Osteoarthritis. Lancet. 1997;350(16):1503–1509. doi: 10.1016/S0140-6736(97)07226-7. [DOI] [PubMed] [Google Scholar]
- 8.Jette AM. Musculoskeletal impairments and associated physical disability in the elderly: insights from epidemiological research. In: Bukwalter JA, Goldberg VM, Woo SL, editors. Musculoskeletal Soft-Tissue Aging: Impact on Mobility. 1993. pp. 7–23. [Google Scholar]
- 9.Brandt EN, Pope AM. Enabling America: Assessing the Role of Rehabilitation Science and Engineering. National Academy Press; 1997. Models of disability and rehabilitation; p. 66. [PubMed] [Google Scholar]
- 10.Ettinger WH, Afable RF. Physical disability from knee osteoarthritis: the role of exercise as an intervention. Medicine and Science in Sports and Exercise. 1994;26(12):1435–1440. [PubMed] [Google Scholar]
- 11.US Department of Health and Human Services. Physical activity and health: a report of the Surgeon General. Atlanta, US: Department of Health and Human Services; 1996. [Google Scholar]
- 12.Messier SP, Loeser RF, Hoove J, et al. Osteoarthritis of the knee: effects on gait, strength, and flexibility. Arch Phys Med Rehab. 1992;73(1):29–36. [PubMed] [Google Scholar]
- 13.Hurley MV. The role of muscle weakness in the pathogenesis of osteoarthritis. Rheum Dis Clin North Am. 1999;25:283–298. doi: 10.1016/s0889-857x(05)70068-5. [DOI] [PubMed] [Google Scholar]
- 14.Minor MA. Exercise in the treatment of osteoarthritis. Rheum Dis Clin North Am. 1999;25(2):397–415. doi: 10.1016/s0889-857x(05)70075-2. [DOI] [PubMed] [Google Scholar]
- 15.McKeag DB. Exercise and arthritis. In: Torg JS, Shephard RJ, editors. Current Therapy in Sports Medicine. 3rd Edition. St Louis: Mosby; 1995. pp. 689–696. [Google Scholar]
- 16.Mankin HJ. The reaction of articular cartilage to injury and osteoarthritis. Part 1. N Eng J Med. 1974;291:1285–1292. doi: 10.1056/NEJM197412122912406. [DOI] [PubMed] [Google Scholar]
- 17.Maurer BT, Stern AG, Kinossian B, et al. Osteoarthritis of the knee: isokinetic quadriceps exercise versus an educational intervention. Arch Phys Med Rehab. 1999;80:1293–1299. doi: 10.1016/s0003-9993(99)90032-1. [DOI] [PubMed] [Google Scholar]
- 18.Kovar PA, Allegrante JP, MacKenzie R, et al. Supervised fitness walking in patients with osteoarthritis of the knee. Ann Int Med. 1992;116:529–534. doi: 10.7326/0003-4819-116-7-529. [DOI] [PubMed] [Google Scholar]
- 19.Ettinger WH, Burns R, Messier SP, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. JAMA. 1997;277:25–31. [PubMed] [Google Scholar]
- 20.Chamberlain MA, Care G, Harfield B. Physiotherapy in osteoarthritis of the knee. Int J Rehab Med. 1982;4:101–106. doi: 10.3109/09638288209166889. [DOI] [PubMed] [Google Scholar]
- 21.Borjesson M, Robertson E, Wedenhielm L, et al. Physiotherapy in knee osteoarthritis: effect on pain and walking. Physiother Res Int. 1996;1:89–97. doi: 10.1002/pri.6120010205. [DOI] [PubMed] [Google Scholar]
- 22.vanBarr ME, Dekker J, Oostendorp RAB, et al. The effectiveness of exercise therapy in patients with osteoarthritis of hip or knee: a randomized clinical trial. J Rheumatol. 1998;25:2431–2439. [PubMed] [Google Scholar]
- 23.vanBarr ME, Assendelft WJJ, Dekker J, et al. Effectiveness of exercise therapy in patients with osteoarthritis of the hip and knee. Arthr Rheum. 1999;42(7):1361–1369. doi: 10.1002/1529-0131(199907)42:7<1361::AID-ANR9>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 24.Bautch JC, Malone DG, Vailas AC. Effects of exercise therapy in patients with osteoarthritis: a pilot study of biologic markers. Arthritis Care Research. 1997;10:48–55. doi: 10.1002/art.1790100108. [DOI] [PubMed] [Google Scholar]
- 25.Puett DW, Griffin MR. Published trials of non-medical and noninvasive therapy for hip and knee osteoarthritis. Ann Int Med. 1994;15:133–140. doi: 10.7326/0003-4819-121-2-199407150-00010. [DOI] [PubMed] [Google Scholar]
- 26.Marks R. Further evidence of impaired position sense in knee ostearthritis. Physiother Res Int. 1996;12:127–36. doi: 10.1002/pri.6120010208. [DOI] [PubMed] [Google Scholar]
- 27.Minor MA, Hewett JE, Webel RR, et al. Efficacy of physical conditioning exercise in patients with rheumatoid arthritis or osteoarthritis. Arthr Rheum. 1989;32:1397–1405. doi: 10.1002/anr.1780321108. [DOI] [PubMed] [Google Scholar]
- 28.Irrgang JJ. Modern trends in ACL rehabilitation. In: Prentice WE, editor. Rehabilitation technique in sports medicine. St Louis: Mosby; 1993. pp. 181–194. [Google Scholar]
- 29.Arnheim D, Prentice W. Principle of athletic training. St. Louis: Mosby Year Book; 1993. pp. 528–536. [Google Scholar]
- 30.Durward BR, Bear GD, Rowe PJ. Measurement issues in functional human movement. In: Durward BR, editor. Functional human movement. Oxford: 1999. pp. 1–13. [Google Scholar]
- 31.Fu F, Woo S, Irrgang J. Current concepts for rehabilitation following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1992 doi: 10.2519/jospt.1992.15.6.270. [DOI] [PubMed] [Google Scholar]
- 32.Palmitier RA, An K, Scott SG, et al. Kinetic chain exercise in knee rehabilitation. Sports Med. 1991;11:402–413. doi: 10.2165/00007256-199111060-00005. [DOI] [PubMed] [Google Scholar]
- 33.Franklin BA, Whaley MH, Howley ET, et al. ACSM’s guidelines for exercise testing and prescription. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 34.Rejeski WJ, Ettinger WH, Schumaker S, et al. Assessing performance-related disability in patients with knee osteoarthritis. Osteoarthritis Cartilage. 1994:157–167. doi: 10.1016/s1063-4584(05)80050-0. [DOI] [PubMed] [Google Scholar]
- 35.Farrel MJ, Gibson SJ, Helme RD. Measuring the Activity of Older People with Chronic Pain. Clin J of Pain. 1996;12(1):6–12.. doi: 10.1097/00002508-199603000-00003. [DOI] [PubMed] [Google Scholar]