Abstract
Advances in early detection and therapy have increased the number of prostate cancer survivors, leading to a greater emphasis on examining patient-reported outcomes (PROs). PROs augment clinical outcomes, providing a more comprehensive assessment of the patient experience, including symptoms and quality of life, that may impact the overall evaluation of new therapies. The successful incorporation of PROs into clinical trials requires adherence to key design and analysis principles. We present these principles and argue that adherence to these principles is vital to ensure valid interpretation of clinical trial findings, identify meaningful differences among investigational strategies, and better translate clinical trial results to diverse stakeholders.
Keywords: Patient-reported outcomes, quality of life, prostate cancer
Introduction
Cancer researchers have increasingly aimed to incorporate the patient’s perspective in examinations of new treatments or interventions [1]. Central to this effort is the use of patient-reported outcomes (PROs), which are designed specifically to reflect the patient’s experience with respect to disease, treatment symptoms, and quality of life (QOL), as well as treatment tolerability and toxicity. PROs augment clinical outcomes through more comprehensive assessment of symptoms and side effects associated with investigational therapies and provide alternative endpoints (such as QOL) that may impact the overall evaluation of new therapies. PROs correlate strongly with typical trial outcomes, such as adverse events, and have been found to be predictive of survival outcomes in certain settings [2]. PROs are used throughout the survivorship spectrum to describe the patient experience, from adjuvant treatment settings to palliative care [3–6].
Advances in cancer treatment over many decades have transformed a cancer diagnosis into a chronic disease for many patients [7]. As the number of cancer survivors increases, research has increasingly focused on patient survivorship. There were about 15 million cancer survivors in the United States in 2016, an estimate projected to climb to 26 million by 2040 [8]. Specific to prostate cancer care, prostate cancer survivors represent about 20% of the survivorship pool in the US [9]. Prostate cancer trials may rely heavily on PROs as part of their designs, with trial interpretations increasingly determined by the PRO results that parallel clinical endpoints. In a recent review, metastatic castration-resistant prostate cancer (mCRPC) trials with PROs better determined treatment impact by identifying toxicity versus cancer control tradeoffs and by providing a more comprehensive evaluation of new treatments [10].
Quality of Life in Prostate Cancer
In localized prostate cancer care, the various treatments for primary management of the prostate cancer have been known to differentially impact patient-reported QOL [11,12], an important observation given the limited accuracy of physician report of patient QOL [13]. This has been validated in clinical trials such as ProtecT, in which patients were randomized to watchful waiting versus intervention with radical prostatectomy or radiation therapy [14]. These studies consistently demonstrate unique patterns of QOL changes for each therapy, with greater impact of surgery on urinary continence and radiation therapy on storage urinary symptoms and bowel function.
Given the sizeable population of prostate cancer survivors and the importance of assessing QOL in prostate cancer, four PRO domains (physical and mental well-being, fatigue, and pain) have been identified as priorities for assessment by a National Cancer Institute (NCI) working group on the inclusion of PRO measures in prostate cancer clinical trials [15]. The European Expert Consensus Panel for the Management of Metastatic CRPC recommended that PROs (pain and QOL) were appropriate as secondary outcomes in Phase III trials [16]. The Prostate Cancer Clinical Trials Working Group 3 recommended the use of patient-reported assessment of adverse events (PRO-CTCAE) developed by the NCI, with a particular emphasis on physical and functional well-being and pain [17,18].
The interpretations of several prostate cancer studies have been influenced by the examination of general and prostate cancer-specific QOL [19]. In their randomized, multicenter study comparing antiandrogen therapy with chemical castration for advanced prostate cancer patients, Chodak, et al., found that the antiandrogen therapy group exhibited better QOL scores through 6 months of treatment [20]. Osoba and colleagues found larger and longer-lasting improvements in QOL among mCRPC patients treated with mitoxantrone and prednisone [21]. SWOG trial S9916 established docetaxel as providing superior survival outcomes for patients with mCRPC [22,23]. In SWOG S9916, patients completed the EORTC QLQ-C30 and the EORTC prostate cancer module (PR25) as well as the McGill Pain Questionnaire Short Form at study randomization, and again 10 weeks, 6 months, and 1 year later. Patients randomized to docetaxel had similar global QOL and pain scores as those randomized to mitoxantrone. Within the subdomain of the EORTC QLQ-C30 of nausea/vomiting, docetaxel patients exhibited a worsening of their symptoms compared with mitoxantrone patients in whom these symptoms subtly improved. Otherwise, the QOL instrument subdomains did not differ by treatment group. Thus, the survival advantage offered by docetaxel did not come at the expense of increased QOL burden.
PRO Design Principles
The inclusion of PROs in cancer trials can provide key insight into patients’ study experience, symptoms, and response to treatments. The successful incorporation of PROs into clinical trials requires adherence to several basic design principles. These principles are broadly characterized as: 1) the use of hypothesis-driven research questions, 2) use of validated PRO instruments, 3) the feasibility of PRO assessment in the context of the trial’s main objective(s), 4) minimizing respondent burden on patients and sites, and 5) avoiding bias in the assessments of PRO outcomes (Table 1).
Table 1.
Key design and analysis principles for studies utilizing patient reported outcomes
| Principle | Concerns | Strategies |
|---|---|---|
| Hypothesis-driven research questions |
|
|
| Validated instruments |
|
|
| Limited patient and site burden |
|
|
| Feasibility |
|
|
| Assessment design |
|
|
| Statistical design |
|
|
| Missing data strategies |
|
|
Hypothesis-driven research questions
The inclusion of PROs in clinical trials should be predicated on investigator’s hypotheses regarding patient experiences and anticipated associations with the investigational therapies. This hypothesis-driven approach permits easier interpretation of clinical impact and provides a valuable patient perspective on the cancer treatment experience. In addition, by focusing only on pertinent QOL questions based on prior observations, the reliance on hypothesis-driven research questions limits the excessive use of PROs in trial settings, thereby reducing the possibility of false positive findings and the burden of form completion for patients and data management for study sites.
Use of validated instruments
Descriptive and comparative examinations of QOL within a study setting must rely on validated instruments. The validation of a PRO is a stepwise process that assures that the instrument accurately measures what it is intended to measure, and measurably demonstrates attributes of validity, reliability, and responsiveness [1,24]. Translations into selected languages specified in eligibility must also be formally executed and responsive to the anticipated study population [25]. Validated instruments should not be altered as this may affect the survey validity. Similarly, extracting single questions from an instrument may subvert the validity of the construct being assessed.
Feasibility
The incorporation of PROs must be feasible within the constraints of a clinical trial. To facilitate feasibility, eligibility criteria for participation in the QOL portion of the study must be clear and limited. Generally, eligibility are limited to eligibility for the clinical study and the ability to complete PRO assessments in their native language with an available language-specific validated instrument. Ideally, all patients in the clinical trial are included in the QOL study to avoid selection bias. In certain instances – such as when QOL endpoints are not vital to the inference of the clinical endpoint – participation in a QOL substudy may be optional, to remove any potential hurdles to patient participation in the clinical study.
Limited patient and site burden
The completion of PRO instruments may be burdensome to patients [26]. However, the elucidation of the patient experience of clinical trial participation is invaluable in assessing the risks and benefits of study treatments, and the use of PROs is generally accepted by patients [27,28]. Thus, we recommend cognizance of respondent burden and limiting the use of PROs to those which inform study-specific hypotheses. Some recommend a threshold of time required for completion of PROs of 20 minutes for baseline assessments and 10–15 minutes for follow-up assessments [29]. This also benefits research team staff, who require adequate resources for the administration and collection of PRO data. Limiting PRO burden helps ensure maximal accrual through reduction in potential hurdles to patient enrollment and follow-up.
Assessment of PROs
The amount of follow-up required for assessment of QOL outcomes must balance the need to assess meaningful differences with the risk of increasing non-response. Importantly, PRO data collection should start at baseline. The duration of the primary QOL endpoint must be sufficient to detect clinically important changes in QOL domains. Yet, as follow-up duration increases, non-response increases, with potential impact on outcome inference, especially if non-response patterns differ by study arm [26,30]. Furthermore, long-term QOL assessments increase the burden to sites and patients and must be justifiable in the context of the study hypotheses. Thus the PRO assessment schedule must minimize overall dropout and differential dropout by study arm. This can be achieved, in part, by aligning PRO assessments with clinical follow-up visits. Such an alignment will also facilitate interpretation of possible relationships between PROs and clinical endpoints. Automated reminder notices and the utilization of electronic PRO and reminder systems can further minimize missing PRO data. PRO assessments should not be linked with clinical outcome status (such as disease progression) to avoid inducing an artifactual statistical dependence between clinical and QOL outcomes, leading to biased study interpretations.
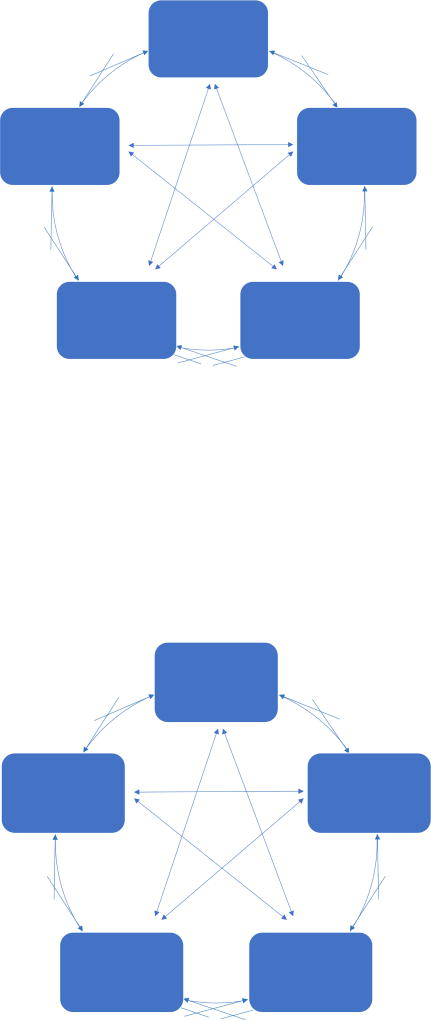
These key design principles are related and induce either a virtuous or a negative cycle, depending on the study design. For instance, the use of hypothesis-driven research questions to provide the foundation for QOL study designs also limits patient burden and enhances feasibility. In contrast, QOL designs without a priori hypotheses may be cumbersome for researchers and burdensome for patients in a manner that is not compensated for by the return value of the research. Figure 1 illustrates the interwoven relationships among the key design principles outlined above.
Figure 1.
Key PRO and QOL design principles and their interrelationships
PRO Analysis Principles
PRO design principles should be incorporated alongside key analysis principles to facilitate reliable and interpretable PRO results. Analysis principles pertain to the statistical design for testing PRO hypotheses and strategies for dealing with missing PRO data.
Statistical Design
PRO statistical designs typically aim to identify a minimally important difference (MID) between arms in a specified PRO instrument. MIDs for validated PRO instruments are available in the literature, and are usually derived from anchor-based (i.e., use of a reference point that is correlated with a QOL domain score) or distribution-based (i.e., use of the standard deviation of observed QOL domain scores) methods. If an MID has not been specified for an instrument, effect size estimates can be used instead. The effect size represents the ratio between the absolute difference in mean PRO scale scores by study arm and the standard deviation of that difference. Cohen has previously suggested that effect sizes can be categorized as small (0.2), medium (0.5), and large (0.8) [31]. Effect sizes from 1/3 to 1/2 a standard deviation are common [32].
MIDs or effect sizes should be assessed at selected follow-up times after trial registration (e.g., 6 months). Power calculations account for the sample size, the MID, and the anticipated standard deviation at a given timepoint. Sample sizes should be large enough to allow comparisons by treatment arm with full power (i.e., >80%). Consistent with such a design, and to aid in interpretation, the main statistical method used for data analysis will often emphasize the difference by arm in specified PRO scale scores at a single assessment time, using linear or logistic regression approaches. However, multiple follow-up assessments are common, and longitudinal analyses should also be included where possible to examine changes in QOL over time between study arms. The use of longitudinal modeling with linear mixed models–with the patient participant as the random effect–can better account for the spectrum of assessments with increased power, although the potential for informative missing data by study arm to influence the interpretation may be increased [33,34]. In either case, covariate adjustment will account for any stratification factors used to balance the randomization assignment and—unless the change in QOL score between baseline and follow-up assessments is the primary endpoint—should also include the baseline PRO score. Other important demographic or clinical factors thought to be associated with the relationship between the intervention and the PRO, such as patient age, can be used in covariate adjustment, preferably pre-specified in the protocol.
Missing Data
Missing PRO data can occur due to patient dropout as well as submission of incomplete PRO forms. Missing data will influence the interpretation of PRO data. The influence of missing data on the results can be reduced, though not wholly eliminated, if appropriately accounted for in the analysis.
To minimize the amount of missing data, a system of automated prospective reminder notifications to sites encouraging timely and complete submission of PRO forms will enable sites to better anticipate follow-up assessments and plan for communication with patients to facilitate data collection. Retrospective queries to sites for missing data are generally inadequate due to the inevitability that patients will already have completed their clinic visit. The developing use of electronic PRO platforms, allowing patients to complete PROs on mobile devices or through web pages should enhance data collection long-term [35].
Even the best quality control practices will not prevent missing PRO data. Patterns of missing PRO data should be routinely monitored to detect potential problems. To identify whether missing data patterns are related to known prognostic factors for the study outcome, the relationship between intervention assignment and important baseline stratification variables between those with and without endpoint data can be examined using interaction tests to assess whether missing PRO data are potentially informative. Missing data patterns can also be analyzed using cohort plots [36]. Mean scores for different cohorts of patients are plotted based on the number of assessments they contributed; if, for instance, missingness depends on the variable itself at the time of dropout (i.e., worse scores at dropout are correlated with fewer assessments), then patterns of missing data are consistent with a non-ignorable mechanism, or non-random missing data [37]. In this case, sensitivity analyses can be conducted using methods such as pattern mixture models, which enable modeling of the observed missing data patterns through covariate adjustment [38,39,40].
Example: The Use of PROs in a Metastatic Prostate Cancer Trial
As an example of the PRO design and analysis principles described above, we present the QOL substudy of a SWOG trial comparing standard systemic therapy (SST) with SST plus definitive treatment of the primary tumor in metastatic prostate cancer (SWOG S1802). As background, men with metastatic prostate cancer have extended expected survival time and may require substantial palliative care for local progression of the primary tumor. This necessitates the implementation of PROs in the studies of new therapeutic strategies for the management of metastatic prostate cancer. Our goal was to compare patient-reported urinary function and bother scores over time by treatment arm. Key design and analysis principles for the study are outlined in Table 2. We hypothesize that men randomized to SST will have worse urinary function and bother scores over time than men receiving SST and definitive treatment. The primary PRO questionnaire is the Expanded Prostate Cancer Index Composite-26 (EPIC-26), a validated instrument that measures urinary, sexual, and bowel symptoms in function and bother domains [41] and was selected by the International Consortium for Health Outcomes Measurement (ICHOM) as the preferred prostate cancer-specific QOL instrument for the assessment of men with localized and advanced prostate cancer [42]. The EPIC-26 is estimated to take 10 minutes to complete and will be administered at baseline and four additional follow-up timepoints through 3 years, limiting patient and site burden. Eligible patients for the QOL study must only be eligible for the clinical study, and be able to complete the EPIC-26 in English or Spanish. The assessment schedule is designed to limit the burden of data collection on sites and patients as well as to minimize missing data. The PRO assessments are scheduled to occur alongside clinical follow-ups, allowing the clinical assessments and PROs to be linked. The assessments are scheduled to occur at initial registration, at randomization (i.e., 6 months after initial registration), and again 1, 2, and 3 years after randomization. Since the primary objectives are to test the difference in EPIC urinary function and bother scores by treatment arm, we set alpha to .025 to account for multiple comparisons. The target difference for urinary function scores is 5 points and for urinary bother scores is 6 points based on published MIDs [43]. Based on these parameters and 1000-patient total planned accrual for the clinical study, we achieve full power for comparing urinary function (97%) and bother (90%) scores by treatment arm. The 12-month urinary function and bother scores will be analyzed using multiple linear regression with stratification factors and baseline PRO scores as covariates. In addition, linear mixed models will examine changes in QOL over time. Finally, the S1802 statistical design will include analyses of dropout and missing data patterns to assess if data are missing at random, and will incorporate sensitivity analyses if data are systematically missing.
Table 2.
Application of PRO Design and Analysis Principles to SWOG Trial 1802
| Principle | Application to S1802 |
|---|---|
| Hypothesis-driven research questions |
|
| Validated instruments |
|
| Limited patient and site burden |
|
| Feasibility |
|
| Assessment design |
|
| Statistical design |
|
| Missing data strategies |
|
Conclusion
PROs that assess symptoms and QOL are critical to newly planned clinical trials. The value of PROs is recognized by the NCI through its support of QOL scientific committees, its promulgation of an electronic PRO platform, and its development of patient-reported toxicity ratings [35,44,45]. As even advanced cancer patients live longer, a patient-centered approach to evaluating investigational treatments with PROs has become increasingly important, to such an extent that a PRO extension for the CONSORT (Consolidated Standards of Reporting Trials) guidelines has been proposed to allow for a more comprehensive interpretation of PROs [46]. Adherence to key PRO design and analysis principles is therefore vital, in order to ensure valid interpretation of clinical trial findings, identify meaningful differences among investigational strategies, and better translate clinical trial results to diverse stakeholders.
Highlights.
Patient-reported outcomes (PROs) enable direct patient report of treatment experience
We outline key principles to guide successful use of PROs in clinical trials
These principles should be incorporated at both the design and analysis stages
Adherence to these principles is vital to ensure valid interpretation of findings
Acknowledgments
Funding/Support: Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under the following grant award numbers: 5U10CA180888-03, 5U10CA180819-03, and 5UG1CA189974.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: The authors have no disclosures to report.
References
- 1.Deshpande PR, Rajan S, Sudeepthi BL, Abdul Nazir CP. Patient-reported outcomes: A new era in clinical research. Perspect Clin Res. 2011 Oct;2(4):137–44. doi: 10.4103/2229-3485.86879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kypriotakis G, Vidrine DJ, Francis LE, Rose JH. The longitudinal relationship between quality of life and survival in advanced stage cancer. Psychooncology. 2016 Feb;25(2):225–31. doi: 10.1002/pon.3846. Epub 2015 May 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Day R, Ganz PA, Costantino JP, Cronin WM, Wickerham DL, Fisher B. Health-related quality of life and tamoxifen in breast cancer prevention: a report from the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Clin Oncol. 1999 Sep;17(9):2659–69. doi: 10.1200/JCO.1999.17.9.2659. [DOI] [PubMed] [Google Scholar]
- 4.Fallowfield L, Cella D, Cuzick J, Francis S, Locker G, Howell A. Quality of life of postmenopausal women in the Arimidex, Tamoxifen, Alone or in Combination (ATAC) Adjuvant Breast Cancer Trial. J Clin Oncol. 2004 Nov 1;22(21):4261–71. doi: 10.1200/JCO.2004.08.029. [DOI] [PubMed] [Google Scholar]
- 5.Gore JM, Brophy CJ, Greenstone MA. How well do we care for patients with end stage chronic obstructive pulmonary disease (COPD)? A comparison of palliative care and quality of life in COPD and lung cancer. Thorax. 2000 Dec;55(12):1000–6. doi: 10.1136/thorax.55.12.1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zimmermann C, Swami N, Krzyzanowska M, Hannon B, Leighl N, Oza A, Moore M, Rydall A, Rodin G, Tannock I, Donner A, Lo C. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet. 2014 May 17;383(9930):1721–30. doi: 10.1016/S0140-6736(13)62416-2. [DOI] [PubMed] [Google Scholar]
- 7.Phillips JL, Currow DC. Cancer as a chronic disease. Collegian. 2010;17(2):47–50. doi: 10.1016/j.colegn.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the "Silver Tsunami": Prevalence Trajectories and Comorbidity Burden among Older Cancer Survivors in the United States. Cancer Epidemiol Biomarkers Prev. 2016 Jul;25(7):1029–36. doi: 10.1158/1055-9965.EPI-16-0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Moor JS, Mariotto AB, Parry C, Alfano CM, Padgett L, Kent EE, Forsythe L, Scoppa S, Hachey M, Rowland JH. Cancer survivors in the United States: prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev. 2013 Apr;22(4):561–70. doi: 10.1158/1055-9965.EPI-12-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nussbaum N, George DJ, Abernethy AP, Dolan CM, Oestreicher N, Flanders S, et al. Patient experience in the treatment of metastatic castration-resistant prostate cancer: state of the science. Prostate Cancer Prostatic Dis. 2016;19(2):111–21. doi: 10.1038/pcan.2015.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, Lin X, Greenfield TK, Litwin MS, Saigal CS, Mahadevan A, Klein E, Kibel A, Pisters LL, Kuban D, Kaplan I, Wood D, Ciezki J, Shah N, Wei JT. Quality of Life and Satisfaction With Outcome Among Prostate Cancer Survivors. The New England Journal of Medicine. 2008;358:1250–1261. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- 12.Resnick MJ, Koyama T, Fan KH, Albertsen PC, Goodman M, Hamilton AS, Hoffman RM, Potosky AL, Stanford JL, Stroup AM, Van Horn L, Penson DF. Long-Term Functional Outcomes After Treatment For Localized Prostate Cancer. The New England Journal of Medicine. 2013;368:436–445. doi: 10.1056/NEJMoa1209978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Litwin MS, Lubeck DP, Henning JM, Carroll PR. Differences in Urologist and Patient Assessments of Health Related Quality of Life in Men With Prostate Cancer: Results of the CaPSURE Database. The Journal of Urology. 1998;159(6):1988–1992. doi: 10.1016/S0022-5347(01)63222-1. [DOI] [PubMed] [Google Scholar]
- 14.Donovan JL, Hamdy FC, Lane A, Mason M, Metcalfe C, Walsh W, et al. Patient-Reported Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. The New England Journal of Medicine. 2016;375:1425–1437. doi: 10.1056/NEJMoa1606221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen RC, Chang P, Vetter RJ, Lukka H, Stokes WA, Sanda MG, et al. Recommended Patient-Reported Core Set of Symptoms to Measure in Prostate Cancer Treatment Trials. J Natl Cancer Inst. 2014;106(7):1–7. doi: 10.1093/jnci/dju132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fitzpatrick JM, Bellmunt J, Fizazi K, Heidenreich A, Sternberg CN, Tombal B, et al. Optimal management of metastatic castration-resistant prostate cancer: Highlights from a European Expert consensus Panel. Eur J Cancer. 2014;50(9):1617–27. doi: 10.1016/j.ejca.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 17.Basch E, Reeve BB, Mitchell SA, Clauser SB, Minasian LM, Dueck AC, et al. Development of the National Cancer Institute's Patient-Reported Outcomes version of the Common Terminiology Criteria for Adverse Events (PRO-CTCAE) J Natl Cancer Inst. 2014;106(9) doi: 10.1093/jnci/dju244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Scher HI, Morris MJ, Stadler WM, Higano C, Basch E, Fizazi K, et al. Trial design and objectives for castration-resistant prostate cancer: Updated recommendations from the Prostate Cancer Clinical Trials Working Group 3. J Clin Oncol. 2016;34(12):1402–18. doi: 10.1200/JCO.2015.64.2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Penson DF, Litwin MS, Aaronson NK. Health Related Quality of Life in Men with Prostate Cancer. The Journal of Urology. 2003;169(5):1653–1661. doi: 10.1097/01.ju.0000061964.49961.55. [DOI] [PubMed] [Google Scholar]
- 20.Chodak G, Rooholloh S, Kasimis B, Block NL, Macramalla E, Kennealey GT. Single-Agent Therapy With Bicalutamide: A Comparison With Medical or Surgical Castration in the Treatment of Advanced Prostate Carcinoma. Urology. 1995;46:849–855. doi: 10.1016/S0090-4295(99)80356-2. [DOI] [PubMed] [Google Scholar]
- 21.Osoba D, Tannock IF, Ernst DS, Neville AJ. Health-Related Quality of Life in Men with Metastatic Prostate Cancer Treated With Prednisone Alone or Mitoxantrone and Prednisone. Journal of Clinical Oncology. 1999;17(6):1654–1663. doi: 10.1200/JCO.1999.17.6.1654. [DOI] [PubMed] [Google Scholar]
- 22.Petrylak DP, Tangen CM, Hussain MH, Lara PN, Jr, Jones JA, Taplin ME, Burch PA, Berry D, Moinpour C, Kohli M, Benson MC, Small EJ, Raghavan D, Crawford ED. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004 Oct 7;351(15):1513–20. doi: 10.1056/NEJMoa041318. [DOI] [PubMed] [Google Scholar]
- 23.Berry DL, Moinpour CM, Jiang CS, Ankerst DP, Petrylak DP, Vinson LV, Lara PN, Jones S, Taplin ME, Burch PA, Hussain MH, Crawford ED. Quality of Life and Pain in Advanced Stage Prostate Cancer: Results of a Southwest Oncology Group Randomized Trial Comparing Docetaxel and Estramustine to Mitoxantrone and Prednisone. Journal of Clinical Oncology. 2006;24(18):2828–2835. doi: 10.1200/JCO.2005.04.8207. [DOI] [PubMed] [Google Scholar]
- 24.Coyne KS, Tubaro A, Brubaker L, Bavendam T. Development and validation of patient-reported outcomes measures for overactive bladder: a review of concepts. Urology. 2006 Aug;68(2 Suppl):9–16. doi: 10.1016/j.urology.2006.05.042. [DOI] [PubMed] [Google Scholar]
- 25.Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, Erikson P, ISPOR Task Force for Translation and Cultural Adaptation Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005 Mar-Apr;8(2):94–104. doi: 10.1111/j.1524-4733.2005.04054.x. [DOI] [PubMed] [Google Scholar]
- 26.Vickers AJ. Multiple assessment in quality of life trials: how many questionnaires? How often should they be given? J Soc Integr Oncol. 2006 Summer;4(3):135–8. doi: 10.2310/7200.2006.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nelson EC, Eftimovska E, Lind C, Hager A, Wasson JH, Lindblad S. Patient reported outcome measures in practice. BMJ. 2015 Feb 10;350:g7818. doi: 10.1136/bmj.g7818. [DOI] [PubMed] [Google Scholar]
- 28.Recinos PF, Dunphy CJ, Thompson N, Schuschu J, Urchek JL, 3rd, Katzan IL. Patient Satisfaction with Collection of Patient-Reported Outcome Measures in Routine Care. Adv Ther. 2017 Feb;34(2):452–465. doi: 10.1007/s12325-016-0463-x. [DOI] [PubMed] [Google Scholar]
- 29.Basch E, Abernethy AP, Mullins CD, Reeve BB, Smith ML, Coons SJ, Sloan J, Wenzel K, Chauhan C, Eppard W, Frank ES, Lipscomb J, Raymond SA, Spencer M, Tunis S. Recommendations for incorporating patient-reported outcomes into clinical comparative effectiveness research in adult oncology. J Clin Oncol. 2012 Dec 1;30(34):4249–55. doi: 10.1200/JCO.2012.42.5967. [DOI] [PubMed] [Google Scholar]
- 30.Rolstad S, Adler J, Rydén A. Response burden and questionnaire length: is shorter better? A review and meta-analysis. Value Health. 2011 Dec;14(8):1101–8. doi: 10.1016/j.jval.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 31.Cohen J. A power primer. Psychol Bull. 1992 Jul;112(1):155–9. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 32.Sloan JA, Dueck A. Issues for statisticians in conducting analyses and translating results for quality of life end points in clinical trials. J Biopharm Stat. 2004;14:73–96. doi: 10.1081/BIP-120028507. [DOI] [PubMed] [Google Scholar]
- 33.Verbeke G. Linear Mixed Models in Practice. Vol. 126. Springer; New York, NY: 1997. Linear Mixed Models for Longitudinal Data. Lecture Notes in Statistics. [Google Scholar]
- 34.Mcculloch CE, Neuhaus JM. Generalized Linear Mixed Models . Encyclopedia of Environmetrics. 2003 [Google Scholar]
- 35.Basch E. The rise of patient-reported outcomes in oncology. ASCO Daily News. 2016 May 26; https://am.asco.org/daily-news/rise-patient-reported-outcomes-oncology.
- 36.Fairclough DL. Design and analysis of quality of life studies in clinical trials, Second Edition. 2. Boca Raton, FL: Chapman & Hall/CRC, Taylor & Francis Group, LLC; 2010. Chapman & Hall/CRC Interdisciplinary Statistics. [Google Scholar]
- 37.Rubin DB. Inference and missing data. Biometrika. 1976;63:581–592. [Google Scholar]
- 38.Little RJA. A Class of Pattern-Mixture Models for Normal Incomplete Data. Biometrika. 1994;81:471–483. [Google Scholar]
- 39.Little RJ, Wang Y. Pattern-mixture models for multivariate incomplete data with covariates. Biometrics. 1996 Mar;52(1):98–11. [PubMed] [Google Scholar]
- 40.Pauler DK, McCoy S, Moinpour C. Pattern mixture models for longitudinal quality of life studies in advanced stage disease. Statistics in Medicine. 2003;22:795–809. doi: 10.1002/sim.1397. [DOI] [PubMed] [Google Scholar]
- 41.Wei JT, et al. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56(6):899–905. doi: 10.1016/s0090-4295(00)00858-x. [DOI] [PubMed] [Google Scholar]
- 42.Martin NE, et al. Defining a standard set of patient-centered outcomes for men with localized prostate cancer. Eur Urol. 2015;67(3):460–7. doi: 10.1016/j.eururo.2014.08.075. [DOI] [PubMed] [Google Scholar]
- 43.Skolarus TA, et al. Minimally important difference for the Expanded Prostate Cancer Index Composite Short Form. Urology. 2015;85(1):101–5. doi: 10.1016/j.urology.2014.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Minasian LM, O'Mara AM, Reeve BB, Denicoff AM, Kelaghan J, Rowland JH, Trimble EL, National Cancer Institute Health-related quality of life and symptom management research sponsored by the National Cancer Institute. J Clin Oncol. 2007 Nov 10;25(32):5128–32. doi: 10.1200/JCO.2007.12.6672. [DOI] [PubMed] [Google Scholar]
- 45.Dueck AC, Mendoza TR, Mitchell SA, Reeve BB, Castro KM, Rogak LJ, Atkinson TM, Bennett AV, Denicoff AM, O'Mara AM, Li Y, Clauser SB, Bryant DM, Bearden JD, 3rd, Gillis TA, Harness JK, Siegel RD, Paul DB, Cleeland CS, Schrag D, Sloan JA, Abernethy AP, Bruner DW, Minasian LM, Basch E, National Cancer Institute PRO-CTCAE Study Group Validity and Reliability of the US National Cancer Institute's Patient-Reported Outcomes Version of the Common Terminology Criteria for Adverse Events (PRO-CTCAE) JAMA Oncol. 2015 Nov;1(8):1051–9. doi: 10.1001/jamaoncol.2015.2639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Calvert M, Blazeby J, Altman DG, Revicki DA, Moher D, Brundage MD, et al. Reporting of patient-reported outcomes in randomized clinical trials: The CONSORT PRO Extension. JAMA. 2013;309(8):814–22. doi: 10.1001/jama.2013.879. [DOI] [PubMed] [Google Scholar]