Abstract
Management of patients with orofacial pain may benefit from a better understanding about patient factors that may lead pain chronicity. In this study, we retrospectively compared physical and psychological factors in patients with acute and chronic orofacial pain. We analyzed data from 854 patients presenting to the Orofacial Pain Center, Department of Dental Anesthesiology, Tokyo Dental College, Suidobashi Hospital between April 2010 and March 2014. We categorized patients into the acute group if their condition had persisted <6 months and the chronic group if their condition had lasted 6 months or longer, based on the classification by the International Association for the Study of Pain. The retrospective data were analyzed by using univariate analysis on background factors from a health questionnaire, pain evaluation sheet, and psychological test completed at the time of presentation. Multiple logistic regression was applied on these factors. Our results suggest that female gender and high trait anxiety may be involved in orofacial pain becoming chronic.
Key Words: Chronic pain, Psychological distress, Myofascial pain, Neuropathic pain, Glossodynia
A number of studies have reported that pain is a risk factor for depression and/or anxiety.1–4 It is estimated that approximately 70% of patients with chronic pain have depression and/or anxiety.5–7 Various physical, psychological, and social factors are involved in chronic pain,8 increasing the complexity of the clinical condition. It has been reported that anxiety and depression have a negative impact on treatment for chronic pain.9 There are various chronic pain conditions occurring in the orofacial region, including neuropathic pain, myofascial pain/temporomandibular joint (TMJ) syndrome, and glossodynia.10,11 Correct diagnosis can be difficult due to the complex anatomy and neurophysiology of the orofacial complex, as well as numerous biopsychosocial factors.12,13
Although previous research into the psychological state of patients with chronic orofacial pain focused on particular diseases or compared chronic pain patients with healthy individuals,14–16 few studies in the dental field have compared the characteristics of patients with acute or chronic pain. Treatment of patients with orofacial pain may benefit from a better understanding regarding various elements of patients' backgrounds, which might lead to pain chronicity. We therefore retrospectively compared physical and psychological variables in patients with acute and chronic orofacial pain presenting to a hospital orofacial pain center.
METHODS
Subjects
Data from patients presenting with pain in the orofacial region visiting the Orofacial Pain Center, Department of Dental Anesthesiology, Tokyo Dental College Suidobashi Hospital between April 2010 and March 2014 were involved in this retrospective study. This study was approved by the Tokyo Dental College Ethics Committee (approval number 500). The requirement for written informed consent was waived by the Tokyo Dental College Ethics Committee because this study was performed by using epidemiological methodology.
Patient Classification and Evaluated Items
All data were extracted from patient records, including their health questionnaires. A total of 1155 patients presented with facial pain to the Orofacial Pain Center, Department of Dental Anesthesiology, Tokyo Dental College Suidobashi Hospital between April 2010 and March 2014. We excluded 301 patients from this study because of insufficient data in the health questionnaire, pain evaluation sheet, or psychological tests. The patients were divided into 2 groups: the acute pain group (pain had persisted <6 months) and the chronic pain group (pain had persisted ≥6 months) based on the International Association for the Study of Pain classification.17 We evaluated the following parameters: age, gender, visual analog scale to evaluate pain intensity, State-Trait Anxiety Inventory (STAI), and Hospital Anxiety and Depression Scale (HADS) to evaluate psychological factors, and the degree to which the pain obstructed activities of daily living. We analyzed the information recorded at their first visit for all parameters. We also investigated treatment history, such as whether medications were prescribed. One of 2 specialist dentists who were members of the Japanese Society of Orofacial Pain diagnosed the type of pain based on the American Academy of Orofacial Pain Guidelines18 after the medical examinations.
Evaluation of Psychological Factors
The STAI was first developed by Spielberger et al19 and we used the Japanese version. The STAI can simultaneously evaluate trait anxiety that shows personality tendencies that dispose an individual to anxiety (A-Trait) and state anxiety that shows the degree of anxiety at the time of evaluation (A-State). A higher point score shows stronger tendencies toward anxiety. The total minimum score of A-Trait and A-State was 20 and the maximum was 80, respectively.
HADS is a psychological test developed by Zigmond and Snaith20 for which we also used the Japanese version. The test evaluates the levels of anxiety and depression experienced while the patient is unwell. Patients with an evaluation of anxiety are described as HADS-A and with depression as HADS-D. The total minimum score of HADS-A and HADS-D was 0 and the maximum was 21, respectively.
The Japanese version of the psychological tests used in this study were validated in previous reports.21,22
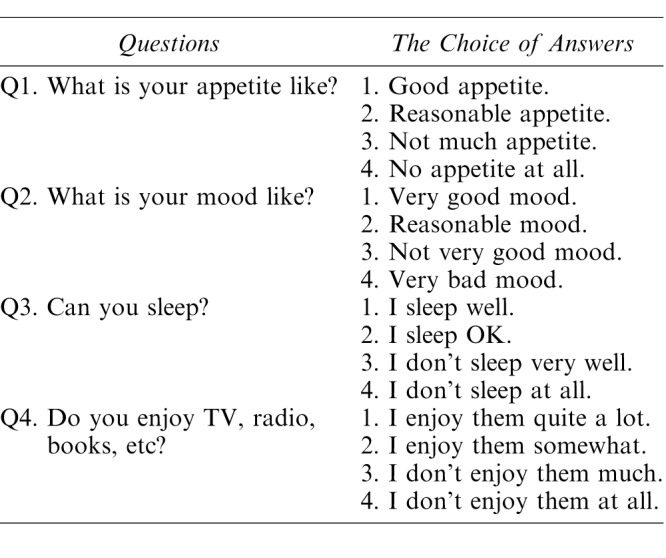
Evaluation of the Degree to Which the Pain Hindered Activities of Daily Living
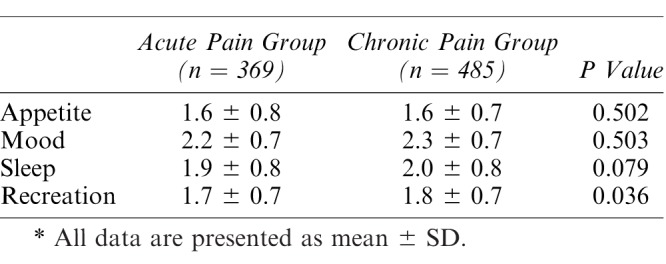
We investigated 4 activities of daily living that may be hindered by pain: appetite, mood, sleep, and recreation23 (Table 1). The questionnaire provided a 4-stage evaluation with a score of 1 to 4 points possible for each question. A higher score showed the patient was more hindered by pain.
Table 1.
The Questionnaire of Degree to Which the Pain Obstructed Activities of Daily Living
Statistical Analysis
To compare between the 2 groups (acute and chronic pain), we used Student's t test for patients' age, a chi-square test for gender, and the Mann-Whitney U test for visual analog scale, A-Trait, A-State, HADS-A, HADS-D, and appetite, mood, sleep, and recreation scores. To clarify the relationship between several factors and chronic orofacial pain, the factors returning p < 0.1 on univariate analysis were selected for further analysis by multiple logistic regression. A step-wise method was used to select the variables. The statistical analysis was performed using SPSS v. 19.0 and a p value less than 0.05 was considered statistically significant.
RESULTS
Patient Backgrounds
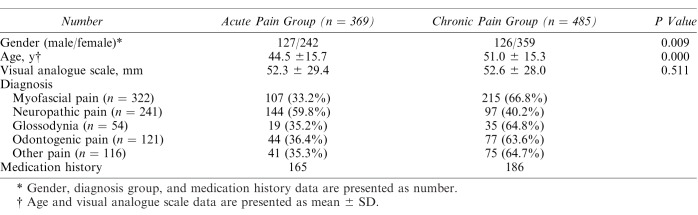
We analyzed 854 patient charts (253 males, 601 females) and divided the patient charts into 2 groups: the acute group (n = 369) and the chronic group (n = 485) (Figure 1). Analysis showed that the chronic pain group included more females and older patients (Table 2).
Figure 1.
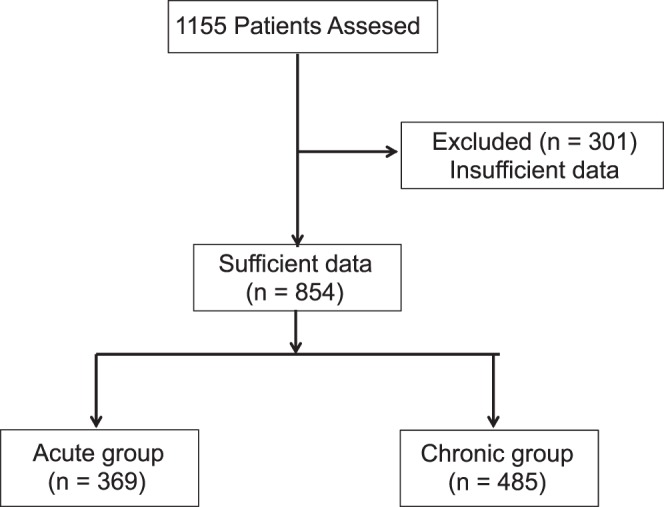
Patient selections for analysis. A total of 1155 patients presented with facial pain. We excluded 301 patients from the study because of insufficient data in the health questionnaire, pain evaluation sheet, or psychological tests. As a result, we analyzed 854 patients (253 males, 601 females) and divided the patients into the acute group (n = 369) and the chronic group (n = 485).
Table 2.
Patient Backgrounds
The diagnoses included myofascial pain/TMJ syndrome (n = 322, 37.7%), neuropathic pain (n = 241, 28.2%), glossodynia (n = 54, 6.3%), and odontogenic pain (n = 121, 14.1%), as well as psychogenic pain and other conditions classified as other pain (n = 116, 13.6%) (Table 2). One hundred sixty-five patients with acute pain and 186 patients with chronic pain received medication, such as analgesics, though details were not clear (Table 2).
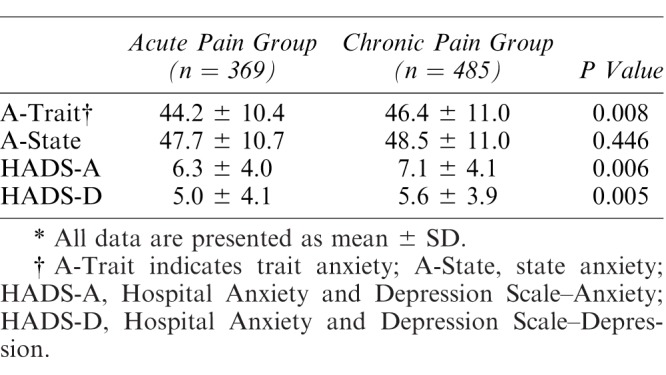
Psychological Factors
Table 3 shows the results of the psychological tests. The scores on A-Trait, HADS-A, and HADS-D were significantly higher in the chronic pain group.
Table 3.
Psychological Factors*
Degree of Obstruction of Activities of Daily Living
The score for recreation was significantly higher (more hindered by pain) in the chronic pain group (Table 4). There was a trend toward poorer sleep in the chronic pain group, which approached significance.
Table 4.
Degree of Disability of Daily Living*
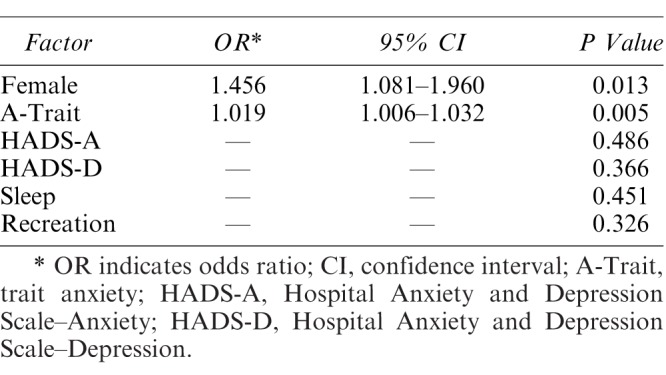
Factors Related to Chronic Orofacial Pain
Based on the results of univariate analysis, gender, A-Trait, HADS-A, HADS-D, sleep score, and recreation score were used as candidates for independent variables. Patient age was excluded from an independent variable because the age at which the disease occurred was not clear in this study. The results showed that female gender and A-Trait were associated with chronic orofacial pain (Table 5). The results from a model chi-square test were significant (p < 0.05), and the results of the Hosmer-Lemeshow test showed satisfactory goodness of fit at p = 0.678, with a discrimination rate of 56.4%.
Table 5.
Multiple Logistic Regression Analysis for Related Factors of Chronic Orofacial Pain
DISCUSSION
We categorized patients with orofacial pain as having acute pain or chronic pain and used multiple logistic regression to investigate whether the physical and/or psychological factors evaluated at the first visit were associated with chronic pain. The results showed that female gender and high trait anxiety were factors associated with chronic pain.
Chronic pain involves various physical, psychological, and social factors,8 increasing the complexity of the clinical condition. One study reported that from a socio-statistical perspective, chronic pain is more common in females.9 Other studies have reported that, compared with males, approximately double the number of females suffer from chronic orofacial pain.24,25 In our study, female patients were overrepresented with 3 times as many female versus male patients in the chronic pain group, which is consistent with previous research.
There are a number of possible factors that may explain the difference in pain between females and males. Two commonly cited factors include females being more sensitive to pain and reproductive hormones having an effect on pain perception. Fillingim and Maixner26 reported that females are more sensitive to pain than males when subjected to various stimuli (mechanical stimulus, pressure stimulus, electrical stimulus, or hot/cold stimulus). A meta-analysis by Riley et al27 showed that females had a lower pain threshold to noxious stimuli compared with males. However, numerous papers have suggested that changes in the balance of reproductive hormones may cause a greater sensitivity to pain, possibly related to the female-specific biological phenomenon of menstruation. One study reported that healthy females might have higher sensitivity to pain just before and after menstruation, because reproductive hormones increase sensitivity to pain in various circumstances.28 Other studies have reported similar increased sensitivity for headache and myofascial pain.29,30 After menopause, ovarian function declines and estrogen secretion decreases. One study reported that female patients with chronic orofacial pain receiving hormone replacement therapy have more severe symptoms than female patients not receiving hormone replacement therapy.31 These results suggest that endogenous and exogenous hormones may be associated with pain response in females.32
Our analysis also showed that high trait anxiety was another factor closely associated with chronic pain. Studies have shown that a highly anxious state can induce coronary artery disease, diabetes, or chronic pain.33,34 Trait anxiety reflects a general tendency toward anxiety related to one's environment and is thought to be an individual and permanent personality trait.18 Schuler et al35 divided patients with various diseases into acute and chronic pain groups and reported a significantly higher number of patients with high trait anxiety in the chronic pain group, with the results suggesting that depression and anxiety could be 1 factor involved in a clinical state transitioning pain from acute to chronic. One study reported that patients with chronic pain under highly anxiety provoking conditions tended to choose immature behavioral responses, while healthy people tended to choose more mature behavioral responses, when evaluated by using STAI, self-rating depression scale, and defense style questionnaires.36 There is clear evidence that a patient's psychological status may be associated with chronic pain.
Studies in patients with orofacial diseases have also shown that a significantly higher number of patients with chronic glossodynia also have high trait anxiety compared with healthy controls, although it is not clear if the chronic pain is the cause of anxiety or vice-versa.15,16 TMJ disorder, including myofascial pain, is a complex condition that involves dysfunction of the TMJ and masticatory muscles; this disorder has a tendency to become chronic.14 Reissmann et al14 analyzed trait anxiety in healthy individuals and TMJ disorder patients and reported that patients with high trait anxiety were more likely to suffer from TMJ disorder. Gamsa37 reported that the psychological factors preceding pain onset may play a role in the genesis and perpetuation of pain. Moreover, Mock et al38 suggests that psychological factors may also be related as initial factors of symptoms in “atypical facial pain.” Although the pathophysiological relationship between trait anxiety and chronic pain is not fully elucidated, our study seems to corroborate this relationship.
In this study, sleep and recreation were not factors associated with chronic pain. This may be because both acute and chronic pain could interfere with sleep and recreation similarly.
One limitation with our study is that we only researched the patient background at the first visit. More detailed research into the background associated with chronic pain might have been possible if we had also performed more extensive psychological tests, such as formal personality testing. The research methods used were cross-sectional and we only investigated the patients' state at the first visit. Accordingly, we were not able to evaluate the proportion of patients in the acute group that transitioned to chronic pain. Additionally, the differences in our psychological tests may not have been clinically significant. Puhan et al39 reported that the minimum clinically significant difference for HADS-A is 1.32 and for HADS-D it is 1.40. In our study, the difference between acute pain and chronic pain was 0.8 for HADS-A and 0.6 for HADS-D. These data were about half of those by Puhan et al.39 However, the patients of the Puhan et al39 study included only 88 Chronic Obstructive Pulmonary Disease patients, about one tenth the number of our cohort of 854 patients in this study. With a higher number of participants, our differences may have proved clinical relevant. Moreover, our study analyzed HADS for acute and chronic pain. Accordingly, it may be difficult to apply Puhan's results to this study. In addition, there are no such studies about trait anxiety. Thus, further studies will be needed to determine the clinical significance of the results of this study. Additionally, we did not perform an analysis based on various diagnoses, including distinguishing between intra-articular versus muscular facial pain, and their tendency toward chronicity.
There is a need to determine whether the results from this study are applicable in the dental field to a wide range of patients with chronic pain, by investigating the relationship between patient background and the transition to chronic pain through prospective follow-up of the psychological state of patients with acute pain. Confirmation of high trait anxiety and female gender might be 1 method to predict the prognosis for chronic pain patients in the dental field. It may be useful to take patient backgrounds into account and to take steps to reduce anxiety and provide concomitant mental-health or psychological treatment in order to prevent pain from becoming chronic.
In conclusion, we used multiple logistic regression to investigate factors associated with chronic pain in 854 patients presenting to a hospital-based orofacial pain clinic. The results showed that female gender and high trait anxiety were closely associated with chronic pain. If these factors are present in acute orofacial pain patients, patient management might be improved by taking into account the possibility of such pain becoming chronic.
Acknowledgments
The authors report no conflicts of interest in this work.
REFERENCES
- 1.Asmundson GJG, Katz J. Understanding the co-occurrence of anxiety disorders and chronic pain: state-of-the-art. Depress Anxiety. 2009;26:888–901. doi: 10.1002/da.20600. [DOI] [PubMed] [Google Scholar]
- 2.Fishbain DA, Cutler R, Rosomoff HL, Rosomoff RS. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clin J Pain. 1997;13:116–137. doi: 10.1097/00002508-199706000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Gerrits MMJG, van Oppen P, van Marwijk HWJ, et al. Pain and the onset of depressive and anxiety disorders. Pain. 2014;155:53–59. doi: 10.1016/j.pain.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 4.Hilderink PH, Burger H, Deeg DJ, et al. The temporal relation between pain and depression: results from the longitudinal aging study Amsterdam. Psychosom Med. 2012;74:945–951. doi: 10.1097/PSY.0b013e3182733fdd. [DOI] [PubMed] [Google Scholar]
- 5.Demyttenaere K, Bruffaerts R, Lee S, et al. Mental disorders among persons with chronic back or neck pain: results from the World Mental Health Surveys. Pain. 2007;129:332–342. doi: 10.1016/j.pain.2007.01.022. [DOI] [PubMed] [Google Scholar]
- 6.Gureje O, Von Korff M, Kola L, et al. The relation between multiple pains and mental disorders: results from the World Mental Health Surveys. Pain. 2008;135:82–91. doi: 10.1016/j.pain.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 7.De Heer EW, Gerrits MMJG, Beekman ATF, et al. The association of depression and anxiety with pain: a study from NESDA. PloS One. 2014;9:e106907. doi: 10.1371/journal.pone.0106907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maia Costa Cabral D, Sawaya Botelho Bracher E, Dylese Prescatan Depintor J, et al. Chronic pain prevalence and associated factors in a segment of the population of São Paulo City. J Pain Off J Am Pain Soc. 2014;15:1081–1091. doi: 10.1016/j.jpain.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 9.Van Hecke O, Torrance N, Smith BH. Chronic pain epidemiology and its clinical relevance. Br J Anaesth. 2013;111:13–18. doi: 10.1093/bja/aet123. [DOI] [PubMed] [Google Scholar]
- 10.L Mehalick M. Assessment of the psychological comorbidity, pathophysiological mechanisms, and treatment implications in patients with chronic orofacial pain. Anaplastology. 2013 doi: 10.4172/2161-1173.S2-001. 02. [DOI]
- 11.Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. 2008;359:2693–2705. doi: 10.1056/NEJMra0802472. [DOI] [PubMed] [Google Scholar]
- 12.Ganzberg S. Pain management part II: pharmacologic management of chronic orofacial pain. Anesth Prog. 2010;57:114–118. doi: 10.2344/0003-3006-57.3.114. quiz 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sessle BJ. Why are the diagnosis and management of orofacial pain so challenging? J Can. Dent Assoc. 2009;75:275–277. [PubMed] [Google Scholar]
- 14.Reissmann DR, John MT, Seedorf H, et al. Temporomandibular disorder pain is related to the general disposition to be anxious. J Oral Facial Pain Headache. 2014;28:322–330. doi: 10.11607/ofph.1277. [DOI] [PubMed] [Google Scholar]
- 15.Schiavone V, Adamo D, Ventrella G, et al. Anxiety, depression, and pain in burning mouth syndrome: first chicken or egg? Headache. 2012;52:1019–1025. doi: 10.1111/j.1526-4610.2012.02171.x. [DOI] [PubMed] [Google Scholar]
- 16.De Souza FTA, Teixeira AL, Amaral TMP, et al. Psychiatric disorders in burning mouth syndrome. J Psychosom Res. 2012;72:142–146. doi: 10.1016/j.jpsychores.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 17.Bogduk N, Merskey H. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. Seattle, WA: IASP Press;; 1994. [Google Scholar]
- 18.de Leeuw R, editor. American Academy of Orofacial Pain. Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management 4th ed. Chicago, IL: Quintessence Publishing;; 2008. pp. 101–113. [Google Scholar]
- 19.Spielberger CD, Gorsuch RL, Lushene RE. Manual for the state-trait anxiety inventory. 1970 Available at: http://ubir.buffalo.edu/xmlui/handle/10477/2895 Accessed November 27, 2014.
- 20.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 21.Himeno C, Nakagawa H, Hamada S, et al. An investigation of state-trait anxiety inventory (STAI) in dizzy patients [in Japanese] Equilibrium Res. 2005;64:225–232. [Google Scholar]
- 22.Hatta H, Higashi A, Yashiro H, et al. A validation of the Hospital Anxiety and Depression Scale [in Japanese] Jpn J Psychosom Med. 1998;38:309–315. [Google Scholar]
- 23.Matsubayashi K, Kimura S, Iwasaki T, et al. Evaluation of subjective happiness in the elderly using a visual analogue scale of happiness to analyze the effect of life style and neurobehavioral function on subjective happiness [in Japanese] Jpn J Geriat. 1992;29:817–822. doi: 10.3143/geriatrics.29.817. [DOI] [PubMed] [Google Scholar]
- 24.Dao TT, LeResche L. Gender differences in pain. J Orofac Pain. 2000;14:169–184. discussion 184–195. [PubMed] [Google Scholar]
- 25.Fillingim RB. Sex, gender, and pain: women and men really are different. Curr Rev Pain. 2000;4:24–30. doi: 10.1007/s11916-000-0006-6. [DOI] [PubMed] [Google Scholar]
- 26.Fillingim RB, Maixner W. Gender differences in the responses to noxious stimuli. Pain Forum. 1995;4:209–221. [Google Scholar]
- 27.Riley JL, Robinson ME, Wise EA, et al. Sex differences in the perception of noxious experimental stimuli: a meta-analysis. Pain. 1998;74:181–187. doi: 10.1016/s0304-3959(97)00199-1. [DOI] [PubMed] [Google Scholar]
- 28.Fillingim RB, Ness TJ. Sex-related hormonal influences on pain and analgesic responses. Neurosci Biobehav Rev. 2000;24:485–501. doi: 10.1016/s0149-7634(00)00017-8. [DOI] [PubMed] [Google Scholar]
- 29.Dao TT, Knight K, Ton-That V. Modulation of myofascial pain by the reproductive hormones: a preliminary report. J Prosthet Dent. 1998;79:663–670. doi: 10.1016/s0022-3913(98)70073-3. [DOI] [PubMed] [Google Scholar]
- 30.Marcus DA. Interrelationships of neurochemicals, estrogen, and recurring headache. Pain. 1995;62:129–139. doi: 10.1016/0304-3959(95)00052-T. [DOI] [PubMed] [Google Scholar]
- 31.Wise EA, Riley JL, Robinson ME. Clinical pain perception and hormone replacement therapy in postmenopausal women experiencing orofacial pain. Clin J Pain. 2000;16:121–126. doi: 10.1097/00002508-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Stavropoulos F, Hastie BA. Chronic facial pain in the female patient: treatment updates. Oral Maxillofac Surg Clin N Am. 2007;19:245–258. doi: 10.1016/j.coms.2007.01.010. vii. [DOI] [PubMed] [Google Scholar]
- 33.Hemingway H, Marmot M. Evidence based cardiology: psychosocial factors in the aetiology and prognosis of coronary heart disease. Systematic review of prospective cohort studies. BMJ. 1999;318:1460–1467. doi: 10.1136/bmj.318.7196.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li C, Barker L, Ford ES, et al. Diabetes and anxiety in US adults: findings from the 2006 Behavioral Risk Factor Surveillance System. Diabet Med J Br Diabet Assoc. 2008;25:878–881. doi: 10.1111/j.1464-5491.2008.02477.x. [DOI] [PubMed] [Google Scholar]
- 35.Schuler M, Njoo N, Hestermann M, et al. Acute and chronic pain in geriatrics: clinical characteristics of pain and the influence of cognition. Pain Med Malden Mass. 2004;5:253–262. doi: 10.1111/j.1526-4637.2004.04040.x. [DOI] [PubMed] [Google Scholar]
- 36.Hara S, Kubo C. The association between anxiety or depression and defense styles on the patients with chronic pain [in Japanese] Psychosomatic Medicine. 2002;6:161–167. [Google Scholar]
- 37.Gamsa A. Is emotional disturbance a precipitator or a consequence of chronic pain? Pain. 1990;42:183–195. doi: 10.1016/0304-3959(90)91161-B. [DOI] [PubMed] [Google Scholar]
- 38.Mock D, Frydman W, Gordon AS. Atypical facial pain: a retrospective study. Oral Surg Oral Med Oral Pathol. 1985;59:472–474. doi: 10.1016/0030-4220(85)90086-6. [DOI] [PubMed] [Google Scholar]
- 39.Puhan MA, Frey M, Büchi S, et al. The minimal important difference of the Hospital Anxiety and Depression Scale in patients with chronic obstructive pulmonary disease. Health Qual Life Outcomes. 2008;6:46. doi: 10.1186/1477-7525-6-46. [DOI] [PMC free article] [PubMed] [Google Scholar]