Abstract
Background:
Various medications are cleared by the kidney, therefore patients with impaired renal function, especially dialysis patients are at risk for adverse drug events (ADEs). There are limited studies on ADEs in maintenance dialysis patients.
Methods:
We utilized a nationally representative database, the Nationwide Emergency Department Sample, from 2008 to 2013 to compare emergency department (ED) visits for dialysis and propensity matched non-dialysis patients. Log binomial regression was used to calculate relative risk of hospital admission and logistic regression to calculate odds ratios for in-hospital mortality while adjusting for patient and hospital characteristics.
Results:
While ED visits for ADEs decreased in both groups, they were over 10-fold higher in dialysis patients than non-dialysis patients (65.8–88.5/1000 patients vs. 4.6 to 5.4 /1000 patients respectively, p<0.001). The top medication category associated with ED visits for ADEs in dialysis patients is agents primarily affecting blood constituents, which has increased. After propensity matching, patient admission was higher in dialysis patients than non-dialysis patients, (88% vs 76%, p<0.001). Dialysis was associated with a 3 percent increase in risk of admission and three times the odds of in-hospital mortality (aOR 3, 95% CI 2.7 – 2.3.3).
Conclusions:
ED visits for ADEs are substantially higher in dialysis patients than non-dialysis patients. In dialysis patients, ADEs associated with agents primarily affecting blood constituents are on the rise. ED visits for ADEs in dialysis patients have higher inpatient admissions and in-hospital mortality. Further studies are needed to identify and implement measures aimed at reducing ADEs in dialysis patients.
Keywords: Adverse drug events, dialysis, emergency department
Introduction:
Many medications such as antibiotics, blood thinners, and pain medications are cleared by the kidneys; which places patients with impaired renal function at risk for adverse drug events (ADEs).[1] Patients on dialysis are at especially high risk of developing ADEs due to variable medication clearance, high comorbidity burden, and high pill burden.[1] Prior small, single center studies have evaluated the complications associated with polypharmacy in dialysis patients but have not evaluated the added burden associated with emergency room visits for ADE and its consequences in dialysis patients. [1,2] While studies have looked at reasons for emergency visits and hospitalizations after inpatient admissions in dialysis patients, little is known on the epidemiology, trends, risk factors, and outcomes of dialysis patients presenting to emergency departments (ED) with ADE.
Utilizing a nationally representative all-payer database, the Nationwide Emergency Department Sample (NEDS), we compared ED visits for ADES between dialysis and non-dialysis patients. We hypothesized that dialysis patients will have more ED visits for ADEs then propensity matched non-dialysis patients, and that rates of hospitalization and mortality will be higher in dialysis patients.
Materials and Methods:
Data sources and study population:
We utilized the NEDS to identify outpatient dialysis patients who presented to the ED with an ADE. The NEDS is part of a group of databases developed for the Healthcare Cost and Utilization Project (HCUP).[3] The NEDS contains discharge data for ED visits from 945 hospitals located in 33 states and the District of Columbia which approximates a 20-percent stratified sample of the U.S. hospital-based ED. The database contains a weight variable which allows for the generation of national estimates. As the NEDS is a publically available, de-identified database the study was considered to be institutional review board exempt.
We excluded patients who had acute short term dialysis, pregnancy, and those with a renal transplant. A study flow diagram is included as Supplemental figure 1. We obtained estimates of prevalent dialysis patients for a specific year from the United States Renal Data System[4].We calculated non-dialysis patients as general population from the United States Census Bureau minus the number of prevalent dialysis patients.[5]
We used the propensity scoring method to reduce bias due to confounding covariates between dialysis and non-dialysis patients. Analyses done prior to propensity matching are presented as weighted numbers, while analyses done after propensity matching are presented as raw unweighted numbers. A propensity score for dialysis was assigned to each ED visit which was computed by a multivariate logistic regression model that included age, gender, and comorbidities of congestive heart failure (CHF), diabetes mellitus (DM), liver disease, AIDS, hypertension (HTN), chronic lung disease, and peripheral vascular disease. Patients with similar propensity scores in the dialysis and non-dialysis groups were matched using a one-to-one scheme without replacement using the greedy algorithm. We chose to do propensity matching instead of comparing with CKD patients as ICD codes for CKD alone not on dialysis has poor sensitivity.[6]
Definition of variables
ADEs were identified utilizing International Classification of Diseases-9 codes (ICD-9-CM) with the exclusion of recreational drugs such as heroin and cocaine. For a full list of codes, please refer to Supplemental table 1. Dialysis patients were identified if they had codes for ESRD (585.6), hemodialysis (39.95, V45.x, V56.0, V56.1) without a concurrent code for AKI, and peritoneal dialysis (54.98, 996.68, V56.2, V56.8, V56.32).
We identified patient comorbidities using the HCUP tool, the Elixhauser Comorbidity Software which identifies comorbidities in hospital discharge records using ICD-9-CM codes.[7] We grouped medications categories using ICD-9-CM codes as per Supplemental table 2.
Analytic approach
Raw rates were calculated as ED visits in dialysis patients divided by number of prevalent dialysis patients for that year and rates in non-dialysis patients as ED visits for ADEs in non-dialysis patients divided by all non-dialysis patients as per above. We assessed trends of ED visits for ADEs over time between dialysis and non-dialysis patients and also in a priori defined subgroups of age, gender, and dialysis modality. As incidence rates are confounded by differences between dialysis and non-dialysis patients, we did direct adjustment or standardization which stratifies within each group and calculates a weighted average of the stratum specific rate, where weights are the numbers of persons in each stratum from the USRDS for dialysis patients and from the U.S. Census for non-dialysis patients. This method only allows for adjustment to a small number of demographic variables (age and gender); however it is the method done by the USRDS.[8] We defined severity of comorbid conditions using Deyo’s Charlson Comorbidity Index (CCI) for each admission.[9] Renal failure was excluded from the calculation as dialysis status was included as a covariate in the model. We then used log binomial regression to calculate relative risk of hospital admission while adjusting for valvular heart disease, alcohol abuse, drug abuse, depression, CCI, primary payer, income quartile by zip, hospital teaching status, and hospital urban/rural designation. Log binomial regression was used instead of logistic regression as odds ratio estimates diverge from relative risk estimates when the risk of the event (hospital admission) is high as in this case. We used logistic regression to calculate odds ratios for in-hospital mortality while adjusting for the variables listed above.)..[10] All analyses were conducted using SAS 9.4 (SAS Institute, Cary NC, USA).
Results:
Unmatched analysis:
Patient characteristics of patients who presented to the ED for ADEs are presented in Table 1. Dialysis patients were older (mean age 63.3±0.1 vs. 57.8±0.01years, p<0.001); with higher prevalence of CHF(23.89 vs. 7.6%, p<0.001), HTN (83.4 vs. 42.8%, p<0.001) and DM (47.9 vs. 19.6%, p<0.001). ED visits for ADEs increased with increasing number of comorbidities in dialysis patients, but plateaued after 4 comorbidities. (Supplemental Figure 2)
Table 1:
Characteristics of patients presenting to the emergency department for adverse drug events.
| Dialysis (197,650) |
Non-dialysis (9,474,763) |
P | |
|---|---|---|---|
| Age (Mean ± SE) | 63.3 ± 0.1 | 57.8 ± 0.01 | <0.001 |
| Female | 101,823 (51.5) | 5,779,778 (61) | <0.001 |
| Comorbidities | |||
| CHF | 47,030 (23.8) | 719,356 (7.6) | <0.001 |
| Valvular disease | 11,076 (5.6) | 316,171 (3.3) | <0.001 |
| Peripheral vascular disease |
24,126 (12.2) | 326,667 (3.5) | <0.001 |
| Hypertension | 164,812 (83.4) | 4,055,164(42.8) | <0.001 |
| Chronic pulmonary disease |
36,537 (18.5) | 1,610,845(17) | <0.001 |
| Diabetes mellitus | 94,649(47.9) | 1,859,001 (19.6) | <0.001 |
| Liver disease | 8,219(4.2) | 190,811 (2) | <0.001 |
| AIDS | 1,945 (1) | 21,329 (0.2) | <0.001 |
| Alcohol abuse | 2,395 (1.2) | 308,548 (3.3) | <0.001 |
| Drug abuse | 5,503(2.8) | 423,496 (4.5) | <0.001 |
| Depression | 14395 (7.3) | 946747 (10) | <0.001 |
| CCI | <0.001 | ||
| 0 | 43252 (21.9) | 4733959 (50) | |
| 1 | 53555 (27.1) | 2298943 (24.3) | |
| 2 | 100842 (51) | 2441861 (25.8) | |
|
Inpatient LOS (Median IQR) |
4.2 (2.1 – 8) | 3.13 (1.6 – 5.7) | <0.001 |
| Primary Payer | <0.001 | ||
| Medicare | 156832 (79.4) | 4492740 (47.4) | |
| Medicaid | 17857 (9) | 1270448 (13.4) | |
| Private Insurance | 18922 (9.6) | 2545951 (26.9) | |
| Other | 3878 (2) | 1149026 (12.1) | |
| Missing | 161 (0.1) | 16599 (0.2) | |
|
Inpatient Discharge Disposition (% of those admitted)a |
<0.001 | ||
| Routine/Home health care |
115,842 (66.9) | 4166730 (76.3) | |
| Transfer to short- term hospital |
3528(2) | 105449 (1.9) | |
| Transfer to SNF, ICF, another type of facility |
44039 (25.4) | 1026556 (18.8) | |
| AMA | 2166 (1.3) | 64835 (1.2) | |
| Died in hospital | 7446 (4.3) | 915174 (1.7) | |
| Missing | 228 (0.1) | 6829 (0.1) | |
|
Income Quartile by Zip Codeb |
<0.001 | ||
| 1 | 63394 (32.1) | 2630288 (27.8) | |
| 2 | 50485 (25.5) | 2528477 (26.7) | |
| 3 | 43932 (22.2) | 2195790 (23.2) | |
| 4 | 35473 (18) | 1901992 (20.1) | |
| Missing | 4367 (2.2) | 218217 (2.3) | |
|
Hospital Teaching Statusc |
<0.001 | ||
| Metropolitan non- Teaching |
84,487 (42.8) | 4278393 (45.2) | |
| Metropolitan teaching |
95,291 (48.2) | 3600750 (38) | |
| Non-metropolitan hospital |
17,872 (9) | 1595620 (16.8) | |
|
Urban-Rural Designationd |
<0.001 | ||
| Large metropolitan areas with at least 1 million residents |
110,735 (56) |
4436647 (46.8) | |
| Small metropolitan areas with less than 1 million residents |
51,944 (26.3) |
2710911 (28.6) | |
| Micropolitan areas | 12,703 (6.4) | 1016375 (10.7) | |
| Not metropolitan or micropolitan (non- urban residual) |
2,377 (1.2) | 454413 (4.8) | |
| Other | 19,891 (10.1) | 856418 (9) |
All values are n (%) except where indicated. CHF, congestive heart failure; AIDS, acquired immunodeficiency syndrome; CCI, Charlson comorbidity index; LOS, length of stay; SNF, skilled nursing facility; ICF, intermediate care facility
Percentages were calculated with the number of patients who were admitted as the denominator
This represents a quartile classification of the estimated median household income of residents in the patient’s ZIP Code. These values are derived from ZIP Code-demographic data obtained from Claritas. The quartiles are identified by values of 1 to 4, indicating the poorest to wealthiest populations.
The hospital’s teaching status was obtained from the AHA Annual Survey of Hospitals. A hospital is considered to be a teaching hospital if it has an AMA-approved residency program, is a member of the Council of Teaching Hospitals (COTH) or has a ratio of full-time equivalent interns and residents to beds of .25 or higher.
Urban-rural designation of the hospital and is based on the county of the hospital, as identified by the American Hospital Association.
Between 2008 and 2013, the incidence of ED visits for ADEs decreased in both the dialysis and the non-dialysis population but remained over ten-fold higher in dialysis patients than non-dialysis patients (84.3/1000 dialysis patients in 2008 to 73.1/1000 dialysis patients in 2013 vs. 5.4/1000 non-dialysis patients in 2013 to 4.6/1000 non-dialysis patients in 2013, p<0.001). While there was a larger absolute decrease in ED visits for ADE in dialysis patients (11.2/1000 patients vs 0.8/1000 patients), there was a larger percent change in the non-dialysis patients (15% vs. 13%). There were 190,203 HD patients, while there were only 7,447 PD patients. Hemodialysis patients had a two-fold higher incidence of ED visits for ADEs than peritoneal dialysis patients (69.2 – 92.7/1000 patients vs. 30.6 – 40.4/1000 patients, p<0.001). ED visits for ADEs in dialysis patients were more common in HD patients, females, and in age ≥65 years. (Figure 1) When adjusted for age and gender, rates of ER visits for dialysis patients were 6 times higher than in non-dialysis patients. (Supplemental Figure 3)
Figure 1:
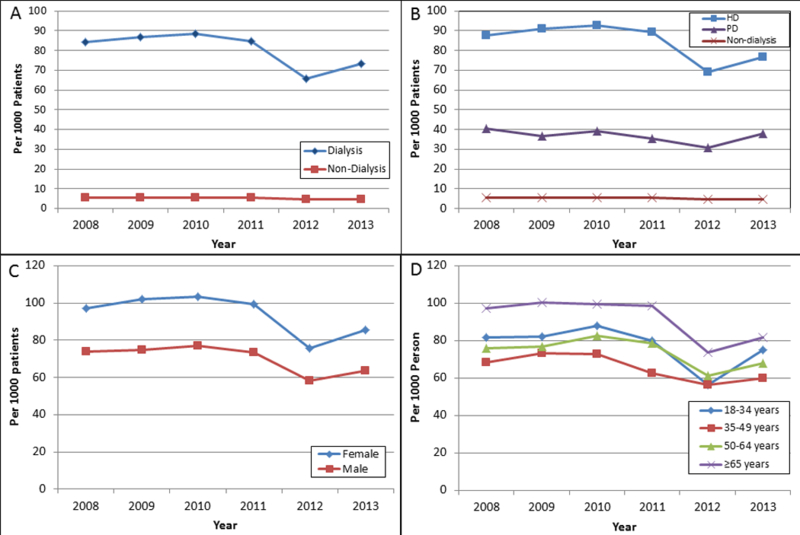
Trends of adverse drug events between (A) dialysis and non-dialysis; (B) hemodialysis (HD), peritoneal dialysis (PD), non-dialysis; (C) female vs male; (D) age groups.
Of the top 10 medications categories leading to ED visits for ADEs, agents primarily affecting blood constituents was the top category and accounted for 20% of all ED visits for ADEs in the dialysis population. (Figure 2a) 94% of medications in this category were anticoagulants. On analysis of trends by medication category, agents primarily affecting blood constituents increased sharply from 2012 to 2013, while all other categories were stable or decreased over time. (Figure 2b) Within this category, oral anticoagulants was the main driver of this increase, with an absolute increase from 5430 in 2012 to 7377 in 2013, a 36% increase in ED visits for ADE due to oral anticoagulants. This accounts for 44% of the difference between all ED visits for ADE in dialysis patients between 2012 and 2013.
Figure 2:
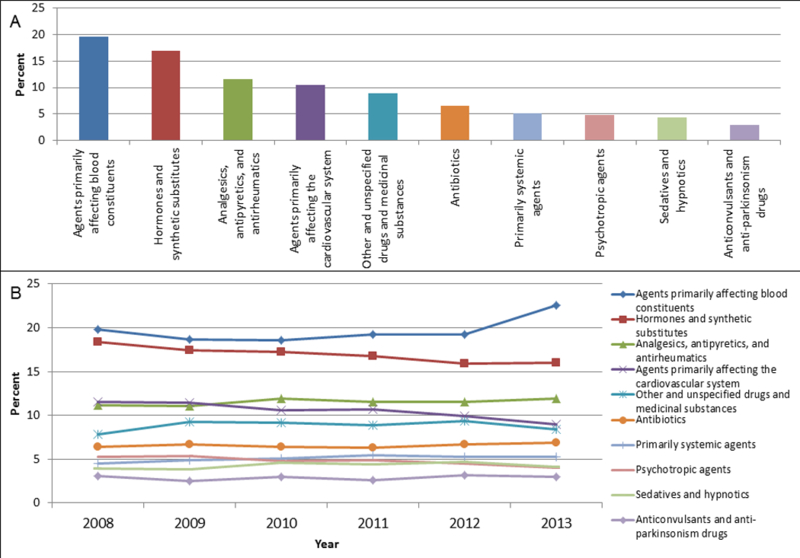
(A) Top 10 medication categories associated with emergency department visits for adverse drug events. (B) Trends of top 10 medication categories associated with emergency visits for adverse drug events.
173,250 (88%) ED visits in dialysis patients resulted in a hospital admission while 5,461,916 (58%) ED visits for ADEs in non-dialysis patients resulted in a hospital admission. Once admitted to the hospital, dialysis patients had longer length of stay (LOS) (4.2 vs 3.1 days, p<0.001) and were more likely to be discharged to a skilled nursing facility (SNF) or intermediate care facility (ICF) (25.4% vs 18.8%, p<0.001). Of those who were admitted to the hospital, 7,446 (4%) dialysis patients died in the hospital while only 91,517(1%) died in the non-dialysis group.
Propensity Matched Analysis:
After propensity matching, there was no significant difference between dialysis and non-dialysis patients on age, gender, or comorbidities of CHF, PVD, HTN, liver disease (Table 2), AIDS. However, dialysis patients had significant higher prevalence of comorbidities of valvular disease (5.6% vs 5.2%, P=0.005), and lower prevalence of comorbidities such as alcohol abuse (1.2% vs. 3.7%, p <0.001), drug abuse (2.8% vs 4%, p<0.001), and depression (7.3% vs. 11.6%, p<0.001). Additionally, more dialysis patients had a CCI score of 2 compared to non-dialysis patients, 50.9% vs 47.4%, p<0.001.
Table 2:
Characteristics of patients after propensity matching
| Dialysis (44,392) |
Non-dialysis Propensity Matched (44,392) |
P | |
|---|---|---|---|
| Age (Mean ± SE) | 63.4 (15) | 63.5 (14.9) | 0.11 |
| Female | 22775 (51.3) | 22783 (51.3) | 0.96 |
| Comorbidities | |||
| CHF | 10479 (23.6) | 10454 (23.55) | 0.84 |
| Valvular disease | 2490 (5.6) | 2302 (5.2) | 0.005 |
| Peripheral vascular disease |
5471 (12.32) | 5465 (12.31) | 0.95 |
| Hypertension | 37030 (83.42) | 37042 (83.44) | 0.91 |
| Chronic pulmonary disease |
8235 (18.55) | 8311 (18.72) | 0.51 |
| Diabetes mellitus | 10396 (23.42) | 10419 (23.47) | 0.86 |
| Liver disease | 1838 (4.14) | 1865 (4.2) | 0.65 |
| AIDS | 426 (1.0) | 384 (0.9) | 0.14 |
| Alcohol abuse | 519 (1.2) | 1637 (3.7) | <.0001 |
| Drug abuse | 1223 (2.8) | 1774 (4) | <.0001 |
| Depression | 3235 (7.3) | 5149 (11.6) | <.0001 |
| CCI | <.0001 | ||
| 0 | 9779 (22.0) | 11532 (26.0) | |
| 1 | 12019 (27.1) | 11826 (26.7) | |
| 2 | 22594 (50.9) | 21034 (47.4) | |
|
Inpatient LOS
(Median IQR) |
5 (3,8) | 4 (2,6) | <.0001 |
| Primary Payer | <.0001 | ||
| Medicare | 35288 (79.5) | 26574 (59.9) | |
| Medicaid | 4004 (9.0) | 5179 (11.7) | |
| Private Insurance | 4189 (9.4) | 9247 (20.9) | |
| Other | 877 (2.0) | 3336 (7.5) | |
| Missing | 34 (0.1) | 56 (0.1) | |
|
Inpatient
Discharge Disposition (% of those admitted)a |
<0.0001 | ||
| Routine/Home health care |
26015 (66.8) | 26072 (77.2) | |
| Transfer to short- term hospital |
777(2) | 629 (1.9) | |
| Transfer to SNF, ICF, another type of facility |
9907 (25.4) | 6189(18.3) | |
| AMA | 507 (1.3) | 381 (1.1) | |
| Died in hospital | 1682 (4.3) | 459 (1.4) | |
| Missing | 52 (0.1) | 36 (0.1) | |
|
Income Quartile by
Zip Codeb |
<.0001 | ||
| 1 | 14102 (31.8) | 13032 (29.4) | |
| 2 | 11393 (25.7) | 11708 (26.4) | |
| 3 | 9965 (22.45) | 10130 (22.9) | |
| 4 | 7982 (18.0) | 8440 (19.0) | |
| Missing | 950 (2.1) | 1082 (2.4) | |
|
Hospital Teaching
Statusc |
<.0001 | ||
| Metropolitan non- teaching |
20443 (46.1) | 21125 (47.6) | |
| Metropolitan teaching |
20276 (45.7) | 17332 (39.0) | |
| Non-metropolitan hospital |
3673 (8.3) | 5935 (13.4) | |
|
Urban-Rural
Designationd |
<.0001 | ||
| Large metropolitan areas with at least 1 million residents |
25583 (57.6) | 22705 (51.2) | |
| Small metropolitan areas with less than 1 million residents |
11844 (26.7) | 12805 (28.9) | |
| Micropolitan areas | 2904 (6.5) | 4169 (9.4) | |
| Not metropolitan or micropolitan (non- urban residual) |
539 (1.2) | 1587 (3.6) | |
| Other | 3522 (7.9) | 3126 (7.0) |
All values are n (%) except where indicated. CHF, congestive heart failure; AIDS, acquired immunodeficiency syndrome; CCI, Charlson comorbidity index; LOS, length of stay; SNF, skilled nursing facility; ICF, intermediate care facility
Percentages were calculated with the number of patients who were admitted as the denominator
This represents a quartile classification of the estimated median household income of residents in the patient’s ZIP Code. These values are derived from ZIP Code-demographic data obtained from Claritas. The quartiles are identified by values of 1 to 4, indicating the poorest to wealthiest populations.
The hospital’s teaching status was obtained from the AHA Annual Survey of Hospitals. A hospital is considered to be a teaching hospital if it has an AMA-approved residency program, is a member of the Council of Teaching Hospitals (COTH) or has a ratio of full-time equivalent interns and residents to beds of .25 or higher.
Urban-rural designation of the hospital and is based on the county of the hospital, as identified by the American Hospital Association.
In the propensity matched group, dialysis patients had higher rates of hospital admission than matched non-dialysis patients (88% vs. 76%, p<0.001). Propensity matching did not change the results of inpatient LOS (5 vs. 4 days, P<0.001) or transfer to SNF or ICF (25.4% vs. 18.3%, p<0.001). On multivariate analysis, dialysis was associated with an increased risk of admission, adjusted relative risk 1.03 95% CI 1.02–1.04. Dialysis patients also had higher rates of in-hospital mortality, 4% vs. 1%, p<0.001. Dialysis was associated with over 3 times the odds of in-hospital mortality (adjusted odds ratio 3 95% CI 3.1 – 3.8) (Figure 3).
Figure 3:
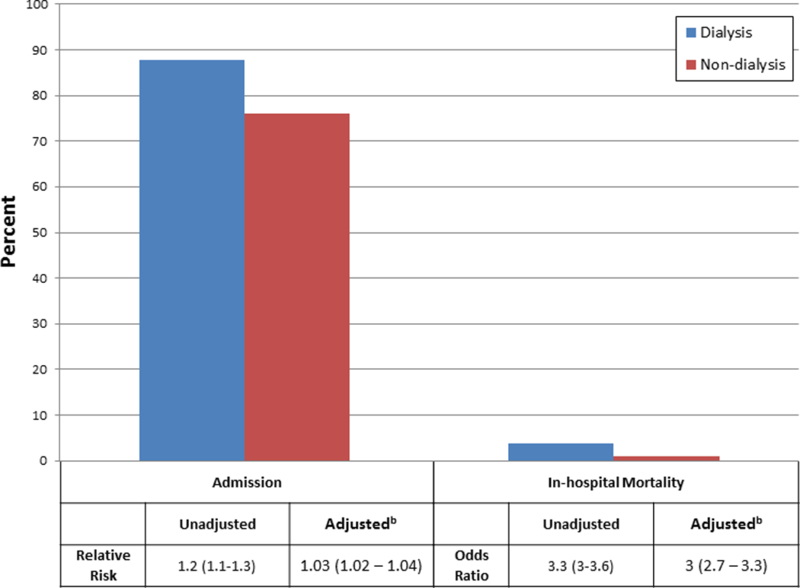
Comparison of hospital admission and in-hospital mortality between matcheda dialysis and non-dialysis patients who present to the emergency department for an adverse drug effect. aMatched for age, gender, congestive heart failure, diabetes mellitus, liver disease, AIDS, hypertension, chronic lung disease, and peripheral vascular disease. bAdjusted for valvular heart disease, alcohol abuse, drug abuse, depression, CCI, primary payer, income quartile by zip, hospital teaching status, and hospital urban/rural designation
Discussion:
Utilizing a large nationally representative all-payer database, we found that while ED visits for ADEs have decreased, they remain 10 times higher in the dialysis population compared to the non-dialysis population. The top medication category associated with ED visits for ADEs was agents that primarily affected blood constituents which increased in frequency while other medication categories decreased. Even after propensity matching and multivariate adjustment, ED visits for ADEs in dialysis patients had significantly higher rates of hospital admission and in-hospital mortality compared to non-dialysis patients.
Overall ED visits for ADEs have decreased between 2008 and 2013. One potential explanation for the decrease in ED visits for ADEs may be related to the increased use of electronic health records (EHR). In 2011, the Centers for Medicare and Medicaid (CMS) established the Medicare and Medicaid Electronic Health Record Incentive Program which has significantly grown EHR use across health systems. EHR allows for e-prescriptions, and the higher use of e-prescribing has been associated with a significantly lower number of ED visits and hospitalizations for ADEs in patients with diabetes.[11]
The widespread use of EHR allows for interventions such as a computer-based program to notify prescribers of patients at high risk of ADEs. One study in the general population found that such a computer program had a sensitivity of 60.4% to 91.7% at identifying criteria associated with high risk of ADEs.[12] Additionally, studies evaluating clinical decision support systems (CDSSs) on reducing ADEs while not statistically significant are suggestive towards reducing ADE’s.[13] Lastly, the addition of a clinical pharmacist to the multidisciplinary care of dialysis patients may be of potential benefit at identifying and reducing drug related problems.[2,14] In a study of 45 hemodialysis patients over a one month period identified 126 drug related problems.[2] Another study done in the Netherlands found that community pharmacist review of medications over a four month period reduced potential drug related problems by an average of 16.3% (95% confidence interval 8.3 – 24.3).[14]
The high proportion of dialysis patients who presented to the ED for ADE likely reflects the higher co-morbidity burden and pill burden that dialysis patients’ face. A chart review of outpatient HD patients found that over 90% of patients had three or more medical problems, and nearly 90% of patients were prescribed six or more medications.[1] While admissions were significantly higher in the dialysis group, the difference was substantially decreased after propensity matching. This suggests that patient comorbidities and demographics, and hospital characteristics are a large contributor to in-patient admissions for ADEs. However, even after propensity matching and additional adjustments, dialysis was associated with a 3% increased risk of hospital admission. Unfortunately date of last dialysis prior to ED visit and route of medication delivery is not included in the NEDS and we are unable to determine the effect of these dialysis specific factors on outcomes of ED visits for ADEs.
We found double the number of ED visits for ADEs in patients on HD compared to PD. It has well been documented that HD patients are older, with more comorbidities than PD patients.[15] Less comorbidities translates to fewer medications. Additionally, clearance of medications differs between HD and PD due to the use of biocompatible membranes in HD versus peritoneal membrane in PD and the thrice-weekly HD prescription as compared to the daily PD prescription. Lastly, medications administered to PD and HD patients differ, with HD patients receiving more intravenous medications such as erythrocyte stimulating agents and vitamin D analogs. Due to the small percentage of patients on PD in this study (<4% of the HD population), comparisons between HD and PD patients were not done.
In attempts to identify a subgroup of patients with similar comorbidity and pill burden as dialysis patients, we performed a propensity match analyses which matched on patient demographics and comorbidities which are common and contribute to the high pill burden of dialysis patients. A surprising finding was that before and after matching, ED visits for non-dialysis patients had significantly higher rates of depression and drug abuse. Depression has been found in multiple populations to be associated with increased ADEs.[16–18] It is currently unclear why depression was higher in ED visits for ADE in non-dialysis patients.
For those ED visits which lead to a hospital admission, LOS was significantly longer for dialysis patients compared to non-dialysis patients. Factors such as age, race, gender, dialysis vintage, and inpatient provider type may affect the LOS of dialysis patients.[19–21] Even after propensity matching, there was no substantial change in the difference in LOS between dialysis and non-dialysis patients. As dialysis treatment days cannot be identified from the NEDs, to what extent the need for the dialysis treatment delayed discharge is currently unclear. Additionally, dialysis patients were more likely to be discharged to SNF, which may be due to the older age of dialysis patients and the increased care required for dialysis patients. The higher rate of discharge to SNF did not change after propensity matching. Unfortunately, we are unable to determine how many patients were already residing in SNFs prior to admission.
An interesting finding is that agents that primarily affected blood constituents was the number one medication category to cause ED visits for ADEs, with most of the drugs being anticoagulants. While ADEs for the other categories were stable or declining, ED visits for agents that primarily affecting blood constituents was the only medication category that increased. This is temporally correlated with the Food and Drug Administration (FDA) approval of new oral anticoagulants (NOACSs) such as dabigatran in 2010, rivaroxaban in 2011, and apixaban in 2012. Most trials of the NOACS excluded patients with renal failure. Of the currently available oral anticoagulants on the market, only apixaban is approved for use in patients on dialysis, however this is based off of a study which was conducted on 8 hemodialysis patients.[22,23] There is an ongoing trial (RENAL-AF) which is testing the safety of apixaban in dialysis patients.[24] Despite the lack of safety and efficacy data in dialysis patients, the use of NOACs was found to be increasing, with a point prevalence for use of dabigatran and rivaroxaban to be 4.6 per 100 atrial fibrillation patients on dialysis.[25] In the same study, dabigatran and rivaroxaban was associated with a 48% and 38%, respectively, increased risk of major bleeding and a 78% and 71% increased risk of hemorrhagic death compared to warfarin. The increase in agents that primary affected blood constituents is a large contributor to the increase in ED visits for ADEs in dialysis patients between 2012 and 2013. However, since we are unable to assess specific anticoagulants responsible for this temporal increase, further studies utilizing more granular data are needed.
This study has several limitations. While the use of the NEDS allows for national estimations to be made, the administrative nature of the database does not allow for identification of exact medications associated with ADEs and important clinical factors such as residual renal function, and timing of medication initiation. We are unable to identify the reasons patients are admitted from the ED to the hospital. Identification of ADEs was done utilizing ICD codes, which while highly specific (98–99%) have relatively low sensitivity (28%), however this is likely to underestimate the impact of ADEs in both dialysis and non-dialysis groups equally.[26] Additionally, it does not contain outpatient data; therefore we do not have information on the number of medications patients were taking at the time of ADE or the reasons these medications were started. Unfortunately, outpatient mortality data is not available and therefore we are unable to assess the association between ADEs and out of hospital mortality. We only had NEDS data until 2013, and therefore the current burden of ADE is unclear. As the NEDS unit of analyses is at the discharge level, it is possible that we are seeing multiple ED visits in the same person. Lastly, as this is an observation study, we cannot determine causality. Despite these limitations, the use of a nationally representative database yields results which are generalizable to the United States dialysis population.
In conclusion, ED visits for ADEs in dialysis patients have decreased over time but remain substantially higher than in the general population. Nearly 90% of all ED visits for ADEs in dialysis patients results in a hospital admission. Further research is needed to identify specific reasons for ADEs and potential interventions to decrease this avoidable complication.
Supplementary Material
Acknowledgements:
None
L.C. is supported in part by the NIH (5T32DK007757 – 18). G.N.N. is supported in part by the NIH (1K23DK107908–01A1).
Footnotes
Disclosures:
References:
- 1.Manley HJ, McClaran ML, Overbay DK, Wright MA, Reid GM, Bender WL, et al. : Factors associated with medication-related problems in ambulatory hemodialysis patients. Am J Kidney Dis 2003;41:386–393. [DOI] [PubMed] [Google Scholar]
- 2.Grabe DW, Low CL, Bailie GR, Eisele G: Evaluation of drug-related problems in an outpatient hemodialysis unit and the impact of a clinical pharmacist. Clin Nephrol 1997. [cited 2017 Jun 23];47:117–21. [PubMed] [Google Scholar]
- 3.NEDS Overview. Healthcare Cost and Utilization Project (HCUP). December 2016. Agency for Healthcare Research and Quality, Rockville, MD: www.hcup-us.ahrq.gov/nedsoverview.jsp. [PubMed] [Google Scholar]
- 4.United States Renal Data System. 2015. USRDS annual data report: Epidemiology of kidney disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2015. [Google Scholar]
- 5.U.S. Census Bureau; Population and Housing Unit Estimates; Available from: https://www.census.gov/programs-surveys/popest/data/tables.2008.html
- 6.Kern EFO, Maney M, Miller DR, Tseng C-L, Tiwari A, Rajan M, et al. : Failure of ICD-9-CM codes to identify patients with comorbid chronic kidney disease in diabetes. Health Serv Res 2006;41:564–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.HCUP: Elixhauser Comorbidity Software, Version 3.7 [cited 2017 Jan 1]; Available from: https://www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp
- 8.ESRD Analytical Methods [cited 2017 Nov 13]; Available from: https://www.usrds.org/2015/view/v2_00_appx.aspx
- 9.Charlson M, Szatrowski TP, Peterson J, Gold J: Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245–1251. [DOI] [PubMed] [Google Scholar]
- 10.Davies HT, Crombie IK, Tavakoli M: When can odds ratios mislead? BMJ 1998. [cited 2017 Dec 1];316:989–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gabriel MH, Powers C, Encinosa W, Bynum JPW: E-Prescribing and Adverse Drug Events. Med Care 2017;55:456–462. [DOI] [PubMed] [Google Scholar]
- 12.Isaksen SF, Jonassen J, Malone DC, Billups SJ, Carter BL, Sintek CD: Estimating risk factors for patients with potential drug-related problems using electronic pharmacy data. IMPROVE investigators. Ann Pharmacother 1999;33:406–12. [DOI] [PubMed] [Google Scholar]
- 13.Kaushal R, Shojania KG, Bates DW, P S, CR B, DW B: Effects of Computerized Physician Order Entry and Clinical Decision Support Systems on Medication Safety. Arch Intern Med 2003;163:1409. [DOI] [PubMed] [Google Scholar]
- 14.Vinks THAM, Egberts TCG, de Lange TM, de Koning FHP: Pharmacist-based medication review reduces potential drug-related problems in the elderly: the SMOG controlled trial. Drugs Aging 2009. [cited 2017 Jun 26];26:123–33. [DOI] [PubMed] [Google Scholar]
- 15.Vonesh EF, Snyder JONJ, Foley RN, Collins AJ: The differential impact of risk factors on mortality in hemodialysis and peritoneal dialysis. Kidney Int 2004;66:2389–2401. [DOI] [PubMed] [Google Scholar]
- 16.Zhou T, Duan J, Zhou G, Cai J, Huang Z, Zeng Y, et al. : Impact of Depression Mood Disorder on the Adverse Drug Reaction Incidence Rate of Anticancer Drugs in Cancer Patients. J Int Med Res 2010. [cited 2018 Feb 21];38:2153–2159. [DOI] [PubMed] [Google Scholar]
- 17.Onder G, Penninx BWJH, Landi F, Atkinson H, Cesari M, Bernabei R, et al. : Depression and Adverse Drug Reactions Among Hospitalized Older Adults. Arch Intern Med 2003;163:301. [DOI] [PubMed] [Google Scholar]
- 18.Kim S-K, Park S-P, Kwon O-Y: Impact of depression and anxiety on adverse event profiles in Korean people with epilepsy. Epilepsy Behav 2015;46:185–91. [DOI] [PubMed] [Google Scholar]
- 19.Yan G, Norris KC, Greene T, Yu AJ, Ma JZ, Yu W, et al. : Race/Ethnicity, Age, and Risk of Hospital Admission and Length of Stay during the First Year of Maintenance Hemodialysis. Clin J Am Soc Nephrol 2014;9:1402–1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kshirsagar A V, Hogan SL, Mandelkehr L, Falk RJ: Length of stay and costs for hospitalized hemodialysis patients: nephrologists versus internists. J Am Soc Nephrol 2000. [cited 2018 Feb 23];11:1526–33. [DOI] [PubMed] [Google Scholar]
- 21.Kumar VA, Sidell MA, Yang W-T, Jones JP: Predictors of Peritonitis, Hospital Days, and Technique Survival for Peritoneal Dialysis Patients in a Managed Care Setting. Perit Dial Int 2014;34:171–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eliquis Package Insert Princeton NJ: Bristol-Myers Squibb [Google Scholar]
- 23.Wang X, Tirucherai G, Marbury TC, Wang J, Chang M, Zhang D, et al. : Pharmacokinetics, pharmacodynamics, and safety of apixaban in subjects with end-stage renal disease on hemodialysis. J Clin Pharmacol 2016;56:628–36. [DOI] [PubMed] [Google Scholar]
- 24.Trial to Evaluate Anticoagulation Therapy in Hemodialysis Patients with Atrial Fibrillation (RENAL-AF) Available from: https://clinicaltrials.gov/ct2/show/NCT02942407.
- 25.Chan KE, Edelman ER, Wenger JB, Thadhani RI, Maddux FW: Dabigatran and Rivaroxaban Use in Atrial Fibrillation Patients on HemodialysisCLINICAL PERSPECTIVE. Circulation 2015. [cited 2017 Jun 23];131 Available from: http://circ.ahajournals.org/content/131/11/972.long [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hohl CM, Karpov A, Reddekopp L, Stausberg J: ICD-10 codes used to identify adverse drug events in administrative data: a systematic review. J Am Med Informatics Assoc 2014;21:547–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


