Abstract
The purpose of this review is to analyse current literature related to the clinical applications of 3D printed models in liver disease. A search of the literature was conducted to source studies from databases with the aim of determining the applications and feasibility of 3D printed models in liver disease. 3D printed model accuracy and costs associated with 3D printing, the ability to replicate anatomical structures and delineate important characteristics of hepatic tumours, and the potential for 3D printed liver models to guide surgical planning are analysed. Nineteen studies met the selection criteria for inclusion in the analysis. Seventeen of them were case reports and two were original studies. Quantitative assessment measuring the accuracy of 3D printed liver models was analysed in five studies with mean difference between 3D printed models and original source images ranging from 0.2 to 20%. Fifteen studies provided qualitative assessment with results showing the usefulness of 3D printed models when used as clinical tools in preoperative planning, simulation of surgical or interventional procedures, medical education, and training. The cost and time associated with 3D printed liver model production was reported in 11 studies, with costs ranging from US$13 to US$2000, duration of production up to 100 h. This systematic review shows that 3D printed liver models demonstrate hepatic anatomy and tumours with high accuracy. The models can assist with preoperative planning and may be used in the simulation of surgical procedures for the treatment of malignant hepatic tumours.
Keywords: Hepatic tumour, Model, Simulation, Surgical planning, Three-dimensional printing
Background
The application of three-dimensional (3D) printing in medicine is a relatively new and rapidly growing area of research [1–7]. Existing literature explores the utilisation of 3D printed models as tools in medical education, simulation in surgical training, patient-doctor communication, diagnosis, and pathological classification [4–7]. More specifically, 3D printed models have been identified as useful tools in the planning and conduction of complex surgical procedures, with the ability of current 3D printing technologies to generate accurate, patient-specific anatomical and pathological characteristics [4–11]. Information pertaining to structural depth, spatial relationships, topological characteristics, and anatomical networks may also be appreciated and understood [12, 13]. Such understandings are facilitated by the visualisation and manipulation of physical 3D printed models, with the tactile experience enhancing the viewer’s comprehension of important features [14, 15].
Deep understanding of the complex liver anatomy is of paramount importance in preoperative planning of any liver resection; however, two-dimensional (2D) diagnostic imaging does not always provide comprehensive understanding of anatomical and pathological complexities which are required by surgeons to perform hepatic resections. 3D printed models are currently being used to understand the complex and highly variable anatomical characteristics of the liver [16–20]. Studies report the application of 3D printing in treatment planning for liver lesions where physical models are used as clinical tools to facilitate the in-depth understanding of patient-specific anatomy and pathology required to direct preoperative (and occasionally intraoperative) decision-making processes [16–20].
Current literature agrees upon various clinical contributions offered by the visualisation and manipulation of 3D printed liver models in surgical planning. However, the reported contributions do not necessarily make these tools feasible for frequent use within the clinical environment [12]. The purpose of this review is to critically analyse current literature that explores the clinical value and applications of utilising 3D printed liver models in clinical practice. It is expected that this systematic review will raise awareness of current applications, feasibility measures and consensus, and the limitations associated with 3D printed liver model production.
Methods
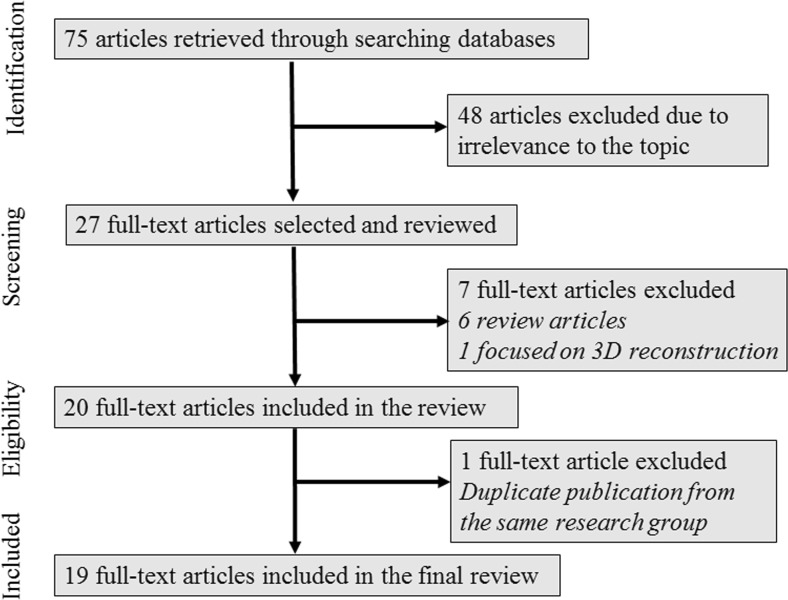
This review was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [21]. A comprehensive search of the literature was conducted to source original studies from a variety of databases including Medline/Pubmed, Scopus, Springer Link, CINHAL Plus, ScienceDirect, and Informit (Health Collection). The keywords utilised to perform the search included ‘three-dimensional’ or ‘3D’, ‘printing’ or ‘print*’, ‘liver’, ‘surgery’, ‘plan*’, and ‘treatment’. The asterisk (*) is a search engine wildcard that was used to facilitate a wider search of the literature. These keywords were used collectively and in various combinations. Articles were included if they were peer-reviewed studies published in English within the last 10 years (last search: February 2018). The title and abstract of each article was assessed to verify relevance and coherence with the review purpose. Review articles including systematic reviews and conference abstracts were excluded according to the selection criteria. Articles were also retrieved through sourcing applicable studies cited within relevant literature. A summary of the literature search process is shown in Fig. 1.
Fig. 1.
Flow chart showing the search strategy to identify eligible studies
It should be noted that original research related to 3D printing in surgical planning for the treatment of liver lesions is limited. To source relevant information, the scope of the literature search was expanded and was not limited to original studies. Consequently, case reports were included in this review due to their dominance within the current literature.
Data Extraction and Critical Appraisal Strategies
Once all relevant literature was collected, each article was analysed to identify and extract discussion related to the accuracy, clinical value, and feasibility of 3D printed liver models in medicine and education. Two assessors independently reviewed the full texts of all relevant articles and agreed upon three topical areas for analysis and discussion. This includes accuracy of 3D printed models and capacity to replicate hepatic anatomical structures and pathologies, the usefulness and feasibility of utilising 3D printed models in surgical planning or simulation in the treatment of liver lesions, and the specifics of 3D printed liver model generation (including software packages used, 3D printing materials and associated costs, time required for 3D printing, and duration of the entire processing related to 3D printing).
Results
Literature Search Outcome
The initial search retrieved 75 articles. After screening the titles and abstracts, 27 full-text articles were selected and reviewed, with 7 articles further excluded with 6 of these being review articles (4 general review articles, 2 systematic reviews) and 1 study focusing on 3D image reconstruction technique instead of 3D printing [22–28]. Another article was also excluded due to duplicate publication in different journals from the same research group [29]. A total of 19 articles met the inclusion criteria and were included for analysis in this review [16–20, 30–43].
Table 1 summarises study characteristics of 3D printed models in liver disease. Of the 19 studies, 17 were isolated case reports with 12 involving the generation of 1 patient-specific 3D printed model of liver tumours or hepatic vessels, and the remaining 5 involving the generation of 3–10 models. The remaining 2 studies were original research papers, consisting of 1 retrospective study [32] and 1 randomised controlled trial [36].
Table 1.
Study characteristics of 3D printing in liver disease
| First author and year of publication | Study sample size | Study purpose | Imaging modalities used for 3D printing | Software used for image segmentation/time for segmentation | 3D printer/printing materials/costs/ printing duration | Key findings |
|---|---|---|---|---|---|---|
| Baimakhanov et al. 2015 [30] | Case report 1 printed model of liver and hepatic veins |
Preoperative simulation | CT | Synapse Vincent Program Time for segmentation: not provided |
Not provided | 3D printed model guides selection of appropriate surgical strategy and is helpful during surgical planning and training. |
| Bucking et al. 2017 [31] | Case demonstration 3 printed models of the ribs, liver and lung |
A workflow to generate 3D printed models using medical imaging data | CT | Seg3D (v2.2.1) and 3D Slicer (v.4.6) Time for segmentation: not provided |
Fused Deposition Modelling Polylactic acid £10 (USD13) 27.5 h |
High accuracy of 3D printed model with percentage error less than 2% between measurements on 3D printed model and those in computer model. |
| Choi et al. 2017 [32] | Retrospective study of 20 patients with liver metastasis before and after chemotherapy. 20 3D printed hepatic tumour models. | Accuracy of 3D printed tumour volume measured by ultrasound in comparison with reference volume from CT images | CT | In-house MISSTA software Time for segmentation: not provided |
MakerBot Replicator Cost and printing duration: not provided |
No significant difference in tumour volume measured between reference CT images and 3D printed models (7.42 ± 5.76 vs. 7.44 ± 5.80 ml, p > 0.05) with excellent correlation between two methods (r > 0.940) and high inter-observer reliability (ICC = 0.958–0.988). |
| Igami et al. 2014 [33] | Case report 1 printed model of liver tumour |
For performing hepatectomy | CT | In-house-developed “PLUTO” software “Marching Cubes” Time for segmentation: not provided |
AGILISTA- 3100 Rigid acrylic resin 70% scale of the model. 50,000¥ (USD444) 36 h (2–3 days finishing work after 3D printing) |
3D printed model is useful in hepatectomy for a small tumour and thus, assists surgical procedures. |
| Javan et al. 2017 [34] | Case demonstration 5 customised printed models of liver, lungs, prostate, coronary arteries and Circle of Willis |
Understanding complex anatomy and segments | 2D diagrams were used to design hepatic anatomical structures | Online source: FlatPyramid.com Time for segmentation: not provided |
i Materialise (online service) Polyamide (nylon) USD40–100 1–3 weeks for digital design 10–14 days for 3D printing and shipping |
3D printed model demonstrates complex anatomy and liver segments and it could serve as medical educational purpose. |
| Javan and Zeman 2017 [35] | 1 customised 3D printed model with hepatic lobes and hollow structures with simulated abscess and tumour | Demonstration and simulation of hepatobiliary interventional procedures and educational purpose | Graphically designed of hepatic structures including the gallbladder and biliary system | Online source: FlatPyramid.com Time for segmentation: not provided |
i Materialise (online service) Resin and polyamide USD1000 for 8 pieces Printing duration: not provided |
The 3D printed model allows for preoperative planning and simulation of different diagnostic and therapeutic interventional procedures such as abscess drainage, artery embolization, and catheter placement. |
| Kong et al. 2016 [36] | Randomised control study: 61 medical students and 6 experts. 1 printed model of healthy candidate |
Development of novel 3D hepatic segment model for teaching anatomy | CT | Geomagic 12 (3D Systems, Morrisville, NC) Time for segmentation: not provided |
Spectrum Z 510 Composite Power Cost and printing duration: not provided |
3D printed model provides good realism for instruction of anatomy teaching and significantly improves knowledge when compared to the traditional method (p < 0.05). |
| Leng et al. 2016 [37] | Case report 1 printed model of liver metastasis |
Construction of realistic liver model | CT | Mimics (Mimics, Materialise, Belgium) Time for segmentation: not provided |
Objet 350 Connex USD100 Printing duration: not provided |
3D printed model represents realistic background textures and thus, could be used to study the effect of radiation dose reduction and detect subtle liver lesions. |
| Madurska et al. 2017 [18] | Case report 1 printed model of hepatic malignant tumour |
Preoperative planning | CT and MRI | Amira 4.5.4 visualisation software (FEI, Hillsboro, NJ) Time for segmentation: not provided |
Object Eden 350 V TangoPlus and TangBlack 1:1 scale USD500–600 Printing duration: not provided |
3D printed liver model demonstrates complex anatomical structures of the liver and their relationship to the tumour. |
| Oshiro et al. 2017 [38] | Case report 1 printed model of liver tumour |
Application of 3D printed model in hepatectomy | CT | SYNAPSE VINCENT (Fuji Film Medical, Tokyo, Japan). 1.5 h |
EOSINT P760 Polyamide 12 50% scale of the model USD600 (cost of materials: < USD150) 72 h |
3D-printed liver model made the surgical procedure easier, reduced the production cost and improved the visibility of small tumours. |
| Perica and Sun 2017 [39] | Case report 1 printed model of liver tumour |
Preoperative planning for resectable HCC | CT | Analyze 12.0 (AnalyzeDirect, Inc., Lexana, KS, USA) and Geomagic Wrap 2017 (3D Systems, Seoul, Korea) 6 h for segmentation 4.25 h for post-processing 4 h for editing |
Objet 500 Connex3 Stratasys VeroClear transparent and rigid opaque photopolymers 60% scale of the model USD980 11 h |
3D printed liver model has limited value in diagnostic radiology; however, it has potential usefulness in pre-surgical planning and intraoperative guidance for HCC treatment; 15–20% difference was found in average dimensional measurements between original CT and STL file and physical 3D model, while 7% difference was found between STL file and 3D model. |
| Soejima et al. 2016 [40] | Case report 1 printed model of a liver graft |
Preoperative simulation in LDLT | CT | ZedView, Data Design, Nagoya, Japan) Time for segmentation: not provided |
Objet Connex500 Acrylic-based photopolymer resin (TangoPlus and TangoBlackPlus) USD2000 24 h |
Preoperative simulation by 3D printed liver model is especially helpful for small infants or neonates receiving LDLT. 3D printed model represents realistic liver graft which allows surgeons to perform donor surgery. |
| Souzaki et al. 2015 [41] | Case report 1 printed model of hepatoblastoma |
Preoperative planning | CT | ZedView, Data Design, Nagoya, Japan) Time for segmentation: not provided |
Objet Connex500 Acrylic ultraviolet curable resin Cost and printing duration: not provided |
3D printed model improves understanding of abnormal anatomy and assists surgical planning of paediatric malignant tumours. |
| Takagi et al. 2014 [42] | Case report 1 printed model of liver with perihilar cholangiocarcinoma |
Reproducibility of 3D printed model and future preoperative simulation | CT | ZedView and Geomagic Graphics (Geomagic, Cary, NC, USA) Time for segmentation: not provided |
Objet Connex260 Printing materials, cost and printing duration: not provided |
First reported case of reproducing 3D printed model of malignant hepatobiliary tumour which could aid future preoperative simulation. |
| Takao et al. 2016 [43] | Case report 10 printed models of portal vein stenosis |
Preoperative simulation and accuracy of the model | CT | OsiriX 6.5.2 Time for segmentation: not provided |
Fused Deposition Modelling Lylon Cost and printing duration: not provided |
Quantitative assessments of models showed high accuracy when compared to those from the mask images in terms of maximum and minimum cross-sectional area (193 ± 1.5, and 18 ± 1.0 mm2 vs. 200 and 15 mm2) and percentage of stenosis (90.6 ± 0.5 vs. 92.5%). |
| Watson 2016 [19] | Case series Multiple 3D printed models of normal hepatic anatomy |
3D printed hepatic model for surgical resident education | CT or MRI | TeraRecon (San Mateo, CA) Time for segmentation: not provided |
Shapeways (online service) Nylon plastic < USD100 Printing duration: not provided |
Feasibility of creating patient-specific 3D printed hepatic models with low cost. |
| Witowski et al. 2017 [17] | Case report 1 printed model of hepatic metastasis |
Preoperative planning | CT | Open-source Horos and Blender, and Meshmixer open-source software | Fused Deposition Modelling Polylactic acid < USD150 60–100 h Time from segmentation to final object: 160 h |
Useful for preoperative planning of complex surgical procedures, such as hepatic resections, also valuable for education of students and patients. |
| Xiang et al. 2015 [20] | Case report 1 printed model of large HCC |
Role of 3D printed model in treatment of massive HCC | CT | Medical Imaging Three Divisional Visualization System (MI-3DVS) and Geomagic 2013 Time for segmentation: not provided |
Spectrum ZTM 510 Composite material Cost and printing duration: not provided |
Assists preoperative planning of complex HCC with variations of hepatic anatomy and guides intraoperative procedures with precision and safety in hepatectomy. |
| Zein et al. 2013 [16] | Case series 6 printed liver models with 3 from living donors and 3 from LDLT recipients. |
Preoperative planning in LDLT | CT and MRI | MeVis (MeVis Medical Solutions AG) and Magics software (Materialise) Time for segmentation: not provided |
Connex 350 TangoPlus/VeroclearPlus TangoPlus/VeroBlue 25–40 h |
3D printed liver models are highly accurate in providing liver volume and geometric measurements when compared to those from recipient’s and donor’s livers with mean dimensional errors < 4 mm for the whole model and < 1.3 mm for vascular diameters (p = 0.91–0.99). |
CT computed tomography, HCC hepatocellular carcinoma, ICC intraclass correlation coefficient, LDLT living donor liver transplantation, MRI magnetic resonance imaging, N/A not available
Original Data Source for 3D Printed Model Generation
Computed tomography (CT) is the most commonly used imaging modality for segmentation of anatomical structures, with 14 studies using CT datasets as the source of data for 3D printing. CT and/or magnetic resonance imaging (MRI) datasets were used in 3 studies, while in the remaining 2 studies, 3D printed models were generated based on 2D diagrams to illustrate hepatic structures (Table 1).
Quantitative Assessment of 3D Printed Liver Model Accuracy
Of the included 19 studies, only 5 provided quantitative assessment of 3D printed model accuracy [16, 31, 32, 39, 43]. Comparison of dimensional accuracy between 3D printed models and original source imaging data were reported in 4 studies [16, 31, 39, 43], while comparison of liver volume between 3D printed models and preoperative CT image, and comparison of hepatic tumour volume between 3D printed models and CT images was reported in 2 studies, respectively [16, 32].
Quantitative analysis of these studies showed that 3D printed models were generally accurate in replicating anatomical hepatic structures and pathologies with differences between 3D printed models and original source images ranging from 0.20 to 20.8%. Of 4 studies comparing hepatic anatomy measurements, high accuracy was found in 3 studies with mean error between 1.30 and 5.08% [16, 31, 43]. Large differences in measurements of hepatic structures were noticed in a recent study when comparing 3D printed model with original CT and standard tesselation language (STL) images [39]. Results of this study showed that the smallest measurement difference was 7.4% when comparing 3D printed model with STL, while the largest difference was 20.80% when comparing 3D printed model with original CT images.
Of two studies comparing liver volumes between 3D printed models and original source images, very high accuracy was reported in one study with mean error of measuring hepatic tumour volume being 0.20% [32]. In the other study [16], the mean difference in volume measurements between 3D printed models and recipient’s liver lobes, 3D printed models and donor’s liver lobes was 6.9 and 4.7%, respectively.
Qualitative Assessment of Usefulness of 3D Printed Liver Models
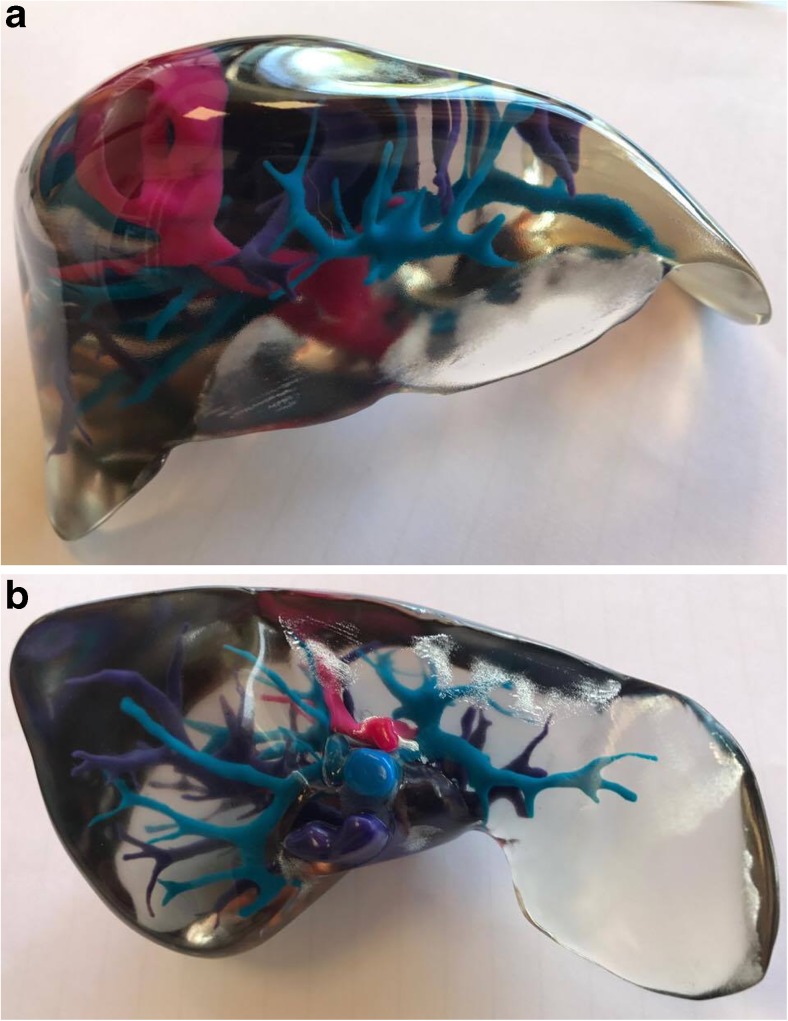
Although most (89%) of the studies in this review are case reports, patient-specific 3D printed models were found to replicate complex hepatic anatomy and tumours (Fig. 2), with some achieving high accuracy determined by comparing measurements taken from 3D printed models and original image data. Further, 3D printed models were shown to be very helpful in preoperative planning and simulation of treatment of malignant hepatic tumours, in particular, guiding intraoperative procedures such as hepatectomy of a small tumour for an infant (Table 1). 3D printed liver models are also reported to play an important role in the education of medical students and patients.
Fig. 2.
3D printed model of hepatocellular carcinoma. a Anterior view of the 3D printed liver model. b Inferior view of the 3D printed model. Pink colour: tumour and hepatic artery, purple colour: hepatic vein, blue colour: portal vein. The model was printed with a scale of 60% of original size with use of a Vero Clear/Transparent photopolymer. Reprinted with permission under the open access from Perica E and Sun Z [39]
In a study conducted by Kong et al. [36], authors compared the educational outcomes of using 3D visualisation, 3D printed models, and traditional anatomical atlases as learning aids. Sixty-one medical students were divided into three groups through random assignment. Each group was given one learning aid to answer questions related to hepatic anatomy. Both 3D visualisation and 3D printed models were found to significantly improve understanding of the hepatic anatomy when compared to the traditional teaching method (p < 0.05), although there were no significant differences between 3D visualisation and 3D printed models in each index of assessments (p > 0.05).
Two studies created 3D printed liver models based on 2D diagram/graphic designs [34, 35]. One of them focused on demonstration of complex anatomy for educational purposes [34], while another one provided insight into the clinical value of 3D printed model for multidisciplinary interventional procedures [35]. In their study, Javan and Zeman developed a 3D printed liver model with hepatic parenchyma, hollowed hepatic vessels, and biliary structures. Further, authors created abscesses and tumours in the model to allow simulation of interventional procedures such as stent placement during transjugular intrahepatic portosystemic shunt procedure (TIPS), or percutaneous cholecystostomy tube placement [35]. Despite its great potential for training and education, patient-specific hepatobiliary models are needed to represent realistic conditions for clinical application.
Cost and Time Associated with 3D Printing in Liver Models
The cost of 3D printing is variable and is highly dependent on the materials used and/or whether the liver was printed as a full-size or scaled down model. The cost associated with 3D printing was reported in 11 studies and ranged from the lowest USD13 to as high as USD2000. Due to the expensive nature, scaling down full-size liver models to 50 and 70% was reported in 3 studies with costs between USD444 and USD980. Different types of 3D printers were used according to this review, with Objet Connex (Stratasys) being the most common one, followed by fused deposition modelling (FDM), which was used in 7 and 3 studies, respectively.
Different software packages were used in image processing and segmentation, including common commercial software such as Mimics and TeraRecon, open-source, and in-house-developed software tools (Table 1). The time spent on image processing, segmentation, and editing of data for 3D printing preparation was only reported in 1 study as shown in the table [39], while in another study, the duration of 1.5 h was reported to include processes from image processing and segmentation to conversion of STL file [38].
Time taken for 3D printing was reported in 6 studies [16, 31, 33, 38–40], with duration of 3D printing process ranging from 11 to 100 h. In a recent study by Javan et al. [34], authors reported that it took 1–3 weeks for digital design of the models and 10–14 days for 3D printing and shipping, which is much longer than other studies which created 3D printed models based on patient’s imaging data. In another study by Witowski et al. [17], authors reported that the total time from image segmentation to final 3D printed object is 160 h.
Discussion
The review analyses 19 studies related to the clinical application of 3D printed liver models with three main key findings summarised: first, 3D printed liver models haven been successfully generated with use of CT or MRI imaging data, replicating hepatic anatomy and pathology with high accuracy. The accuracy of 3D printed models was confirmed by quantitative analysis, comparing measurements taken from 3D printed models and the original image data or reference images. Second, 3D printed models have served as valuable tools in preoperative planning and simulation of surgical or interventional procedures for treatment of malignant hepatic tumours. Last, 3D printed models have also been successfully applied in an educational setting, being used as tools in the education of medical students and patients to improve their understanding of complex hepatic anatomy and pathology.
There are two similar systematic review articles currently available in the literature; however, their analyses consist of different types of articles. Witowski et al. reviewed 14 articles; however, 3 of them are conference abstracts and 1 is a general review article [22]. Soon et al. only identified 6 eligible articles in their review; however, 1 of them is a general review article [23, 24]. In this systematic review, we searched different databases with inclusion of 19 studies dealing with the applications of 3D printed models in liver disease. Thus, this review represents a more comprehensive analysis of the current literature regarding the clinical applications of 3D printed liver models. Findings of this review are consistent with those reported in the other systematic reviews, but more detailed analysis of the literature in terms of both quantitative and qualitative assessments of the clinical value of 3D printed liver models is provided in this review, thus further advancing the current literature.
Despite wide availability of 2D and 3D visualisation techniques in liver image analysis [44–46], it may be difficult to fully understand the hepatic tumours in relation to surrounding complex anatomy. 3D printed models are increasingly used in clinical practice showing great value in preoperative planning and simulation of surgical and interventional procedures, in particular in the field of cardiovascular disease [4–8]. 3D printed physical models provide direct visualisation of anatomical structures when compared to the reconstructed 3D virtual models in liver disease which are generated from medical images [34]. Further, 3D printed models offer tactile experience which allow surgeons to practice and plan surgical procedures achieving the goal of personalisation and precision in medicine [47]. This is confirmed by this review. In addition to accurate replication of anatomical structures and assistance in pre-surgical planning and simulation, 3D printed liver models demonstrate potential value in detecting subtle lesions and guiding surgical resection of small hepatic tumours as reported in 2 studies [33, 36], although more robust studies are needed to further confirm these findings.
3D printed models may be considered valuable; however, issues related to cost and time of production may challenge the practicality, clinical value, and feasibility. There are two main challenges associated with 3D printing of realistic anatomical models. The first challenge is the considerable amount of time required to complete pre-print processes. This includes semi-automatic or manual segmentation of medical imaging data, and a number of editing processes that are applied to ensure successful 3D printing outcomes. Although medical image processing and segmentation using commercially available software or open-source software tools have been widely reported in the literature [48–51], data segmentation and editing for 3D printing purpose is subject to the use of software environment and user expertise. To ensure accuracy of image segmentation and identification of anatomical structures required for pre-surgical planning of liver disease, users should have a sound understanding of the software used and the normal anatomy and pathology of interest [22, 35, 39, 52]. Madurska et al. reported that while automatic and semi-automatic algorithms for liver segmentation do exist, the outcomes of their application are often unsuccessful in image datasets where hepatic and non-hepatic structures exhibit similar radiographic densities [18]. CT datasets are commonly used for the generation of 3D printed liver models due to its high spatial resolution. This allows for detection and definition of hepatic anatomical structures during different phases of contrast enhancement. Although MRI is sensitive to visualise other liver structures, the spatial resolution of current MRI scanners is inferior to that of CT which leads to information loss, thus requiring a significant amount of editing during image processing and segmentation to make it appear more natural. The time spent on image processing, segmentation, and editing could be up to 15 h as reported in 1 study [39]; the whole process of generating a 3D printed liver model could be up to 4–5 days as shown in this review. This needs to be addressed in future studies to make the 3D printing more efficient and feasible for clinical application.
Another challenge is the expense of printing full-sized 3D liver models. Low-cost materials are used in some studies as shown in the review, with costs less than USD100 when the model was printed with Nylon plastic or polylactic acid [19, 31]. However, a high-quality full-sized liver model printed with photopolymer resin (TangoPlus) can cost up to USD2000. Even with models scaling down to 50 to 70%, the cost is between USD400 and USD980 [33, 36, 39]. Thus, reducing the costs associated with 3D printed liver models is necessary to improve feasibility and clinical value.
Some limitations in this review should be acknowledged. First, despite our comprehensive search for relevant articles through different databases, the majority of current studies are based on individual case reports, which is one of the main limitations in the current literature. This is mainly due to the fact that 3D printing in liver disease is a relatively new and emerging technique; thus, it is still at an early stage when compared to other applications such as 3D printing in cardiovascular disease [5, 53]. Further studies, in particular, quantitative assessment with inclusion of more cases, reporting the clinical value of 3D printing in treatment of malignant hepatic tumours are needed because only 5 studies involving quantitative analysis of accuracy of 3D printed liver models were available in this review. Second, although it is generally agreed that 3D printing is a time-consuming process with inclusion of image post-processing, segmentation, editing, and post-print processing, the time spent on image processing and segmentation was only reported in 2 studies, while the duration for the whole 3D printing process was available in 6 studies. This is mainly due to the use of different software packages for image processing and segmentation, as well as researchers’ experience in image post-processing analysis. Therefore, most of the authors did not report the time they spent on image processing and analysis. Further, as discussed previously, most of the current studies are case reports with only 1 model printed; thus, it is difficult to gather information about the average time required for 3D printing. According to this review, it could take up to 100 h to create a 3D printed liver model; thus, further improvement should focus on increasing production speed and reducing cost.
In conclusion, this review demonstrates the feasibility and accuracy of 3D printed liver models in depicting anatomical structures and pathologies. 3D printed models are shown to reliably and accurately replicate hepatic structures and tumours when compared to original images. Further, 3D printed models are reported as useful tools in pre-surgical planning and simulation of liver surgeries, in particular guiding surgical management of small or subtle hepatic lesions, or performing interventional procedures. Future research should address the long duration and high cost associated with 3D printing process. In addition, qualitative and quantitative assessment of clinical value of 3D printed model in liver tumours needs to be determined based on a large cohort of patients.
Compliance with Ethical Standards
Conflict of Interest
The authors declared that they have no conflicts of interest.
References
- 1.Naftulin JS, Kimchi EY, Cash SS. Streamlined, inexpensive 3D printing of the brain and skull. PLoS ONE. 2015;10:1–15. doi: 10.1371/journal.pone.0136198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ho D, Squelch A, Sun Z. Modelling of aortic aneurysm and aortic dissection through 3D printing. J Med Radiat Sci. 2017;64:10–17. doi: 10.1002/jmrs.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmauss D, Haeberle S, Hagl C, Sodian R. Three-dimensional printing in cardiac surgery and interventional cardiology: a single-centre experience. Eur J Cardiothorac Surg. 2015;47:1044–1052. doi: 10.1093/ejcts/ezu310. [DOI] [PubMed] [Google Scholar]
- 4.Valverde I, Gomez G, Gonzales A, Suarez-Mejias C, Adsuar AF, Coserria JF, Uribe S, Gomez-Cia T, Hosseinpour AR. Three-dimensional patient-specific cardiac model for surgical planning in Nikaidoh procedure. Cardiol Young. 2015;25:698–704. doi: 10.1017/S1047951114000742. [DOI] [PubMed] [Google Scholar]
- 5.Sun Z, Lee S. A systematic review of 3-D printing in cardiovascular and cerebrovascular diseases. Anatol J Cardiol. 2017;17:423–435. doi: 10.14744/AnatolJCardiol.2017.7464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Giannopoulos AA, Mitsouras D, Yoo SJ, Liu PP, Chatzizisis YS, Rybicki FJ. Applications of 3D printing in cardiovascular diseases. Nat Rev Cardiol. 2016;13:701–718. doi: 10.1038/nrcardio.2016.170. [DOI] [PubMed] [Google Scholar]
- 7.Martelli N, Serrano C, van den Brink H, Pineau J, Prognon P, Borget I, El Batti S. Advantages and disadvantages of 3-dimensional printing in surgery: A systematic review. Surgery. 2016;159:1485–1500. doi: 10.1016/j.surg.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 8.Jones DB, Sung R, Weinberg C, Korelitz T, Andrews R. Three-dimensional modeling may improve surgical education and clinical practice. Surg Innov. 2015;23:189–195. doi: 10.1177/1553350615607641. [DOI] [PubMed] [Google Scholar]
- 9.Bernhard J, Isotani S, Matsugasumi T, Duddalwar V, Hung A, Suer E, Baco E, Satkunasivam R, Djaladat H, Metcalfe C, Hu B, Wong K, Park D, Nguyen M, Hwang D, Bazargani ST, de Castro Abreu AL, Aron M, Ukimura O, Gill IS. Personalized 3D printed model of kidney and tumor anatomy: a useful tool for patient education. World J Urol. 2016;34:337–345. doi: 10.1007/s00345-015-1632-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vukicevic M, Mosadegh B, Min JK, Little SH. Cardiac 3D printing and its future directions. JACC Cardiovasc Imaging. 2017;10:171–184. doi: 10.1016/j.jcmg.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ploch CC, Mansi CSSA, Jayamohan J, Kuhl E. Using 3D printing to create personalized brain models for neurosurgical training and preoperative planning. World Neurosurg. 2016;90:668–674. doi: 10.1016/j.wneu.2016.02.081. [DOI] [PubMed] [Google Scholar]
- 12.Lambrecht JT, Berndt DC, Schumacher R, Zehnder M. Generation of three-dimensional prototype models based on cone beam computed tomography. Int J Comput Assist Radiol Surg. 2009;4:175–180. doi: 10.1007/s11548-008-0275-9. [DOI] [PubMed] [Google Scholar]
- 13.Preece D, Williams SB, Lam R, Weller R. “Let’s get physical”: Advantages of a physical model over 3D computer models and textbooks in learning imaging anatomy. Anat Sci Educ. 2013;6:216–224. doi: 10.1002/ase.1345. [DOI] [PubMed] [Google Scholar]
- 14.Waran V, Narayanan V, Karuppiah R, Pancharatnam D, Chandran H, Raman R, Rahman ZA, Owen SL, Aziz TZ. Injecting realism in surgical training - Initial simulation experience with custom 3D models. J Surg Educ. 2014;71:193–197. doi: 10.1016/j.jsurg.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 15.Zheng Y, Yu D, Zhao J, Wu Y, Zheng B. 3D printout models vs. 3D-rendered images: which is better for preoperative planning? J Surg Educ. 2016;73:518–523. doi: 10.1016/j.jsurg.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Zein NN, Hanouneh IA, Bishop PD, Samaan M, Eghtesad B, Quintini C, Miller C, Yerian L, Klatte R. Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transpl. 2013;19:1304–1310. doi: 10.1002/lt.23729. [DOI] [PubMed] [Google Scholar]
- 17.Witowski JS, Pędziwiatr M, Major P, Budzyński A. Cost-effective, personalized, 3D-printed liver model for preoperative planning before laparoscopic liver hemihepatectomy for colorectal cancer metastases. Int J Comput Assist Radiol Surg. 2017;12:2047–2054. doi: 10.1007/s11548-017-1527-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madurska MJ, Poyade M, Eason D, Rea P, Watson AJM. Development of a patient-specific 3D-printed liver model for preoperative planning. Surg Innov. 2017;24:145–150. doi: 10.1177/1553350616689414. [DOI] [PubMed] [Google Scholar]
- 19.Watson RA. A low-cost surgical application of additive fabrication. J Surg Educ. 2014;71:14–17. doi: 10.1016/j.jsurg.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 20.Xiang N, Fang C, Fan Y, Yang J, Zeng N, Liu J, Zhu W. Application of liver three-dimensional printing in hepatectomy for complex massive hepatocarcinoma with rare variations of portal vein: preliminary experience. Int J Clin Exp Med. 2015;8:18873–11887. [PMC free article] [PubMed] [Google Scholar]
- 21.Mohr D. Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 Statement. Syst Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Witowski JS, Coles-Black J, Zuzak TZ, Pedziwiatr M, Chuen J, Major P, Budzyriski A. 3D printing in liver surgery: a systematic review. Telemed J E Health. 2017;23:943–947. doi: 10.1089/tmj.2017.0049. [DOI] [PubMed] [Google Scholar]
- 23.Soon DSC, Chae MP, Pilgrim CHC, Rozen WM, Spychal RT, Hunter-Smith DJ. 3D hepatic modelling for preoperative planning of hepatic resection: a systematic review. Ann Med Surg (Lond) 2016;10:1–7. doi: 10.1016/j.amsu.2016.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quintini C, Aucejo F, Hashimoto K, Zein N, Miller C. State of the art and future developments for surgical planning in LDLT. Curr Transpl Rep. 2014;1:35–42. doi: 10.1007/s40472-013-0008-z. [DOI] [Google Scholar]
- 25.Alkhouri N, Zein NN. Three-dimensional printing and pediatric liver disease. Curr Opin Pediatr. 2016;28:626–630. doi: 10.1097/MOP.0000000000000395. [DOI] [PubMed] [Google Scholar]
- 26.Oshiro Y, Ohkohchi N. Three-dimensional liver surgery simulation: computer-assisted surgical planning with three-dimensional simulation software and three-dimensional printing. Tissue Eng Part A. 2017;23:474–480. doi: 10.1089/ten.tea.2016.0528. [DOI] [PubMed] [Google Scholar]
- 27.Yao R, Xu G, Mao SS, Yang HY, Sang XT, Sun W, Mao YL. Three-dimensional printing: review of application in medicine and hepatic surgery. Cancer Biol Med. 2016;13:443–451. doi: 10.20892/j.issn.2095-3941.2016.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fang CH, Tao HS, Yang J, Fang ZS, Cai W, Liu J, Fan YH. Impact of three-dimensional reconstruction technique in the operation planning of centrally located hepatocellular carcinoma. J Am Coll Surg. 2015;220:28–37. doi: 10.1016/j.jamcollsurg.2014.09.023. [DOI] [PubMed] [Google Scholar]
- 29.Leng S, Yu L, Vrieze T, Kuhlmann J, Chen B, McCollough CH. Construction of realistic liver phantoms from patients images using 3D printer and its application in CT image quality assessment. Proc SPIE Int Soc Opt Eng 2015, 2015 [DOI] [PMC free article] [PubMed]
- 30.Baimakhanov Z, Soyama A, Takatsuki M, Hidaka M, Hirayama T, Kinoshita A, Natsuda K, Kuroki T, Eguchi S. Preoperative simulation with a 3-dimensional printed solid model for one-stop reconstruction of multiple hepatic veins during living donor liver transplantation. Liver Transpl. 2015;21:266–268. doi: 10.1002/lt.24019. [DOI] [PubMed] [Google Scholar]
- 31.Bucking TM, Hill E, Robertson JL, Maneas E, Plumb AA, Nikitichev DI. From medical imaging data to 3D printed anatomical models. Plos One. 2017;12:e0178540. doi: 10.1371/journal.pone.0178540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Choi YR, Kim JH, Park SJ, Hur BY, Han JK. Therapeutic response assessment using 3D ultrasound for hepatic metastasis from colorectal cancer: application of a personalized, 3D-printed tumor model using CT images. Plos One. 2017;12:e0182596. doi: 10.1371/journal.pone.0182596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Igami T, Nakamura Y, Hirose T, Ebata T, Yokoyama Y, Sugawara G, Mizuno T, Mori K, Nagino M. Application of a three-dimensional print of a liver in hepatectomy for small tumors invisible by intraoperative ultrasonography: Preliminary experience. World J Surg. 2014;38:3163–3166. doi: 10.1007/s00268-014-2740-7. [DOI] [PubMed] [Google Scholar]
- 34.Javan R, Herrin D, Tangestanipoor A. Understanding spatially complex segmental and branch anatomy using 3D printing: liver, lung, prostate, coronary arteries, and circle of willis. Acad Radiol. 2016;23:1183–1189. doi: 10.1016/j.acra.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 35.Javan R, Zeman M. A prototype educational model for hepatobiliary interventions: unveiling the role of graphic designers in medical 3D printing. J Digit Imaging. 2018;31:133–143. doi: 10.1007/s10278-017-0012-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kong X, Nie L, Zhang H, Wang Z, Ye Q, Tang L, Li J, Huang W. Do three-dimensional visualization and three-dimensional printing improve hepatic segment anatomy teaching? A randomized controlled study. J Surg Educ. 2016;73:264–269. doi: 10.1016/j.jsurg.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 37.Leng S, Chen B, Vrieze T, Kuhlman J, Yu L, Alexander A, Matsumoto J, Morris J, McCollough CH. Construction of realistic phantoms from patients images and a commercial three-dimensional printer. J Med Imag (Bellingham) 2016;3:033501. doi: 10.1117/1.JMI.3.3.033501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oshiro Y, Mitani J, Okada T, Ohkohchi N. A novel three-dimensional print of liver vessels and tumors in hepatectomy. Surg Today. 2017;47:521–524. doi: 10.1007/s00595-016-1383-8. [DOI] [PubMed] [Google Scholar]
- 39.Perica E, Sun Z. Patient-specific three-dimensional printing for pre-surgical planning in hepatocellular carcinoma treatment. Quant Imaging Med Surg. 2017;7:668–677. doi: 10.21037/qims.2017.11.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Soejima Y, Taguchi T, Sugimoto M, Hayashida M, Yoshizumi T, Ikegami T, Uchiyama H, Shirabe K, Maehara Y. Three-dimensional printing and biotexture modeling for preoperative simulation in living donor liver transplantation for small infants. Liver Transpl. 2016;22:1610–1614. doi: 10.1002/lt.24516. [DOI] [PubMed] [Google Scholar]
- 41.Souzaki R, Kinoshita Y, Ieiri S, Hayashida M, Koga Y, Shirabe K, Hara T, Maehara Y, Hashizume M, Taguchi T. Three-dimensional liver model based on preoperative CT images as a tool to assist in surgical planning for hepatoblastoma in a child. Pediatr Surg Int. 2015;31:593–596. doi: 10.1007/s00383-015-3709-9. [DOI] [PubMed] [Google Scholar]
- 42.Takagi K, Nanashima A, Abo T, Arai J, Matsuo N, Fukuda T, Nagayasu T. Three-dimensional printing model of liver for operative simulation in perihilar cholangiocarcinoma. Hepatogastroenterology. 2014;61:2315–1216. [PubMed] [Google Scholar]
- 43.Takao H, Amemiya S, Shibata E, Ohtomo K. Three-dimensional printing of hollow portal vein stenosis models: a feasibility study. J Vasc Interv Radiol. 2016;27:1755–1758. doi: 10.1016/j.jvir.2016.05.022. [DOI] [PubMed] [Google Scholar]
- 44.Crossingham JL, Jenkinson J, Woolridge N, Gallinger S, Tait GA, Moulton CA. Interpreting three-dimensional structures from two-dimensional images: a web-based interactive 3D teaching model of surgical liver anatomy. HPB (Oxford) 2009;11:523–528. doi: 10.1111/j.1477-2574.2009.00097.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hansen C, Wieferich J, Ritter F, Rieder C, Peitgen H-O. Illustrative visualization of 3D planning models for augmented reality in liver surgery. Int J Comput Assist Radiol Surg. 2010;5(2):133–141. doi: 10.1007/s11548-009-0365-3. [DOI] [PubMed] [Google Scholar]
- 46.Su L, Dong Q, Zhang H, Zhou X, Chen Y, Hao X, Li X. Clinical application of a three-dimensional imaging technique in infants and young children with complex liver tumours. Pediatr Surg Int. 2016;32(4):387–395. doi: 10.1007/s00383-016-3864-7. [DOI] [PubMed] [Google Scholar]
- 47.Matsumoto JS, Morris JM, Foley TA, Kuhlmann JL, Nesberg LE, Vrtiska TJ. Three-dimensional physical modeling: applications and experience at Mayo clinic. Radiographics. 2015;35:1989–2006. doi: 10.1148/rg.2015140260. [DOI] [PubMed] [Google Scholar]
- 48.Echegaray Sebastian, Bakr Shaimaa, Rubin Daniel L., Napel Sandy. Quantitative Image Feature Engine (QIFE): an Open-Source, Modular Engine for 3D Quantitative Feature Extraction from Volumetric Medical Images. Journal of Digital Imaging. 2017;31(4):403–414. doi: 10.1007/s10278-017-0019-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Presti GL, Carbone M, Ciriad D, Aramini D, Ferrari M, Ferrari V. Assessment of DICOM viewers capable of loading patient-specific 3D models obtained by different segmentation platforms in the operating room. J Digit Imaging. 2015;28:518–527. doi: 10.1007/s10278-015-9786-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bangerjee P, Hu M, Kannan R, Krishnaswamy S. A semi-automatic approach to improve the efficiency of medical imaging segmentation for haptic rendering. J Digit Imaging. 2017;30:519–527. doi: 10.1007/s10278-017-9985-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Park JS, Chung MS, Hwang SB, Lee YS, Har DH. Technical report on semiautomatic segmentation using the Adobe photoshop. J Digit Imaging. 2015;18:333–343. doi: 10.1007/s10278-005-6704-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mitsouras D, Liacouras P, Imanzadeh A, Giannopolous AA, Cai T, Kumamaru KK, George E, Wake N, Caterson EJ, Pomahac B, Ho VB, Grant GT, Rybicki FJ. Medical 3D printing for the radiologist. Radiographics. 2015;35:1965–1988. doi: 10.1148/rg.2015140320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lau Ivan, Sun Zhonghua. Three-dimensional printing in congenital heart disease: A systematic review. Journal of Medical Radiation Sciences. 2018;65(3):226–236. doi: 10.1002/jmrs.268. [DOI] [PMC free article] [PubMed] [Google Scholar]