Abstract
HIV-associated neurocognitive disorders (HAND) remain a substantial problem in the era of combination antiretroviral therapy. Neither the Mini Mental State Exam nor the HIV Dementia Scale is sufficiently sensitive for HAND. The Montreal Cognitive Assessment shows promise, but current data suggest that adding an additional test will be needed to improve sensitivity for the clinical setting. Patient reporting of symptoms is insensitive as most cases of HAND are asymptomatic. Examination of cerebrospinal fluid (CSF) is sometimes warranted in select patients to evaluate for CSF HIV RNA detectability. CSF escape of virus, when CSF HIV RNA is detectable but plasma HIV RNA is not, appears to be a relatively uncommon event in the clinical setting where the level of detectability for typical clinical assays is around 50 copies/mL. In cases of CSF escape, cognitive improvement has been linked to changes in antiretroviral regimens that are aimed at either overcoming antiretroviral resistance or improving central nervous system (CNS) penetration-effectiveness. Currently, for most patients with HAND in the absence of unusual features, there are insufficient data for a recommendation to routinely intensify therapy with a neurointensive antiretroviral regimen; however, there is considerable uncertainty given emerging data and variability in approach among experts in the field. This article summarizes a case-based presentation by Victor G. Valcour, MD, at the 14th Annual Clinical Conference for the Ryan White HIV/AIDS Program held in Tampa, Florida, in June 2011. The Clinical Conference is sponsored by the IAS–USA under the Health Resources and Services Administration (HRSA) contract number HHSH250200900010C.
A number of questions are frequently raised by HIV clinicians regarding the evaluation and follow-up of cognitive impairment. These questions include: How is screening best conducted? When is a lumbar puncture indicated? How should one balance the concerns for escape of virus in cerebrospinal fluid (CSF) with the understanding that more than 50% of patients will have cognitive impairment and that CSF escape appears to be a relatively uncommon event? How can one distinguish HIV-associated neurocognitive disorders (HAND) from neurodegenerative disorders, such as Alzheimer’s disease, in older HIV patients? What follows are some basics, illustrated by a case study, on how to approach HIV-infected patients with cognitive complaints in the clinical setting.
Typical Presentations of HAND
In the era before potent antiretroviral therapy, it was already apparent that HIV entered and replicated in the brain within days following infection. Widespread involvement of virus was evident at autopsy, with greater viral density in the deeper brain structures as opposed to cortical regions. This anatomy informs the clinical phenotype of HIV cognitive impairment in contrast to neurodegenerative diseases such as Alzheimer’s disease, where brain involvement early in disease typically results in more focal cortical deficits, such as that for encoding memory. The greater involvement of subcortical structures in HAND may be associated with clinical features such as slowing of processing speed; motor and psychomotor involvement; and executive, planning, or multitasking dysfunction. Behaviorally, there may be a greater impact on motivational drive, often recognized clinically as apathy.
HAND can be viewed as a neurobehavioral syndrome, affecting the 3 broad areas of cognitive, behavioral, and motor function. In the realm of cognition, problems can be seen with memory, concentration, mental processing speed, comprehension, or higher cognitive abilities. Behaviorally, one can observe apathy, depression, agitation, or in rare cases, mania. Motor dysfunction includes unsteady gait, poor coordination, abnormal tone, and tremor. A feature of HAND that is not typically seen with other dementia syndromes is the fluctuation in symptoms and testing performance that has been documented in several large series. Diagnostic transitions have been observed with serial testing, in which the performance of individuals (worse or better) varies longitudinally.1,2 In contrast to dementia syndromes such as Alzheimer’s disease, relentless progression is less common in HIV-infected subjects who are adequately treated with combination antiretroviral therapy. Such cases require more comprehensive evaluations that may need to consider contributing etiologies.
Confirming Cognitive Problems in the Clinical Setting: Limitations of Typical Bedside Screening Instruments
Dr Valcour described a hypothetical 58-year-old HIV-infected woman who was cared for by the same clinician for 10 years. She acquired HIV infection from injection drug use, and initially presented with Pneumocystis jiroveci pneumonia and a CD4+ cell count of 5/μL. Since diagnosis, she has been continuously treated with zidovudine, lamivudine, and efavirenz and now has a CD4+ cell count of 580/μL with a plasma HIV RNA level that has been undetectable for 10 years. She denies illicit drug use since the time of her HIV diagnosis.
The patient now complains of subtle “memory problems” affecting her work. Although she feels her memory is OK, she is slow to recall items and has made errors while multitasking. She remarks on new interpersonal conflicts that have been brought to her attention by her supervisor. Overall, the symptoms have not bothered her, as she has learned to compensate for the inefficiency, but now she fears she may lose her job. The symptoms have been present for approximately 5 years, and do not seem to be worsening.
Should this patient be screened for cognitive impairment and if so, which instrument should be used: the Mini Mental State Exam (MMSE), the HIV Dementia Scale (HDS), the clock-drawing test, or is the report of symptoms sufficient to make a diagnosis without confirmation through cognitive testing?
First, consider the issue of screening HIV-infected patients for cognitive impairment in the clinical setting. A more comprehensive review of this topic is available elsewhere.3 Briefly, the MMSE is in the diagnostic toolbox of most clinicians. Its familiarity, rapidity of administration, and ease of interpretation are all compelling factors. Unfortunately, it has poor sensitivity and specificity for HAND. The instrument is better utilized for cortical dementia syndromes, such as Alzheimer's disease, because it is heavily weighted on factors impacted in such syndromes. The first 10 items of the MMSE, for example, address orientation, a factor that is typically preserved in most HAND cases with the exception of advanced cases.
Areas that would be more important to test include domains of attention and working memory, but these are poorly represented in the MMSE. Published studies have shown that the MMSE is poor at detection of HAND.4,5 In Dr Valcour's preliminary data from the UCSF HIV Over 60 Cohort (HIV-infected patients older than 60 years), the mean MMSE score was 29 in those without cognitive impairment compared with a mean of 28 in those with impairment.
The HDS was designed to identify HIV-associated dementia (HAD), a condition that is now the least common HAND diagnosis. Most HAND cases are now classified as asymptomatic neurocognitive impairment (ANI) or mild neurocognitive disorder (MND). The HDS contains items testing registration, memory recall, psychomotor speed, and attention, and works well for detecting HAD, but it is insensitive to more mild disease, which now encompasses about 95% of HAND. Removing the antisaccadic eye movement test to create the modified and international versions of the HDS further decreased sensitivity.6 Numerous studies have shown that HDS is poor at differentiating HAND, with 1 study showing that among individuals wishing to return to work, its sensitivity was 39% compared with neuropsycho-logic testing.7-9
The clock-drawing test is part of the Montreal Cognitive Assessment (MoCA) (http://www.mocatest.org/), an instrument that shows some promise in identifying HAND (Figure 1). There are no published reports on using the clock-drawing task alone, but it is likely to be too limited for broad utility as a screening instrument for HAND. In contrast, the MoCA is more comprehensive and designed to capture impairment caused by cortical and subcortical processes. It includes several tests likely to be sensitive for HAND, including those for attention, concentration, working memory, executive functioning, and reasoning. The instrument includes a trail-making test (follow the dots alternating from letter to number), which tests executive functioning, and the clock-drawing test, which tests executive functioning and visual and spatial skills. The memory testing includes several trials that permit the tester to give cues, including category and multiple-choice cues. It is characteristic of HAND patients and patients with other subcortical dementias to have impaired spontaneous recall, but for their recall to be improved with cues. This is less typical of more cortical dementia syndromes such as Alzheimer's disease.
Figure 1.
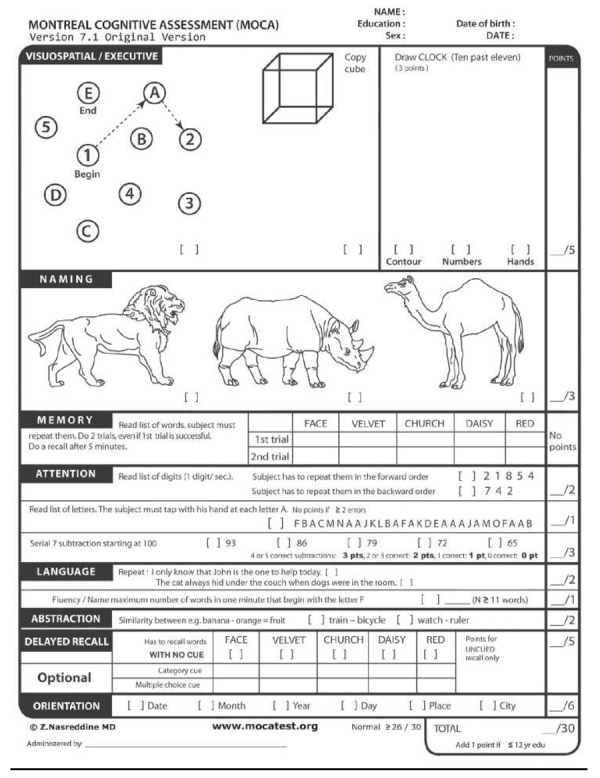
The Montreal Cognitive Assessment (MoCA). Test reproduced with permission from copyright owner Ziad Nasreddine, MD.
In a study recently reported by Clifford and colleagues, the MoCA had a sensitivity of 59% and specificity of 81% for identifying cognitive impairment using a score cutpoint of 26.10 Sensitivity improved to 83% with a cutpoint of 28, but such a change will decrease specificity. Accuracy may be higher in symptomatic patients or with the addition of another test. Thus, although the accuracy of the MoCA in its current form is not optimal for detecting HAND, the test may yet prove useful in the clinic as a component of a short battery.
HAND cannot be detected on the basis of symptoms alone. In the CHARTER (CNS [central nervous system] HIV Antiretroviral Therapy Effects Research) study, a study of community-dwelling adult HIV-infected subjects, more than two-thirds of subjects found to have cognitive impairment were asymptomatic, and thus deemed to have ANI.11 The term "asymptomatic" may be misleading, because it is often based on self-report and likely to be less reliable among subjects with cognitive impairment. A study by Heaton and colleagues demonstrated that neu-ropsychologic impairment was associated with functional impairment irrespective of whether patients reported symptoms.12 Similarly, preliminary
data in the UCSF HIV Over 60 Cohort suggest that both ANI and MND subjects perform worse than controls on objective tests of function (data not published).
In summary, among the bedside cognitive tests, the MMSE should not be used for HAND and the HDS should not be used alone, unless one seeks to identify only the most severe form of HAND (ie, dementia). The MoCA shows promise and has empiric benefit compared with the MMSE and HDS. For clinical use, the MoCA is readily available at no cost and instructions are provided (http://www.mocatest.org/).13 The test has been translated into many languages, although caution should be executed regarding cultural validity in these settings. It takes approximately 8 minutes to administer. Relying on symptoms or patient reports of functional change to identify HAND will result in missing most cases.
Workup for HAND
In the case scenario, the subject was referred for formal neuropsycholog-ic testing, which revealed deficits in working memory and attention. Her memory testing demonstrated inefficiency due to poor learning and attention. Her depression screen was elevated. She returns for a workup in your office.
A typical workup for HAND should include some basic aspects to search for factors that may be modifiable or inform alternative etiologies. This should include:
Careful neurologic examination and careful assessment for signs of opportunistic infection. This would be intensified in settings of low CD4+ cell count or in patients not on antiretroviral therapy.
Review of histories for antiretro viral therapy, CD4+ cell counts, and plasma viral load levels with emphasis on adherence.
Review of medications, pre scribed and otherwise, to consid er adverse effects that can impact cognition.
Evaluation for depression.
Assessment of key comorbidities, including liver, renal, cardiac, and cerebrovascular conditions.
Evaluation for other factors that can impact cognition, including syphilis, vitamin B12 levels (with consideration for homocysteine and methylmalonic acid levels, particularly when white matter le sions are noted), thyroid function, sleep apnea, and hepatitis, among other potential targeted investiga tions.
Brain imaging.
In our case scenario, results of the patient's neurologic examination demonstrated some inattention, neuropathy, and mild increased tone in extremities. A brain magnetic resonance imaging (MRI) was read as normal. A comprehensive blood workup that included thyroid function, vitamin B12 level, serum rapid plasma reagin (RPR), and renal and liver function tests yielded normal results.
The factors influencing the approach to this patient's case thus far include the following: she had a low CD4+ cell count nadir, increasing the risk for HAND. She had a history of injection drug use, which, depending on use pattern and coexisting factors, such as loss of consciousness or head injuries, could increase risk for cognitive impairment. She has had an undetect-able plasma viral load for a decade and her CD4+ cell count is now in the normal range. A high CD4+ cell count and consistently controlled virus are linked to a lower risk for HAND. The normal CD4+ count suggests that opportunistic infection is unlikely.
The duration of symptoms is 5 years and appears relatively stable. The duration suggests a more indolent course common with HAND and the relative stability over 5 years is less typical of neurodegenerative disorders such as Alzheimer's disease. However, there should be some question about whether her condition has become worse recently, as the patient has identified new associated problems. Symptom reporting and testing indicate motor, behavioral, and cognitive problems that are more typical of HAND. Her laboratory workup and MRI do not suggest an alternative etiology.
In this case, the subject was diagnosed with MND in HIV and treatment for depression was initiated. The next consideration is whether patients like this one, with cognitive impairment, should be referred to a specialist for further workup and possible lumbar puncture for CSF evaluation. There is great variability in how such cases are managed. There are a number of factors in this patient that suggest she can likely be managed without immediate evaluation of CSF. The course of her cognitive syndrome is 5 years. More rapid progression should be evaluated aggressively, but in cases with longstanding impairment that are relatively stable, there are insufficient data to suggest that CSF evaluation will meaningfully impact treatment approaches. This patient is already on effective antiretroviral treatment with a normal CD4+ cell count, suggesting that CSF evaluation for opportunistic infection is not likely to be helpful. She is also RPR-negative. Most patients seen in Dr Valcour’s referral clinic have profiles similar to this patient’s, in which CSF evaluation will probably not yield information that will change management. But there are no clear guidelines around referral for CSF evaluation, and the decision should be based on the combination of findings and clinical judgment based on the presence of worrisome features.
The algorithm for referral and lumbar puncture would be more aggressive in cases of subacute or acute cognitive impairment, among individuals not on antiretroviral therapy and not responding to initiation of treatment, and in cases with features not typical of HAND. However, focused studies are lacking and this approach is based on clinical judgment based on the presence of worrisome features. Initiation of antiretroviral therapy is indicated in subjects not on treatment who are diagnosed with HAND. Among individuals who do not improve after 3 to 6 months of antiretroviral therapy, evaluation of CSF may be useful to ensure adequate treatment of this compartment by ensuring that CSF HIV RNA level is undetectable. This approach is not applicable, however, for patients with a more chronic form of cognitive impairment, currently a common finding in the clinical setting. In such cases, there are insufficient published data to recommend a uniform approach, with the only clinical study not providing adequate support for a global recommendation.14
There are a number of potential benefits to CSF evaluation in patients with cognitive impairment. It can be used (1) in cases with high suspicion for unusual causes of cognitive impairment, including infection, that require further investigation; (2) to determine if CSF immune activation is present (typically used in research settings); and (3) to evaluate for HIV CSF escape, a relatively uncommon phenomenon in the clinical setting where the sensitivity of typical assays is to around 50 copies/mL. If a patient is sent for lumbar puncture, one should consider CSF for evaluation for virus (quantitative HIV RNA in CSF), white blood cell (WBC) count, and other markers of inflammation such as oligoclonal bands, an IgG index, and protein level. More focused evaluation for infections would be done on a case-by-case basis.
It may be helpful to review the literature on CSF escape, which has been documented in several case reports. In addition, there is a small literature on subjects with HIV RNA levels below 50 copies/mL in both CSF and plasma, but with low-level detection that is higher in CSF than in plasma. This latter finding is beyond the scope of clinical care at the current time and a subject of ongoing research. One case series presented 3 patients with meningoencephalitis due to CSF escape, each of whom improved with altering antiretroviral therapy components.15
A European report confirmed 11 cases from 2 university infectious diseases clinics caring for about 6000 HIV-infected patients annually (Table 1). Although this study was not designed to determine frequency of CSF escape, the identification of 11 cases in such a large setting is somewhat reassuring that clinically relevant CSF escape is likely to be uncommon.16 Most of these patients had neurologic signs or symptoms such as cerebellar disorders or headache rather than just the cognitive symptoms of the type observed in the case described here. The patients in this case series improved when antiretroviral therapy was changed based on genotypic testing or to improve drug CNS penetration-effectiveness.
Table 1.
European Case Series of Patients with HIV Cerebrospinal Fluid (CSF) Escape
| Case number | Age (years) | CD4+ Count (cells/μL) | Time Level (months) | with HIV RNA < 50 copies/mL | Neurologic Symptoms | CSF HIV RNA Level (copies/mL) | Plasma HIV RNA Level (copies/mL) |
|---|---|---|---|---|---|---|---|
| 1 | 50 | 592 | 36 | Persistent headache | 12,885 | 147 | |
| 2 | 49 | 190 | 11 | Memory cerebellar disorder, ataxia | 845 | < 50 | |
| 3 | 43 | 400 | 18 | Cerebellar cerebellar ataxia dysarthria, | 1190 | < 50 | |
| 4 | 50 | 432 | 68 | Tactile allodynia | 870 | 78 | |
| 5 | 36 | 107 | 75 | Glasgow Coma Score of 3 | 5035 | < 50 | |
| 6 | 47 | 631 | 64 | Persistent headache | 580 | < 50 | |
| 7 | 44 | 544 | 14 | Memory ataxia, pyramidal disorder, syndrome cerebellar | 558 | < 50 | |
| 8 | 53 | 360 | 12 | Lower hypoesthesia limb dysesthesia and | 1023 | < 50 | |
| 9 | 68 | 147 | 12 | Memory limb dysesthesia disorder, left lower | 586 | < 50 | |
| 10 | 68 | 534 | 18 | Temporospatial tion, cerebellar disorienta- ataxia | 880 | < 50 | |
| 11 | 55 | 593 | 10 | Memory dysarthria disorder, cerebellar | 6999 | 483 | |
Adapted from Canestri et al.16
In summary, there are a number of situations in which lumbar puncture and evaluation of CSF may be advisable. Some examples are acute or subacute presentations, rapid progression of impairment, new neurologic findings, and inability to exclude other infectious etiologies (eg, syphilis) based on serum tests, history, and imaging. In some settings, a CSF evaluation may also be considered for patients with impairment in whom a change in antiretroviral therapy is being considered or in whom a change in therapy has been made in order to monitor response in the CSF; however, a universal recommendation for these reasons cannot be supported with the existing literature.
Changing Antiretroviral Therapy to Improve CNS-Penetration Effectiveness
In our case example, the patient was receiving zidovudine, lamivudine, and efavirenz. Using published data, this patient would be considered to have a moderate to high CNS-penetration effectiveness (CPE) score. According to a CNS penetration rating for antiretroviral drugs developed by Letendre and colleagues, zidovudine and efavirenz have higher levels of penetration-effectiveness and lamivudine has moderate penetration effectiveness.17,18 Although switching from lamivudine to emtricitabine (a relatively minimal change in terms of therapy, but adding to the pill burden and possibly impacting adherence) can improve the CPE, there are no data to suggest this will improve outcomes, with one study suggesting such an empiric intensification choice will not be beneficial.14 No data are available to guide an empiric change of therapy in a case such as the one described here. The decision to change therapy can create unease clinically when a patient is on an antiretroviral regimen with overall poor CPE, paired with the knowledge that higher CPE has been linked to lower CSF virus levels. In such cases, Dr Valcour sometimes considers assuring that CSF virus is below detectable limits. Changing antiretroviral therapy does carry risks, which may outweigh uncertain benefits in patients not clearly in need of a change. These risks could include new adverse effects that can impact cognition negatively, exposure to more antiretroviral medications that could impact resistance profiles for future options, and change in pill burden. Consequently, the approach to patients with HAND must be individualized and more clinical data from randomized studies are urgently needed.
Summary
Cognitive impairment remains a substantial problem in the era of antiretroviral therapy, occurring in about one-half of community-dwelling HIV-infected adults. Most patients with HAND identified in research settings are categorized as having ANI, likely due, at least in part, to difficulty in obtaining accurate reports of functional limitations from impaired patients. Current screening tools have large limitations. Neither the MMSE nor HDS is useful for distinguishing HAND, however, the MoCA test may have promise. Used alone, the performance characteristics may not be sufficient for broad use, but studies are underway aimed at determining if adding additional tests may improve performance.
There are many things that can be done in the primary care setting to initiate a workup for cognitive impairment, although referral to specialized centers will be required in some cases. The literature is not informative regarding empiric changes in antiretroviral therapy to better target the CNS in subjects with HAND. In special cases, including those involving CSF HIV escape, change in medications has been found to be of benefit. A high index of suspicion in unusual presentations is warranted, but recommendations for CSF evaluation in all cases of HAND may be premature.
References
- 1.Antinori A, Arendt G, Becker JT, et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology. 2007;69:1789-1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McArthur JC, Haughey N, Gartner S, et al. Human immunodeficiency virus-associated dementia: an evolving disease. J Neurovirol. 2003;9:205-221. [DOI] [PubMed] [Google Scholar]
- 3.Valcour V, Paul R, Chiao S, Wendelken LA, Miller B. Screening for cognitive impairment in human immunodeficiency virus. Clin Infect Dis. 2011;53:836-842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ganasen KA, Fincham D, Smit J, Seedat S, Stein D. Utility of the HIV Dementia Scale (HDS) in identifying HIV dementia in a South African sample. J Neurol Sci. 2008;269:62-64. [DOI] [PubMed] [Google Scholar]
- 5.Skinner S, Adewale AJ, DeBlock L, Gill MJ, Power C. Neurocognitive screening tools in HIV/AIDS: comparative performance among patients exposed to antiretroviral therapy. HIV Med. 2009;10:246-252. [DOI] [PubMed] [Google Scholar]
- 6.Davis HF, Skolasky RL Jr., Selnes OA, Burgess DM, McArthur JC. Assessing HIV-associated dementia: modified HIV dementia scale versus the Grooved Pegboard. AIDS Read. 2002;12:29-31, 38. [PubMed] [Google Scholar]
- 7.Smith CA, vanGorp WG, Ryan ER, Ferrando SJ, Rabkin J. Screening subtle HIV-related cognitive dysfunction: the clinical utility of the HIV dementia scale. JAIDS. 2003;33:116-118. [DOI] [PubMed] [Google Scholar]
- 8.Morgan EE, Woods SP, Scott JC, et al. Predictive validity of demographically adjusted normative standards for the HIV Dementia Scale. J Clin Exp Neuropsychol. 2008;30:83-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Waldrop-Valverde D, Nehra R, Sharma S, et al. Education effects on the International HIV Dementia Scale. J Neurovirol. 2010;16:264-267. [DOI] [PubMed] [Google Scholar]
- 10.Overton ET, Ances B, Grubb J, et al. Novel screening tools for HIV-associated neurocognitive disorders. [Abstract 401.] 18th Conference on Retroviruses and Infections (CROI). February 27-March 2, 2011; Boston, MA. [Google Scholar]
- 11.Heaton RK, Clifford DB, Franklin DR Jr., et al. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology. 2010;75:2087-2096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heaton RK, Marcotte TD, Mindt MR, et al. The impact of HIV-associated neuropsychological impairment on everyday functioning. J Int Neuropsychol Soc. 2004;10:317-331. [DOI] [PubMed] [Google Scholar]
- 13.Nasreddine Z. The Montreal Cognitive Assessment. http://www.mocatest.org. Accessed October 19, 2011.
- 14.Marra CM, Zhao Y, Clifford DB, et al. Impact of combination antiretroviral therapy on cerebrospinal fluid HIV RNA and neurocognitive performance. AIDS. 2009;23:1359-1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wendel KA, McArthur JC. Acute meningoencephalitis in chronic human immunodeficiency virus (HIV) infection: putative central nervous system escape of HIV replication. Clin Infect Dis. 2003;37:1107-1111. [DOI] [PubMed] [Google Scholar]
- 16.Canestri A, Lescure FX, Jaureguiberry S, et al. Discordance between cerebral spinal fluid and plasma HIV replication in patients with neurological symptoms who are receiving suppressive antiretroviral therapy. Clin Infect Dis. 2010;50:773778. [DOI] [PubMed] [Google Scholar]
- 17.Letendre S, FitzSimons C, Ellis R, et al. Correlates of CSF viral loads in 1221 volunteers of the CHARTER cohort. [Abstract 172]. 17th Conference on Retroviruses and Infections (CROI). February 16-19, 2010; San Francisco, CA. [Google Scholar]
- 18.Letendre S. Central nervous system complications in HIV disease: HIV-associated neurocognitive disorder. Top Antivir Med. 2011;19:137-142. [PMC free article] [PubMed] [Google Scholar]


