Abstract
A recent outbreak of HIV infection centered in the rural town of Austin in Scott County, Indiana, was associated with widespread injection drug use and a socioeconomically depressed population. Control of the outbreak required coordinated efforts by state, federal, local, and academic institutions to implement and maintain on-site programs and services that included contact tracing, HIV and hepatitis C virus testing, insurance enrollment, syringe exchange, rehabilitation services, care coordination, preexposure prophylaxis, and HIV treatment. This article summarizes a presentation by Diane M. Janowicz, MD, at the IAS–USA continuing education program, Improving the Management of HIV Disease, held in Los Angeles, California, in April 2016.
Keywords: HIV, Indiana outbreak, injection drug use, contact tracing, syringe exchange, HIV transmission
Many clinicians and researchers in the field of HIV medicine are aware of the outbreak of HIV infection that occurred in the rural town of Austin in Scott County, Indiana. It is fortunate that, to date, this outbreak has not been a harbinger of future outbreaks as many had predicted. For now, it is a cautionary tale, given the epidemic of injection drug use occurring in the United States today.
The Evolution and Characteristics of the Indiana Outbreak
At the end of 2014, just as the HIV outbreak in Indiana was beginning, an estimated 12,500 people were living with HIV/AIDS in the state, the majority of whom resided in urban areas, including the northwest part of the state (adjacent to Chicago) and Indianapolis (in the central part of the state). The outbreak occurred in Scott County, a small rural county approximately 80 miles southeast of Indianapolis. Over the prior 10 years, only 5 persons in Scott County were diagnosed with HIV infection. The epicenter of the outbreak was Austin, a small town with a population of approximately 4200. The town has a 10% unemployment rate, with 19% of the population living below the federal poverty line and 21% who did not graduate from high school. Scott County ranks last in life expectancy out of 92 counties in Indiana.
It is estimated that there were more than 500 syringe-sharing partners in Scott County as of 2015. Injection practices were multigenerational and injection equipment was commonly shared. Individuals diagnosed with HIV infection during the outbreak had an average of 9 high-risk syringe-sharing, sex, or social partners who needed to be tested for infection. The drug most commonly used was oxymorphone, in a reformulation available since 2012, which was crushed and injected. Oxymorphone produces a fixed but short-lived high, and individuals may inject the substance as many as 20 times per day.
The outbreak was first identified in December 2014, when a physician in a town neighboring Austin observed within a short time frame that 2 individuals were HIV seropositive on screening. Another individual was soon diagnosed with HIV infection, and an astute disease intervention specialist was able to connect these cases with an additional 8 infected contacts by January 23, 2015. The Centers for Disease Control and Prevention (CDC) was alerted in February 2015 by the Indiana State Department of Health, and in March a large number of disease intervention specialists were deployed door to door to trace the contacts who had so far been identified, in order to offer HIV testing. A public health emergency was declared on March 26, 2015, by which date there were 55 confirmed cases and 13 preliminary cases of HIV infection (all subsequently confirmed). The numbers of HIV diagnoses per week are show in the Figure.
By the end of the public health emergency order in June 2015, 170 individuals had been diagnosed with HIV infection. A total of 444 of 513 contacts had been located and offered HIV testing during the emergency order, and point-of-care rapid testing and a simultaneous blood draw for syphilis and hepatitis C virus (HCV) infection testing were provided. The overall rate of positive HIV test results among tested contacts in Scott County was 38%. Surveillance of high-risk individuals has continued, and by April 2016 there were 188 confirmed cases of HIV infection. Based on the estimate that 80% of the people diagnosed with HIV infection lived in Austin, the HIV prevalence rate in that town would be nearly 5%. The HIV-infected individuals had a median age of 34 years (range, 18-60 years), 58% were men, 100% were of white race, 92% (160/174) had HCV coinfection, and 95% had an annual income of less than $10,000; very few had private health insurance, with all others being enrolled in the expanded Indiana Medicaid program.
Phylogenetic analysis of HIV polymerase sequences from the first 57 samples, performed by Galang and colleagues from the CDC, showed approximately 98% identity.1,2 Subsequent analysis of 157 isolates by these investigators showed 98.7% identity, confirming that it was the introduction of a single case of HIV infection into this large, tight network of persons who inject drugs that precipitated this outbreak.3 Avidity testing indicated that all of the initially identified HIV infections had occurred within the previous 6 months, consistent with clinical and laboratory data from the first 73 individuals seen in the HIV clinic. Many individuals reported symptoms consistent with acute HIV infection in the past 1 to 2 months prior to being evaluated in the clinic, and the elevated average CD4+ cell count (approximately 650/μL) and plasma HIV RNA level (approximately 272,000 copies/mL) were consistent with early infection.
Figure 1.
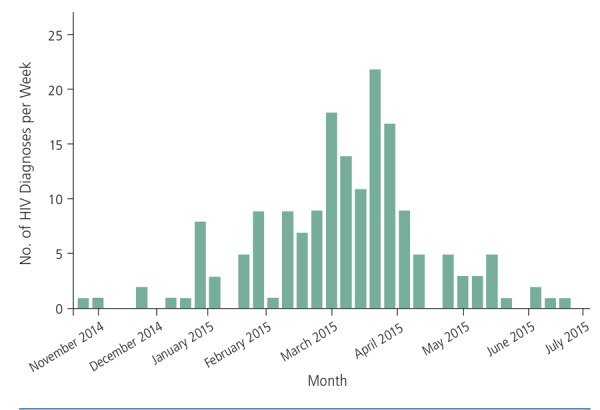
HIV diagnoses per week from November 2014 through July 2015 in Scott County, Indiana. Additional cases have been diagnosed since then. Adapted with permission from Brooks.6
Containing the Outbreak
Many services were initiated and maintained to contain the HIV outbreak in Indiana, including community-wide surveillance, contact tracing and door-to-door testing, targeting of high-risk populations, and outreach programs for transient populations. The county jail system implemented universal HIV screening at the start of the epidemic, which was instrumental in engaging otherwise difficult-to-reach individuals. Truck drivers working with the local canning industry who might be exposed through needle sharing or contact with sex workers were tested in an attempt to prevent the spread of HIV infection beyond county borders. Addiction treatment and harm-reduction services, including a syringe-exchange program and a program to administer preexposure prophylaxis (PrEP) were set up. No on-site, permanent addiction treatment services existed in Austin prior to the outbreak. Further, an HIV treatment program was implemented.
Setting up these services was a multipronged effort coordinated by the Indiana State Department of Health, involving other state partners, federal partners (eg, the CDC, the Substance Abuse and Mental Health Services Administration, and the Health Resources and Services Administration), academic partners (eg, the Indiana University Schools of Medicine and Public Health), and local partners (eg, faith-based organizations).
The effort allowed for construction of what became known as the “One-Stop Shop,” located in a warehouse building in which the Community Outreach Center was established. The services offered at this site included HIV and HCV testing, vital records, drivers’ license and state ID services, insurance enrollment, immunizations, rehabilitation and mental health services, care coordination, the Department of Workforce Development, and a syringe-exchange program. Individuals were offered free transportation to the site, which was open 7 days per week with extended evening hours. Participants in the syringe-exchange program were issued unique ID cards and could complete exchanges weekly, during which they received sterile syringes, a wound kit, and referrals to health and substance use services. More than 28,000 needles were dispensed.4 The syringe-exchange program also featured a mobile unit, comprising 2 nurses tasked to drive through neighborhoods and offer clean syringes. In a study among the first 100 participants in the syringe-exchange program, the proportion who shared syringes decreased from 34% to 5% over 3 months, with the median frequency of reuse declining from 4 times to 1 time; the proportion who shared syringes to divide drugs dropped from 38% to 10%; and the proportion who shared other injection equipment dropped from 44% to 11%.5 A key to the success of the syringe-exchange program was the involvement of the community and of local law enforcement early in the process.
Rehabilitation services offered included behavioral and drug rehabilitation and mental health services, including inpatient and outpatient services. Outpatient services are now available at a permanent site in Austin in a location that adjoins areas with the highest incidence of drug use. Additional services implemented during the emergency order included medication-assisted therapy (eg, increased access to naloxone and training programs for buprenorphine and naltrexone prescribing).
During HIV testing, HIV-seronegative persons were informed about the needle-exchange program, referred for behavioral health services, and encouraged to undergo repeat HIV testing based on ongoing exposure risks. Individuals found to be HIV infected began care coordination in the field and were referred for antiretroviral therapy.
The Clinic
Before the HIV outbreak in Austin, the nearest provider offering HIV care, a Ryan White HIV/AIDS Program–funded clinic, was 20 miles away. As the scope of the outbreak became apparent, the Indiana State Department of Health requested assistance from the Indiana University School of Medicine. Within 6 days, the Indiana University School of Medicine had set up a free clinic staffed with 2 infectious disease specialists in a borrowed space to provide HIV testing, treatment, education, and PrEP.
Collaboration with local health care practitioners provided invaluable community-specific knowledge that facilitated locating difficult-to-find individuals, follow-up, and identifying individuals’ distinct needs. Local practitioners adopted unique roles in care, as not all wished to be involved in direct HIV treatment, instead opting to focus on testing, counseling, or behavioral or mental health rehabilitation programs. Through such collaboration, an effective paradigm for local treatment and care was established.
In the HIV clinic, in the absence of an electronic medical record system, paper intake forms were developed to obtain comprehensive medical histories. HIV treatment was prioritized and other aspects of care, such as pneumococcal vaccination and treatment of other medical issues, were staggered; the primary goals were to initiate antiretroviral treatment for as many HIV-infected individuals as possible as quickly as possible in order to reduce risk of continued HIV transmission. Educational materials were designed specifically for each visit, with emphasis on consistent messaging regarding treatment for all patients. Efforts to educate local pharmacists were also undertaken to ensure that they were knowledgeable with regard to antiretroviral treatment and associated adverse effects that might threaten adherence.
At the clinic, individuals underwent insurance enrollment, basic laboratory testing, and physician assessment and counseling. Individuals with wild-type HIV genotypes and normal serum creatinine levels were prescribed 1 of 2 regimens: abacavir/lamivudine/dolutegravir (slash indicates a coformulation) for those who tested negative for the HLA-B*5701 allele or tenofovir/emtricitabine plus dolutegravir for those who tested positive for the HLA-B*5701 allele or were coinfected with hepatitis B virus. These regimens were selected for use on the basis of their tolerability and efficacy and to reduce the chances of drug-drug interactions with oxymorphone, medication-assisted treatment, and anti-HCV therapies. Individuals were asked to return to the clinic in 2 weeks to assess adherence and adverse effects and to address any barriers to treatment or ongoing care.
Prominent themes that emerged during the effort to curtail the HIV outbreak and link infected individuals to care included the need for a wide range of knowledge (including local knowledge about the residents and community) and the need to address stigma, ensure privacy, and emphasize longterm care. Every effort was made to provide a welcoming, nonjudgmental, and respectful environment for individuals to access HIV care, and this was instrumental in the success of the clinic and related programs. Word of mouth was important in bringing HIV-infected individuals into the clinic. Coordination with the jail system to provide treatment, evaluation, and follow-up was also an important component of the community interventions; at any given time, an estimated 10% to 20% of the HIV-infected population in Austin is in short-term incarceration.
Continuity of care remains challenging. At the end of 2015, among 176 individuals who were eligible for HIV treatment, 86% had been engaged in care, 74% had undergone care coordination, 59% had been prescribed antiretroviral therapy, and 32% had achieved virologic suppression. As of April 2016, including incarcerated individuals receiving directly observed therapy, 52% of HIV-infected individuals had achieved virologic suppression. To date, cases of transmission are still being observed, indicating the need for amplification of harm-reduction measures. These efforts include an emphasis on increasing the availability of PrEP and improving uptake of PrEP in the community, which has been suboptimal thus far.
Lessons Learned
Community and practitioner awareness of the realities of injection drug use and HIV infection within the community is essential. Efforts of community programs and health care practitioners are crucial to engagement and retention in multidisciplinary HIV care. Treatment as prevention is fundamental to reducing HIV transmission. Program sustainability at the local level is vital and requires commitment and planning.
The battle against the HIV outbreak in Indiana is ongoing. Not all HIV-infected individuals have been engaged in or retained in care; therefore, not all HIV-infected individuals have achieved virologic suppression. Ongoing efforts include coordination with the local jail system and inpatient and outpatient rehabilitation services. It remains a constant challenge to obtain resources for the local efforts and services necessary for a sustainable HIV care infrastructure.
References
- 1.Galang RR, Gentry J, Peters PJ et al. HIV-1 and HCV molecular epidemiology of a large community outbreak of HIV-1 infection linked to injection drug use of oxymorphone-Indiana, 2015. IAS Conference on HIV Pathogenesis, Treatment, and Prevention July 19-22, 2015; Vancouver, Canada. [Google Scholar]
- 2.Campbell EM, Galang RR, Heneine W, et al. Infer and characterize a transmission network in an opioid-driven HIV-1 outbreak. Top Antivir Med. 2016;24(e-1):84-85. [Google Scholar]
- 3.Peters PJ, Pontones P, Hoover KW, et al. HIV infection linked to injection use of oxymorphone in Indiana, 2014–2015. N Engl J Med. 2016;375:229-239 [DOI] [PubMed] [Google Scholar]
- 4.Indiana State Department of Health. State health officials discuss long term planning process for HIV outbreak response and transition. http://www.in.gov/isdh/files/June_19_State_Health_Officials_Discuss_Long_Term_Planning_Process_for_HIV_Outbreak_Response_and_Transition_.pdf. Accessed on August 1, 2016.
- 5.Patel MR, Combs B, Hall P et al. Reduction in injection risk behaviors after institution of an emergency syringe exchange program during an HIV outbreak among persons who inject drugs, Indiana 2015. ID Week. October 7-11, 2015; San Diego, California. [Google Scholar]
- 6.Brooks JT. The evolving epidemiology of HIV infection in persons who inject drugs: Indiana 2015. [CROI Abstract 132]. In Special Issue: Abstracts From the 2016 Conference on Retroviruses and Opportunistic Infections. Top Antivir Med. 2016;24(e-1):51. [Google Scholar]


