Abstract
In the era of antiretroviral therapy, HIV infection has become a chronic illness with associated multimorbidity, and practitioners are faced with an emerging population of HIV-infected patients with evolving needs for advance care planning (ACP), defined as communication between individuals and their proxies to plan for future health care decisions. This article provides a review of original research studies on ACP in HIV-infected adults in the era of antiretroviral therapy (1996-present) from PubMed, EMBASE, and PsycINFO. Eleven studies conducted between 1996 and 2015 met the selection criteria, with study sizes ranging from 9 to 2864 participants. Most studies consisted of white men in outpatient settings and had poorly defined definitions of ACP. Prevalence of ACP was variable (36%-54% had end-of-life communication, 8%-47% had advance directives). Lack of ACP was most commonly associated with low income, followed by lower severity of illness, low education level, black or Hispanic race, female sex, younger age, injection drug use, and social isolation. Practitioners reported limited time or energy and inadequate preparation or training as barriers to ACP. Existing literature on ACP in the era of antiretroviral therapy is limited, but shows that ACP prevalence in HIV-infected individuals is variable depending on socioeconomic factors, severity of illness, and practitioner resources and training. More research is needed to increase ACP among HIV-infected individuals.
Keywords: HIV, AIDS, advance care planning, advance directive, end-of-life care
Since the advent of effective antiretroviral therapy in 1996,1,2 HIV-related mortality has declined substantially, and HIV has transitioned from a rapidly fatal illness to a chronic, manageable disease. The gain in life expectancy from antiretroviral therapy has resulted in an increasing proportion of older HIV-infected adults. By 2020, more than 50% of HIV-infected individuals in the United States will be older than 50 years.3
As HIV-infected individuals grow older, they are at increased risk of multimorbidity, defined as the development of multiple chronic conditions that interact to worsen mortality and functional outcomes.4,5 As life expectancy among HIV-infected individuals becomes more influenced by multimorbid conditions instead of HIV infection in the era of antiretroviral therapy, multimorbidity has important ramifications on end-of-life experiences and advance care planning (ACP) in HIV-infected individuals.6
ACP is defined as a process of communication between individuals and their health care agents to understand, reflect on, discuss, and plan for a time when they may not be able to make their own health care decisions, in order to help maximize patient autonomy.7 ACP may take many written forms, including advance directive, designation of health care proxies, living will, physician orders for life-sustaining treatment (POLST),8 and documentation in electronic palliative care coordination systems,9 among others.
As HIV evolved from a rapidly fatal illness to a chronic disease with early multimorbidity, the content and scope of ACP for HIV-infected individuals has also changed. The focus has shifted from living wills designed to address the circumstances of HIV-related, imminent death to more comprehensive ACP that includes treatment preferences for a range of possible clinical scenarios in the setting of chronic multimorbidity. On the other hand, certain ACP challenges unique to HIV-infected individuals remain the same despite improvements in HIV treatment. For example, HIV-infected individuals may experience HIV-related stigma, resulting in limited social support or isolation. They may receive help only from HIV-infected partners and friends and may lose this support network to HIV-related death or debility.10 Without appropriate documentation of surrogate medical decision makers or effective ACP, decisions regarding end-of-life or emergent care for HIV-infected individuals may be legally deferred to estranged family members who may be unaware of the individual’s HIV serostatus or treatment wishes.11 Other challenges include a rapidly evolving knowledge base and the advent of new therapies that further complicate accurate prognostication, as well as disproportionate HIV infection in vulnerable populations who may have low health literacy or a limited understanding of ACP, including those of black or Hispanic race, those with mental illness, injection drug users, and prisoners.12
As more HIV-infected individuals survive into older age and new generations are protected from experiencing HIV infection as a life-limiting illness, it should be remembered that longevity does not obliterate the need for ACP. On the contrary, practitioners must look ahead and prepare for the changing end-of-life needs of this uniquely vulnerable population. Currently, the US Department of Health and Human Services (DHHS) recommends ACP for all individuals with chronic, life-limiting illness or those aged 55 years and older, regardless of health status.13 It is suggested that practitioners identify surrogate decision makers for their patients if possible, and that they document goals of care and preferences using POLST. However, the issue of ACP was not addressed in Infectious Diseases Society of America (IDSA) or DHHS HIV/AIDS practice guidelines.14,15 There are currently no evidence-based recommendations on when or how HIV practitioners should discuss ACP with HIV-infected patients, especially those whose prognosis is driven by non–HIV-related multimorbidity in the era of antiretroviral therapy. Consequently, the available body of literature was examined to determine what is known about ACP in HIV-infected adults in the era of antiretroviral therapy. Based on existing knowledge, areas of crucial need for future research were also identified.
Methods
Overview
This review describes original research studies on ACP for HIV-infected adults in the era of antiretroviral therapy. Because existing research on this topic is limited and heterogeneous, precluding a systematic review, this article provides a narrative review describing what is known about the topic. This research received no grant funding from any agency.
Search Strategy
This review utilized 2 groups of search terms: 1) those related to ACP; and 2) those related to HIV. Various search terms within the same group were combined using “OR,” then the 2 groups of search terms (related to ACP or HIV) were combined using “AND.”
Search terms within the ACP-related group that were combined using “OR” included advance care planning; advance health care planning, advance medical planning; advance directive; advance directives; resuscitation order; resuscitation orders; withholding resuscitation; resuscitation policy; resuscitation policies; do-not-resuscitate order; do-not-resuscitate orders; do not resuscitate order; do not resuscitate orders; resuscitation decision; resuscitation decisions; medical power of attorney; health care power of attorney; healthcare power of attorney; psychiatric will; end-of-life; and end-of-life communication. Search terms within the HIV-related group that were combined using “OR” included HIV and AIDS.
Afterward, ACP-related search terms were combined with HIV-related search terms using “AND.” They were then used to search PubMed, EMBASE, and PsycINFO databases on September 4, 2015. The search was conducted by a professional librarian skilled and experienced in article searches. In PubMed, each of the above search terms was used as an official medical subject heading (MeSH) term and keyword. Related entry terms within each MeSH heading were also included in keyword searches.
Selection Criteria
Because of the focus on ACP in HIV-infected adults in the era of antiretroviral therapy, this review excluded articles on children or adolescents, studies conducted before 1996 (before effective antiretroviral therapy was available), articles in languages other than English, nonmedical articles (eg, legal articles), and nonoriginal research articles (eg, case reports, review articles, editorials, book chapters, and newspaper articles).
Procedure
In the first round of searches, web-based commercial reference management software (RefWorks, Bethesda, MD) was used to exclude duplicates. In the second round, article titles of all publications identified by the search strategy described above were reviewed to exclude results that did not focus on ACP in HIV-infected adults. If it was unclear based on the title whether an article should be included, a full review of the article’s abstract was conducted to make the decision. During the third round, the above selection criteria were applied to the remaining articles to arrive at the studies included in this review. Common elements were extracted from each of the articles, including study design, types and numbers of subjects, demographic characteristics, severity of HIV disease, study definitions of ACP, rates of ACP reported, and factors associated with lack of ACP. To determine the level of significance of each factor despite the heterogeneous nature of available studies, this review also calculated the percentage of the number of times each factor was statistically significantly associated with lack of ACP per the number of times it was evaluated in the existing literature. During the review, common findings were also identified to establish themes that may be generalizable across populations.
Results
Of 716 publications identified using the search strategy described above, 11 articles met the selection criteria and were included in this review (Figure). Key features of the studies are summarized in Table 1. All studies were conducted in outpatient settings between 1996 and 2015, except for the study by de Caprariis and colleagues, which was conducted in an inpatient setting.16 The number of participants ranged from 9 to 2864. Across studies, most participants were white men with education below the college level, except for the study by Mosack and colleagues in which most participants were black men.17 The definitions of ACP were often broad, variable, and poorly defined, described as any form of end-of-life communication, any form of advance directive, or any discussion about the kind of care an individual would want if they were to become ill.
Figure.
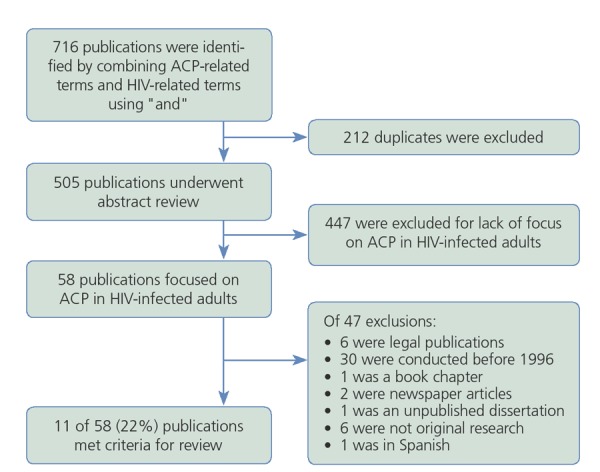
Article review flow chart.
Prevalence of Advance Care Planning Among HIV-Infected Individuals
Four of the studies reviewed examined the prevalence of advance directives. The completion rate of advance directives among the 4 studies ranged between 8% and 47%.11,16,18,19 The majority of advance directives were completed in inpatient or presurgical settings,18 and few HIV-infected patients completed advance directives in outpatient settings prior to hospital admission (7.6%).16
Of the 8 studies that investigated end-of-life communication, 3 described patient-reported prevalence rates of end-of-life communication, which ranged from 36% to 54%.19-21 However, there were discrepancies between patient and physician reports of the occurrence of end-of-life communication. Curtis and colleagues found that 15 of 57 (26%) physician-patient pairs disagreed on whether end-of-life communication had taken place, with physicians overestimating its occurrence.20 In 5 of the 15 discordant pairs, patients reported that end-of-life communication had taken place whereas physicians did not; in the remaining 10 discordant pairs, physicians reported that end-of-life communication had taken place whereas patients did not. The researchers did not comment on possible reasons for the discrepancies between patient and physician reports of end-of-life communication. However, a later study by Mosack and colleagues may shed some light on this discordance.17 Based on data from qualitative interviews, they found a notable difference in how physicians and patients defined end-of-life communication. Practitioners tended to focus on the desired medical interventions at the end of life, while patients generally referenced the paperwork that results from end-of-life communication (eg, a living will or a power of attorney) instead of the process of ACP itself or the types of medical interventions enacted when there is a decline in health.
Factors Associated With Lack of ACP
Eight studies reported patient characteristics that are associated with a lack of an advance directive or end-of-life communication (Table 2). The most commonly reported factor per the number of times evaluated was low income. This was followed by lower severity of illness, described as a lack of current or prior history of AIDS, higher CD4+ cell count, fewer symptoms, or a lack of recent hospitalizations within the past 6 months. In 2 studies, rates of completion of advance directives were higher among HIV-infected individuals with certain comorbid conditions, such as cardiovascular disease (adjusted odds ratio [aOR], 2.3; 95% confidence interval [CI], 1.1-4.6),11,18 neurologic disorders (aOR, 5.0; 95% CI, 2.2-12.1), chronic kidney disease (aOR, 3.3; 95% CI, 1.3-8.3), or malignancy (aOR, 2.8; 95% CI, 1.3-6.0).18 Other factors included low education, black or Hispanic race, female sex, younger age, injection drug use, and social isolation (reported as living alone, having limited social support, or experiencing HIV-related stigma).
Table 2.
| Source | Rate of ACPc | Characteristics | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Low Income | Lower Ill-ness Severityt | Low Educaion Level | Nonwhite Raced | Female Sex | Younger Age | Injection Drug Use | Social Isolation | ||
| Erlandson et al,11 2012 | 47% | AD | AD | AD | 0 | AD | AD | … | AD |
| de Caprariis et al,16 2013 | 8% | … | … | … | … | … | … | … | … |
| Mosack et al,17 2015 | … | … | … | … | … | … | … | … | … |
| Barocas et al,18 | 23% AD | … | AD | … | 0 | 0 | AD | 0 | 0 |
| 2015 | |||||||||
| Wenger et al,19 2001 | 38% AD, 50% EOL | … | AD and EOL | EOL | AD and EOL | EOL | 0 | AD and EOL | EOL |
| Curtis et al,20 1999 | 54% EOL | EOL | 0 | 0 | EOL | EOL | 0 | EOL | … |
| Mouton et al,21 1997 | 36% EOL | EOL | EOL | EOL | EOL | 0 | … | 0 | 0 |
| Hutson,22 2015 | … | … | … | … | … | … | … | … | EOL |
| Curtis et al,23 1997 | … | EOL | EOL | EOL | EOL | EOL | EOL | EOL | 0 |
| Karasz et al,24 2003 | … | … | … | … | … | … | … | … | … |
| Curtis et al,25 | … | … | EOL | … | … | … | … | … | … |
| 2000 | |||||||||
| Times reported per times evaluated | … | 100% | 86% | 80% | 67% | 67% | 60% | 60% | 50% |
Abbreviations: ACP, advance care planning; AD, advance directive; EOL, end-of-life communication.
Zeroes indicate no associations reported.
Ellipses indicate not evaluated by the study.
Data show rate of overall ACP when unspecified.
Black or Hispanic race.
Three other themes also emerged as patient-related factors associated with advance directives and end-of-life communication. First, 3 studies reported that the prevalence of advance directives and end-of-life communication increased when individuals possessed positive psychosocial characteristics, such as less denial of illness, positive coping skills, a desire to be involved in medical decision making, a lack of discomfort discussing death, more social support, and living with family members (especially children).11,19,22 Second, 1 study reported that certain misconceptions negatively correlated with rates of ACP, including the belief that discussing ACP will cause harm or death, or that having a living will makes it unnecessary to discuss ACP further.23 Third, 4 studies reported how patients’ relationships with their practitioners affected rates of ACP. For example, ACP was less likely to occur if patients had short relationships with or less trust in their clinicians.19 ACP was also less likely if patients were cared for by physician assistants or nurse practitioners instead of physicians, despite no difference in disease conditions or overall satisfaction with care.20 Researchers postulated that this may be due to some patients’ beliefs that mid-level practitioners will not be the ones caring for them in the hospital, or the possibility that mid-level practitioners may have less education or experience conducting discussions about end-of-life care. Additionally, both physicians and patients reported waiting for the other to bring up the topic of ACP: patients expressed a desire to protect physicians from uncomfortable discussions, while physicians thought that discussing ACP might undermine a patient’s hope.17,23 Ultimately, a lack of discussions of ACP by clinicians was an important predictor of fewer completions of advance directives (aOR, 5.82; 95% CI, 4.50-7.52).19
Three additional studies described barriers to end-of-life communication reported by physicians. Barriers included limited time, energy, or preparation; uncertainty regarding prognosis; cultural discordance between practitioner and patient; potential change of physician at the end of life if enrolled in hospice; and the belief that the physician themselves or the patient was not ready to discuss end-of-life care.23-25
Table 1.
Characteristics of Studies of Advance Care Planning
| Characteristics | ||||||
|---|---|---|---|---|---|---|
| Source | Study Design | Type of Participants | N | Demographics | Study Inclusion Criteria | Definition of ACP |
| Erlandson et al,11 2012 | Cross-sectional survey/interview | Patients | 369 | 70% aged >55 y; 84% men; 76% white; 72% without college-level education; 20% were admitted to the hospital in the prior year | Aged 45-65 y; taking antiretroviral therapy; plasma HIV RNA level < 200 copies/mL in the prior 6 mo | “Do you have an advance directive, living will, or durable power of attorney of health care decisions?” |
| de Caprariis et al,16 2013 | Retrospective chart review | Patients | 182 | Median age, 47 y; 70% men; median time from HIV diagnosis, 9.5 y | Admitted to the hospital between 2004 and 2011 | Any living will, health care proxy, or do-not-resuscitate order |
| Mosack et al,17 2015 | Cross-sectional survey/interview | Practitioners and patients | 11 and 42, respectively | 65% men; 91% black; 25% had been diagnosed with AIDS at the time of the study | HIV specialists in a midsized Midwestern city and HIV-seropositive persons from the same clinics | The medical care one would want to receive should they become ill |
| Barocas et al,18 2015 | Retrospective chart review | Patients | 588 | Mean age, 47 y; 81% men; 72% white; 41% had private insurance; mean CD4+ cell count, 634/μL | Aged >18 y; not in a prison or menta health facility; no legal guardian | An advance directive that allows patients to communicate health care preferences in the event that they are no longer able to make decisions |
| Wenger et al,19 2001 | Cross-sectional survey/interview | Patients | 2864 | 89% aged >50 y; 77% men; 49% white; 52% without high school-level education; 59% had AIDS | Aged >18 y with 1 visit to a nonmilitary, nonprison medical practitioner | Any end-of-life communication |
| Curtis et al,20 1999 | Prospective cohort | Practitioners and patients | 38 and 57, respectively | Median age, 39 y; 52% men; 65% white; 79% without college-level education; 63% with >24 mo since AIDS diagnosis | Prior AIDS-defining illness and CD4+ cel count <100/μL | Communications about end-of-life care |
| Mouton et al,21 1997 | Cross-sectional survey/interview | Patients | 861 | Mean age, 35 y; 90% men; 66% white; 70% MSM; 47% without college-level education; 88% with AIDS | Aged >18 y | "Have you told your physicians that this is the approach you want taken in your treatment?" |
| Hutson,22 2015 | Cross-sectional survey/interview | Patients | 9 | 77% aged >50 y; 55% men; 66% white; 66% without college-level education; average time since HIV diagnosis, 16 y | Aged >21 y, residing in an Appalachian county in Tennessee | Not defined |
| Curtis et al,23 1997 | Cross-sectional survey/interview | Practitioners and patients | 19 and 47, respectively | Median age, 38 y; 66% men; 64% white | AIDS-defining illness and CD4+ cell count < 200/μL | The kind of care one would want if they became too ill to speak for themselves |
| Karasz et al,24 2003 | Cross-sectional survey/interview | Practitioners | 16 | Mean time in field, 16 y; 75% men | Caring for late-stage HIV-infected patients | Not defined |
| Curtis et al,25 2000 | Prospective cohort | Practitioners and patients | 38 and 57, respectively | Mean age, 39 y; 91% men; 65% white, 64% with CD4+ cell count > 200/μL | AIDS-defining illness and CD4+ cell count > 100/μL | The kind of care one would want if they became too ill to speak for themselves |
Abbreviations: ACP, advance care planning; MSM, men who have sex with men.
Discussion
Research on ACP among HIV-infected individuals in the era of antiretroviral therapy is limited. Based on review of the existing literature, the reported rates of ACP among HIV-infected individuals are highly variable. Additionally, these rates were drawn from a small group of heterogeneous research studies, none of which were true prevalence studies. In the existing literature, the reported rate of end-of-life communication ranged between 36% and 54%, and the rate of completion of advance directives ranged between 8% and 47%, with most advance directives completed in acute care settings (in hospitals or prior to surgery). In comparison, the rate of completion of advance directives in the general US population ranged between 15% and 25%,26 with only 18% completed prior to admittance to a hospital.27
This review identified multiple patient-related factors that correlated with a lack of ACP. Although heterogeneity across studies prevents statistical comparison among these factors, the frequency of statistical significance for each factor aggregated across studies may imply a level of importance. For example, low income may be an important contributor to lack of ACP, as it was most commonly reported as statistically significant when evaluated in the existing literature (4/4 studies) (Table 2). Akin to prior research in the uninfected population,28,29 higher rates of ACP were found among HIV-infected individuals who were older or experienced a higher severity of illness, described as advanced HIV infection or comorbid conditions associated with increased morbidity and mortality, such as cardiovascular disease, neurologic disorders, chronic kidney disease, or malignancy. Additionally, similar to the general population, ACP in HIV-infected individuals was less common among vulnerable subgroups (those of black or Hispanic race, injection drug users, those of lower socioeconomic status, and those who were socially isolated).29-38 The prevalence of ACP may be lower among such individuals because of less trust in practitioners, cultural discordance, the misconception that discussing ACP will cause harm, a lack of available health care proxies,22 or a lack of incentive to ensure the well-being of survivors, especially a lack of children in the household.11,19
From practitioners’ perspectives, 2 types of factors limited ACP. First, logistic reasons may inhibit practitioners from discussing ACP, including limited time or energy and the loss of long-term relationships with patients owing to a change of physician after hospice enrollment. Second, some practitioners also reported feeling prohibited by inadequate preparation and training, described as not feeling ready to discuss ACP or having insufficient knowledge for the process (insufficient understanding of a patient’s culture or discomfort with prognostication). Similar barriers were found in the general population, with lower rates of end-of-life communication and completion of advance directives if physicians lacked time or knowledge about how to engage in ACP.39
Despite substantial changes in the clinical course and treatment of HIV infection, as well as progress in the realm of ACP, many issues regarding ACP for HIV-infected individuals remained consistent from 1996 to recent years. Regardless of when they were conducted, most studies recommended that more efforts were needed to increase the quantity and quality of ACP among HIV-infected individuals.11,16-25 Many barriers to ACP remained statistically significant over the past 2 decades, such as low education, low income, and lower severity of illness. Issues of discordance in end-of-life communication between patients and practitioners also persisted, such as discrepancies in reported occurrences of end-of-life communication or differences in how patients and practitioners define end-of-life communication.17,20
This research was limited by the small number of available studies. Because only a few of these studies were conducted in recent years, findings in the existing literature may not represent the current issues surrounding ACP and end-of-life communication among HIV-infected individuals. Moreover, there was a large amount of heterogeneity among the studies, limiting the opportunity for analysis of pooled data or statistical comparisons among risk factors related to the lack of ACP.
This review revealed several important gaps in the existing literature on ACP in the era of antiretroviral therapy. First, further investigation focusing on vulnerable subgroups is needed. Current evidence suggests that rates of ACP are lower in these populations and that some are particularly at risk for legal or familial conflicts if ACP is not completed. For example, with the rapidly shifting legal and political climates surrounding the issue of same-sex marriage, the hierarchy of surrogate decision makers for HIV-infected individuals with same-sex partners may change, creating a potential for confusion if ACP is not in place.40-44
Second, methods for increasing the rate of effective ACP among HIV-infected individuals should be developed, and future research should leverage factors associated with increased rates of ACP, such as targeting patients with higher severity of illness, building a trusting relationship between patient and practitioner, or encouraging ACP to promote the well-being of survivors. To increase rates and quality of ACP in the outpatient setting prior to a medical crisis, effective interventions are needed to equip practitioners with practical, time-saving tools that can help elicit patient-centered goals of care and accurate prognostication in the setting of multimorbidity. Although some tools are available for the general population, they have not yet been studied in HIV-infected individuals.45,46
Third, HIV service networks should develop strategies to translate research on ACP among HIV-infected individuals into policy and practice. Future efforts should employ multipronged approaches that remove barriers to ACP for both patients and practitioners, such as raising patient awareness regarding misconceptions around ACP and providing practitioners with recommendations on ACP and end-of-life communication in evidence-based practice guidelines, such as those from the IDSA or DHHS.
Last, as HIV-infected individuals survive longer with increased multimorbidity, their ACP needs may become similar to those of their uninfected counterparts who may be cared for by geriatricians and palliative care practitioners. As a result, collaborations between HIV and geriatrics or palliative care service networks may increase the prevalence and quality of ACP among HIV-infected individuals, possibly through direct contact with patients or through professional education. However, more research is needed to determine the most effective ways for such collaborations to take place.
Conclusion
Research on ACP in the era of antiretroviral therapy is limited but does reveal a highly variable prevalence of ACP among HIV-infected individuals. Rates of ACP are particularly low in vulnerable subgroups, possibly because of distrust, misconceptions, cultural discordance, or social isolation. In contrast, rates of ACP are higher among individuals who are older, have higher severity of illness, or suffer from certain comorbid conditions as part of multimorbidity, an entity that necessitates a new paradigm for ACP in the era of antiretroviral therapy. Practitioners reported clinical logistics and inadequate preparation as barriers to ACP. More research is needed to inform policy and create guidelines for HIV practitioners on when and how to discuss ACP with patients. Collaborations with geriatrics and palliative care service networks may help increase the prevalence and quality of ACP among HIV-infected patients, as these networks also care for patients with complex ACP needs. However, more research is needed to further define the ideal involvement of these networks in the care of this emerging population.
References
- 1.Hammer SM, Squires KE, Hughes MD, et al. A controlled trial of two nucleoside analogues plus indinavir in persons with human immunodeficiency virus infection and CD4 cell counts of 200/µL or less. N Engl J Med. 1997;337:725-733. [DOI] [PubMed] [Google Scholar]
- 2.Gulick RM, Mellors JW, Havlir D, et al. Treatment with indinavir, zidovudine, and lamivudine in adults with human immunodeficiency virus infection and prior antiretroviral therapy. N Engl J Med. 1997;337(11):734-739. [DOI] [PubMed] [Google Scholar]
- 3.Brooks JT, Buchacz K, Gebo KA, Mermin J. HIV infection and older Americans: the public health perspective. Am J Public Health. 2012; 102(8):1516-1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pathai S, Bajillan H, Landay AL, High KP. Is HIV a model of accelerated or accentuated aging? J Gerontol A Biol Sci Med Sci. 2014; 69(7):833-842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.High KP, Brennan-Ing M, Clifford DB, et al. HIV and aging: state of knowledge and areas of critical need for research. A report to the NIH Office of AIDS Research by the HIV and Aging Working Group. JAIDS. 2012;60(Suppl 1):S1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim DJ, Westfall AO, Chamot E, et al. Multimorbidity patterns in HIV-infected patients: the role of obesity in chronic disease clustering. JAIDS. 2012;61(5):600-605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. International Society of Advance Care Planning and End of Life Care. The definition of advance care planning. http://acpelsociety.com/index.php. Accessed on January 18, 2016.
- 8. Physician Orders for Life-Sustaining Treatment Paradigm (POLST). The national POLST paradigm. http://www.polst.org/. Accessed on January 18, 2016.
- 9.Mullick A, Martin J, Sallnow L. An introduction to advance care planning in practice. BMJ. 2013;347:f6064. [DOI] [PubMed] [Google Scholar]
- 10.Poindexter C, Shippy RA. Networks of older New Yorkers with HIV: fragility, resilience, and transformation. AIDS Patient Care STDs. 2008;22(9):723-733. [DOI] [PubMed] [Google Scholar]
- 11.Erlandson KM, Allshouse AA, Duong S, Mawhinney S, Kohrt WM, Campbell TB. HIV, aging, and advance care planning: are we successfully planning for the future? J Palliat Med. 2012;15(10): 1124-1129.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kutzen HS. Integration of palliative care into primary care for human immunodeficiency virus-infected patients. Am J Med Sci. 2004; 328(1):37-47. [DOI] [PubMed] [Google Scholar]
- 13. Agency for Health Research and Quality. National guideline clearinghouse. http://www.guideline.gov/content.aspx?id=47803. Accessed on January 18, 2016.
- 14.Aberg JA, Gallant JE, Ghanem KG, Emmanuel P, Zingman BS, Horberg MA. Primary care guidelines for the management of persons infected with HIV: 2013 update by the HIV medicine association of the Infectious Diseases Society of America. Clin Infect Dis. 2014; 58(1):1-10. [DOI] [PubMed] [Google Scholar]
- 15. Department of Health and Human Services. Guidelines for the use of antiretroviral agents in HIV-1–infected adults and adolescents. http://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf. Accessed on January 18, 2016.
- 16. de Caprariis PJ, Carballo-Dieguez A, Thompson S, Lyon C. Advance directives and HIV: a current trend in the inner city. J Community Health. 2013;38(3):409-413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mosack KE, Wandrey RL. Discordance in HIV-positive patient and health care provider perspectives on death, dying, and end-of-life care. Am J Hosp Palliat Care. 2015;32(2):161-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barocas JA, Erlandson KM, Belzer BK, Hess T, Sosman J. Advance directives among people living with HIV: room for improvement. AIDS Care. 2015;27(3):370-377. [DOI] [PubMed] [Google Scholar]
- 19.Wenger NS, Kanouse DE, Collins RL, et al. End-of-life discussions and preferences among persons with HIV. JAMA. 2001;285(22): 2880-2887. [DOI] [PubMed] [Google Scholar]
- 20.Curtis JR, Patrick DL, Caldwell E, Greenlee H, Collier AC. The quality of patient-doctor communication about end-of-life care: a study of patients with advanced AIDS and their primary care clinicians. AIDS. 1999;13(9):1123-1131. [DOI] [PubMed] [Google Scholar]
- 21.Mouton C, Teno JM, Mor V, Piette J. Communication of preferences for care among human immunodeficiency virus-infected patients. Barriers to informed decisions? Arch Fam Med. 1997;6(4):342-347. [DOI] [PubMed] [Google Scholar]
- 22.Hutson SP. Climbing back up the mountain: reflections from an exploration of end-of-life needs of persons living with HIV/AIDS in Appalachian Tennessee. Am J Hosp Palliat Care. 2015;[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 23.Curtis JR, Patrick DL. Barriers to communication about end-of-life care in AIDS patients. J Gen Intern Med. 1997;12(12):736-741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karasz A, Dyche L, Selwyn P. Physicians' experiences of caring for late-stage HIV patients in the post-HAART era: challenges and adaptations. Soc Sci Med. 2003;57(9):1609-1620. [DOI] [PubMed] [Google Scholar]
- 25.Curtis JR, Patrick DL, Caldwell ES, Collier AC. Why don't patients and physicians talk about end-of-life care? Barriers to communication for patients with acquired immunodeficiency syndrome and their primary care clinicians. Arch Intern Med. 2000;160(11):1690-1696. [DOI] [PubMed] [Google Scholar]
- 26.Miles SH, Koepp R, Weber EP. Advance end-of-life treatment planning. A research review. Arch Intern Med. 1996;156(10):1062-1068. [PubMed] [Google Scholar]
- 27.Salmond SW, David E. Attitudes toward advance directives and advance directive completion rates. Orthop Nurs. 2005;24(2):117-127. [DOI] [PubMed] [Google Scholar]
- 28.Rao JK, Anderson LA, Lin FC, Laux JP. Completion of advance directives among U.S. consumers. Am J Prev Med. 2014;46(1):65-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dobalian A. Advance care planning documents in nursing facilities: results from a nationally representative survey. Arch Gerontol Geriatr. 2006;43(2):193-212. [DOI] [PubMed] [Google Scholar]
- 30.Beck A, Brown J, Boles M, Barrett P. Completion of advance directives by older health maintenance organization members: the role of attitudes and beliefs regarding life-sustaining treatment. J Am Geriatr Soc. 2002;50(2):300-306. [DOI] [PubMed] [Google Scholar]
- 31.Kiely DK, Mitchell SL, Marlow A, Murphy KM, Morris JN. Racial and state differences in the designation of advance directives in nursing home residents. J Am Geriatr Soc. 2001;49(10):1346-1352. [DOI] [PubMed] [Google Scholar]
- 32.Colenda C, Jensen M, Foster J, Kendrick B, Mewhinny K, Messick C. Variables predicting the completion of an advance directive by older adults. Ann Longterm Care. 1998;6(3). [Google Scholar]
- 33.Gordon NP, Shade SB. Advance directives are more likely among seniors asked about end-of-life care preferences. Arch Intern Med. 1999;159(7):701-704. [DOI] [PubMed] [Google Scholar]
- 34.Carrese JA, Rhodes LA. Western bioethics on the Navajo reservation. Benefit or harm? JAMA. 1995;274(10):826-829. [PubMed] [Google Scholar]
- 35.Caralis PV, Davis B, Wright K, Marcial E. The influence of ethnicity and race on attitudes toward advance directives, life-prolonging treatments, and euthanasia. J Clin Ethics. 1993;4(2):155-165. [PubMed] [Google Scholar]
- 36.Buckle JM, Horn SD, Oates VM, Abbey H. Severity of illness and resource use differences among white and black hospitalized elderly. Arch Intern Med. 1992;152(8):1596-1603. [PubMed] [Google Scholar]
- 37.Blackhall LJ, Murphy ST, Frank G, Michel V, Azen S. Ethnicity and attitudes toward patient autonomy. JAMA. 1995;274(10):820-825. [PubMed] [Google Scholar]
- 38.Eleazer GP, Hornung CA, Egbert CB, et al. The relationship between ethnicity and advance directives in a frail older population. J Am Geriatr Soc. 1996;44(8):938-943. [DOI] [PubMed] [Google Scholar]
- 39.Morrison RS, Morrison EW, Glickman DF. Physician reluctance to discuss advance directives. An empiric investigation of potential barriers. Arch Intern Med. 1994;154(20):2311-2318. [PubMed] [Google Scholar]
- 40. Loue S. Living wills, durable powers of attorney for health care, and HIV infection. The need for statutory reform. J Leg Med. 1995; 16(4):461-480. [DOI] [PubMed] [Google Scholar]
- 41. New York State Department of Health. Fact sheet: family health care decisions act and HIV/AIDS. https://www.health.ny.gov/diseases/aids/providers/regulations/fhcda/ai_fact_sheet.htm. Accessed on January 18, 2016.
- 42. The White House. Respecting the rights of hospital patients to receive visitors and to designate surrogate decision makers for medical emergencies. https://www.whitehouse.gov/the-press-office/presidential-memorandum-hospital-visitation. Accessed on January 18, 2016.
- 43. Riou, G. Hospital visitation and medical decision making for same-sex couples. https://www.americanprogress.org/issues/lgbt/news/2014/04/15/88015/hospital-visitation-and-medical-decision-making-for-same-sex-couples/. Accessed on January 18, 2016.
- 44. Liptak, A. Supreme court asked to look abroad for guidance on same-sex marriage. http://www.nytimes.com/2015/04/07/us/supreme-court-asked-to-look-abroad-for-guidance-on-same-sex-marriage.html?_r=0. Accessed on January 18, 2016.
- 45. University of California San Francisco. ePrognosis: estimating prognosis for elders. http://eprognosis.ucsf.edu/. Accessed on January 18, 2016.
- 46.Sudore RL, Knight SJ, McMahan RD, et al. A novel website to prepare diverse older adults for decision making and advance care planning: a pilot study. J Pain Symptom Manage. 2014;47(4):674-686. [DOI] [PMC free article] [PubMed] [Google Scholar]


