Supplementary oxygen is frequent in the management of patients admitted to the intensive care unit (ICU) [1]. However, some studies have suggested deleterious effects of hyperoxia on these patients [2–4]. This main study objective was to assess the association between hyperoxia, at any time of the ICU stay, and ICU mortality regardless of the cause of patient admission.
Our study was an observational, retrospective, and single-centre study in the Hôpital Européen George Pompidou medical ICU, Paris, France. All patients admitted between November and December 2017 were included regardless of their admission cause and all of their arterial blood gases (ABGs) were analysed. Hyperoxia was defined as a partial arterial pressure in oxygen (PaO2) superior to 100 mmHg (13.3 kPa). The principal judgement criterion was occurrence of at least one hyperoxia episode during the ICU stay. All statistical tests were two-tailed with a significance threshold of 0.05. Analyses were performed with R v3.2.4. Survival analysis was estimated by Kaplan–Meier methods.
A total of 130 patients, median age 68 (57–79) years and median SAPS II 45 (35–56), were included. The mean reason for ICU admission was respiratory failure (60 patients, 46%) and 83 patients (64%) needed mechanical ventilation. Thirty-five patients (27%) died during their ICU stay.
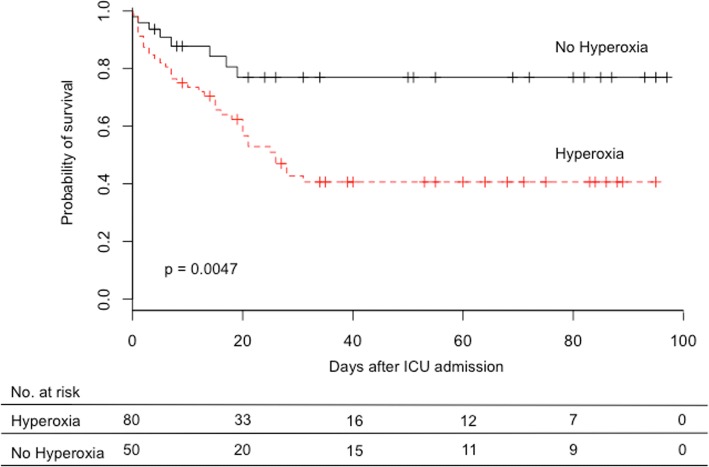
Eighty patients (62%) presented at least one episode of hyperoxia. Overall survival (OS) was significantly lower in patients who presented at least one episode of hyperoxia during their ICU stay: median OS was 26 days (95% CI 20–NR) versus median not reached, p = 0.0047 (Fig. 1).
Fig. 1.
Kaplan–Meier estimation of overall survival. Hyperoxia group, patients who presented at least one hyperoxia episode during ICU stay. No hyperoxia group, patients who presented no hyperoxia episode during ICU stay. Overall survival median in hyperoxia group 26 days (95% CI 20–NR); overall survival median in no hyperoxia group not reached. ICU intensive care unit
In univariate analysis, hyperoxia was a risk factor for mortality: 31 deceased patients presented hyperoxia (89%) versus 49 alive patients (52%), p < 0.001. SAPS II and mechanical ventilation time were also mortality risk factors in univariate analysis (Additional file 1: Table S1). Multivariate analysis showed that hyperoxia was an independent risk factor for ICU mortality: OR = 3.80 (95% CI 1.08–16.01), p = 0.047 (Table 1).
Table 1.
Mortality risk factors in the medical ICU, multivariate analysis
| Mortality risk factor | Deceased (n = 35) | Alive (n = 95) | Odds ratio (95% CI) | p |
|---|---|---|---|---|
| Age (years) | 70 (66–75) | 65 (61–69) | 0.15 | |
| SAPS II | 64 (56–72) | 41 (37–45) | < 0.001 | |
| Mechanical ventilation time | 9 (7–12) | 5 (3–7) | 0.074 | |
| At least one PaO2 > 100 mmHg (13.3 kPa) | 31 (89%) | 49 (52%) | 3.80 (1.08–16.01) | 0.047 |
Data presented as mean (95CI) or n (%)
R2 = 0.453
CI confidence interval, ICU intensive care unit, PaO2 partial arterial pressure in oxygen, SAPS II Simplified Acute Physiology Score II
Despite a conservative oxygen policy, 62% of patients presented at least one episode of hyperoxia, which reinforces the statement by Helmerhorst et al. [5]. Previous studies had a focus on specific categories of selected patients [2–4]. On the contrary, our study is a pragmatic study in real-life conditions. We included all consecutive patients admitted to the medical ICU without any exclusion criteria, regardless of the admission cause, mechanical ventilation need, or initial severity, and we collected prospectively a large amount of 1.450 ABG. In this study, we demonstrated that hyperoxia at any time of the ICU stay significantly decreases OS and is an independent mortality risk factor.
Additional file
Table S1. Mortality risk factors in medical ICU, univariate analysis. (DOCX 17 kb)
Acknowledgments
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABG
Arterial blood gas
- ICU
Intensive care unit
- OS
Overall survival
- PaO2
Partial arterial pressure in oxygen
- SAPS II
Simplified Acute Physiology Score II
Authors’ contributions
MR participated in data acquisition, data analysis, and data interpretation, wrote the manuscript, and created Fig. 1. EG designed the study and revised the manuscript. CB and NA participated in the study and designed and revised the manuscript. JN participated in data acquisition and analysis. CH-B, BH, J-LA, SO, DV, and J-LD are physicians and were involved in patient care. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Data collection and analyses were conducted in accordance with the French national guidelines: under French law, a retrospective study using data from medical charts requires only a declaration to the Commission nationale Informatique et Libertés. The hospital’s computerised database was declared at this commission. There is no requirement for declaration to an ethic committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mathilde Ruggiu, Phone: 01-56-09-32-12, Email: mathilde.ruggiu@hotmail.fr.
Nadia Aissaoui, Email: nadia.aissaoui@aphp.fr.
Julien Nael, Email: julien.nael@gmail.com.
Caroline Haw-Berlemont, Email: caroline.haw-berlemont@aphp.fr.
Bertrand Herrmann, Email: bertrand.herrmann@aphp.fr.
Jean-Loup Augy, Email: jean-loup.augy@aphp.fr.
Sofia Ortuno, Email: ortunosofia1@gmail.com.
Damien Vimpère, Email: damien.vimpere@aphp.fr.
Jean-Luc Diehl, Email: jean-luc.diehl@aphp.fr.
Clotilde Bailleul, Email: clotilde.bailleul@aphp.fr.
Emmanuel Guerot, Email: emmanuel.guerot@aphp.fr.
References
- 1.Panwar R, Capellier G, Schmutz N, Davies A, Cooper DJ, Bailey M, et al. Current oxygenation practice in ventilated patients—an observational cohort study. Anaesth Intensive Care. 2013;41:505–514. doi: 10.1177/0310057X1304100412. [DOI] [PubMed] [Google Scholar]
- 2.Vincent J-L, Taccone FS, He X. Harmful effects of hyperoxia in postcardiac arrest, sepsis, traumatic brain injury, or stroke: the importance of individualized oxygen therapy in critically ill patients. Can Respir J. 2017;2017:1–7. doi: 10.1155/2017/2834956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Damiani E, Adrario E, Girardis M, Romano R, Pelaia P, Singer M, et al. Arterial hyperoxia and mortality in critically ill patients: a systematic review and meta-analysis. Crit Care [Internet]. 2014;4(1):23. Available from: http://ccforum.biomedcentral.com/articles/10.1186/s13054-014-0711-x. Cited 2018 Jul 15. [DOI] [PMC free article] [PubMed]
- 4.Helmerhorst HJF, Roos-Blom M-J, van Westerloo DJ, de Jonge E. Association between arterial hyperoxia and outcome in subsets of critical illness: a systematic review, meta-analysis, and meta-regression of cohort studies. Crit Care Med. 2015;43:1508–1519. doi: 10.1097/CCM.0000000000000998. [DOI] [PubMed] [Google Scholar]
- 5.Helmerhorst HJ, Schultz MJ, van der Voort PH, Bosman RJ, Juffermans NP, de Jonge E, et al. Self-reported attitudes versus actual practice of oxygen therapy by ICU physicians and nurses. Ann Intensive Care [Internet]. 2014;18(6):711. Available from: http://www.annalsofintensivecare.com/content/4/1/23. Cited 2018 Jul 15. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Mortality risk factors in medical ICU, univariate analysis. (DOCX 17 kb)
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.