Abstract
Background
The working environment plays an important role in public health. This study investigates the risk for long-term sickness absence (LTSA) from the combination of factors related to physical work demands.
Methods
Employees (n = 22 740) of the general population (the Danish Work Environment & Health study 2012) were followed for two years in the Danish Register for Evaluation of Marginalisation. Using Cox regression analyses we determined the risk of LTSA from four factors; (i) physical work demands, (ii) physical exertion during work, (iii) fatigue after work and (iv) work-limiting pain.
Results
During follow-up 10.2% experienced LTSA. Each of the four factors increased the risk of LTSA with hazard ratios (HR) ranging from 1.30 to 1.57. Scoring high on one (30.3% of the respondents), two (24.4%), three (19.9%) and all four factors (9.2%) gradually increased the risk of LTSA (HR’s of 1.39 [95% CI 1.16–1.66], 1.66 [95% CI 1.39–1.99], 1.90 [95% CI 1.57–2.29] and 3.02 [95% CI 2.47–3.68], respectively). Risk estimates remained robust in stratified analyses of age, sex and socioeconomic position. Population attributable fractions were high across all subgroups; 39% (general population), 36% (younger workers), 45% (older workers), 36% (men), 41% (women), 30% (higher socioeconomic position) and 45% (lower socioeconomic position).
Conclusion
The risk of LTSA gradually increased with number of factors related to high physical work demands, underlining the importance of targeting combined factors in risk assessment and preventive interventions.
Introduction
High physical work demands remain a relevant risk factor for developing health problems.1–5 With access to high-quality registers in the Nordic countries this has been studied in relation to labour market consequences. In the general population of Denmark and Norway, the proportion of long-term sickness absence (LTSA) from work that could be attributed to high physical work demands were 25% and 26%, respectively.1,4 Thus, appropriate preventive measures at the workplaces related to these demands could theoretically prevent up to one quarter of all LTSA in the population. Among a subgroup of blue-collar workers in the Danish study the corresponding number was 40% showing an even higher potential for prevention among workers with manual labour and high physical work demands.1 Similar subgroup analyses could be relevant to perform where differences in the balance between physical capacity of the individual worker and physical work demands may exist, for example, men vs. women and younger vs. older workers. The latter is especially relevant in the light of the demographic changes in the population towards an increased proportion of elderly. Many European countries have increased statuary retirement age and reduced the access to early retirement to keep older workers longer at the labour market.
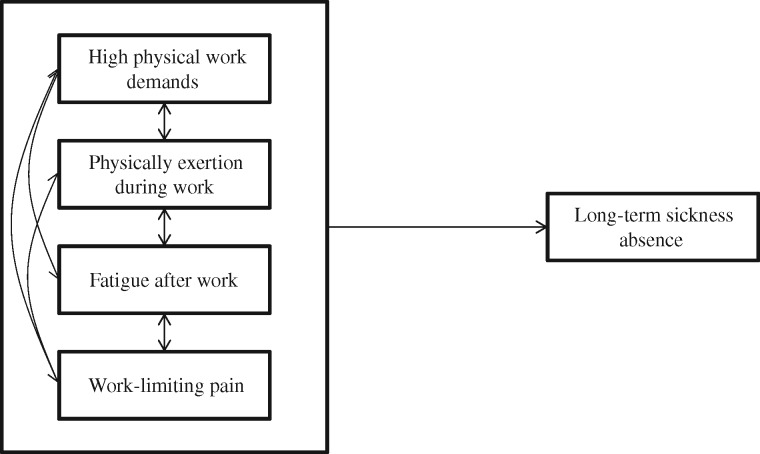
It is well known that high physical work demands can be experienced as physically exerting, and lead to fatigue after work and work-limiting musculoskeletal pain.1–12 These factors related to high physical work demands constitute an inter-dependent causal chain to long-term health problems. Despite of the inter-dependency of these factors, previous studies have investigated their independent effects on health. Thus, high physical work demands, such as frequent lifting, heavy lifting, working with bent or twisted back, prolonged standing and working with arms above shoulder height are known risk factors for both musculoskeletal disorders and LTSA.1–12 High physical work demands are also known to cause an acute perception of higher physical exertion during work,13 which by itself increases the risk for both musculoskeletal pain14 and LTSA.15 Likewise, musculoskeletal pain by itself is an early predictor of LTSA.16,17Figure 1 illustrates the conceptual model in this causal chain to long-term health consequences. Because of the clear inter-dependency of these factors in a causal chain to health impairments, treating them as independent might provide underestimated risk estimates for long-term health problems. Moreover, because many workers (e.g. several blue-collar groups) experience the combination of these factors, the results of previous studies may be misleading for preventive interventions at the workplaces.
Figure 1.
Conceptual model. In the causal chain to long-term health consequences, high physical work demands increase perceived physical exertion during work, leading to higher levels of fatigue after work and consequently work-limiting pain. However, work-limiting pain can also intensity the perception of physical exertion and fatigue, and may also lead to work-modifications of less demanding tasks. Thus, when studying complex phenomena like labour market attachment, combining inter-dependent factors to investigate the risk for long-term health consequences is a more realistic scenario
This study investigates the risk for register-based LTSA from the combination of factors related to physical work demands among employees from the general population.
Methods
Study design and population
The study design is a prospective register follow-up on questionnaire respondents. Reporting is in accordance with the STROBE guidelines.18 Data on work environment and health were obtained from the 2012 round of the Danish Work Environment & Health Study.19
In the 2012 round, a random sample of 50 806 employees, aged 18–64 years, employed for a minimum of 35 h per month, with an income of minimum 3000 DKK (∼400€) per month in the past 3 months were drawn from Danish registers and invited to participate in the study. A total of 25 804 (50.8%) chose to participate. The response percentage was different among sex (women 56.6%, men 45.6%), age-groups (younger than 35 years 36.0%, between 35 and 50 years 51.3%, older than 50 years 63.3%) and among groups of different socioeconomic positions; workers of lower socioeconomic position (unskilled workers 48.4% and skilled workers 49.0%), workers of higher socioeconomic position (top leaders 50.8%, academics 59.5%, people with 3–4 years of vocational education 58.9%), unknown position (41.6%). After excluding those not being employees (e.g. self-employed or out of work at the time of the questionnaire reply), 22 740 employees were included in the analyses (table 1). All were currently employed at the time of their questionnaire reply.
Table 1.
Characteristics of the employees (N = 22 740). Values are percentage of participants or mean and standard deviations (SD)
| N | % | Mean | SD | |
|---|---|---|---|---|
| Age, years | 22 740 | 45.9 | 10.7 | |
| Sex | ||||
| Men | 10 528 | 46.3 | ||
| Women | 12 212 | 53.7 | ||
| Psychosocial work factors (0–100) | ||||
| Influence at work | 22 465 | 79.4 | 19.0 | |
| Emotional demands | 22 452 | 49.6 | 26.8 | |
| Support from colleagues | 22 457 | 79.1 | 17.3 | |
| Support from superior | 22 011 | 60.1 | 24.4 | |
| Smoking | ||||
| Yes, every day | 3768 | 16.9 | ||
| Yes, once in a while | 1075 | 4.8 | ||
| Ex-smoker | 6644 | 29.7 | ||
| No, never | 10 854 | 48.6 | ||
| BMI (kg m−2) | 22 206 | 25.6 | 4.4 | |
| Leisure physical activity (hours week−1) | 22 264 | 2.4 | 2.3 | |
| Previous long-term sickness absence | ||||
| No | 20 770 | 91.3 | ||
| Yes | 1970 | 8.7 | ||
| Long-term sickness absence during follow-up | ||||
| No | 20 430 | 89.8 | ||
| Yes | 2310 | 10.2 | ||
| Chronic disease | ||||
| Depression | ||||
| Yes | 1223 | 5.7 | ||
| No | 20 338 | 94.3 | ||
| Diabetes | ||||
| Yes | 614 | 2.9 | ||
| No | 20 850 | 97.1 | ||
| Cardiovascular disease | ||||
| Yes | 268 | 1.3 | ||
| No | 21 155 | 98.8 | ||
| Stroke | ||||
| Yes | 117 | 0.6 | ||
| No | 21 298 | 99.5 | ||
| Cancer | ||||
| Yes | 294 | 1.4 | ||
| No | 21 140 | 98.6 | ||
Risk factors related to the physical work environment
The questionnaire asked about four factors related to the physical work environment; (i) physical work demands, (ii) physical exertion during work, (iii) fatigue after work and (iv) work-limiting pain.
For physical work demands20 the questions were, ‘How much of your working time do you …’ (i) walk or stand?, (ii) work with twisted or bent back without support from the hands and arms?, (iii) have the arms lifted to or above shoulder height, (iv) do the same arm movements several times a minute? (e.g. package work, mounting, machine feeding, carving), (v) squat or kneel when you work?, (vi) push or pull? and (vii) lift or carry? Response options for each of the seven questions were ‘almost all the time’, ‘approx. 3/4 of the time’, ‘approx. 1/2 of the time’, ‘approx. 1/4 of the time’, ‘seldom/very little’ and ‘never’. Those performing lifting or carrying replied to an additional question, (viii) ‘How much does it typically weigh?’ with the response options ‘less than 5 kg’, ‘5–15 kg’, ‘16–29 kg’ and ‘30 kg or above’. For the subsequent analyses, physical work demands was dichotomized to low and high by the following procedure1: Low was defined as those replying ‘never’ to ‘approx. 1/4 of the time’ for question 1 and ‘never’ to ‘seldom/very little’ for questions 2–7. Respondents had to be in the low category for all these seven questions to be defined as low. High was defined as replying ‘approx. 1/2 of the time’ to ‘almost all the time’ for question 1, or ‘approx. 1/4 of the time’ to ‘almost all the time’ for questions 2–7, or ‘30 kg or above’ to question 8. Respondents had to be in the high category in at least one of these eight questions to be defined as high.
For physical exertion during work15 the question was ‘How physically exerting do you usually perceive your current work?’ with a horizontally oriented 0–10 response scale,21 where 0 is no exertion and 10 is maximal exertion. For the subsequent analyses, physical exertion during work was dichotomized to low and high as 0–5 and 6–10, respectively.
Using a modified version of a single item from the Need for Recovery after work questionnaire22 the question for fatigue after work was: ‘How fatigued are you after a typical working day?’ with a 5-point response scale of ‘not fatigued’, ‘a little fatigued’, ‘somewhat fatigued’, ‘very fatigued’ and ‘completely fatigued’. For the subsequent analyses, fatigue after work was dichotomized to low and high as ‘not fatigued’ to ‘a little fatigued’ and ‘somewhat fatigued’ to ‘completely fatigued’, respectively.
Using a modified version of the Standardised Nordic Questionnaire for Musculoskeletal Symptoms,23 the question for work-limiting pain was ‘Have you due to pain been limited in your work during the last 3 months?’ with a response scale of ‘No’, ‘Yes, a little’, ‘Yes, somewhat’ and ‘Yes, very’. For the subsequent analyses, work-limiting pain was dichotomized to low and high as no and yes (the three categories together), respectively.
Subsequently, an index from 0 to 4 of physical over-load was defined as the sum of low’s (value 0) and high’s (value 1) of the four factors related to the physical work environment.
Outcome variable, LTSA
Information about sickness absence was derived from Danish Register for Evaluation of Marginalisation (DREAM),24,25 and linked to the questionnaire replies of the Danish Work Environment & Health Study through the unique personal identification number which is given to all Danish citizens at birth or foreigners immigrating to Denmark. The sickness absence data in DREAM are based on the municipalities’ actual payments of benefits, and the validity is therefore considered to be high. The necessity for such a register in research on sickness absence is important, because self-reports—which are typically inaccurate due to recall bias—only show low agreement with the DREAM register for temporary transfer income such as sickness benefit and unemployment benefit.25 For the present analyses, we defined LTSA as having registered sickness absence in DREAM for a period at least six consecutive weeks during 2-year follow-up starting the week after the questionnaire reply.
Control variables
Age (continuous variable) and sex for each individual were drawn from the Central Person Register of Denmark. The four dimensions of the psychosocial work environment were based on the Copenhagen Psychosocial Questionnaire (COPSOQ) and each included two questions about (i) influence at work, (ii) support from colleagues, (iii) support from superiors and (iv) emotional demands, that were converted to a scale of 0–100, where 100 is best,26 and included as a continuous variable. Lifestyle included smoking status (categorical variable: daily, once in a while, ex-smoker, never), body mass index (continuous variable, BMI, kg m−2), leisure-time physical activity (continuous variable, hours of moderate to high intensity leisure physical activity). Previous LTSA was determined from the DREAM register in the same way as described above, but for two years prior to the questionnaire reply (categorical variable, yes/no). Treatment for chronic disease during the last year (categorical variable, yes/no) included depression, diabetes, cardiovascular disease, stroke and cancer. Socioeconomic position (categorical variable) were drawn from the Employment Classification Module27 and included top leaders, academics, people with 3–4 years of vocational education, skilled workers, unskilled workers as well as a smaller group of unknown position. These control variables were chosen because they may be associated with both predictors and outcome, although it may be argued that some of them will lead to over-adjustment. Thus, we chose to present both a minimally and fully adjusted model, as well as a sensitivity analysis.
Statistical analyses
The Cox proportional hazard model28 was used to model the probability of LTSA during 2-year follow-up (Proc PHREG of SAS version 9.4.). The estimate from this model is hazard ratios (HR), which assess ratios between number of cases and person-time (time-to-event). For simplicity we use the term ‘risk’ when discussing the results. The outcome variable was LTSA. Data on LTSA correspond to survival times which in most cases are censored as most of the study population did not experience a LTSA-event during follow-up. Data were also censored in case of one of the following events: early retirement, disability pension, statutory retirement, emigration or death. When individuals had an onset of LTSA during follow-up, survival times were non-censored and referred to as event times.
The four factors related to the physical work environment were the explanatory variables. As a first step, these four factors were analysed separately, and as a second step they were combined as an index of 0–4, where 0 and 4 is scoring low and high on all four, respectively, and as a third step, the analyses of the index were stratified for sex, age and socioeconomic position [categorized into lower (skilled workers, unskilled workers) and higher (top leaders, academics, people with 3–4 years of vocational education)]. The analyses were performed in three successive models. Model 1 was adjusted for age and sex. Model 2 (final model) was the same as Model 1, but additionally included psychosocial work environment, lifestyle, previous LTSA and chronic disease, and socioeconomic position. Model 3 was a sensitivity analysis of Model 2, excluding those with previous LTSA. Results are reported as HR’s with 95% confidence intervals (95% CI).
Population attributable fractions (PAF) were calculated for the 0–4 index based on the HR’s and proportions exposed (Pe) from Model 2 of the second and third set of analyses where PAF (%) = ∑Pe(HRe - 1)/(∑ Pe(HRe - 1) + 1) * 100%. The Pe included all above index 0. PAF expresses the contribution of a risk factor to LTSA.
Results
During follow-up, 10.2% of the study population experienced LTSA with a mean (SD) time to event of 46.6 (32.6) weeks. A total of 5.6% were censored before the end of 2-year follow-up with a mean (SD) time to censoring of 44.5 (31.0) weeks.
Table 2 shows that all individual factors were risk factors for LTSA. In the fully adjusted Model 2, the HR’s ranged from 1.30 to 1.57. These results remained in a sensitivity analyses (Model 3), excluding those with previous LTSA.
Table 2.
Risk of long-term sickness absence during 2-year follow-up from scoring high in physical work demands, physical exertion during work, fatigue after work or work-limiting pain, as well as scoring high in one to four of these factors (index). On the basis of Model 2 the population attributable fraction is 39% for the index. Estimates are hazard ratios (HR) and 95% confidence intervals (CI)
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| N | % | HR (95% CI) | HR (95% CI) | HR (95% CI) | ||
| Physical work demands | Low | 9491 | 42.7 | 1 | 1 | 1 |
| High | 12 756 | 57.3 | 1.90 (1.73–2.08) | 1.49 (1.34–1.65) | 1.56 (1.38–1.76) | |
| Physical exertion during work | Low | 15 904 | 70.9 | 1 | 1 | 1 |
| High | 6515 | 29.1 | 1.83 (1.69–1.99) | 1.39 (1.25–1.53) | 1.43 (1.27–1.60) | |
| Fatigue after work | Low | 8003 | 35.6 | 1 | 1 | 1 |
| High | 14 449 | 64.4 | 1.60 (1.46–1.76) | 1.30 (1.17–1.44) | 1.30 (1.16–1.46) | |
| Work-limiting pain | Low | 16 834 | 75.2 | 1 | 1 | 1 |
| High | 5561 | 24.8 | 2.09 (1.92–2.27) | 1.57 (1.43–1.73) | 1.54 (1.38–1.72) | |
| Index | 0 of 4 | 3569 | 16.2 | 1 | 1 | 1 |
| 1 of 4 | 6698 | 30.3 | 1.57 (1.32–1.87) | 1.39 (1.16–1.66) | 1.34 (1.10–1.63) | |
| 2 of 4 | 5383 | 24.4 | 2.18 (1.84–2.59) | 1.66 (1.39–1.99) | 1.66 (1.36–2.02) | |
| 3 of 4 | 4405 | 19.9 | 2.76 (2.33–3.27) | 1.90 (1.57–2.29) | 1.85 (1.51–2.27) | |
| 4 of 4 | 2028 | 9.2 | 5.01 (4.20–5.97) | 3.02 (2.47–3.68) | 3.09 (2.48–3.86) |
Notes: Model 1: Adjusted for age and sex.
Model 2: Model 1 + psychosocial work environment (influence at work, support from colleagues, support from leader, emotional demands), lifestyle (smoking, BMI, leisure physical activity), previous long-term sickness absence, chronic disease (depression, diabetes, cardiovascular disease, stroke, cancer) and socioeconomic position.
Model 3: Sensitivity analysis of Model 2, excluding those with previous long-term sickness absence.
Table 2 also shows the risk for LTSA increased gradually from scoring high on one to all four factors. In Model 1 and Model 2, respectively, scoring high on all four factors increased the risk of LTSA with HR’s of 5.01 and 3.02. Figure 2 shows the survival plot of Model 2 (using direct adjusted survivor functions). The unadjusted percentage of LTSA during follow-up among those scoring high on 0, 1, 2, 3 and 4 factors were 4.9%, 7.6%, 10.5%, 12.8% and 21.2%, respectively (not shown in the table).
Figure 2.
Survival plot. X-axis is the time from baseline and y-axis is the survival probability based on the final model (Model 2) using direct adjusted survivor functions. The lines represent from above to below 0 of 4, 1 of 4, 2 of 4, 3 of 4 and 4 of 4 factors (high physical work demands, physical exertion during work, fatigue after work and work-limiting pain), respectively
Table 3 shows that the main results (Model 2 of table 2), remained stable in stratified analyses of sex, age and socioeconomic position. This was further confirmed by three separate interaction analyses of sex, age and socioeconomic position with the number of factors related to the physical work environment, which all showed non-significant interactions.
Table 3.
Risk of long-term sickness absence during 2-year follow-up from scoring high in one to four of the following factors: physical work demands, physical exertion during work, fatigue after work and work-limiting pain. Stratified analyses (sex, age and socioeconomic position) of Model 2 in table 2 adjusting for age, sex, psychosocial work environment, lifestyle, previous LTSA, chronic disease and socioeconomic position. Estimates are hazard ratios (HR) and 95% confidence intervals (CI). The population attributable fraction (PAF) is provided for each subgroup as well
| Index | N | % | HR (95% CI) | PAF (%) | N | % | HR (95% CI) | PAF (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Age | <50 years | 50 years or more | |||||||
| 0 of 4 | 2182 | 17.0 | 1 | 36% | 1387 | 15.0 | 1 | 45% | |
| 1 of 4 | 3825 | 29.8 | 1.26 (1.00–1.59) | 2873 | 31.0 | 1.62 (1.21–2.15) | |||
| 2 of 4 | 3081 | 24.0 | 1.53 (1.21–1.93) | 2302 | 24.9 | 1.92 (1.44–2.57) | |||
| 3 of 4 | 2562 | 20.0 | 1.79 (1.41–2.28) | 1843 | 19.9 | 2.13 (1.58–2.88) | |||
| 4 of 4 | 1171 | 9.1 | 3.14 (2.44–4.05) | 857 | 9.3 | 2.96 (2.14–4.09) | |||
| Sex | Men | Women | |||||||
| 0 of 4 | 1767 | 17.3 | 1 | 36% | 1802 | 15.2 | 1 | 41% | |
| 1 of 4 | 3061 | 30.0 | 1.31 (0.96–1.78) | 3637 | 30.6 | 1.42 (1.14–1.77) | |||
| 2 of 4 | 2339 | 22.9 | 1.55 (1.13–2.13) | 3044 | 25.6 | 1.71 (1.37–2.13) | |||
| 3 of 4 | 2061 | 20.2 | 1.72 (1.24–2.38) | 2344 | 19.7 | 1.98 (1.57–2.50) | |||
| 4 of 4 | 975 | 9.6 | 2.97 (2.11–4.18) | 1053 | 8.9 | 3.01 (2.35–3.85) | |||
| Socioeconomic position | Higher | Lower | |||||||
| 0 of 4 | 2550 | 23.2 | 1 | 30% | 807 | 8.3 | 1 | 45% | |
| 1 of 4 | 4301 | 39.1 | 1.30 (1.04–1.63) | 1997 | 20.6 | 1.52 (1.10–2.11) | |||
| 2 of 4 | 2651 | 24.1 | 1.67 (1.32–2.11) | 2383 | 24.6 | 1.62 (1.18–2.23) | |||
| 3 of 4 | 1164 | 10.6 | 1.99 (1.53–2.59) | 2947 | 30.4 | 1.79 (1.30–2.45) | |||
| 4 of 4 | 334 | 3.0 | 2.59 (1.87–3.60) | 1550 | 16.0 | 3.07 (2.23–4.23) | |||
PAF’s were high across all subgroups; 39% (general population), 36% (younger workers), 45% (older workers), 36% (men), 41% (women), 30% (higher socioeconomic position) and 45% (lower socioeconomic position).
Discussion
The main finding of our study was that the risk of LTSA gradually increased with number of factors related to high physical work demands. This underlines the importance of targeting the combination of such factors in risk assessment and preventive interventions at workplaces.
In agreement with several previous studies regarding factors related to physical work demands and health,1–12 our register follow-up of >20 000 employees from the general population showed that high physical work demands, physical exertion during work, fatigue after work and work-limiting pain are risk factors of LTSA. Separately, each of the four factors related to the physical work demands increased the risk of LTSA with HR between 1.30 and 1.57. This finding confirms the relevance of each respective factor for the risk of developing long-term health problems.
As a novel finding, our study showed that scoring high on more factors related to physical work demands gradually increased the risk estimates for LTSA, that is, with HR going from 1.39 for one to 3.02 for four factors. This finding underlines the considerable increased risk for LTSA from high demands, exertion, fatigue and work-limiting pain, and indicates the importance of combining them rather than treating them as independent factors. While only 30% of the employees of general population scored high on one of these four factors, more than half of the working population scored high on two or more. In line with this, a recent Nordic project highlighted the existence of several risk factors in the physical working environment for early retirement from the labour market especially among elderly women in blue-collar jobs.29 To elaborate on this, we performed stratified analyses of sex, age and socioeconomic position and calculated PAF’s by combining risk estimates with Pe. While the risk estimates remained largely robust in the stratified analyses, the PAF’s differed slightly. Thus, the highest PAF’s were seen among older workers, women and workers in lower socioeconomic position. Although supporting the conclusions from the Nordic project, PAF’s were relatively high in all subgroups with the lowest value of 30% among workers in higher socioeconomic position. This stresses the importance of targeting risk assessment and preventive interventions across all strata of society, and particularly among elderly and workers in lower socioeconomic position. For future generations of workers, preventive effort should start early as cumulative physical load during working life increases the risk of sickness absence and disability pension among older workers.30
Figure 1 illustrates the conceptual model of the complex interplay between several factors related to physical work demands and risk for LTSA. In the causal chain, high physical work demands are known to increase perceived physical exertion during work,13 leading to higher levels of fatigue after work and consequently work-limiting pain.2,3,6–8,10 However, work-limiting pain can also intensify the perception of physical exertion and fatigue, and may also lead to work-modifications of less demanding tasks. Accordingly, these factors can influence each other, and studying them separately may therefore lead to flawed conclusions. For example, an office worker having work-limiting pain but with low physical demands, low exertion and low fatigue is likely to only have slightly increased risk for LTSA, while for example a construction worker with work-limiting pain having high physical demands, high exertion and high fatigue can be expected to be at considerably increased risk for LTSA. Thus, when studying complex phenomena like labour market attachment, combining inter-dependent factors to investigate the risk for long-term health consequences can provide a more realistic picture. This has relevance not only for research, but also for risk assessment and preventive interventions at the workplaces.
Strengths and limitations
Our study has both strengths and limitations. First, because the employer is prohibited by law to ask the employee for the reason of sickness absence, the DREAM register does not contain such information. However, this also minimizes the potential bias of self-reported reasons for sickness absence as well as recall bias of period and length of sickness absence. Because the employer has a strong economic incentive to be reimbursed for the economic loss of sickness absence, the accuracy of the DREAM register is considered to be high.25 Second, the four factors related to physical work demands used as risk factors or predictors of LTSA in the present study were self-reported, that is, obtained from questionnaires, which is less accurate than direct measurements at the workplace.31,32 However, direct measurements are time-consuming and expensive, and questionnaires are therefore commonly used in epidemiology. The results can therefore easily be compared with previous studies. The results of the study have high generalizability as we used a representative sample of the general population. Furthermore, the risk estimates of the four-factor index remained robust across different strata of age, sex and socioeconomic position, further strengthening the validity and generalizability of the observed results. Thus, our results are unlikely to be caused by, for example, socioeconomic confounding. In addition, the analyses were controlled for several other factors known to influence the risk for sickness absence, and a sensitivity analysis (Model 3) excluding those with prior sickness absence showed similar results as the final Model 2.
Conclusion
The risk of LTSA gradually increased with number of factors related to high physical work demands, that is, HR—going from one to all four factors—increased gradually from 1.39 to 3.02. This underlines the importance of targeting the combination of these factors in risk assessment and preventive interventions at workplaces. Furthermore, analyses of PAF’s showed that potential for prevention is high across all strata of society, and particularly among elderly and workers in lower socioeconomic position.
Acknowledgements
We would like to express our gratitude to Ebbe Villadsen and Lisbeth Nielsen for valuable help during the project and access to the data.
Ethical approval
The study has been notified to and registered by The Danish Data Protection Agency. According to Danish law, questionnaire and register based studies neither need approval by ethical and scientific committees, nor informed consent.33,34 All data were de-identified and analysed anonymously on the server of Statistics Denmark.
Conflicts of interest: None declared.
Key points
Previous studies show that high physical work demands can be exerting, lead to fatigue after work and work-limiting musculoskeletal pain.
Although these factors are dependent and influence each other, most studies have investigated their independent effects on health.
There is gradually increased risk of long-term sickness absence with the number of factors related to high physical work demands.
Preventive interventions in the working environment ought to target the combination of high physical work demands, perceived exertion, fatigue after work and work-limiting musculoskeletal pain, rather than treating them as independent factors.
References
- 1. Andersen LL, Fallentin N, Thorsen SV, et al. Physical workload and risk of long-term sickness absence in the general working population and among blue-collar workers: prospective cohort study with register follow-up. Occup Environ Med 2016;73:246–53. [DOI] [PubMed] [Google Scholar]
- 2. Mayer J, Kraus T, Ochsmann E. Longitudinal evidence for the association between work-related physical exposures and neck and/or shoulder complaints: a systematic review. Int Arch Occup Environ Health 2012;85:587–603. [DOI] [PubMed] [Google Scholar]
- 3. da Costa BR, Vieira ER. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med 2010;53:285–323. [DOI] [PubMed] [Google Scholar]
- 4. Sterud T. Work-related mechanical risk factors for long-term sick leave: a prospective study of the general working population in Norway. Eur J Public Health 2014;24:111–6. [DOI] [PubMed] [Google Scholar]
- 5. Foss L, Gravseth HM, Kristensen P, et al. The impact of workplace risk factors on long-term musculoskeletal sickness absence: a registry-based 5-year follow-up from the Oslo health study. J Occup Environ Med 2011;53:1478–82. [DOI] [PubMed] [Google Scholar]
- 6. Sterud T, Tynes T. Work-related psychosocial and mechanical risk factors for low back pain: a 3-year follow-up study of the general working population in Norway. Occup Environ Med 2013;70:296–302. [DOI] [PubMed] [Google Scholar]
- 7. Coenen P, Gouttebarge V, van der Burght AS, et al. The effect of lifting during work on low back pain: a health impact assessment based on a meta-analysis. Occup Environ Med 2014;71:871–7. [DOI] [PubMed] [Google Scholar]
- 8. Holtermann A, Hansen JV, Burr H, et al. Prognostic factors for long-term sickness absence among employees with neck-shoulder and low-back pain. Scand J Work Environ Health 2010;36:34–41. [DOI] [PubMed] [Google Scholar]
- 9. Sommer TG, Svendsen SW, Frost P. Sickness absence and permanent work disability in relation to upper- and lower-body pain and occupational mechanical and psychosocial exposures. Scand J Work Environ Health 2016;42:481–9. [DOI] [PubMed] [Google Scholar]
- 10. van den Heuvel SG, Ariens GA, Boshuizen HC, et al. Prognostic factors related to recurrent low-back pain and sickness absence. Scand J Work Environ Health 2004;30:459–67. [DOI] [PubMed] [Google Scholar]
- 11. Hoogendoorn WE, Bongers PM, de Vet HC, et al. High physical work load and low job satisfaction increase the risk of sickness absence due to low back pain: results of a prospective cohort study. Occup Environ Med 2002;59:323–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Andersen LL, Fallentin N, Ajslev JZN, et al. Association between occupational lifting and day-to-day change in low-back pain intensity based on company records and text messages. Scand J Work Environ Health 2017;43:68–74. [DOI] [PubMed] [Google Scholar]
- 13. Jakobsen MD, Sundstrup E, Persson R, et al. Is Borg’s perceived exertion scale a useful indicator of muscular and cardiovascular load in blue-collar workers with lifting tasks? A cross-sectional workplace study. Eur J Appl Physiol 2014;114:425–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Holtermann A, Clausen T, Jørgensen MB, et al. Patient handling and risk for developing persistent low-back pain among female healthcare workers. Scand J Work Environ Health 2013;39:164–9. [DOI] [PubMed] [Google Scholar]
- 15. Andersen LL, Clausen T, Persson R, et al. Dose-response relation between perceived physical exertion during healthcare work and risk of long-term sickness absence. Scand J Work Environ Health 2012;38:582–9. [DOI] [PubMed] [Google Scholar]
- 16. Andersen LL, Clausen T, Burr H, et al. Threshold of musculoskeletal pain intensity for increased risk of long-term sickness absence among female healthcare workers in eldercare. PLoS ONE 2012;7:e41287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Andersen LL, Clausen T, Mortensen OS, et al. A prospective cohort study on musculoskeletal risk factors for long-term sickness absence among healthcare workers in eldercare. Int Arch Occup Environ Health 2012;85:615–22. [DOI] [PubMed] [Google Scholar]
- 18. Vandenbroucke JP, von EE, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med 2007;4:e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. National Research Centre for the Working Environment. Arbejdsmiljø og Helbred i Danmark 2012–20. Det Natl. Forskningscenter Arb, 2016. Available at: http://www.arbejdsmiljoforskning.dk/da/arbejdsmiljoedata/arbejdsmiljoe-og-helbred-20 (29 May 2017, date last accessed).
- 20. Orhede E. Nordic cooperation in research on the work environment. Scand J Work Environ Health 1994;20:65–6. [DOI] [PubMed] [Google Scholar]
- 21. Pincus T, Bergman M, Sokka T, et al. Visual analog scales in formats other than a 10 centimeter horizontal line to assess pain and other clinical data. J Rheumatol 2008;35:1550–8. [PubMed] [Google Scholar]
- 22. de Croon EM, Sluiter JK, Frings-Dresen MHW. Psychometric properties of the Need for Recovery after work scale: test–retest reliability and sensitivity to detect change. Occup Environ Med 2006;63:202–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon 1987;18:233–7. [DOI] [PubMed] [Google Scholar]
- 24. Lund T, Kivimaki M, Labriola M, et al. Using administrative sickness absence data as a marker of future disability pension: the prospective DREAM study of Danish private sector employees. Occup Environ Med 2008;65:28–31. [DOI] [PubMed] [Google Scholar]
- 25. Hjollund NH, Larsen FB, Andersen JH. Register-based follow-up of social benefits and other transfer payments: accuracy and degree of completeness in a Danish interdepartmental administrative database compared with a population-based survey. Scand J Public Health 2007;35:497–502. [DOI] [PubMed] [Google Scholar]
- 26. Pejtersen JH, Kristensen TS, Borg V, et al. The second version of the Copenhagen Psychosocial Questionnaire. Scand J Public Health 2010;38:8–24. [DOI] [PubMed] [Google Scholar]
- 27. Petersson F, Baadsgaard M, Thygesen LC. Danish registers on personal labour market affiliation. Scand J Public Health 2011;39:95–8. [DOI] [PubMed] [Google Scholar]
- 28. Cox DR. Regression models and life tables. J R Stat Soc Ser B 1972;34:187–220. [Google Scholar]
- 29. Poulsen OM. Arbejdsmiljøets betydning for fastholdelse af ældre arbejdstagere, 2017. Available at: http://www.arbejdsmiljoforskning.dk/da/projekter/arbejdsmiljoets-betydning-for-fastholdelse-af-aeldre-arbejdstagere (11 July 2017, date last accessed).
- 30. Sundstrup E, Hansen ÅM, Mortensen EL, et al. Cumulative occupational mechanical exposures during working life and risk of sickness absence and disability pension: prospective cohort study. Scand J Work Environ Health 2017;43:415–25. [DOI] [PubMed] [Google Scholar]
- 31. Viikari-Juntura E, Rauas S, Martikainen R, et al. Validity of self-reported physical work load in epidemiologic studies on musculoskeletal disorders. Scand J Work Environ Health 1996;22:251–9. [DOI] [PubMed] [Google Scholar]
- 32. Lagersted-Olsen J, Korshoj M, Skotte J, et al. Comparison of objectively measured and self-reported time spent sitting. Int J Sports Med 2014;35:534–40. [DOI] [PubMed] [Google Scholar]
- 33. Committee System on Biomedical Research Ethics. Guidelines about Notification, 2011. Available at: http://www.dnvk.dk/English/guidelinesaboutnotification.aspx.
- 34. The Danish Data Protection Agency. Compiled version of the Act on Processing of Personal Data, 2014. Available at: https://www.datatilsynet.dk/english/the-act-on-processing-of-personal-data/read-the-act-on-processing-of-personal-data/compiled-version-of-the-act-on-processing-of-personal-data/ (9 July 2017, date last accessed).