Abstract
BACKGROUND
Otosclerosis is a common cause of progressive hearing impairment that causes fixation of the stapes. Surgical intervention is the preferred treatment approach to ameliorate the conductive hearing loss associated with stapedial otosclerosis. However, given that it is a difficult and delicate procedure, the surgery may fail for a number of reasons. Therefore, it is very important to evaluate the success rate of the surgical approach used in each regional center.
OBJECTIVE
To examine the effectiveness of stapedotomy in improving hearing sensitivity for otosclerotic patients at King Abdul Aziz University Hospital in Riyadh.
DESIGN
Retrospective chart review with an analysis of pre- and postoperative surgical treatment.
SETTING
Tertiary referral otolaryngology clinic.
PATIENTS AND METHODS
All cases who underwent stapedotomy between 1997 and 2009 were retrospectively reviewed. Preoperative and postoperative audiometric assessments were conducted using conventional pure tone audiometry. Differences were analyzed by two-way repeated measures ANOVA.
MAIN OUTCOME MEASURE(S)
Pre- and postoperative pure tone thresholds for air and bone conduction.
RESULT
Fifty-three patients underwent stapedotomy. Stapedotomy yielded significant improvements in mean (SD) postoperative air-conduction thresholds of about 18.7 (11.7) dB (P<.0001) and mean (SD) postoperative bone-conduction thresholds of about 2 (7.2) dB (P<.05). Additionally, a significant correlation was found between improvement in air-conduction thresholds and the size of preoperatve air-bone gap (P<.01) About 70%of patients achieved an air-bone gap of 20 dB or better. None of the cases examined in this study exhibited sensorineural hearing loss or adverse complications following stapedotomy.
CONCLUSIONS
Stapedotomy is a safe and effective treatment option for patients with otosclerosis. Given that the majority of participants in this study exhibited mixed hearing loss preoperatively, the results further suggest that stapedotomy can also be effective in improving thresholds for these patients.
LIMITATIONS
The sample size was relatively small.
Otosclerosis is a common cause of progressive hearing impairment which is characterized by the formation of an abnormal growth of bone on the middle ear ossicles. This disorder affects the stapes footplate and in more advanced stages the cochlear capsule can be affected as well.1 Generally, bone growth may disrupt the ability of the acoustical signal to travel from the middle ear to the inner ear in an effective manner, which may result in hearing impairment. This hearing impairment can be manifested as conductive, sensorineural, or mixed hearing loss depending on the extent and the progress of the disease. If the bone growth extends into the annular ligament of the oval window, it can cause stapes fixation and a conductive hearing impairment. However, if the bone growth extends into the endosteal layer of the cochlea, then sensorineural components might be manifested. On the other hand, otosclerosis might result in sensorineural hearing loss if cochlear otosclerosis is present.2 However, it is more common for otosclerosis to surround the stapes than to damage the inner ear.
A diagnosis of otosclerosis is based generally on a clinical history of progressive hearing loss and audiological findings. Audiological evaluation typically reveals a type As tympanogram which indicates increased stiffness in the mobility of the tympanic membrane and the middle ear system. Elevated bone conduction thresholds occur, particularly at 2 kHz, which is a hallmark of otosclerosis known as Carhart’s notch. This is due to the elimination of factors that contribute to hearing sounds through bone conduction.3 Additional diagnostic assessments include an imaging investigation, which has been demonstrated as essential to confirm the diagnosis of otosclerosis.4
Treatment options for otosclerosis include medical treatment, amplification, and surgical intervention. Generally, surgical treatment of otosclerosis is considered the most effective option.5 These surgical corrections may include a small opening within the central footplate of the stapes, which is referred to as a stapedotomy or a total or partial removal of the stapes footplate which is known as stapedectomy. Generally, there are no substantial differences in both surgical techniques and both have been reported to yield similar clinical outcomes.6,7 A stapedotomy fenestration can be created by using either a microdrill or laser-assisted technique. Some authors prefer laser over conventional fenestration in stapedotomy for they believe it offers the advantage of higher precision in its application and a lower risk of footplate mobilization.8 However, others have reported that there are no significant differences in the surgical outcome or complication rates of either surgical technique.7,9
Overall, surgical intervention for stapes fixation is widely reported to yield excellent hearing results.10,11 Surgery can close the gap in the air-bone thresholds, thus improving hearing sensitivity, and in some cases, reducing the need for amplification as well as improving tinnitus symptoms associated with otosclerosis.12,13 Overall, surgical techniques have improved substantially, thus decreasing the number of failed surgeries. However, given that it is a difficult and delicate procedure, the surgery may fail for a number of reasons. These may include displacement of the prosthetic device, erosion of the incus, or sustaining head trauma. In these cases, a revision might be required; however, revision surgery is less successful at improving hearing loss than primary surgery.14 In general, there are many factors that could contribute to the success of the primary procedure such as the surgeon’s experience as well as the anatomy and the extent of the otosclerotic focus. Therefore, it is very important to evaluate the success rate of the surgical approach used in each regional center. Hence, the current study aimed to serve as a review of all patients who underwent stapedial surgery in our center to evaluate the efficacy of using this approach in managing patients with otosclerosis.
PATIENTS AND METHODS
We retrospectively reviewed charts of all otosclerotic patients who underwent stapedotomy between 1997 and 2009 at King Abdul Aziz University Hospital in Riyadh, Saudi Arabia. All cases were surgically treated by the same group of surgeons using the same surgical procedure. This study was approved by the local Institutional Review Board of King Abdul Aziz University Hospital.
Pure tone audiometry was performed pre- and postoperatively to measure the functional improvement in performance as a result of the surgical procedure. The standard audiometric assessment included pure tone thresholds for air conduction (AC) at frequencies of 0.25, 0.5, 1, 2, 4 and 8 kHz and bone conduction (BC) at 0.5, 1, 2 and 4 kHz. The postoperative air-bone gap (ABG) was calculated by subtracting the postoperative bone conduction threshold (BCT) from the postoperative air conduction threshold (ACT) as recommended by the Committee for Hearing and Equilibrium of the American Academy of Otolaryngology.15 Postoperative overclosure or sensorineural hearing loss was calculated by subtracting postoperative BCT from that obtained preoperatively. Hearing results were calculated using the last audiogram obtained preoperatively and an audiogram obtained one year postoperatively. All audiologic procedures were conducted in a standard soundproof room using a calibrated clinical audiometer.
Surgery was performed under general anesthesia using the same surgical techniques. A small-fenestra stapedotomy technique, which creates a fenestration in the stapes for the placement of the prosthesis was used in all surgical cases. Generally, all surgeries used an endaural skin incision to access the surgical site. The tympanomeatal flap was elevated to expose the middle ear structure until the annulus was reached. The ossicles were then inspected and their mobility was assessed by palpation to ensure stapes fixation. The incudostapedial joint was then separated and the stapedial muscle tendon cut to detach the stapes. The stapes superstructure was subsequently removed to facilitate the prosthesis placement and the distance from the incus to the fixed footplate was measured and the prosthesis was sized accordingly. A fenestration in the stapes footplate was created and sized using a microdrill to allow placement of the prosthesis. Different prostheses were used. After placing the prosthesis, a gelfoam was applied around it to keep it in place. The tympanomeatal flap was then repositioned followed by closing of the endaural incision. The corda tympani was preserved in all cases. All patients were discharged from the hospital the day following the surgery; no complications were reported.
Differences between pre- and postoperative measures were analyzed by two-way repeated measures ANOVA with treatment (pre- and post-operative results) and frequency (.25, .5, 1, 2, 4, and 8 kHz) as the within subject variables. Post hoc analyses were completed using paired t tests after applying Bonferroni correction for multiple comparisons. To examine the factors that could influence the extent of improvement in ACTs postoperatively, a regression analysis was conducted. SPSS version 16 was used for the analyses.
RESULTS
From 64 cases identified, 11 were excluded for having had revision surgery (2 patients) or lacking complete preoperative and/or postoperative data (9 patients). The remaining 53 patients were 24 (45.3%) females and 29 (54.7%) males (Table 1). The mean (standard deviation) age of patients at intervention was 37 (17) years, with a range of 19 to 69 years.
Table 1.
Patient demographics.
| Gender | Male | 24 (45.3) |
| Female | 29 (54.7) | |
|
| ||
| Surgical side | Right | 31 (58.5) |
| Left | 22 (41.5) | |
|
| ||
| Type of hearing loss | Mixed | 28 (52.8) |
| Conductive | 25 (47.2) | |
n (%) unless noted otherwise.
Stapedotomy yielded significant improvements in mean (SD) postoperative air-conduction thresholds of about 18.7 (11.7) dB (P<.0001) and mean (SD) postoperative bone-conduction thresholds of about 2 (7.2) dB (P<.05). Additionally, a significant correlation was found between improvement in air-conduction thresholds and the size of preoperatve air-bone gap (P<.01)
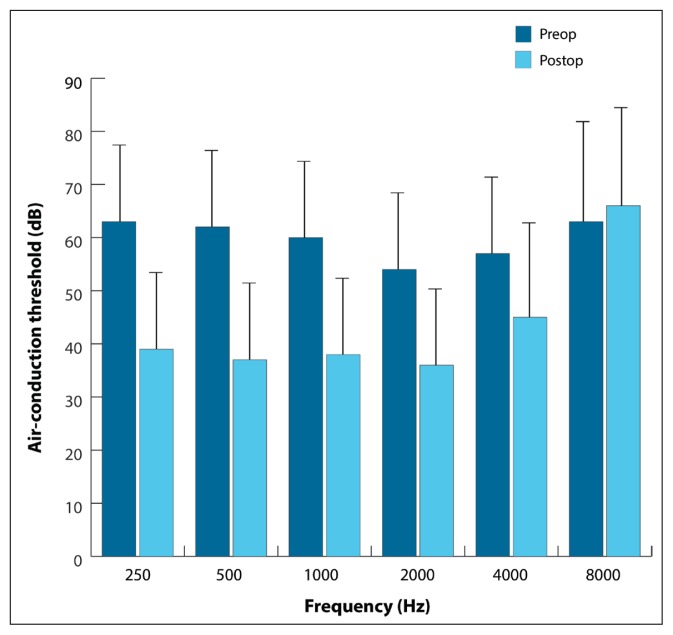
Mean differences in ACTs for the pre- and postoperative measurements indicated that the main effect of treatment was significant [F (df 1, 52)=124.1, P<.0001] (Figure 1). The postoperative ACTs were lower, indicating an improvement from preoperative ACTs. The main effect of frequency was statistically significant [F (5, 52)=26.7, P<.0001] indicating that differences in thresholds occurred across the tested frequencies. Mauchly’s test indicated that the assumption of sphericity had been violated χ2(14)=142.560, P=.001, therefore degrees of freedom were corrected using Greenhouse-Geisser estimates of sphericity (e=.484). The results showed that there was a significant effect of frequency, F(52, 125.877) = 26.703, P<.0005.
Figure 1.
Mean (SD) air-conduction thresholds in dB are compared for the pre- and postoperative measurements as a function of frequency (Hz).
There was also a significant interaction for the main effect effects of treatment and frequency [F (5, 52)=57.5, P<.0001]. However, Mauchly’s test indicated that the assumption of sphericity had been violated χ2(14)=87.557, P=.001, therefore degrees of freedom were corrected using Greenhouse-Geisser estimates of sphericity (e=.590). The results showed that the interaction was significant [F(2.951, 153.435)=57.48, P<.0005]. These results suggest that improvement in thresholds postoperatively was not consistent across the different frequencies. Specifically, post hoc analyses showed that postoperative thresholds were lower than preoperative thresholds (P<.0001) across all the different frequencies except at 8 kHz. Link to SPSS reports for Figure 1 (https://goo.gl/hZ0ItV), Figure 2 (https://goo.gl/qf94da) and Figure 3 (https://goo.gl/UtN977).
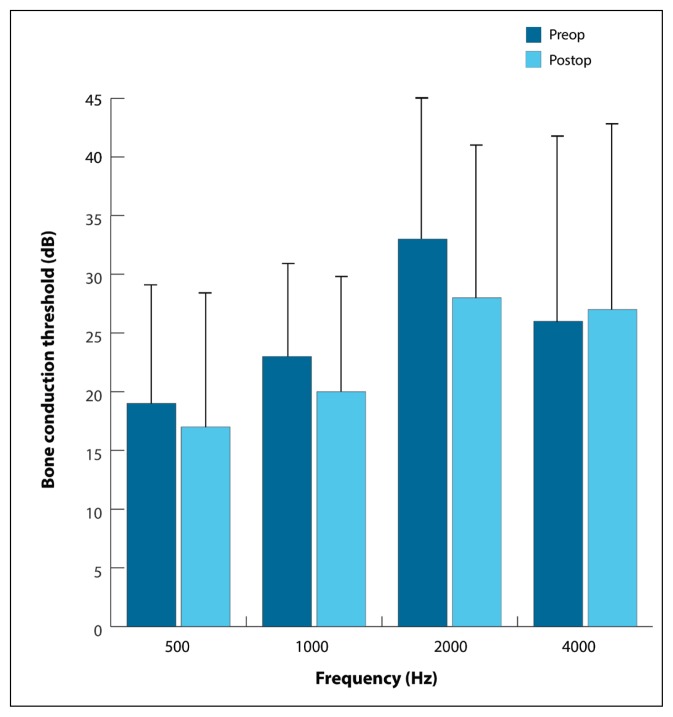
Figure 2.
Average bone-conduction thresholds in dB (±SD) are compared for the pre- and postoperative measurements as a function of frequency (Hz).
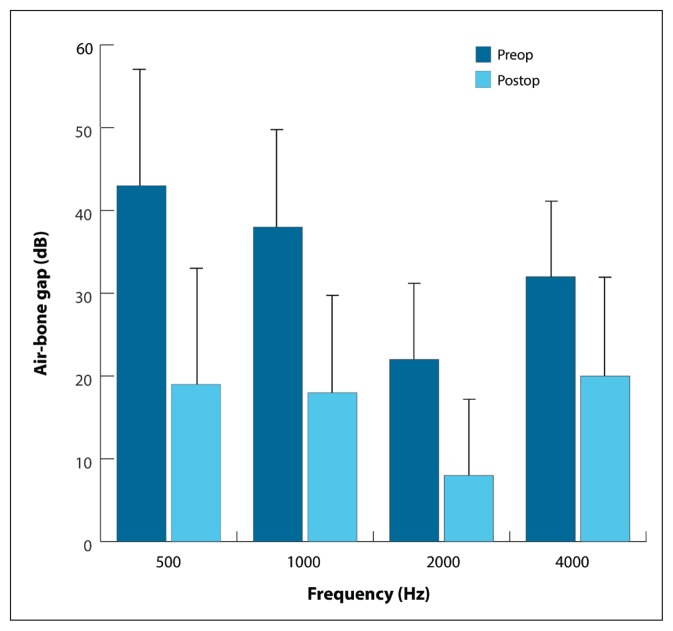
Figure 3.
Average air-bone gaps in dB (±SD) are compared for the pre- and postoperative measurements as a function of frequency (Hz).
The main effect of treatment on BCTs was significant [F (1, 52) =4.1, P<.05] (Figure 2). Postoperative thresholds were lower than the preoperative thresholds, but the difference was small as suggested by the small F value. The main effect of frequency was significant [F (3, 52)=24.5, P<.0001]. Mauchly’s test indicated that the assumption of sphericity had been violated χ2(5)= 34.941, P=.001, therefore degrees of freedom were corrected using Greenhouse-Geisser estimates of sphericity (e=.72). The results showed that there was a significant effect [F(2.181, 113.417)=24.54, P<.0005]. Post-hoc analyses revealed that BCTs improved postoperatively only at 2 kHz (P<.0001) but not at .5, 1, and 2 kHz.
There was a mean improvement in ABG [F (1, 52)=115.7, P<.0001] (Figure 3). Additionally, ABGs differed across the four frequencies [F (3, 52)=67.2, P<.0001]. Mauchly’s test indicated that the assumption of sphericity had been violated χ2(5)=17.860, P=.001, therefore degrees of freedom were corrected using Huynh-Feldt estimates of sphericity (e=.87). The results showed that there was a significant effect of frequency [F(2.627, 136.596)=67.2, P<.0005]. Post-hoc analysis showed that ABG consistently decreased with increasing frequency (P<.01), but was smallest at 2 kHz (P<.01). Additionally, ABG was dependent on the frequency as suggested by the significant interaction [F (3, 52)=20.5, P<.0001]. Post hoc t tests showed that postoperative ABGs were consistently smaller than preoperative ABGs (P<.01) across the different tested frequencies.
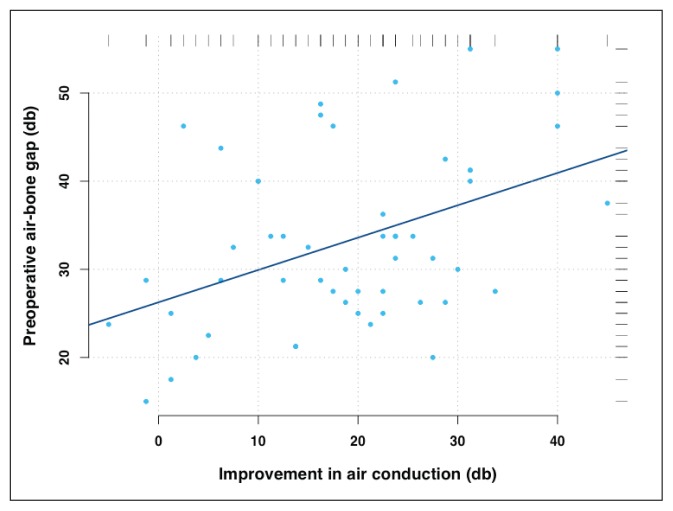
A modest correlation was found between improvement in ACTs and the size of preoperative ABG (r=0.43, 95% CI 0.18–0.63, P<.0012) (Figure 4). Specifically, a larger improvement in ACTs was found as preoperative ABG increased. These results suggest that patients with mixed hearing loss are likely to show less improvement than those with conductive impairment.
Figure 4.
A modest correlation between improvement in preoperative to postoperative ACT versus the size of preoperative ABG (r =0.43, 95% CI 0.18–0.63, P<.0012). ACT improved for each patient. Change in ACT was calculated by subtracting the postoperative ACT from the preoperative ACT.
DISCUSSION
Stapes surgery is the preferred treatment for conductive hearing loss secondary to stapedial otosclerosis.16,17 However, many surgeons favor stapedotomy over stapedectomy because theoretically it carries less risk to the inner ear structure.18,19 Given the delicate nature of the surgical procedure, it is important to evaluate the effectiveness of the surgical methodology used in remediating stapes fixation in each regional center. Hence, the purpose of this study was to examine the success of stapedotomy procedure in our center, especially since it is considered one of the largest otology centers in the region.
Generally, stapedotomy provides excellent results for correcting conductive hearing loss in patients with otosclerosis. As demonstrated in Figure 1, improvement in ACTs can be observed. This improvement in postoperative thresholds occurred at frequencies between .25–4 kHz, with no statistically significant improvement for 8 kHz. Overall, these results are consistent with that reported in the literature.20–23 Using a four frequency pure tone average (0.5, 1, 2, 4 kHz), mean improvement after surgery was 18.7 dB. This might be slightly less than that reported in previous studies.23,24 However, our results demonstrated that improvement in ACTs was dependent on the preoperative ABG such that the greater preoperative ABG, the larger improvement in ACTs after surgery (Figure 4). These findings are generally consistent with previous reports.25 Therefore, given that the majority of patients in this study exhibited mixed hearing loss (69.8%), less improvement in ACTs is expected in comparison with results in patients with conductive hearing loss who might have larger preoperative ABGs.
Stapes surgeries are generally considered successful in improving hearing for the majority of treated patients. However, one of the known potential risks following stapes surgery is sensorineural hearing loss especially at the higher frequencies. Generally, sensorineural hearing loss is considered a rare complication of stapes surgery and it is anticipated that less than 1% of cases develop sensorineural hearing loss.26–28 In the current study, ACTs remained unchanged after surgery in three cases (5.6%) and a rather slight increase in thresholds occurred at the higher frequencies (4 and 8 kHz). As discussed above, the size of the preoperative ABG is likely to contribute to the lack of improvement in the ACTs for these patients. Additionally, consistent with these results, some studies reported less benefit from stapes surgery at higher frequencies.29,30 The lack of improvement in thresholds at high frequencies has been attributed to the effect of surgical trauma, perilymph leakage, and the noise generated by the surgical drilling on the sensory cells.31 Postoperative overclosure or sensorineural hearing is typically determined by subtracting postoperative BCT from that measured preoperatively.25,32 In the current study, overclosure is defined as a change in BC pure-tone average (PTA) of 15 dB or more.24 Using these criteria, none of the cases examined in this study exhibited sensorineural hearing loss following stapedotomy.
On the other hand, BC PTA could improve with surgery due to the Carhart effect in which BC thresholds are depressed at 2 kHz due to impedance mismatch between the middle and inner ear as a result of the fixation of the stapes.33 In the current results, a mean (SD) improvement of 2 (7.2) dB was achieved postoperatively with the largest gain (4.4 dB) occurring at 2 kHz (Figure 2). For the remaining frequencies, there was no statistically significant difference. Generally, different results have been reported for improvement of BCTs after stapes surgery. For example, results varied from no change to an improvement of 7 dB post surgery.24,34–37 Therefore, our results are within those reported in the literature. In theory, the improvement in BCT is dependent on the extent of restoration of the stapes footplate. This is particularly important given that sensitivity by BC is dependent on the effective transmission of the vibration to the cochlear fluid by direct compression of the otic capsule initiated by the stapes footplate.38
Successful stapes surgery is typically defined as a closure of the ABG of 10 dB or better. In this study, ABG is calculated as the difference between the postoperative AC and BC thresholds and presented in 10 dB increments as recommended by the committee on hearing and equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss.15 Overall, mean ABG closure was within 10 dB in 32.1% of cases, between 11–20 dB in 37.7% of cases, between 21–30 dB in 22.6% of cases, and >30 dB in 7.5% of cases. It might be difficult to compare these results with previous studies, given that some previous studies calculated ABG by subtracting the preoperative BCT from the postoperative ACT.23,39–41 Previous studies demonstrated that using the preoperative BCT instead of postoperative BCT could inflate the success rate because of ABG overclosure due to the Carhart effect.42,43 The percentage of patients who have an ABG within 10 dB perhaps is considered relatively less than desirable. However, it has been suggested that patients with an ABG greater than 10 dB had mixed sensorineural hearing loss preoperatively;19 the majority of our patients had mixed hearing loss. Additionally, many authors consider an ABG within 20 dB satisfactory.25,44 The overall percentage of patients that achieved an ABG within 20 dB in this study was about 70%. On the other hand, one should consider the possibility of a reduction or a complete closure of ABG due to a decreased bone conduction, which is considered an adverse postoperative complication for stapes surgery.
In general, there were no adverse events reported during the period of this study. One of the rare complications of stapes surgery is the development of reparative granuloma, which involves an excessive inflammation that forms granulation tissue around the prosthesis and the oval window.45 Symptoms may develop within one to eight weeks after surgery and typically present as sensorineural hearing loss and vertigo.46 None of the participants involved in this study developed granulomatous reaction or any other complications as a result of the surgery.
The ratio of females to males in this study was 0.83:1, which is less than that reported in previous studies. It has been shown that females are affected more frequently than males, with a female-to-male ratio of 2:1.47 These differences perhaps are related to cultural differences where women in the region of the study are less likely to seek medical help than males. Overall results demonstrated that stapedotomy is a safe and effective treatment option for patients with otosclerosis. However, given the delicate nature of this surgical procedure, the experience of the surgeon could play a major role.48–50
In summary, our results demonstrated successful improvement in hearing thresholds following stapedotomy with a low rate of complications. None of the cases exhibited sensorineural hearing loss postoperatively. Therefore, these results suggest that stapedotomy can serve as a safe and effective treatment to ameliorate thresholds in otosclerotic patients and those with mixed hearing loss.
Acknowledgments
The authors would like to thank Dr. Abd El Aziz Yassin for helping in statistics, Dr. Mohammed Alshehri and Dr. Khaled Aloshish for their help in data collection. The project was supported by king Saud University, Deanship of Science Research, Prince Sultan Research Chair for Hearing Disability and Implantable Hearing Devices. This project was recommended by Saudi ORL society.
Footnotes
Conflict of interest
The authors declared no conflict of interest.
REFERENCES
- 1.Cureogle S, Baylan M, Paparell M. Cochlear otosclerosis. Curr Opin Otolaryngol Head Neck Surg. 2010;18:357–362. doi: 10.1097/MOO.0b013e32833d11d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Uppal S, Bajaj Y, Rustom I, Coatesworth AP. Otosclerosis: the aetiopathogenesis of otosclerosis. Int J Clin Pract. 2009;63:1526–30. doi: 10.1111/j.1742-1241.2009.02045.x. [DOI] [PubMed] [Google Scholar]
- 3.Probst R. Audiological evaluation of patients with otosclerosis. In: Arnold W, Hausler R, editors. Otosclerosis and stapes surgery. Adv Otorhinolaryngol. Vol. 65. Basel: Karger; 2007. pp. 119–126. [DOI] [PubMed] [Google Scholar]
- 4.Abdel-Ghany A, Osman N, Botros S. Correlation between the size, CT density of otosclerotic foci, and audiological tests in cases of otosclerosis. Int Adv Otol. 2014;10:156–61. [Google Scholar]
- 5.Kisilevsky VE, et al. Hearing results of 1145 stapedotomies evaluated with Amsterdam hearing evaluation plots. J Laryngol Otol. 2009;123:730–6. doi: 10.1017/S0022215109004745. [DOI] [PubMed] [Google Scholar]
- 6.Persson P, Harder H, Magnuson B. Hearing results in otosclerosis surgery after partial stapedectomy, total stapedectomy and stapedotomy. Acta Otolaryngol. 1997;117:94–9. doi: 10.3109/00016489709117998. [DOI] [PubMed] [Google Scholar]
- 7.Sedwick JD, Louden CL, Shelton C. Stapedectomy vs stapedotomy. Do you really need a laser? Arch Otolaryngol Head Neck Surg. 1997;123:177–80. doi: 10.1001/archotol.1997.01900020059008. [DOI] [PubMed] [Google Scholar]
- 8.Häusler R, Messerli A, Romano V, Burkhalter R, Weber HP, Altermatt HJ. Experimental and clinical results of fiberoptic argon laser stapedotomy. Eur Arch Otorhinolaryngol. 1996;253:193–200. doi: 10.1007/BF00171127. [DOI] [PubMed] [Google Scholar]
- 9.Sommer T, Vercruysse JP, Zarowski A, Verstreken M, Offeciers E. Stapedotomy with microdrill or carbon dioxide laser: influence on inner ear function. Ann Otol Rhinol Laryngol. 2006;115:880–885. doi: 10.1177/000348940611501203. [DOI] [PubMed] [Google Scholar]
- 10.Marchese MR, Paludetti G, De Corso E, Cianfrone F. Role of stapes surgery in improving hearing loss caused by otosclerosis. J Laryngol Otol. 2007;121:438–43. doi: 10.1017/S0022215106004257. [DOI] [PubMed] [Google Scholar]
- 11.Vincent R, Sperling NM, Oates J, Jindal M. Surgical findings and long-term hearing results in 3,050 stapedotomies for primary otosclerosis: a prospective study with the otology-neurotology database. Otol Neurotol. 2006;27:S25–47. doi: 10.1097/01.mao.0000235311.80066.df. [DOI] [PubMed] [Google Scholar]
- 12.Sparano A, Leonetti JP, Marzo S, Kim H. Effects of stapedectomy on tinnitus in patients with otosclerosis. Int Tinnitus J. 2004;10:73–7. [PubMed] [Google Scholar]
- 13.Ayache D, Earally F, Elbaz P. Characteristics and postoperative course of tinnitus in otosclerosis. Otolo Neurotolo. 2003;24:48–51. doi: 10.1097/00129492-200301000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Gros A, Vatovec J, Zargi M, Jenko K. Success rate in revision stapes surgery for otosclerosis. Otolo Neurotolo. 2005;26:1143–8. doi: 10.1097/01.mao.0000172414.64907.9d. [DOI] [PubMed] [Google Scholar]
- 15.Committee on Hearing and Equilibrium. Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. Otolaryngol Head Neck Surg. 1995;113:186–7. doi: 10.1016/S0194-5998(95)70103-6. [DOI] [PubMed] [Google Scholar]
- 16.Merán Gil JL, Masgoret Palau E, Avilés Jurado FJ, Domènech Vadillo E, Flores Martín JC, Figuerola Massana E. Stapedotomy outcomes in the treatment of otosclerosis: Our experience. Acta Otorrinolaringol Esp. 2008;59:448–54. [PubMed] [Google Scholar]
- 17.Tange RA, Grolman W. Late postoperative hearing results after stapedotomy. Int Adv Otol. 2009;5:323–6. [Google Scholar]
- 18.Thamjarayakul T, Supiyaphun P, Snidvongs K. Stapes Fixation surgery: Stapedectomy versus stapedotomy. Asian Biomedicine. 2010;4:429–434. [Google Scholar]
- 19.Baradaranfar MH, Dabirmoghaddam P. The hearing results in otosclerosis after stapedotomy. Acta Medica Iran. 2004;42:277–80. [Google Scholar]
- 20.Spandow O, Sodenberg O, Bohlin L. Long-term results in otosclerotic patients operated by stapedectomy or stapedotomy. Scand Audiol. 2000;29:186–90. doi: 10.1080/010503900750042752. [DOI] [PubMed] [Google Scholar]
- 21.De Bruijn AJG, Tange AT, Dreschler WA. Efficacy of evaluation of audiometric results after stapes surgery in otosclerosis. I. The effects of using different audiologic parameters and criteria on success rates. Otolaryngol Head Neck Surg. 2001;124:76–83. doi: 10.1067/mhn.2001.111601. [DOI] [PubMed] [Google Scholar]
- 22.House H, Hansen M, Aziz AA, Al D, House JW. Stapedectomy versus Stapedotomy: Comparison of Results with long-Term follow-up. Laryngoscope. 2002;112:2046–50. doi: 10.1097/00005537-200211000-00025. [DOI] [PubMed] [Google Scholar]
- 23.Dall’igna C, Texeira V, Dall’gna D, Rosito L. Results of stapes surgery for otosclerosis with two kinds of prosthesis in residency training. Braz J Otorhinolaryngol. 2008;74:826–32. doi: 10.1016/S1808-8694(15)30142-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vincent R, Sperling N, Oates J, Jindal M. Surgical findings and long-term hearing results in 3,050 stapedotomies for primary otosclerosis: A prospective study with the otology-neurotology database. Otology & Neurotology. 2006;27:S25–S47. doi: 10.1097/01.mao.0000235311.80066.df. [DOI] [PubMed] [Google Scholar]
- 25.De Bruijn A, Tange R, Dreschler W. Efficacy of evaluation of audiometric results after stapes surgery in otosclerosis. II. A method for reporting results from individual cases. Otolaryngol Head Neck Surg. 2001;124:84–9. doi: 10.1067/mhn.2001.111600. [DOI] [PubMed] [Google Scholar]
- 26.Gantz BJ, Jenkins HA, Kishimoto S, Fisch U. Argon laser stapedotomy. Ann Otol Rhinol Laryngol. 1982;91:25–26. doi: 10.1177/000348948209100107. [DOI] [PubMed] [Google Scholar]
- 27.Marcos V, Goycoolea M. Otosclerosis. In: Paparella MM, editor. Otolaryngology. 3rd ed. Philadelphia: WB Saunders; 1991. pp. 1489–1522. [Google Scholar]
- 28.House JW. Otosclerosis. In: Cummings CW, editor. Otolaryngology head and neck surgery. 3rd ed. Baltimore: Mosby; 1998. pp. 3126–3135. [Google Scholar]
- 29.Bauchet St, Martin M, Rubinstein EN, Hirsch BE. High-frequency sensorineural hearing loss after stapedectomy. Otol Neurotol. 2008;29:447–52. doi: 10.1097/MAO.0b013e318172d6a3. [DOI] [PubMed] [Google Scholar]
- 30.Strömbäck K, Köbler S, Rask-Andersen High frequency hearing following stapes surgery. Acta Otolaryngol. 2012;132:944–50. doi: 10.3109/00016489.2012.677859. [DOI] [PubMed] [Google Scholar]
- 31.Bagger-Sjöbäck D, Strömbäck K, Hultcrantz M, Papatziamos G, Smeds H, Danckwardt-Lillieström N, Tideholm B, Johansson A, Hellström S, Hakizimana P, Fridberger A. High-frequency hearing, tinnitus, and patient satisfaction with stapedotomy: A randomized prospective study. Sci Rep. 2015;5:13341. doi: 10.1038/srep13341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Babighian G, Albu S. Failures in stapedotomy for otosclerosis. Otolaryngology-Head and Neck surgery. 2009;141:395–400. doi: 10.1016/j.otohns.2009.03.028. [DOI] [PubMed] [Google Scholar]
- 33.Carhart R. Clinical application of bone conduction audiometry. Arch Otolaryngol. 1950;51:798–808. doi: 10.1001/archotol.1950.00700020824003. [DOI] [PubMed] [Google Scholar]
- 34.Awengen DF. Change of bone conduction thresholds by total footplate stapedectomy in relation to age. Am J Otalaryngol. 1993;14:105–110. doi: 10.1016/0196-0709(93)90048-c. [DOI] [PubMed] [Google Scholar]
- 35.Aarnisalo AA, Vasama JP, Hopsu E, Ramsay H. Long-term hearing results after stapes surgery: a 20-year follow-up. Otol Neurotol. 2003;24:567–571. doi: 10.1097/00129492-200307000-00006. [DOI] [PubMed] [Google Scholar]
- 36.Quaranta N, Besozzi G, Fallacara RA, Quaranta A. Air and bone conduction change after stapedotomy and partial stapedectomy for otosclerosis. Otolaryngol Head Neck Surg. 2005;133:116–120. doi: 10.1016/j.otohns.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 37.Moscillo L, Imperiali M, Carra P, Catapano F, Motta G. Bone conduction variation poststapedotomy. Am J Otolaryngol. 2006;27:330–333. doi: 10.1016/j.amjoto.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 38.Tonndorf J. Bone conduction hearing. In: Keidel WD, NeV WD, editors. Handbook of sensory physiology. Springer; Berlin: 1994. pp. 172–247. [Google Scholar]
- 39.Bailey Hat, Jr, Pappas J, Graham S. Small fenestra stapedectomy technique: reducing risk and improving hearing. Otolaryngol Head Neck Surg. 1983;91:516–20. doi: 10.1177/019459988309100508. [DOI] [PubMed] [Google Scholar]
- 40.Engel T, Schindler R. Stapedectomy in residency training. Laryngoscope. 1984;94:768–71. doi: 10.1288/00005537-198406000-00007. [DOI] [PubMed] [Google Scholar]
- 41.Chandler J, Rodriguez-Torro O. Changing patterns of Otosclerosis surgery in teaching institutions. Otolaryngol Head Neck Surg. 1983;91:239–45. doi: 10.1177/019459988309100307. [DOI] [PubMed] [Google Scholar]
- 42.Elonka D, Derlacki E, Harrison W. Stapes prosthesis comparison. Otolaryngol Head Neck Surg. 1982;90:263–5. doi: 10.1177/019459988209000222. [DOI] [PubMed] [Google Scholar]
- 43.Berliner KI, Jo Doyle KJ, Goldenberg RA. Reporting Operative Hearing Results in Stapes Surgery: Does Choice of Outcome Measure Make a Difference? Otology & Neurotology. 1996;17:214–220. [PubMed] [Google Scholar]
- 44.Rondini-Gilli E, Bozorg Grayeli A, Boutin P, Tormin Borges Crosara PF, Mosnier I, Bouccara D, Cyna-Gorse F, Rufat P, Sterkers O. Otosclerosis surgical techniques and results in 150 patients. Ann Otolaryngol Chir Cervicofac. 2002;119:227–33. [PubMed] [Google Scholar]
- 45.Yonamine FK, Segalla DK, Antunes ML. Post-stapedotomy granulomatous reaction. Braz J Otorhinolaryngol. 2010;76:138. doi: 10.1590/S1808-86942010000100024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Parelkar K, Nagle S, Jagade M, Khairnar P, Pandare M, Nataraj R, Hanwate R, Nagrale B, Rangaraja D. Post-Stapedectomy Granuloma: A rare case report. Journal of Otolaryngology and Head & Neck Surgery. 2015;4:273–276. [Google Scholar]
- 47.Roland P. Otosclerosis. In: Baily BJ, editor. Head and neck surgery: otolaryngology. 3rd ed. Philadelphia: Lippincott William Wilkins; 2001. pp. 1829–1841. [Google Scholar]
- 48.Puxeddu R, Ledda GP, Pelagatti CL, Salis G, Agus G, Puxeddu P. Revision stapes surgery for recurrent transmissional hearing loss after stapedectomy and stapedotomy for otosclerosis. Acta Otorhinolaryngol Ital. 2005;25:347–352. [PMC free article] [PubMed] [Google Scholar]
- 49.Shiao AS, Kuo CL, Cheng HL, Wang MC, Chu CH. Controversial issues of optimal surgical timing and patient selection in the treatment planning of otosclerosis. Eur Arch Otorhinolaryngol. 2014;271:1007–14. doi: 10.1007/s00405-013-2529-6. [DOI] [PubMed] [Google Scholar]
- 50.Gerard JM, Serry P, Gersdorff MC. Outcome and lack of prognostic factors in stapes surgery. Otol Neurotol. 2008;29:290–94. doi: 10.1097/mao.0b013e318161ab0f. [DOI] [PubMed] [Google Scholar]