Abstract
Background:
Studies comparing acetabular labral repair with debridement have generally demonstrated better clinical outcomes with repair. However, it is not clear whether hip arthroscopic surgeons agree on the indications for labral repair and debridement, bringing the generalizability of these (and future) studies into question.
Purpose:
To investigate surgical decision making for acetabular labral tears, with a specific focus on indications for repair or debridement, by performing an international survey of hip arthroscopic surgeons.
Study Design:
Cross-sectional study.
Methods:
A total of 35 hip arthroscopic surgeons from around the world were invited to participate in this survey study. Surgeons selected the factors that they consider when deciding to repair or debride acetabular labral tears. For each variable selected, computerized adaptive logic prompted additional questions to better define how that variable affects decision making. Six deidentified intraoperative videos of a variety of labral tears were included to determine the level of agreement between the experts on which labral tears are repairable.
Results:
The survey response rate was 86%. A majority (77%) of hip arthroscopic surgeons selected the intraoperative appearance of the labrum as the most important factor affecting their decision making. Specific factors affecting surgical decision making included pattern of the labral tear (73% of surgeons), ossification of the labrum (70%), magnetic resonance imaging findings (70%), patient age (63%), activity level (57%), radiographic findings (53%), calcification of the labrum (50%), and thickness of the labrum (47%). Three intraoperative videos had ≥90% agreement for labral repair, while the other 3 had ≤76% agreement.
Conclusion:
The intraoperative appearance of the labrum is the most important factor affecting surgical decision making. However, different surgeons viewing the same tear arthroscopically may select different treatments. The indications to repair a torn acetabular labrum are highly variable among hip arthroscopic surgeons.
Keywords: hip/pelvis/thigh, hip arthroscopic surgery, femoroacetabular impingement, groin pain
In the past decade of the rapid growth of arthroscopic hip surgery, there has been a paradigm shift away from debridement of symptomatic acetabular labral tears and toward preservation of the labrum. The driving force behind this shift is better understanding of the multiple functions of the labrum.27 This includes biomechanical studies demonstrating increased contact stress on the femoral head and acetabular articular cartilage after removal of the labrum,10 clinical studies showing improved outcomes with labral repair versus debridement,8,14,16,23,29 and improved surgical instrumentation and techniques. It is not clear when evaluating hip arthroscopic surgery outcome studies, however, if different surgeons are repairing and/or debriding the same tears. Further, the question “Which labral tears are appropriate for repair and which should be debrided?” has not been definitively answered.
Hip arthroscopic surgeons may weigh several different factors in making their decision to repair or debride labral tears. Some of these factors, such as patient age, sex, activity level, duration of symptoms, and imaging findings, are known before entering the operating room, while others, such as the pattern of the tear and quality of the tissue, are discovered at the time of hip arthroscopic surgery. The importance of each of these factors to the decision making of hip arthroscopic surgeons has not previously been investigated. The purpose of this study was to investigate surgical decision making for acetabular labral tears, with a specific focus on indications for repair or debridement, among an international cohort of hip arthroscopic surgeons. We hypothesized that the intraoperative appearance of the labrum is the most important factor affecting surgical decision making.
Methods
A 36-question survey featuring computerized adaptive testing was designed using Qualtrics software. A minimum of 13 questions had to be answered to complete the survey. After obtaining institutional review board approval, the survey was distributed to 35 surgeons via email. These surgeons are all active members of the International Society for Hip Arthroscopy and participate in several other national and international societies (eg, American Orthopaedic Society for Sports Medicine; European Society of Sports Traumatology, Knee Surgery & Arthroscopy; Asia-Pacific Knee, Arthroscopy and Sports Medicine Society). Invited participants were initially given 30 days to complete the survey. Automated reminder emails were sent 2 weeks and 4 weeks after the initial invitation to surgeons who had not yet completed the survey. After 6 weeks, 18 of the invited surgeons had responded, which was determined to be an inadequate response rate. Therefore, the remaining nonrespondents were sent a personalized email from the senior author (M.R.S.), requesting their participation. The survey was finally closed 56 days after the initial email invitation.
Surgeon demographic data were collected, including geographic location, practice setting, number of years performing hip arthroscopic surgery, and estimated number of hip arthroscopic procedures per year. The senior author, who has over 20 years of experience performing hip arthroscopic surgery, created a list of potential factors affecting surgical decision making for acetabular labral tears. The survey asked the surgeons to select those factors that they consider when deciding whether to repair or debride acetabular labral tears. For each variable selected, computerized adaptive logic prompted additional questions to better define how that variable affects their decision making.
Multiple-choice questions were designed for categorical variables, such as patient sex and the Hip Sports Activity Scale (HSAS),31 while a sliding ruler was used to answer continuous variables, such as age, thickness of the labrum, and lateral center-edge angle (LCEA). Because magnetic resonance imaging (MRI) findings and computed tomography (CT) findings for acetabular labral tears may vary widely, surgeons incorporating these variables into their decision making were prompted to explain how these findings affect their decision making in free text. To determine the level of agreement between hip arthroscopic surgeons on which labral tears are repairable based on findings at diagnostic arthroscopic surgery, 6 deidentified intraoperative videos of a variety of labral tears were uploaded into YouTube to ensure viewing compatibility and were linked with the survey. After viewing each video, surgeons were asked to choose whether they would debride or repair each labral tear. Surgical indications for labral reconstruction were outside the scope of this study; therefore, surgeons who would debride the tear and then reconstruct the labrum were instructed to select “debride.”
Statistical analysis was conducted using Fisher exact tests and t tests to explore associations between surgeon demographics and variables affecting surgeon decision making, with Bonferroni correction for multiple analyses. Because of the lack of variance and skewed nature of the responses, we did not calculate kappa values for the intraoperative videos. All analyses were performed using the statistical computing package R.25,26 The survey questions, including branching logic for completing the survey, are listed in the Appendix.
Results
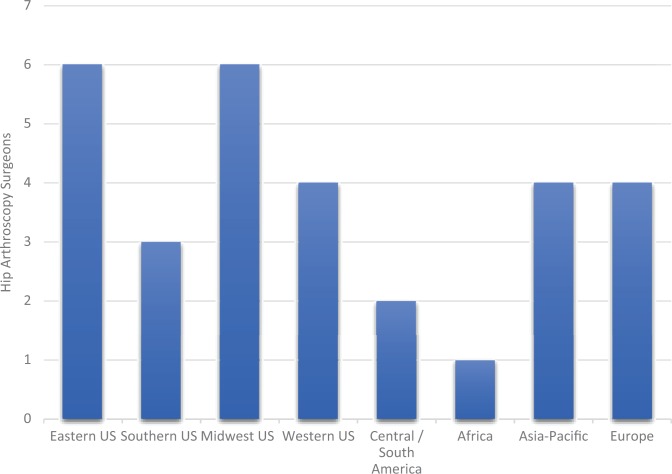
Thirty-two international hip arthroscopic surgeons took the survey. Two surgeons completed only the demographic questions and were excluded from the study, yielding an overall response rate of 86%. One surgeon did not complete the video analysis portion of the survey. The mean number of questions answered using branching logic was 22.3 ± 5.2 (range, 13-35). Fourteen (47%) surgeons were in private practice, 15 (50%) worked at a university, and 1 (3%) was employed at a hospital. The surgeons had a mean of 16.13 years of experience (range, 3-33 years) performing hip arthroscopic surgery and estimated performing a mean of 273 hip arthroscopic procedures per year (range, 80-600; median, 249). The geographic locations of participating surgeons are recorded in Figure 1.
Figure 1.
Geographic distribution of hip arthroscopic surgeons.
Four preoperatively known factors were identified as important to decision making of at least 50% of the hip arthroscopic surgeons: MRI or magnetic resonance arthrography (MRA) findings, age, activity level, and radiographic findings (Table 1). Patient sex was considered important by only 1 of the surgeons (3%).
TABLE 1.
Hip Arthroscopic Surgeons’ Responses to the Following Question: “Which of the Following Preoperatively Known Factors Influence Your Decision Whether to Repair a Tear of the Acetabular Labrum (Select All That Apply)?”
| Preoperatively Known Factor | Surgeons Who Selected the Factor as Important in Their Decision Making, n (%) |
|---|---|
| Magnetic resonance imaging findings | 21 (70) |
| Age | 19 (63) |
| Activity level | 17 (57) |
| Radiographic findings | 16 (53) |
| Computed tomography findings | 9 (30) |
| Chronicity of the tear by patient history | 6 (20) |
| Sex | 1 (3) |
Of the 21 hip arthroscopic surgeons who chose MRI/MRA findings as an important variable, 20 provided a written explanation to the following prompt: “Describe how MRI/MRA influences your decision to repair or debride a labral tear.” Nine of the 20 responses referred to the amount of arthritis in the joint, while 6 surgeons looked for either labral degeneration or ossification.
The 19 surgeons who chose age as an important factor selected a mean patient age of 52 ± 9.08 years (range, 30-60 years) as the age below which they favored repair over debridement and a mean age of 54 ± 6.41 years (range, 40-60 years) as the age above which they favored debridement over repair of labral tears. The 17 surgeons who considered patient activity level in their decision making were asked to select the HSAS score31 above which they favored labral repair. Ten selected level 0 (no recreational or competitive sports), 6 selected level 1 (recreational sports: swimming, cycling, hiking, Nordic walking), and 1 selected level 6 (competitive sports [elite level]: golf, bicycle racing, mountain biking, swimming, rowing, cross-country skiing, biathlon, horseback riding, cricket, dancing, figure skating, rock climbing, fencing, OR competitive sports [minor league/collegiate]: downhill skiing, snowboarding).
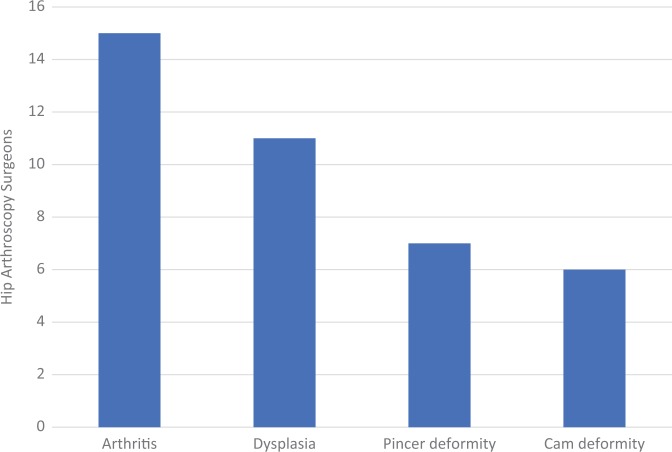
The 16 international hip arthroscopic surgeons who chose radiographic findings as an important factor were queried as to which radiographic findings influenced their decision making (Figure 2).
Figure 2.
Sixteen of 30 hip arthroscopic surgeons who selected “radiographic findings” as an important factor were asked the following: “Please indicate which radiographic findings influence your decision to repair or debride a labral tear (select all that apply).”
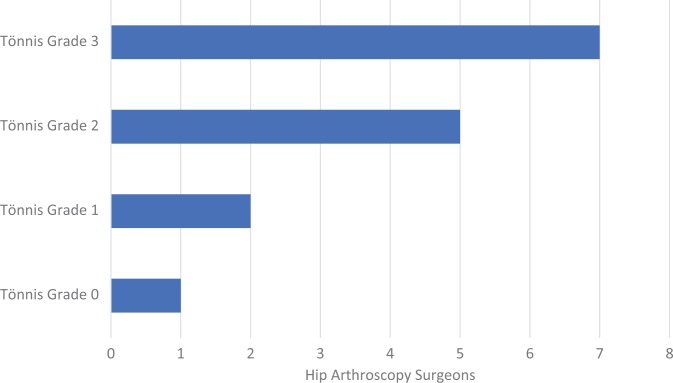
Fifteen surgeons selected “arthritis” as an important radiographic finding. These surgeons then selected the Tönnis grade at and above which they favored debridement over repair. Most surgeons selected Tönnis grade 2 or 3 (Figure 3).
Figure 3.
Fifteen hip arthroscopic surgeons who selected “arthritis” as a radiographic finding influencing their treatment of acetabular labral tears were asked the following: “Please select the Tönnis grade at and above which you favor labral debridement over repair.”
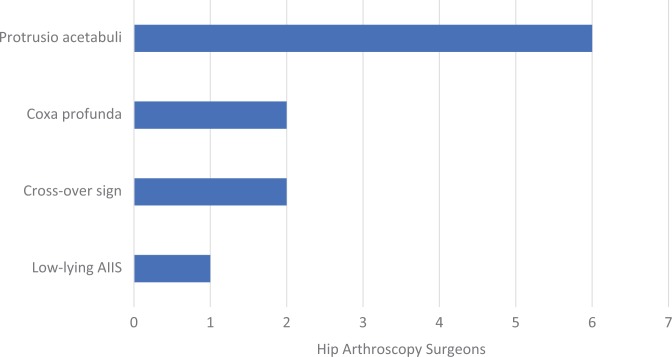
Eleven surgeons chose “dysplasia” as an important radiographic finding. These surgeons chose a mean LCEA of 24.55° (range, 20°-25°) as the LCEA below which they favored repair over debridement. Seven surgeons selected “pincer deformity” as an important radiographic finding. The mean LCEA above which these surgeons favored labral debridement over repair was 43.71° (range, 26°-50°). These 7 surgeons were also asked to choose which pincer deformities caused them to favor labral debridement over repair. Protrusio acetabuli was the most commonly chosen pincer deformity for which labral debridement was the favored treatment (Figure 4).
Figure 4.
Seven hip arthroscopic surgeons who selected “pincer deformity” as a radiographic finding influencing their treatment of acetabular labral tears were asked the following: “For which pincer deformities do you favor labral debridement over repair (select all that apply)?” AIIS, anterior inferior iliac spine.
Six surgeons who chose “cam deformity” as an important radiographic finding answered that the mean alpha angle above which they favored labral debridement over repair was 60° ± 19.84° (range, 40°-80°).
Four intraoperative diagnostic arthroscopic surgery findings were identified as important to decision making of at least 47% of the hip arthroscopic surgeons: the pattern of the labral tear (Seldes classification), ossification within the labrum, calcification within the labrum, and thickness of the labrum at the site of the tear (Table 2).
TABLE 2.
Hip Arthroscopic Surgeons’ Responses to the Following Question: “After Performing Diagnostic Arthroscopic Surgery of the Hip, Which of the Following Characteristics of the Labral Tear Affect Your Decision to Repair or Debride the Tear (Select All That Apply)?”
| Diagnostic Arthroscopic Surgery Finding | Surgeons Utilizing This Finding for Intraoperative Decision Making, n (%) |
|---|---|
| Pattern of the tear (chondrolabral separation vs intrasubstance) | 22 (73) |
| Ossification within the labrum | 21 (70) |
| Calcification within the labrum | 15 (50) |
| Thickness of the labrum at the site of the tear | 14 (47) |
| Length of the tear along the acetabular rim | 10 (33) |
| Yellow discoloration of the labrum | 9 (30) |
| Location of the tear on the acetabular rim | 9 (30) |
| Cartilage delamination adjacent to the labral tear | 9 (30) |
| Os acetabuli adjacent to the labral tear | 6 (20) |
| Bruising/inflammation/redness of the labrum | 4 (13) |
Twenty-one of 22 surgeons (95%) stated that they were more likely to repair a chondrolabral separation, while 1 (5%) was more likely to repair an intrasubstance tear. Seventeen of 21 surgeons (81%) stated that they were more likely to debride an ossified labral tear, in contrast with 4 (19%) who selected repair. Eight of 15 surgeons (53%) stated that they were more likely to repair a labral tear with intrasubstance calcification, while 7 (47%) were more likely to debride calcified labral tears. Fourteen surgeons (47%) who chose thickness as an important factor selected a mean of 2.93 ± 1.64 mm (range, 0.4-5.1 mm) as the minimum thickness of the labrum required to perform labral repair.
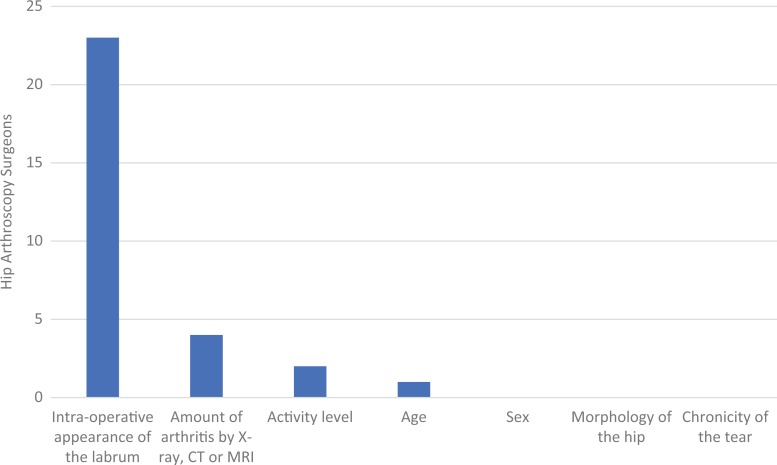
Twenty-three surgeons (77%) selected “intraoperative appearance of the labrum” as the single most important factor affecting their decision to repair or debride a labral tear (Figure 5).
Figure 5.
Hip arthroscopic surgeons’ responses to the following question: “When deciding whether to repair an acetabular labral tear, what is the single most important factor affecting your decision (select one)?” CT, computed tomography; MRI, magnetic resonance imaging.
The surgeons favored repair over debridement for each of the 6 acetabular labral tears demonstrated by intraoperative video, with varying levels of agreement. Three cases had repair as the preferred choice by ≥90% of surgeons, and 1 case had nearly equal preference for repair and for debridement (Table 3).
TABLE 3.
Hip Arthroscopic Surgeons’ Responses as to Whether They Would “Repair” or “Debride” the Acetabular Labral Tears Demonstrated in Each Intraoperative Video
| Repair, n (%) | Debride, n (%) | |
|---|---|---|
| Video 1: https://youtu.be/h3qBvbKbceU | 27 (93.1) | 2 (6.9) |
| Video 2: https://youtu.be/Gh3QgtOAGow | 21 (72.4) | 8 (27.6) |
| Video 3: https://youtu.be/hfrPtMkMee0 | 15 (51.7) | 14 (48.3) |
| Video 4: https://youtu.be/1iPfNjK6eSk | 28 (96.5) | 1 (3.5) |
| Video 5: https://youtu.be/dIqXdlXqICg | 22 (75.9) | 7 (24.1) |
| Video 6: https://youtu.be/8PwKtuOjlB0 | 26 (89.7) | 3 (10.3) |
Statistical analysis revealed no statistically significant associations between surgeon demographics and which variables were selected as important to surgical decision making.
Discussion
The purpose of this study was to investigate surgical decision making by international hip arthroscopic surgeons for acetabular labral tears, with a specific focus on indications for debridement versus repair. A previous survey study of 27 hip arthroscopic surgeons by Gupta et al11 found an estimated labral repair rate of 77%, with a wide range of responses (20%-100%). However, that study did not ask the surgeons how they made their decision to repair or debride labral tears. The results of this study confirmed our hypothesis that the intraoperative appearance of the labrum is the single most important factor affecting hip arthroscopic surgeons’ decision to repair or debride a tear of the acetabular labrum. This finding parallels decision making in the treatment of meniscal tears of the knee, in which diagnostic arthroscopic surgery is the gold standard for evaluating tear patterns and guiding treatment.22
Our study of surgical decision making for acetabular labral tears revealed several interesting findings when compared with published treatment algorithms. Philippon et al24 published an acetabular labral tear treatment algorithm in 2012 based exclusively on the intraoperative findings of labral size (small or large) and whether the labrum was detached, degenerated, bruised, or torn. In our study, 77% of international hip arthroscopic surgeons selected the intraoperative appearance of the labrum as the most important factor affecting their decision, and 73% considered the pattern of the labral tear in their decision making, consistent with the algorithm by Philippon et al24 of “detached,” “degenerated,” or “torn” variables. However, only 47% of international hip arthroscopic surgeons utilized thickness of the labrum in their decision making, and only 13% considered bruising of the labrum to be an important variable. A more recent algorithm published by Domb et al7 in 2017 included patient age, stability of the labrum, quality and vascularity of the labrum, and amount of calcification of the labrum as important variables to consider. Our study reveals that the majority of surgeons agreed with the variables selected for this algorithm. Age was selected as an important factor by 63% of the surgeons, while ossification and calcification of the labrum were deemed important by 70% and 50% of surgeons, respectively.
One interesting finding of our study was the lack of agreement between surgeons regarding the treatment of labral tears with intrasubstance calcification. Of the 15 surgeons who factored calcification of the labrum into their decision making, 53% favored repair versus 47% who favored debridement. One explanation for this finding is that the amount of intrasubstance calcification may vary widely between different cases, and our survey did not inquire as to where the critical threshold lies. Another explanation could be that a paucity of literature exists to guide the treatment of calcified labral tears because, to our knowledge, there is only 1 report of 2 cases of endoscopic debridement of calcified labral tears, which showed good results with debridement in both cases.30 Another noteworthy finding was that there was excellent agreement among surgeons regarding the treatment of ossified labral tears, for which 81% selected “debride” in our study. This is most likely because labral ossification replaces labral tissue, leaving minimal, if any, labral cartilage to repair and/or function.
Hip arthroscopic surgery is one of the most rapidly developing fields of orthopaedic surgery in the United States and across the world.1,6,18,19,21,32 Up to 92% of patients undergoing hip arthroscopic surgery for femoroacetabular impingement (FAI) will have a tear of the acetabular labrum.23 Although good results have been reported with debridement of acetabular labral tears in patients without arthritis,2,3,9,13,28 most comparative studies have shown better outcomes with labral repair compared with debridement.
Espinosa et al8 in 2006 were the first to show improved outcomes with labral refixation over debridement in patients who underwent open surgical dislocation for the treatment of FAI. Retrospective cohort studies by Larson et al,15,16 Philippon et al,23 Schilders et al,29 and Kalore and Jiranek12 all showed better outcomes with arthroscopic labral repair versus debridement, while Cetinkaya et al4 found no difference in outcome scores between the 2 treatments. One prospective randomized controlled trial compared labral repair to debridement in 36 female patients; Krych et al14 found the postoperative Hip Outcome Score for sports and activities of daily living to be significantly better in the repair group versus the debridement group, with a greater number of patients rating their hip as normal or near normal in the repair group. As a consequence of these studies, and with most studies demonstrating important functions of the labrum,27 labral repair has been recommended over debridement “when appropriate.”29 Which labral tears meet this criterion, however, has not been definitively established.
One limitation of the current literature on labral repair versus debridement is that 3 of the 5 studies comparing these treatment options excluded patients with Tönnis grade 2 and 3 arthritis.4,14,29 Retrospective reviews on outcomes of hip arthroscopic surgery have reported debridement as the predominant treatment of labral tears in patients with at least Tönnis grade 2 arthritis.5,17 A recently published 10-year follow-up study of patients treated with labral repair or debridement showed no significant difference in the rate of conversion to total hip arthroplasty or outcome scores when controlling for preoperative joint space, age, and acetabular microfracture.20 In our study, 13% of hip arthroscopic surgeons selected the amount of arthritis by radiography, CT, or MRI/MRA as the single most important factor affecting their decision to repair or debride a labral tear. However, the surgeons’ responses regarding what level of arthritis is an indication for labral debridement differed (see Figure 3).
Because it was expected that the intraoperative appearance of the labrum would influence a surgeon’s decision on whether to repair, we presented deidentified surgical videos from 6 hip arthroscopic surgery cases demonstrating labral tears. This was meant to further help identify if indications for acetabular labral repair differ between hip arthroscopic surgeons when viewing the same tear. Three cases had ≥90% agreement to repair, while the other 3 cases had more disparate responses, including 1 case (case 3) that was nearly equal in preference for repair or debridement. This suggests that there is a lack of consensus on reparability, which needs to be considered in evaluating hip arthroscopic surgery outcome studies comparing labral repair with debridement.
This is the first study to demonstrate variability in the indications for acetabular labral repair or debridement among an international cohort of hip arthroscopic surgeons. The strengths of our study are the inclusion of hip arthroscopic surgeons from around the world and the excellent response rate (86%) of the survey. The use of computerized adaptive logic allowed us to inquire about a large number of potential decision-making factors (17 in total) and then focus subsequent questions on only the selected factors, maximizing efficiency for survey participants. Less than 10 minutes was required to complete the survey. Finally, the questions regarding the 6 arthroscopic videos of labral tears simulate “real-world” decision making, affording a context to the other survey responses, and highlight a small number of tear patterns in which hip arthroscopic surgeons agree and disagree.
There are limitations to our study that merit consideration. First, the hip arthroscopic surgeons invited to participate in our study were limited to those identified by the senior author, which subjects our results to selection bias. Undoubtedly, there are high-volume hip arthroscopic surgeons who were not included and whose responses would have increased our number of data points. Second, the survey was conducted in English, not translated into the native languages of our international cohort of surgeons. Third, the survey was not formally validated, and some of the survey questions may have been better worded to improve comprehension and clarity. Fourth, our study did not investigate the indications for labral reconstruction, which some surgeons may perform primarily instead of labral repair or debridement. The survey also did not ask surgeons if they perform labral reconstruction. Surgeons who do not perform labral reconstruction may be more cautious with labral debridement and more aggressive with repair, while the opposite may be true for surgeons who do perform labral reconstruction. Finally, the 6 labral tears demonstrated in the intraoperative videos of our study represent a mere fraction of the wide-ranging morphologies of acetabular labrum tears. Although the survey could have included several more intraoperative videos, this would, by necessity, have increased the time required to complete the survey, but the limitation of not including every possible acetabular labral tear morphology would still exist.
In conclusion, the intraoperative appearance of the labrum is the most important factor affecting surgical decision making. However, different surgeons viewing the same tear arthroscopically may select different treatments. The indications to repair a torn acetabular labrum are highly variable among hip arthroscopic surgeons. This variability in surgical decision making should be considered when evaluating studies comparing acetabular labral repair to debridement.
Acknowledgment
The authors acknowledge Andrea K. Finlay, PhD, for her assistance with the statistical analyses for this study. The authors also acknowledge and thank the many hip arthroscopic surgeons worldwide who participated in this study.
Appendix
Survey Questions, Answers, and Branching (Computerized Adaptive) Logic
- Where is your hip arthroscopic surgery practice located?
- Eastern US
- Southern US
- Midwestern US
- Western US
- Canada
- Central/South America
- Africa
- Asia-Pacific
- Europe
- Please choose the option that most closely identifies your practice setting.
- University
- Private practice
- Hospital
Approximately how many years have you been performing hip arthroscopic surgery?
Approximately how many hip arthroscopic surgery cases do you perform each year?
- Which of the following preoperatively known factors influence your decision whether to repair a tear of the acetabular labrum (select all that apply)?
- Age
- Sex
- Activity level
- Chronicity of the tear by patient history
- Radiographic findings
- CT findings
- MRI/MRA findings
If age chosen: Slide the ruler to the age below which you favor repair over debridement AND slide the ruler to the age above which you favor debridement over repair.
If sex chosen: Are you more likely to repair the labrum in a female patient or a male patient?
- If activity level chosen: Please select the HSAS score above which you favor labral repair over debridement.
- Level 8: Competitive sports (elite level): soccer, ice hockey, field hockey, American football, rugby, martial arts, tennis, track and field, beach volleyball, lacrosse, baseball, softball, water polo, synchronized swimming, weight lifting, wrestling, gymnastics, bobsled, basketball, volleyball, squash, racquetball, handball, badminton
- Level 7: Competitive sports (elite level): downhill skiing, snowboarding. Competitive sports (minor league, collegiate): soccer, ice hockey, field hockey, American football, rugby, martial arts, tennis, track and field, beach volleyball, lacrosse, baseball, softball, water polo, synchronized swimming, weight lifting, wrestling, gymnastics, bobsled, basketball, volleyball, squash, racquetball, handball, badminton
- Level 6: Competitive sports (elite level): golf, bicycle racing, mountain biking, swimming, rowing, cross-country skiing, biathlon, horseback riding, cricket, dancing, figure skating, rock climbing, fencing. Competitive sports (minor league, collegiate): downhill skiing, snowboarding
- Level 5: Competitive sports (minor league, collegiate): golf, bicycle racing, mountain biking, swimming, rowing, cross-country skiing, biathlon, horseback riding, cricket, dancing, figure skating, rock climbing, fencing
- Level 4: Recreational sports: tennis, downhill skiing, snowboarding, baseball, softball, water polo, synchronized swimming, wrestling, gymnastics, bobsled, running (marathon), CrossFit, basketball, volleyball, squash, racquetball, handball, badminton
- Level 3: Recreational sports: aerobics, jogging, lower extremity sports, weight lifting, horseback riding, cricket
- Level 2: Recreational sports: golf, bicycle racing, mountain biking, swimming, rowing, cross-country skiing, biathlon, dancing, inline skating, rock climbing, fencing
- Level 1: Recreational sports: swimming, cycling, hiking, Nordic walking (quick walking with ski poles)
- Level 0: No recreational or competitive sports
If chronicity of the tear by patient history chosen: Slide the ruler to indicate the number of weeks from the injury or onset of symptoms before which you favor repair over debridement.
If chronicity of the tear by patient history chosen: Slide the ruler to indicate the number of months from the injury or onset of symptoms after which you favor debridement over repair.
- If radiographic findings chosen: Please indicate which radiographic findings influence your decision whether to repair the labrum (select all that apply).
- Arthritis
- Dysplasia
- Pincer deformity
- Cam deformity
If arthritis chosen: Please select the Tönnis grade at and above which you favor labral debridement over repair (0, 1, 2, or 3).
If dysplasia chosen: For patients with dysplasia, below what LCEA do you favor labral repair over debridement (slide the ruler to select)?
If pincer deformity chosen: For patients with pincer-type FAI, above what LCEA do you favor labral debridement over repair (slide the ruler to select)?
- If pincer deformity chosen: Which of the following pincer deformities trigger you to favor labral debridement over repair (select all that apply)?
- Cross-over sign
- Low-lying anterior inferior iliac spine
- Coxa profunda
- Protrusio acetabuli
If cam deformity chosen: For patients with cam-type FAI, above what alpha angle do you favor labral debridement over repair (slide ruler to select)?
If CT findings chosen: Describe how CT influences your decision to repair or debride a labral tear.
If MRI findings chosen: Describe how MRI/MRA influences your decision to repair or debride a labral tear.
- After performing diagnostic arthroscopic surgery of the hip, which of the following characteristics of the labral tear affect your decision to repair or debride the tear (select all that apply)?
- Pattern of the labral tear (chondrolabral separation vs intrasubstance tear)
- Length of the tear along the acetabular rim
- Location of the tear on the acetabular rim
- Thickness of the labrum at the site of the tear
- Calcification within the labrum
- Ossification within the labrum
- Os acetabuli adjacent to the labral tear
- Cartilage delamination adjacent to the labral tear
- Bruising/inflammation/redness of the labrum
- Yellow discoloration of the labrum
If pattern of the labral tear chosen: Which tear pattern are you more likely to repair (chondrolabral separation or intrasubstance tear)?
If length of the tear along the acetabular rim chosen: Slide the ruler to select labral tear length (in cm) above which you favor labral debridement over repair.
If location of the tear on the acetabular rim chosen: Select the location(s) on the acetabular rim where you favor labral repair over debridement (anterior, anterolateral, lateral, posterolateral, posterior).
If thickness of the labrum at the site of the tear chosen: Select the minimum thickness of the labrum (in mm) that you require to perform labral repair.
If calcification within the labrum chosen: Are you more likely to repair or debride a labral tear with intrasubstance calcification?
If ossification within the labrum chosen: Are you more likely to repair or debride an ossified labral tear?
If os acetabuli adjacent to the labral tear chosen: Are you more likely to repair or debride a labral tear adjacent to os acetabuli?
If cartilage delamination adjacent to the labral tear chosen: Are you more likely to repair or debride a tear with adjacent cartilage damage?
If bruising/inflammation/redness of the labrum chosen: Are you more likely to repair or debride a tear with inflammation/redness/bruising?
If yellow discoloration of the labrum chosen: Are you more likely to repair or debride a tear with yellow discoloration?
- When deciding whether to repair an acetabular labral tear, what is the single most important factor affecting your decision (select one)?
- Age
- Sex
- Activity level
- Chronicity of the tear by patient history
- Amount of arthritis on radiography, CT, or MRI
- Morphology of the hip joint on radiography, CT, or MRI
- Intraoperative appearance of the labrum
31-36. For each of the next 6 questions, click on the link to view the video of a labral tear and then choose if you would repair or debride the tear. If you would debride the tear and then perform reconstruction, please choose debride. If you want to replay the video, click the icon in the lower left of the screen. Note: all videos were taken while viewing from the posterolateral portal with a 70° arthroscope.
Footnotes
One or more of the authors has declared the following potential conflict of interest and source of funding: P.K.H. has received educational funding from Linvatec and hospitality payments from Smith & Nephew. M.R.S. has received research funding from Ferring Pharmaceuticals, ISAKOS, and ConMed Linvatec; has received fellowship funding from Smith & Nephew, Ossur, ConMed Linvatec, and Biomet; is a consultant for Medacta and Smith & Nephew; and receives royalties from Stryker, DJ Orthopedics, Smith & Nephew, and Howmedica. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by Stanford University.
References
- 1. Bozic KJ, Chan V, Valone FH, Feeley BT, Vail TP. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28(suppl 8):140–143. [DOI] [PubMed] [Google Scholar]
- 2. Byrd JWT, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy. 2009;25(4):365–368. [DOI] [PubMed] [Google Scholar]
- 3. Byrd JWT, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16(6):578–587. [DOI] [PubMed] [Google Scholar]
- 4. Cetinkaya S, Toker B, Ozden V, Dikmen G, Taser O. Arthroscopic labral repair versus debridement in patients with femoroacetabular impingement: a minimum 2.5 year follow-up study. Hip Int. 2016;26(1):20–24. [DOI] [PubMed] [Google Scholar]
- 5. Chandrasekaran S, Darwish N, Gui C, Lodhia P, Suarez-Ahedo C, Domb BG. Outcomes of hip arthroscopy in patients with Tönnis grade-2 osteoarthritis at a mean 2-year follow-up: evaluation using a matched-pair analysis with Tönnis grade-0 and grade-1 cohorts. J Bone Joint Surg Am. 2016;98(12):973–982. [DOI] [PubMed] [Google Scholar]
- 6. Colvin AC, Harrast J, Harner C, et al. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94(4):e23. [DOI] [PubMed] [Google Scholar]
- 7. Domb BG, Hartigan DE, Perets I. Decision making for labral treatment in the hip. J Am Acad Orthop Surg. 2017;25(3):e53–e62. [DOI] [PubMed] [Google Scholar]
- 8. Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88(5):925–935. [DOI] [PubMed] [Google Scholar]
- 9. Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy. 1999;15(2):132–137. [DOI] [PubMed] [Google Scholar]
- 10. Ferguson SJ, Bryant JT, Ganz R, Ito K. The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech. 2000;33(8):953–960. [DOI] [PubMed] [Google Scholar]
- 11. Gupta A, Suarez-Ahedo C, Redmond JM, et al. Best practices during hip arthroscopy: aggregate recommendations of high-volume surgeons. Arthroscopy. 2015;31(9):1722–1727. [DOI] [PubMed] [Google Scholar]
- 12. Kalore NV, Jiranek WA. Save the torn labrum in hips with borderline acetabular coverage. Clin Orthop Relat Res. 2012;470(12):3406–3413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kim K-C, Hwang D-S, Lee C-H, Kwon S-T. Influence of femoroacetabular impingement on results of hip arthroscopy in patients with early osteoarthritis. Clin Orthop Relat Res. 2007;456(456):128–132. [DOI] [PubMed] [Google Scholar]
- 14. Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46–53. [DOI] [PubMed] [Google Scholar]
- 15. Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25(4):369–376. [DOI] [PubMed] [Google Scholar]
- 16. Larson CM, Giveans MR, Stone R. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40(5):1015–1021. [DOI] [PubMed] [Google Scholar]
- 17. Larson CM, Giveans MR, Taylor M. Does arthroscopic FAI correction improve function with radiographic arthritis? Clin Orthop Relat Res. 2011;469(6):1667–1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lee YK, Ha YC, Yoon BH, Koo KH. National trends of hip arthroscopy in Korea. J Korean Med Sci. 2014;29(2):277–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maradit Kremers H, Schilz SR, Van Houten HK, et al. Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013. J Arthroplasty. 2017;32(3):750–755. [DOI] [PubMed] [Google Scholar]
- 20. Menge TJ, Briggs KK, Dornan GJ, Mcnamara SC, Philippon MJ. Survivorship and outcomes 10 years following hip arthroscopy for femoroacetabular impingement: labral debridement compared with labral repair. J Bone Joint Surg Am. 2017;99:997–1004. [DOI] [PubMed] [Google Scholar]
- 21. Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013;29(4):661–665. [DOI] [PubMed] [Google Scholar]
- 22. Newman AP, Daniels AU, Burks RT. Principles and decision making in meniscal surgery. Arthroscopy. 1993;9(1):33–51. [DOI] [PubMed] [Google Scholar]
- 23. Philippon MJ, Briggs KK, Yen Y-M, et al. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br. 2009;91:16–23. [DOI] [PubMed] [Google Scholar]
- 24. Philippon MJ, Peixoto LP, Goljan P. Acetabular labral tears: debridement, repair, reconstruction. Oper Tech Sports Med. 2012;20(4):281–286. [Google Scholar]
- 25. R Core Team. R: a language and environment for statistical computing. 2017. Available at: https://www.r-project.org/. Accessed June 15, 2017.
- 26. RStudio. RStudio: integrated development environment for R. 2017. Available at: http://www.rstudio.com/. Accessed June 15, 2017.
- 27. Safran MR. The acetabular labrum: anatomic and functional characteristics and rationale for surgical intervention. J Am Acad Orthop Surg. 2010;18:338–345. [DOI] [PubMed] [Google Scholar]
- 28. Santori N, Villar RN. Acetabular labral tears: result of arthroscopic partial limbectomy. Arthroscopy. 2000;16(1):11–15. [DOI] [PubMed] [Google Scholar]
- 29. Schilders E, Dimitrakopoulou A, Bismil Q, Marchant P, Cooke C. Arthroscopic treatment of labral tears in femoroacetabular impingement: a comparative study of refixation and resection with a minimum two-year follow-up. J Bone Joint Surg Br. 2011;93(8):1027–1032. [DOI] [PubMed] [Google Scholar]
- 30. Schmitz CC, Haas H, Müller-Stromberg J. Endoscopic treatment of calcinosis circumscripta of the hip joint: a report of 2 cases of arthroscopic removal of a calcific deposition between the labrum and capsule. Arthroscopy. 2010;26(8):1135–1138. [DOI] [PubMed] [Google Scholar]
- 31. Shibata KR, Matsuda S, Safran MR. Arthroscopic hip surgery in the elite athlete: comparison of female and male competitive athletes. Am J Sports Med. 2017;45(8):1730–1739. [DOI] [PubMed] [Google Scholar]
- 32. Sing DC, Feeley BT, Tay B, Vail TP, Zhang AL. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy. 2015;31(12):2307–2313. [DOI] [PubMed] [Google Scholar]