Abstract
Study Design:
Systematic review.
Objectives:
In patients undergoing posterior spinal fusion: (1) What are the types and risks of wound complications in major (≥3 levels) surgery, and does the risk vary by number of levels fused? (2) What types of fascial closure result in the fewest wound complications? (3) What subcutaneous closure technique is more effective in preventing wound complications for obese patients (body mass index >30 kg/m2)? (4) What type of skin closure results in the fewest wound complications? (5) What type of dressing results in the fewest wound complications?
Methods:
Electronic databases and reference lists of key articles were searched from January 1, 2000 to December 4, 2017 to identify studies meeting inclusion criteria.
Results:
Six lower quality retrospective studies (evidence level III) met the inclusion criteria. The risk of wound complications in patients with ≥3 level posterior spine fusion ranges from 1.5% to 3.7% depending on the definition of wound complications. Skin closure with sutures resulted in fewer wound infections compared with staples (0.0% vs 8.0%, P = .023). We were unable to demonstrate an association between the number of levels fused and infection risk. Wound infections, primarily superficial, occurred less frequently with Silverlon dressing versus routine dressing.
Conclusions:
We were unable to determine if infection risk changed with increasing number of levels fused. There is a lack of evidence for optimal wound closure technique in posterior spine surgery. Several questions still remain unanswered, such as the optimal fascial closure technique or the optimal subcutaneous closure technique in obese patients.
Keywords: spine surgery, wound complication, wound infection, wound closure, skin closure
Introduction
Wound complications represent a significant risk factor in spinal sugery, particularly in complex multilevel procedures. Surgical site infections (SSI) are the most common health care–associated infection, accounting for 31% of all hospitalized patients with a health care–associated infection.1 The reported incidence of SSIs following spine surgery ranges from 0.2% to 18.8%.2–4
The main goals of wound closure are to enable rapid skin healing, to minimize the risk of infection, and to facilitate early mobilization while allowing an acceptable cosmetic result. Most common skin closure methods in orthopedic surgery make use of sutures and staples.5 The mechanical equivalence of stapled and sutured wounds have been shown in animal studies. Furthermore, this study states that stapled wounds are less time consuming and narrower, which was associated with less inflammation than sutured wounds.6 However, clinical studies in various nonorthopedic specialties described staples as preferred choice because it is faster and has lower inflammation compared with sutures, but failed to show a difference in cosmetic appearance or patient satisfication.7,8
Though a number of studies evaluating skin closure methods have been reported in the orthopedic literature, there is no consensus on the optimal wound closure type or technique following traditional midline open posterior spine fusion surgery. The results and conclusions are conflicting implying a higher risk of infection with staples, whereas others state a higher infection risk with sutures.5,9,10 The aim of this sytematic review is to answer the following clinical key questions (KQs):
Clinical Questions
KQ 1: What are the types and risks of wound healing complications in major (≥3 level) posterior spine fusion? Does the risk of complications vary by number of levels fused?
KQ 2: What types of fascial closure results in the fewest wound healing complications after posterior spine surgery? Does the risk of wound healing complications vary by number of levels fused?
KQ 3: What subcutaneous closure technique is most effective in preventing wound healing complications for obese (BMI >30 kg/m2) patients receiving posterior spine fusion?
KQ 4: What type of skin closure (staples, interrupted, running, glue, nylon, subcutaneous) results in the fewest wound healing complications after posterior spine fusion? Does the risk of wound healing complications vary by number of levels fused?
KQ 5: What type of dressing (dry/composite dressings, hydrocolloid dressings, transparent dressings, antimicrobials dressings, foams, hydrogel) results in the fewest wound healing complications after posterior spine fusion? Does the risk of complications vary by number of levels fused?
Materials and Methods
Study Design: Systematic Review
Information Sources
PubMed and Cochrane Central Register of Controlled Trials (CENTRAL) databases from January 1, 2000 to December 4, 2017, and bibliographies of included articles.
Eligibility Criteria
The inclusion criteria were (1) adults ≥18 years and <75 years who underwent posterior spinal fusion (cervical, thoracic, or lumbar); (2) comparison of different wound closure types or techniques to close the fascia, subcutaneous tissue, or skin; (3) comparison of different types of postoperative wound dressing; (4) outcomes included wound healing complication frequency; (5) comparative studies for KQs 2 to 5, longitudinal studies for KQ 1; and (6) publications during or after the year 2000. The exclusion criteria were (1) anterior fusion, anterior-posterior fusion, decompression alone; (2) drains as an intervention; and (3) reviews or case reports.
Outcomes: Wound Healing Complications
Data Collection Items and Process
Data was extracted by a single individual and verified independently by a second investigator.
Analysis
Incidence of wound complications and the “rule of 3” standard deviation estimation for studies where zero events were reported for an outcome.11,12
Overall Strength of Evidence
The overall strength of evidence across studies was based on precepts outlined by the Grades of Recommendation Assessment, Development and Evaluation (GRADE) Working Group.13,14 Study critical appraisals and the reasons for upgrading and downgrading for each outcome can be found in the online supplementary material.
Results
Study Selection
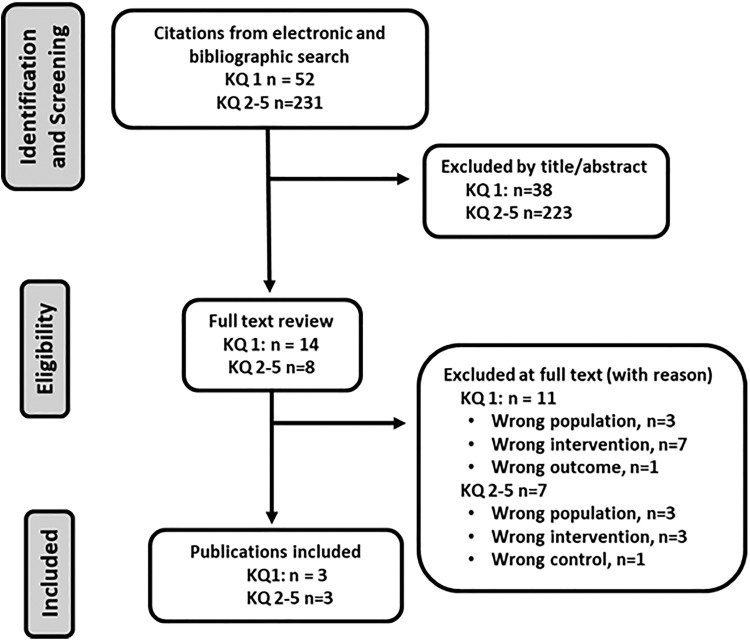
We identified 6 studies meeting inclusion criteria, all were poor-quality retrospective studies, class of evidence (CoE) level III. Figure 1 shows the inclusion/exclusion of articles from the search. CoE rating and a list of excluded articles can be found in the supplemental material at http://www.aospine.org/ebsj.
Figure 1.
Flow diagram showing results of literature search.
Risk of Wound Complications in ≥3 Levels of Posterior Spine Fusion
Three studies report cumulative incidence of wound complications following ≥3 level posterior spine fusion (Table 1).15–17 Mean ages ranged from 59 to 64 years with the proportion of males ranging from 39% to 68%. Follow-up times for 2 studies were 1 month and 2 years.15,17 One study reported only deep infections (0.9% for 3 levels, 2.3% for ≥4 levels, P = .055)16; 1 study reported superficial, deep and organ/space infection (2.1% for 3 levels, 0.0% for ≥4 levels)15; and 1 study included wound dehiscence, superficial, deep and organ/space infection (3.7% overall).17
Table 1.
Study Characteristics Reporting Types and Risks of Wound Healing Complications in ≥3 Levels of Posterior Spine Fusion.
| Author, Year, Country (CoE) | Study Design (Dates Collected) | Diagnosis and Procedure | Population Characteristics | Outcome Definition | Results | F/U Time, F/U Percent |
|---|---|---|---|---|---|---|
| Kuo, 2004, China (CoE: III) | Retrospective cohort (Jan 1997–Dec 2002) | Diagnosis: Spondylolisthesis, spinal stenosis, scoliosis, herniated disc, spinal fracture and adjacent syndrome Procedure: Posterior decompression with and without instrumentation, instrumentation revision, and removal of implant | N = 1278 Agea: 59 years Malea: 55.0% | SSI: deep wound infection defined as extensive infection below fascia layer | 3 levels: SSI deep: 0.9% (7/775) ≥4 levels: SSI deep: 2.3% (12/503) | Time NR % NR |
| Kim, 2015, Korea (CoE: III) | Retrospective cohort (Jan 2005–Sep 2012) | Diagnosis: NR Procedure: PLIF: 100% | N = 115 Ageb: 63.6 years Maleb: 68.2% | SSI: all wound infections to include superficial, deep, and organ/space | 3 levels: SSI total: 2.1% (2/96) ≥4 levels: SSI total: 0.0% (0/16) | 2 years 78.0% |
| Lee, 2017, USA (CoE: III) | Retrospective cohort (ACS NSQIP) (2010-2014) | Diagnosis: Adult spinal deformity Procedure: Long, multilevel (3-13+ levels) posterior fusion (CPT codes 22 842, 22 843, 22 844) | N = 1626 Agec: <51 years, 22% 51-60 years, 26% 61-70 years, 32% >70 years, 21% Malec: 39.3% | Wound complication to include superficial and deep SSI, wound dehiscence, or organ space infection | Long fusion: All wound complications: 3.7% (60/1626) | 30 days % NR |
Abbreviations: ACS NSQIP, American College of Surgeons National Surgical Quality Improvement Program database; CoE, class of evidence; DDD, degenerative disc disease; F/U, follow-up; NR, not reported; PLIF, posterior lumbar interbody fusion; SSI, surgical site infection.
aPatient characteristics given for entire population, which included 1251 two-level procedures.
bPatient characteristics given for entire population, which included 1831 one- and two-level procedures.
cPatient characteristics given for entire population, which included 4177 anterior or combined fusions and one- and two-level posterior procedures.
Wound Closure in the Obese
Our search did not reveal any studies comparing wound closure techniques for obese patients undergoing posterior spine fusion.
Comparison of Different Skin Closure
Two lower quality studies compared different suture materials18,19 and 1 study compared different wound dressings (Table 2).20 All were retrospective cohort studies with nonconcurrent controls. Mean ages ranged from 49 to 65 years with the proportion of males ranging from 48% to 64%. One study included surgeries with multilevel fusion,19 1 study included only 1 or 2 level fusions,20 and 1 study did not specify the number of levels fused.18
Table 2.
Study Characteristics Reporting Comparisons of Different Skin Closure or Dressing Types.
| Author, Year, Country, Study Type (Quality) | Intervention | Population | Surgery | Outcome Definition | Adverse Effects |
|---|---|---|---|---|---|
| Skin closure | |||||
| Ando, 2014, Japan, nonconcurrent retrospective cohort study (CoE: III) | A. 2-octyl-cyanoacrylate (n = 96) B. Staples (n = 87) Subcutaneous layers were closed with 2-0 absorbable sutures followed by skin closure with 2-octyl-cyanoacrylate or skin staples. Staples were removed 10-14 days postoperation | A vs B Age: 66.4 (13-94) vs 65.3 (15-91) years Male: 55% vs 51% Follow-up time: >1 year Follow-up %: 100 | A vs B Cervical: 31% vs 28% Thoracic: 14% vs 10% Lumbar: 55% vs 62% 1-2 levels fused: 53% vs 57% 3 levels fused: 16% vs 25% 4-6 levels fused: 58% vs. 46% ≥7 levels fused: 5% vs. 2% Anterior: 1% vs 1% Posterior: 99% vs 99% | Wound infection occurring within 30 days of the operation in noninstrumented and within 1 year in instrumented surgery. Superficial: infection of skin and subcutaneous tissue. Deep: infection of the deep soft-tissue muscle and fascia. | A vs B Wound infection 1-2 levels Any: 0.0% (0/51) vs 2.0% (1/50) Superficial: 0.0% (0/51) vs 0.0% (0/50) Deep: 0.0% (0/51) vs 2.0% (1/50) 3 levels Any: 0.0% (0/15) vs 20% (2/10) Superficial: 0.0% (0/15) vs 10% (1/10) Deep: 0.0% (0/15) vs 10% (1/10) 4-6 levels Any: 0.0% (0/19) vs 15% (3/20) Superficial: 0.0% (0/19) vs 5% (1/20) Deep: 0.0% (0/19) vs 10% (2/20) ≥7 levels Any: 0.0% (0/11) vs 14.3% (1/7) Superficial: 0.0% (0/11) vs 0.0% (0/7) Deep: 0.0% (0/11) vs 14.3% (1/7) All levels combined Any: 0.0% (0/96) vs 8.0% (7/87) Superficial: 0.0% (0/96) vs 2.3% (2/87) Deep: 0.0% (0/96) vs 5.7% (5/87) |
| Ueno, 2015, Japan, nonconcurrent retrospective cohort study (CoE: III) | A. Triclosan-coated polyglactin 910 suture (Vicryl plus) n = 30 (May 2011–Apr 2012) B. Polyglactin 910 suture (Vicryl) n = 36 (May 2010–Apr 2011) All patients received IV antibiotic prophylaxis for 3 days. Wound closure was achieved by interrupted suturing technique. Size 1 Vicryl or Size 1 Vicryl Plus was used for suturing the fascia and muscular layers, 3-0 Vicryl or Vicryl Plus for subcutaneous tissue, and surgical staples for the skin. Skin staples removed on postoperative day 10 | A vs B Agea: 56.8 vs 57.4 Malea: 63% vs 64% Follow-up time: NR Follow-up %: NR | A vs B Cervical: 3% vs 11% Lumbar: 63% vs 61% Thoracic: 3% vs 8% Spinal injury: 30% vs 19% Number of levels fused: NR | Wound infection defined as the presence of erythema, induration, pain, and culture-positive discharge of serous or contaminated fluid. | A vs B Wound infection Any: 0.0 (0/30) vs 2.8% (1/36) Superficial: 0.0% (0/30) vs 0.0% (0/36) Deep: 0.0% (0/30) vs 2.8% (1/36) |
| Dressing type | |||||
| Epstein, 2007, USA, Nonconcurrent retrospective cohort study (CoE: III) | A. Silverlon dressing (n = 106) B. Routine dressing (n = 128) Dressing duration for each: 2 weeks | A vs B Age: 49.6 (23-77) vs 49.1 (29-75) Male 48% vs 58% Follow-up time: 1 to 2.5 years vs 2.2 to 16 years Follow-up %: NR | A vs B Multilevel lumbar laminectomy with 1 or 2 level posterolateral instrumented fusion 1 level fusion: 73% vs 69% 2 level fusion: 27% vs 31% | Wound infections confirmed based on cultures and corroborated with enhanced MRI scans. | A vs B Wound infection Any: 0.0% (0/106) vs 10.9% (14/128) Superficial: 0.0% (0/106) vs 8.6% (11/128) Deep: 0.0% (0/106) vs 2.3% (3/128) |
Abbreviations: CoE, class of evidence; IV, intravenous; MRI, magnetic resonance imaging; NR, not reported.
a Patient characteristics given for entire population, which included 339 additional patients not receiving adult posterior fusion.
In 1 lower quality study,19 wound closure by sutures using 2-octyl-cyanoacrylate resulted in no wound infections compared with 7 (8.0%) in those receiving staples, P = .023. Five of 7 (71%) wound infections in the staples group were deep infections. Though the proportion of patients with deep infection increased as the number of levels fused increased, the test for a linear trend was not statistically significant. One small study compared triclosan-coated suture with noncoated suture.18 The investigators reported no infections (0/30) in the triclosan-coated suture group versus 2.8% (1/36) deep infections in the noncoated suture group.
One limited quality study20 reported more wound infections in postoperative patients treated with routine dressings versus “Silverlon” (Argentum Medical, LLC, Lakefront, GA), 10.9% versus 0% (P = .000). Most of these infections (79%) were superficial infections.
Illustrative Case
A 63-year-old male patient with an extensive wound complication after major posterior fusion surgery (Figure 2). Wound healing was impaired and most of the wound was dehiscent. The patient underwent hyperbaric oxygen therapy for 6 months at an outside facility before being transferred for further treatment. Revision surgery required pulsatile lavage, extensive debridement of the wound bed, and a muscle flap performed by plastic surgery (not shown).
Figure 2.

Wound complication after major posterior spine surgery.
Discussion
Wound complications after spine surgery remain a common source of morbidity with negative impact on patients recovery.21 Closure techniques in spine surgery are typically performed by surgeon preference, with little or no consensus described in the literature for specific closure types.
For traditional open posterior midline approaches, we were unable to demonstrate that the risk of wound complications varied by the number of level fused. Given that wound infection, particularly deep infection, is relatively uncommon, our findings may be the result of the low power in the 2 studies comparing risk of infection by level.
While it is considered important in proper surgical technique to reconstruct the fascia, we found no data supporting a specific fascial closure type following adult posterior midline spine surgery. In general, little data exists analyzing the fascial closure technique in other populations. Ward et al21 retrospectively compared a nonstandardized closure technique (n = 42) with a plastic surgery multilayered technique (n = 34) in patients with adolescent nonidiopathic scoliosis. The wound complication rate in the nonstandardized closure group was significantly higher. Note that the multilayered technique was performed by a plastic surgeon and the nonstandardized closure technique was not further described. In a randomized trial, Trimbos et al22 compared interrupted and continuous suture fascial closure in patients who underwent a midline laparotomy and found no difference in terms of wound infection or dehiscence. Prospective randomized controlled trials comparing various closure types would be optimal to determine the best closure method to minimize the risk of wound complications; however, given the relatively low number of such events, a high number of patients would need to be enrolled and such a study may not be feasible in practice.
While some studies describe the negative impact of obesity (BMI >30 kg/m2) on surgical treatment and outcomes, we were unable to identify any studies describing the effect of subcutaneous wound closure technique in the obese after posterior spine surgery. The extra adipose tissue involved in superficial closure has been thought to contribute to higher wound complications in the past.23 In their meta-analysis, Meng et al24 reported a higher risk of surgical site infection in obese patients (odds ratio [OR] = 2.13; 95% CI = 1.55-2.93). Likewise, Fei et al25 reported a 2 times greater risk for surgical site infection in spine surgery patients with a BMI >35 kg/m2. Furthermore, there is some evidence to suggest that the skin-to-lamina distance and the thickness of the subcutaneous fat are positively associated with surgical site infections.26 Therefore, it is our contention that minimizing of the subcutaneous dead space may be helpful to reduce wound complications and surgical site infections. Future studies are needed comparing different types of subcutaneous wound closure (interrupted vs running suture material) and fascial closure techniques in obese patients following posterior spine fusion.
The discussion about sutures versus staples remains controversial. In their systematic review, Krishnan et al27 showed that there was no significant difference in superficial infection or secondary outcomes comparing sutures to staples in patients who underwent hip or knee surgery. In a meta-analysis of nonorthpedic conditions, Iavazzo et al10 reported a lower rate of wound infections and decreased wound closure time for staples. However, Ando et al19 showed a significantly higher wound infection rate for stapled wounds following posterior spine fusion compared with subcuticular closure followed by 2-octyl-cyanoacrylate glue. Nevertheless, all these studies provide poor evidence with very high heterogeneity. Different surgical approaches may benefit from different wound closure mechanism and therefore there is a need to explore current evidences on ideal wound closure mechanism.
While the analysis of antibiotic-coated suture (triclosan-coated vs noncoated suture) did not show a significant difference in wound infection rates, the comparison of different dressing types did show a significantly lower infection rate in patients treated with “Silverlon” (Argentum Medical, LLC, Lakefront, GA) dressings compared with routine dressing (0.0% vs 10.9%, P = .000). These results are supported by the fact that silver as an antimicrobial topical substance has been previously shown to reduce wound complications in other fields.28,29
Evidence Summary (Table 3)
Table 3.
Evidence Summary Table.
| Outcome | Follow-up | Studies, N | Study Limitations | Serious Inconsistency | Serious Indirectness | Serious Imprecision | Quality | Conclusions |
|---|---|---|---|---|---|---|---|---|
| Key Question 1. What are the types and risks of wound healing complications in major (≥4 level) posterior spine fusion? Does the risk of complications vary by number of levels fused? | ||||||||
| Deep infection only | NR | 1 observational study, N = 1278 | Yes | Unknown | No | Yes | Very low | 3 levels: 0.9% (7/775) ≥4 levels: 2.3% (12/503) P = .055 |
| Superficial, deep or organ/space infection | 2 years | 1 observational study, N = 115 | Yes | Unknown | No | Yes | Very low | 3 levels: 2.1% (2/96) ≥4 levels: 0.0% (0/16) P = 1.00 |
| Wound dehiscence, superficial, deep or organ/space infection | 30 days | 1 observational study, N = 1626 | Yes | Unknown | No | Yes | Very low | Long fusion: 3.7% (60/1626) |
| Key Question 2: What types of fascia closure results in the fewest wound healing complications after posterior spine surgery? Does the risk of wound healing complications vary by number of levels fused? | ||||||||
| No evidence | ||||||||
| Key Question 3: What subcutaneous closure technique is more effective in preventing wound healing complications for very obese (BMI >30 kg/m2) patients receiving posterior spine fusion? | ||||||||
| No evidence | ||||||||
| Key Question 4: What type of skin closure results in the fewest wound healing complications after posterior spine fusion? Does the risk of wound healing complications vary by number of levels fused? | ||||||||
| 2-Octyl-cyanoacrylate vs staples | ||||||||
| Wound infection | >1 year | 1 retrospective non-concurrent ?thyc=5?> cohort study N = 183 | Yes | Unknown | No | Yes | Very low | Any level fusion Any infection: 0.0% (0/96) vs 8.0% (7/87), P = .005 Deep infection: 0.0% (0/96) vs 5.7% (5/87), P = .023 ≥4 level fusion Any infection: 0.0% (0/30) vs 14.8% (4/27), P = .044 Deep infection: 0.0% (0/30) vs 5.7% (3/27), P = .100 |
| Triclosan-coated polyglactin 910 suture (Vicryl plus) vs Polyglactin 910 suture (Vicryl) | ||||||||
| Wound infection | NR | 1 retrospective nonconcurrent cohort study, N = 66 | Yes | Unknown | No | Yes | Very low | Any infection: 0.0 (0/30) vs 2.8% (1/36), P = 1.00 Deep infection: 0.0% (0/30) vs 2.8% (1/36), P = 1.00 |
| Key Question 5: What dressing technique/type results in the fewest wound healing complications after posterior spine fusion? Does the risk of complications vary by number of levels fused? | ||||||||
| Wound infection | 1 retrospective nonconcurrent cohort study, N = 183 | Yes | Unknown | No | Yes | Very low | Any infection: 0.0% (0/106) vs 10.9% (14/128), P = .000 Deep infection: 0.0% (0/106) vs 2.3% (3/128), P = .253 | |
Abbreviations: BMI, body mass index; NR, not reported.
The risk of wound complications in patients with ≥3 levels of posterior spine fusion accomplished through a traditional posterior midline surgery was 1.5% in 1 study when complications were defined as deep infections; 1.8% in 1 study when wound complications were defined as superficial, deep or organ/space infection; and 3.7% in 1 study when wound complications were defined as wound dehiscence, superficial, deep or organ/space infection (strength of evidence very low). Deep wound infection occurred more frequently in patients with fusion ≥4 levels (2.3%) versus 3 levels (0.9%), but failed to reach statistical significance, P = .055 (strength of evidence very low).
There was no evidence assessing types of fascial or subcutaneous closure techniques in obese patients undergoing posterior spine fusion.
Wound closure using 2-octyl-cyanoacrylate resulted in no wound infections compared with 7 (8.0%) in those receiving staples, in one small, poor-quality study, P = .023 (strength of evidence very low).
Wound closure using triclosan-coated sutures reported no infections (0/30) versus 2.8% (1/36) deep infections in the noncoated sutures in 1 poor-quality small study (strength of evidence very low).
One poor-quality study reported fewer wound infections in postoperative posterior spine fusion patients treated with “Silverlon” (Argentum Medical, LLC, Lakefront, GA) dressings versus routine dressings, 0.0% (0/106) versus 10.9% (14/128), P = .000. Most of these infections (79%) were superficial infections (strength of evidence very low).
Conclusions
The risk of wound complications in patients with ≥3 level posterior spine fusion ranges from 1.5% to 3.7%. We were unable to determine if infection risk changed with increasing number of levels fused done through conventional posterior midline surgery. There is a lack of evidence for an optimal wound closure technique in posterior spine surgery. Several questions remain unanswered, such as the optimal fascial closure technique or the optimal subcutaneous closure technique in obese patients.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Magill SS, Hellinger W, Cohen J, et al. Prevalence of healthcare-associated infections in acute care hospitals in Jacksonville, Florida. Infect Control Hosp Epidemiol. 2012;33:283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chahoud J, Kanafani Z, Kanj SS. Surgical site infections following spine surgery: eliminating the controversies in the diagnosis. Front Med (Lausanne). 2014;1:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Silber JS, Anderson DG, Vaccaro AR, Anderson PA, McCormick P; NASS. Management of postprocedural discitis. Spine J. 2002;2:279–287. [DOI] [PubMed] [Google Scholar]
- 4. Rechtine GR, Bono PL, Cahill D, Bolesta MJ, Chrin AM. Postoperative wound infection after instrumentation of thoracic and lumbar fractures. J Orthop Trauma. 2001;15:566–569. [DOI] [PubMed] [Google Scholar]
- 5. Smith TO, Sexton D, Mann C, Donell S. Sutures versus staples for skin closure in orthopaedic surgery: meta-analysis. BMJ. 2010;340:c1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Roth JH, Windle BH. Staple versus suture closure of skin incisions in a pig model. Can J Surg. 1988;31:19–20. [PubMed] [Google Scholar]
- 7. Rousseau JA, Girard K, Turcot-Lemay L, Thomas N. A randomized study comparing skin closure in cesarean sections: staples vs subcuticular sutures. Am J Obstet Gynecol. 2009;200:265e1–e4. [DOI] [PubMed] [Google Scholar]
- 8. Khan AN, Dayan PS, Miller S, Rosen M, Rubin DH. Cosmetic outcome of scalp wound closure with staples in the pediatric emergency department: a prospective, randomized trial. Pediatr Emerg Care. 2002;18:171–173. [DOI] [PubMed] [Google Scholar]
- 9. Shantz JA, Vernon J, Leiter J, Morshed S, Stranges G. Sutures versus staples for wound closure in orthopaedic surgery: a randomized controlled trial. BMC Musculoskelet Disord. 2012;13:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Iavazzo C, Gkegkes ID, Vouloumanou EK, Mamais I, Peppas G, Falagas ME. Sutures versus staples for the management of surgical wounds: a meta-analysis of randomized controlled trials. Am Surg. 2011;77:1206–1221. [PubMed] [Google Scholar]
- 11. Eypasch E, Lefering R, Kum CK, Troidl H. Probability of adverse events that have not yet occurred: a statistical reminder. BMJ. 1995;311:619–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hanley JA, Lippman-Hand A. If nothing goes wrong, is everything all right? Interpreting zero numerators. JAMA. 1983;249:1743–1745. [PubMed] [Google Scholar]
- 13. Atkins D, Best D, Briss PA, et al. ; GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–406. [DOI] [PubMed] [Google Scholar]
- 15. Kim JH, Ahn DK, Kim JW, Kim GW. Particular features of surgical site infection in posterior lumbar interbody fusion. Clin Orthop Surg. 2015;7:337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kuo CH, Wang ST, Yu WK, Chang MC, Liu CL, Chen TH. Postoperative spinal deep wound infection: a six-year review of 3230 selective procedures. J Chin Med Assoc. 2004;67:398–402. [PubMed] [Google Scholar]
- 17. Lee NJ, Shin JI, Kothari P, et al. Incidence, impact, and risk factors for 30-day wound complications following elective adult spinal deformity surgery. Global Spine J. 2017;7:417–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ueno M, Saito W, Yamagata M, et al. Triclosan-coated sutures reduce wound infections after spinal surgery: a retrospective, nonrandomized, clinical study. Spine J. 2015;15:933–938. [DOI] [PubMed] [Google Scholar]
- 19. Ando M, Tamaki T, Yoshida M, et al. Surgical site infection in spinal surgery: a comparative study between 2-octyl-cyanoacrylate and staples for wound closure. Eur Spine J. 2014;23:854–862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Epstein NE. Do silver-impregnated dressings limit infections after lumbar laminectomy with instrumented fusion? Surg Neurol. 2007;68:483–485. [DOI] [PubMed] [Google Scholar]
- 21. Ward JP, Feldman DS, Paul J, et al. Wound closure in nonidiopathic scoliosis: does closure matter? J Pediatr Orthop. 2017;37:166–170. [DOI] [PubMed] [Google Scholar]
- 22. Trimbos JB, Smit IB, Holm JP, Hermans J. A randomized clinical trial comparing two methods of fascia closure following midline laparotomy. Arch Surg. 1992;127:1232–1234. [DOI] [PubMed] [Google Scholar]
- 23. Gurusamy KS, Toon CD, Davidson BR. Subcutaneous closure versus no subcutaneous closure after non-caesarean surgical procedures. Cochrane Database Syst Rev. 2014;(1):CD010425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Meng F, Cao J, Meng X. Risk factors for surgical site infections following spinal surgery. J Clin Neurosci. 2015;22:1862–1866. [DOI] [PubMed] [Google Scholar]
- 25. Fei Q, Li J, Lin J, et al. Risk factors for surgical site infection after spinal surgery: a meta-analysis. World Neurosurg. 2016;95:507–515. [DOI] [PubMed] [Google Scholar]
- 26. Mehta AI, Babu R, Karikari IO, et al. 2012 Young Investigator Award winner: The distribution of body mass as a significant risk factor for lumbar spinal fusion postoperative infections. Spine (Phila Pa 1976). 2012;37:1652–1656. [DOI] [PubMed] [Google Scholar]
- 27. Krishnan R, MacNeil SD, Malvankar-Mehta MS. Comparing sutures versus staples for skin closure after orthopaedic surgery: systematic review and meta-analysis. BMJ Open. 2016;6:e009257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Krieger BR, Davis DM, Sanchez JE, et al. The use of silver nylon in preventing surgical site infections following colon and rectal surgery. Dis Colon Rectum. 2011;54:1014–1019. [DOI] [PubMed] [Google Scholar]
- 29. Bowler PG, Welsby S, Hogarth A, Towers V. Topical antimicrobial protection of postoperative surgical sites at risk of infection with Propionibacterium acnes: an in-vitro study. J Hosp Infect. 2013;83:232–237. [DOI] [PubMed] [Google Scholar]