Abstract
Study Design:
Retrospective analysis. Level of evidence III.
Objectives:
Low-energy vertebral compression fractures are an increasing socioeconomic problem among elderly patients. Percutaneous vertebroplasty has been extensively used for the treatment of painful fractures because of its effectiveness. However, some complications have been described; among them, new vertebral compression fractures, whether adjacent or not to the treated vertebra, are commonly reported complications (8% to 52%).
Methods:
We retrospectively analyzed epidemiological and technical variables presumably associated with new vertebral compression fractures. To determine the relationship between new vertebral compression fracture and percutaneous vertebroplasty, 30 patients (study group) with this complication were compared with 60 patients treated with percutaneous vertebroplasty without this condition (control group).
Results:
A higher cement percentage was found in the study group (40.3%) compared with the control group (30.5%). Initial vertebral kyphosis was significantly higher in the first group (15°) compared with the control group (9°). Epidemiological factors were similar in both groups.
Conclusions:
In our study, increased cement percentage injected and a higher kyphosis were associated with new vertebral compression fractures.
Keywords: vertebroplasty, new vertebral fracture, osteoporosis, vertebral body fracture
Introduction
Low-energy vertebral compression fractures (VCFs) represent a significant cause of morbidity among elderly patients. Percutaneous vertebroplasty (PV) is an effective and well-recognized treatment for VCF.1,2 This procedure is considered the first line of treatment for osteoporotic fractures when conservative treatment has failed.2–5
Although PV is a relatively safe procedure, complications such as cement leakage, cord compression, nerve root damage, infection, and new VCF have been described.6–8
The frequency of new VCF varied, ranging from 8% to 52%,8–11 and most of these reported fractures occurred at adjacent levels.2,10
In the literature, it is well recognized that aspects related to patients, such as low bone mineral density and low body mass index (BMI), as well as other technical factors such as vertebral height restoration, are associated with new VCF.11–16 Other variables such as presence of intradiscal cement leakage, relative amount of cement (measured as cement percentage), or postprocedure initial vertebral kyphosis are not clearly established.
The objective of our study was to evaluate epidemiological and technical variables in patients who suffered a new VCF requiring a new PV in comparison with a control group.
Material and Methods
The study protocol was approved by the ethics review board of Hospital Italiano de Buenos Aires (Approval Number IRB00010193) and in concordance with the Declaration of Helsinki.
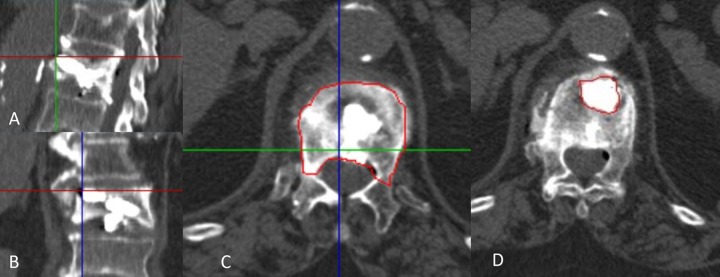
We designed a case-control study nested in a cohort of consecutive adult patients who underwent PV for low-energy fractures between April 2008 and November 2014 at the Hospital Italiano de Buenos Aires, a tertiary university hospital. Inclusion criterion was the following: PV after low-energy VCF at 1 level (Figure 1), with a minimum 1-year follow-up. Exclusion criteria were the following: more than 1-level vertebroplasty, metastasis, previous spine surgery, hemangiomas, and less than 12-month follow-up (Figure 2).
Figure 1.
A 72-year-old female patient without traumatic event presents with severe back pain. (A) Pre-vertebroplasty sagittal view T2-weighted magnetic resonance (MR) image shows bone marrow edema of T9 (arrow). (B) Cone-beam computed tomography coronal reconstruction image after vertebroplasty shows correct cement filling of T9. (C) Spine lateral radiograph view after T9 vertebroplasty shows disc leakage (arrowhead). (D) Sagittal view T2-weighted MR image 3 months later, when the patient returned with new pain, shows new bone marrow edema of T10 (asterisk). (E) Spine lateral radiograph view shows the needle in T10. (F) Spine lateral radiograph view after second vertebroplasty with correct filling of T10 (arrow).
Figure 2.
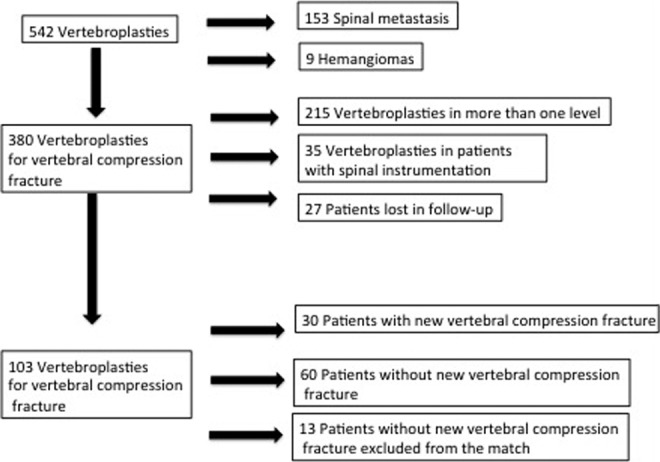
Flow of patients treated with vertebroplasty in our institution.
The study group included 30 consecutive patients having new VCF that required another vertebroplasty during the first year after the procedure, and the new VCF was classified as adjacent (superior or inferior to the treated level) and nonadjacent (at least 1 level spared between the original vertebroplasty and the new VCF). As a control group, we selected 60 patients (2:1 ratio) matched for age (± 5 years) and level (thoracic, lumbar).
Baseline characteristics (sex, age), comorbidities, BMI, osteoporosis (defined as less than 2.5 densitometry), level of vertebroplasty, initial vertebral kyphosis, as well as technical measurements such as percentage of cement filling in the fractured vertebra and cement leakage to the superior or inferior disk space were also collected in a standardized form by retrospective review of the clinical chart. Before the procedure, all patients were studied with standing X-rays and magnetic resonance imaging (MRI; Achieva, Phillips, Netherlands). Vertebroplasty was performed in an angiography suite with cone-beam computed tomography (Artis Zeego, Siemens, Germany).
The measurement of vertebral kyphosis was performed by Surgimap 2.2.8 on lateral X-rays with the patient in standing position; superior and inferior end plates of the fractured vertebra were measured. Measurement of percentage of cement and volume in the fractured vertebras as well as cement leakage to the superior or inferior disk spaces were assessed with Vitrea Advance workstation (Vital Images, Toshiba Medical, MN). Volume calculation was performed by taking the vertebral perimeter on an axial plane from the superior endplate (Figure 3A) up to the inferior endplate to calculate the exact percentage and volume of the intravertebral cement (Figure 3B–D); the software generates a surface using the height of the vertebra and cement in order to assess a volume.
Figure 3.
(A) Sagittal vertebral view at the cemented level. (B) Coronal vertebral view. (C) Vertebral body volume measurement. (D) Vertebral cement measurement.
A total of 542 patients underwent PV between 2008 and 2014. Among them, 153 patients (28%) with spinal metastasis and 9 patients (1.6%) with aggressive hemangiomas were excluded; 380 patients (70%) with osteoporotic vertebral fractures were further evaluated; 215 patients were excluded because of compromise at more than 1 level, 35 patients were excluded for having spinal instrumentation, and 27 patients were lost to follow-up (Figure 2). Finally, the study population consisted of 103 patients, 30 experienced a new VCF and 73 without a new VCF; in order to make the match ratio 2:1, 13 patients were randomly removed from the control group. Thus, 452 patients (83%) were excluded.
Bisphosphonates and calcium-rich diet were the main medical intervention, 1 patient from group 1 and 2 patients from group 2 developed osteoporosis secondary to chronic corticoids therapy.
Vertebroplasty Technique
Percutaneous vertebroplasty was performed in an angiographic suite. All procedures were done under general anesthesia. One 11-gauge bone needle was advanced through a transpedicular or costovertebral approach. The needle tip was placed in the anterior third of the vertebral body under anteroposterior and lateral fluoroscopy. Methylmethacrylate was mixed in five 1-mL syringes. Under biplane fluoroscopic guidance, the cement was injected by using the syringes. We injected bone cement (polymethylmethacrylate) and stopped when the cement reached the posterior third of the vertebral body or when any leakage occurred.
Statistical Analysis
Numerical variables were described as means with standard deviation or median and interquartile range according to distribution, and categorical variables were described as absolute frequencies and percentage. Univariate analysis was performed using conditional logistic regression to assess association with new fracture after vertebroplasty. Confounders were adjusted using the multivariate conditional regression logistic model. Candidates’ variables for the multivariate model were osteoporosis, initial vertebral kyphosis, percentage of cement, and cement volume injected. The search for the best model was based on clinical and statistical significance. A P value less than .05 was considered statistically significant. The analysis was performed using STATA version 13 (College Station, TX).
Results
Thirty patients experienced a new VCF within the first year after PV. The incidence of new VCF after PV was 8.5% (95% confidence interval = 6.4% to 10.9%).
Among the 90 patients (cases and controls), females represented 81% (73), and the mean age was 76 years (74.8 in group 1 and 76.3 in group 2).
Table 1 shows the description of the patients who experienced a new vertebral fracture after PV (case group).
Table 1.
New Vertebral Compression Fracture Group.
| Patient No. | Age/Sex | Vertebral Level Treated | Time | New Vertebral Level Treated |
|---|---|---|---|---|
| 1 | 80/female | L1 | 8 months 12 days | T12 |
| 2 | 88/female | T9 | 25 days | T10 |
| 3 | 80/female | L2 | 45 months 28 days | T11 |
| 4 | 88/female | L3 | 29 months 24 days | T12 |
| 5 | 60/female | T12 | 30 d | L4, L5 |
| 6 | 85/female | T12 | 2 months 11 days | T11 |
| 7 | 84/female | L2 | 25 months 3 days | L1 |
| 8 | 85/male | L5 | 26 months 13 days | L2 |
| 9 | 76/male | T8 | 30 months 24 days | T12 |
| 10 | 81/female | L3 | 12 months 7 days | L4 |
| 11 | 73/female | T11 | 11 months 16 days | T7, T8, T9 |
| 12 | 78/female | L3 | 9 months 10 days | T11, L1 |
| 13 | 68/female | L1 | 12 months 7 days | T11 |
| 14 | 75/female | T12 | 1 month 11 days | L1 |
| 15 | 73/female | T12 | 10 months 15 days | L1 |
| 16 | 87/female | T12 | 9 months 27 days | T10 |
| 17 | 79/female | T10 | 5 months 6 days | T8 |
| 18 | 85/male | L1 | 3 months 13 days | T12 |
| 19 | 60/female | T9 | 1 month 28 days | T8 |
| 20 | 77/male | L1 | 55 months 15 days | T11 |
| 21 | 65/male | L1 | 17 days | T7 |
| 22 | 52/female | T5 | 34 days | T6 |
| 23 | 78/female | L2 | 11 months 8 days | L4 |
| 24 | 46/male | T12 | 11 months 2 days | T2 |
| 25 | 83/female | L1 | 53 months 17 days | T10, T11 |
| 26 | 73/female | T8 | 5 months 23 days | T7 |
| 27 | 77/female | L1 | 2 months 12 days | T8 |
| 28 | 58/female | L1 | 1 month 24 days | T11 |
| 29 | 81/male | L3 | 3 months 18 days | T7, T8 |
| 30 | 70/male | T12 | 65 months | L2 |
Baseline Characteristics
Table 2 describes baseline characteristics in both groups (cases and controls).
Table 2.
Baseline and Technical Characteristics of Patients in Both Groups.
| All Patients | Group 1 | Group 2 | P | |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Number | 90 | 30 | 60 | |
| Age | 75.8 ± 9.8 | 74 ± 10 | 76 ± 9.2 | .14 |
| Percentage of women | 83.3 | 73 | 85 | >.05 |
| Osteoporosis (%) | 62.1 | 65 | 59.2 | >.05 |
| BMI | 27.6 ± 3.8 | 27.06 | 27.69 | >.05 |
| Technical characteristics | ||||
| Mean volume cement percentage | 34.2 ± 11 | 40.28 | 30.55 | .01 |
| Mean vertebral kyphosis (°) | 11.15 | 14.9 | 9.18 | .011 |
| Mean cement leakage into the disk (%) | 24.4 | 30 | 21.6 | .46 |
Abbreviation: BMI, body mass index.
Factors Associated With New Symptomatic VCF After PV
Table 3 shows factors studied in relation to new symptomatic VCF after PV.
Table 3.
Factors Associated With Symptomatic New VCP.
| OR Crude | 95% CI | P | OR Adjusted | 95% CI | P | |
|---|---|---|---|---|---|---|
| Age (years) | 0.82 | 0.4-0.9 | .03 | 1.06 | 0.8-1.5 | .73 |
| Female | 1.6 | 0.5-4.9 | .44 | — | — | — |
| BMI | 0.9 | 0.8-1.1 | .32 | — | — | — |
| Osteoporosis | 2.2 | 0.6-8 | .21 | 2.3 | 0.3-18.5 | .42 |
| Volume cement percentage | 1.12 | 1.0-1.2 | .007 | 1.27 | 1-1.52 | .008 |
| Vertebral kyphosis | 1.18 | 1.1-1.3 | .001 | 1.16 | 1.04-1.3 | .011 |
Abbreviations: VCF, vertebral compression fracture; OR, odds ratio; CI, confidence interval; BMI, body mass index.
Among the factors, age, female sex, osteoporosis, and BMI were found to have no statistical difference between groups (P > .05). However, we noticed a tendency for new VCF in women with osteoporosis, elderly patient, and high BMI.
Regarding osteoporosis, we found no differences in terms of medical treatment modalities in both groups.
In relation with technical factors, there was no significant difference when comparing disk cement leakage between groups (P = .46).
Vertebral cement percentage and initial vertebral kyphosis were factors in which we found statistically significant difference. The mean percentage of cement filling was 40.3% in the case group versus 30.6% in the control group (P = .01), and the initial vertebral kyphosis was 14.9° versus 9.2° (P = .01).
Adjacent and Nonadjacent New VCF in the Study Group
In the study group, from a total of 30 new fractures, 11 were adjacent at the level from the PV (37%). When comparing baseline and technical features in this subgroup with the nonadjacent group, there was no significant difference. However, the percentage of women was higher in adjacent VCF and the time of new vertebral fracture was sooner. In addition, vertebral cement percentage was higher in adjacent VCF, although no significant differences were observed between these 2 subgroups (Table 4).
Table 4.
Comparison Between Adjacent and Nonadjacent New Vertebral Compression Fracture.
| Adjacent VCF (N = 11) | Nonadjacent VCF (N = 19) | |
|---|---|---|
| Baseline characteristics | ||
| Mean age, years (IR) | 81 (76-85) | 75 (65-79) |
| Percentage of women,% (n) | 90 (10) | 63 (12) |
| Mean BMI, kg/m2 (IR) | 27 (25-31) | 26 (25-29) |
| Mean days to new fracture (IR) | 103 (71-299) | 351 (108-936) |
| Technical characteristics | ||
| Mean percentage vertebral cement (IR) | 42 (33-60) | 38 (31-42) |
| Mean degrees of vertebral kyphosis (IR) | 15 (11-20) | 16 (12-19) |
Abbreviations: VCF, vertebral compression fracture; IR, interquartile range; BMI, body mass index.
Discussion
Percutaneous vertebroplasty is a safe and effective therapeutic option for the treatment of painful VCF when medical treatment is not effective; however, some complications have been described such as new vertebral fracture at another level.5–7 This study evaluates factors associated with new symptomatic VCF after PV, including BMI, osteoporosis, age, and sex distribution, as well as procedure-related factors such as vertebral cement percentage, disk cement leakage, and vertebral kyphosis. In this series from our institution, the incidence of new VCF was 8.5% after 1-year follow-up, lower than those reported by Anselmetti et al2 in a multicenter study (EVEREST group) with 13% of new vertebral fracture. Voormolen et al12 and Lin et al13 reported a higher incidence of new VCF of 24% and 30%, respectively. Although the evidence of new VCF varies from 8% to 52%,8–11 our results could be explained by the study design. Our incidence might be lower due to the inclusion of only symptomatic fractures with new vertebroplasty requirement and no active screening.
Our findings show that factors associated with new VCF at bivariate analysis were age, vertebral cement percentage, and degrees of initial vertebral kyphosis. Previous studies have analyzed factors related to increased risk of new vertebral fracture. Ma et al,14 in a systematic review, observed 3 strong factors associated with VCF after PV (lower bone mineral density, vertebral height restoration, and intradiscal cement leakage) and 6 moderate-evidence factors such as lower BMI, number of preexisting vertebral fractures, thoracolumbar junction, cement distribution, older age, and number of treated vertebrae.
Osteoporosis and low BMI are known major factors associated with increased risk of vertebral fractures.14–16 In our study, however, osteoporosis, BMI, and sex distribution showed no differences between the new vertebral fracture group and the control group. Regarding osteoporosis, we observed a higher prevalence in the study group compared with the control group, without significant differences, and we also evaluated the medical treatment and found no differences in terms of therapeutic algorithm in both groups.
Concerning procedure-related factors, the amount of cement injected was considered presumably associated with adjacent fracture9,17,18; however, there are no specific algorithms with regard to the most appropriate cement fraction required to restore stiffness without increasing the risk of cement leakage and new VCF. Nieuwenhuijse et al19 analyzed the vertebral cement body fraction required to reduce pain after vertebral osteoporotic fractures and found an optimal fraction of 24% of the vertebral body. Liebschner et al,20 in an experimental study, found that restoration of stiffness was reached with 15% of vertebral cement volume and use of a 30% fill increased stiffness by more than 50% compared with the predamaged value.
The difference between cemented vertebra and adjacent osteoporotic level creates pulling forces that increase the risk of new vertebral fracture17,18 associated with patients’ increased activity secondary to pain relief that may create a mechanical stress.9
Luo et al21 in a biomechanical study found that 3.5 mL were required to restore normal stress distribution after VCF. However, other authors9 suggested that a fractured vertebra should be filled as much as possible. In our study, vertebral cement percentage was significantly higher in the new VCF group compared with the control group. These results can be explained by increased stiffness of the cemented vertebra.
Initial vertebral kyphosis after fracture could increase the risk of new fracture because of spinal imbalance, especially at the thoracolumbar junction.17,18 In addition, kyphosis restoration was also found to be a risk factor for new fracture.22 In our study, significantly higher vertebral kyphosis in the new fracture group compared with the control group was found; however, kyphosis restoration was not evaluated in our study. Fifty-one percent of fractures occurred at the thoracolumbar junction; however, thoracolumbar junction was not associated with risk of new VCF in the present study.
Cement migration to the disk space with consequent stiffness increment has been associated with new VCF.8 Results of multivariate analysis suggest that the risk of new VCF is 4.6 times higher in patients with cement leakage than in patients free of leakage.11 In our study, cement leakage into the disk space was higher in the study group compared with the control group (30% and 21%, respectively); however, no significant differences were found. Similar results were observed by Lin et al, who reported 21% of cement leakage in the new VCF group compared with 22% in the non–new VCF group.13 The lack of statistical significance in factors associated with new symptomatic VCF after PV could be explained by the small number of patients. Additionally, difference from previous studies could be due to patients’ detection method (limited case detection), including types of events (symptomatic VCF).
Regarding adjacent and nonadjacent VCF, it is accepted that adjacent osteoporotic VCF is more common than nonadjacent VCF after PV and usually within the first month.9,10,23 Takahara et al22 found increasing age and low BMI as risk factors of adjacent VCF in osteoporotic postmenopausal women. In our study, the number of adjacent VCF12 and nonadjacent VCF20 were similar; adjacent VCF occurred sooner than nonadjacent VCF, but without significant differences. Anselmetti et al,2 in a multicenter study, observed that 80% of new VCF occurred adjacent to the vertebroplasty. Analyzing epidemiological risk factors, we observed a tendency of adjacent VCF to occur in older females with low BMI, but without significant differences. Our study has strengths. First, one spinal fellow who does not perform the procedures made analysis; electronic medical records allow specific clinical and interventional data. This means that the data collection process is reliable as it collects information in a systematic and rigorous manner, with a standardized process. Second, Hospital Italiano receives patients who are representative of the Buenos Aires population. In addition, we would like to highlight limitations including retrospective data re-collection. Additionally, the population with only symptomatic VCF were included, which could underestimate the real number of new VCFs. There are strong factors associated with new VCF; however, no thoroughly evidence-based recommendation exists with regard to procedure-related factors, such as the exact amount of cement required to relieve pain and not to increase the rate of new VCF. More evidence is required to establish a proper technical algorithm in vertebroplasty.
Conclusion
In summary, in our study, 8.5% of the patients analyzed had new vertebral fractures that required new PV, and the most important factors associated with new VCF after vertebroplasty were vertebral cement percentage and initial vertebral kyphosis, and both factors were statistically significant in the new vertebral fracture group. These aspects should be considered in order to decrease the rate of new VCF.
Footnotes
Authors’ Note: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Tseng YY, Yang ST, Tu PH, Yang TC, Lo YL. Minimally invasive vertebroplasty in the treatment of pain induced by spinal metastatic tumor. Minim Invasive Neurosurg. 2008;51:280–284. [DOI] [PubMed] [Google Scholar]
- 2. Anselmetti GC, Marcia S, Saba L, et al. Percutaneous vertebroplasty: multi-centric results from EVEREST experience in large cohort of patients. Eur J Radiol. 2012;81:4083–4086. [DOI] [PubMed] [Google Scholar]
- 3. DePalma MJ, Ketchum JM, Frankel BM, Frey ME. Percutaneous vertebroplasty for osteoporotic vertebral compression fractures in the nonagenarians: a prospective study evaluating pain reduction and new symptomatic fracture rate. Spine (Phila Pa 1976). 2011;36:277–282. [DOI] [PubMed] [Google Scholar]
- 4. Klazen CA, Lohle PN, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010;376:1085–1092. [DOI] [PubMed] [Google Scholar]
- 5. Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol. 1997;18:1897–1904. [PMC free article] [PubMed] [Google Scholar]
- 6. Laredo JD, Hamze B. Complications of percutaneous vertebroplasty and their prevention. Skeletal Radiol. 2004;33:493–505. [DOI] [PubMed] [Google Scholar]
- 7. Yeom JS, Kim WJ, Choy WS, Lee CK, Chang BS, Kang JW. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Joint Surg Br. 2003;85:83–89. [DOI] [PubMed] [Google Scholar]
- 8. Lin EP, Ekholm S, Hiwatashi A, Westesson PL. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004;25:175–180. [PMC free article] [PubMed] [Google Scholar]
- 9. Uppin AA, Hirsch JA, Centenera LV, Pfiefer BA, Pazianos AG, Choi IS. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology. 2003;226:119–124. [DOI] [PubMed] [Google Scholar]
- 10. Trout AT, Kallmes DF, Kaufmann TJ. New fractures after vertebroplasty: adjacent fractures occur significantly sooner. AJNR Am J Neuroradiol. 2006;27:217–223. [PMC free article] [PubMed] [Google Scholar]
- 11. Komemushi A, Tanigawa N, Kariya S, et al. Percutaneous vertebroplasty for osteoporotic compression fracture: multivariate study of predictors of new vertebral body fracture. Cardiovasc Intervent Radiol. 2006;29:580–585. [DOI] [PubMed] [Google Scholar]
- 12. Voormolen MH, Lohle PN, Juttmann JR, van der Graaf Y, Fransen H, Lampmann LE. The risk of new osteoporotic vertebral compression fractures in the year after percutaneous vertebroplasty. J Vasc Interv Radiol. 2006;17:71–76. [DOI] [PubMed] [Google Scholar]
- 13. Lin WC, Cheng TT, Lee YC, et al. New vertebral osteoporotic compression fractures after percutaneous vertebroplasty: retrospective analysis of risk factors. J Vasc Interv Radiol. 2008;19(2 pt 1):225–231. [DOI] [PubMed] [Google Scholar]
- 14. Ma X, Xing D, Ma J, et al. Risk factors for new vertebral compression fractures after percutaneous vertebroplasty: qualitative evidence synthesized from a systematic review. Spine (Phila Pa 1976). 2013;38:E713–E722. [DOI] [PubMed] [Google Scholar]
- 15. Lee DG, Park CK, Park CJ, Lee DC, Hwang JH. Analysis of risk factors causing new symptomatic vertebral compression fractures after percutaneous vertebroplasty for painful osteoporotic vertebral compression fractures: a 4-year follow-up. J Spinal Disord Tech. 2015;28:E578–E583. [DOI] [PubMed] [Google Scholar]
- 16. Zhang Z, Fan J, Ding Q, Wu M, Yin G. Risk factors for new osteoporotic vertebral compression fractures after vertebroplasty: a systematic review and meta-analysis. J Spinal Disord Tech. 2013;26:E150–E157. [DOI] [PubMed] [Google Scholar]
- 17. Baroud G, Heini P, Nemes J, Bohner M, Ferguson S, Steffen T. Biomechanical explanation of adjacent fractures following vertebroplasty. Radiology. 2003;229:606–607. [DOI] [PubMed] [Google Scholar]
- 18. Baroud G, Nemes J, Heini P, Steffen T. Load shift of the intervertebral disc after a vertebroplasty: a finite-element study. Eur Spine J. 2003;12:421–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nieuwenhuijse MJ, Bollen L, van Erkel AR, Dijkstra PD. Optimal intravertebral cement volume in percutaneous vertebroplasty for painful osteoporotic vertebral compression fractures. Spine (Phila Pa 1976). 2012;37:1747–1755. [DOI] [PubMed] [Google Scholar]
- 20. Liebschner MA, Rosenberg WS, Keaveny TM. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine (Phila Pa 1976). 2001;26:1547–1554. [DOI] [PubMed] [Google Scholar]
- 21. Luo J, Daines L, Charalambous A, Adams MA, Annesley-Williams DJ, Dolan P. Vertebroplasty: only small cement volumes are required to normalize stress distributions on the vertebral bodies. Spine (Phila Pa 1976). 2009;34:2865–2873. [DOI] [PubMed] [Google Scholar]
- 22. Takahara K, Kamimura M, Moriya H, et al. Risk factors of adjacent vertebral collapse after percutaneous vertebroplasty for osteoporotic vertebral fracture in postmenopausal women. BMC Musculoskelet Disord. 2016;17:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Aquarius R, van der Zijden AM, Homminga J, Verdonschot N, Tanck E. Does bone cement in percutaneous vertebroplasty act as a stress riser? Spine (Phila Pa 1976). 2013;38:2092–2097. [DOI] [PubMed] [Google Scholar]