Abstract
In general, there is agreement that robust integrated information systems are the foundation for building successful regional health care delivery systems. Integrated Advanced Information Management System (IAIMS) institutions that, over the years, have developed strategies for creating cohesive institutional information systems and services are finding that IAIMS strategies work well in the even more complex regional environment. The key elements of IAIMS planning are described and lessons learned are discussed in the context of regional health information systems developed. The challenges of aligning the various information agencies and agendas in support of a regional health information system are complex ; however, the potential rewards for health care in quality, efficacy, and cost savings are enormous.
Changes in the health care environment are occurring at an ever-accelerating rate. Academic medical centers as well as other health care delivery organizations are finding that change is one of the few constants. Current and emerging themes include : increased emphasis on ambulatory care, capitated payments versus fee-for-service, supporting primary care training, building multidisciplinary care teams, and a shift in focus from treating illness to improving health. A second constant is the development of health care systems—groups of hospitals, clinics, private practices, long-term care facilities, public health clinics, and other health care agencies, often existing over a large geographic area and sometimes including multistate entities that support the health care of large populations of patients. These multi-type entities often have very complex contractual relationships and include owned as well as unowned but affiliated entities.
In general, there is agreement that robust integrated information systems are the foundation for building successful regional health care delivery systems, even though direct cost benefits of integration of health care information systems are still difficult to measure. According to the Healthcare Financial Management Association, most progressive health care organizations intend to invest greater proportions of their operating budgets in information systems and consolidation over the next three to five years. Indirect cost benefits predicted include :
Enhanced clinical productivity
More accurate billing
Increased throughput
Reduction in order-entry redundancies
Staffing reductions 1
Integrated Advanced Information Management System (IAIMS) institutions, over the years, have developed strategies for creating coherent information-systems-planning processes and have implemented comprehensive coordinated information systems. The organizations are finding that the same strategies that worked for institutional development are even more valuable in the creation of regional health information systems. In times of rapid change, these institutions are reaffirming that strategic planning is vital. The components of an IAIMS planning process include : environmental analysis and planning, assessing capabilities of key institutional information agencies and providers, and organizing individuals and institutional units for change.
Characteristics of the Distributed Environment—Primary Care Sites
Distance from the academic medical center results in special challenges as well as incentives to develop integrated information and communication systems. Avoiding the movement of patients to specialized centers except when absolutely necessary is clearly desirable from many points of view—financial as well as patient convenience. In some areas of the United States, the weather as well as geographic isolation thwarts the movement of patients to specialty care sites. Avoidance of transfer of patients saves travel costs, reduces impatient charges, and can provide a better support environment for the patient and the patient's family. Provider feelings of isolation can be reduced through electronic access to colleagues, electronic information resources, and continuing education opportunities.
Unfortunately, the distributed sites often have under-developed or nonexistent technical infrastructures. Hospitals (especially small ones), clinics, and physicians' offices frequently lack internal local-area networks or computers capable of accessing the local-area network, the health care wide-area network, or the Internet. Inadequate numbers of aging computers are typical. Practice-management software varies widely from site to site, with a lack of data or vocabulary standards for sharing patient records or other types of data. The level of computer use among health care providers outside the academic health sciences center is low, 2 and there is little access to technicians to provide training and support the use of the equipment.
Communication systems in many rural areas are often unreliable. There is a general lack of digital services in many rural areas, especially in the West, and the cost of voice communications is often high. The Tele-communications Act of 1996 may bring some relief to rural areas through its twin goals of development of competition in all communication markets and the preservation and advancement of universal service. Universal service is based on the concept that all consumers, regardless of income and location, should have access to basic telephone services at affordable rates, even if the market is unable to deliver this public good at reasonable rates.
Characteristics of the Distributed Environment—Then and Now
Charles Babbage admonished that “the man who aspires to fortune or to fame by new discoveries must be content to examine with care the knowledge of his contemporaries, or to exhaust his efforts in inventing again, what he will most probably find has been better executed before.” 3
A look at the history of IAIMS development is a useful lens for viewing current efforts. The early IAIMS institutional environment has been well documented. 4,5,6,7,8,9 The environment in academic institutions in the mid-1980s, which prompted the IAIMS initiative, included numerous islands of proprietary information systems and stand-alone information services throughout the academic schools and medical centers, each operating autonomously with a variety of types of software, hardware, and user interfaces and little or no data sharing.
An analogous situation exists now with our regional partners. The problems and challenges we face are very similar to those that faced the early IAIMS institutions, with some new issues and challenges thrown in. The new challenges include political and social challenges : how to build information linkages between institutions and facilities that are not under a common “ownership” or, in fact, at some levels, may be competitors.
Another characteristic of the early IAIMS environment was the lack of a mature organizational structure for collaborative development of systems. Integration in academic institutions and hospitals was a “foreign” concept. Multiple information systems providers existed in isolation from each other. The Internet, in its infancy, was a tool of the few, primarily researchers, and the World Wide Web did not exist. Proprietary, vertical information systems were the rule, with a predominant focus on administrative and financial management uses. Libraries were print-based. Online bibliographic databases existed, but remote access from home, clinic, or hospital was unusual. Data dictionaries were nonexistent or rudimentary. The Unified Medical Language System (UMLS) was still a theoretical construct.
Now, integration is the marketing theme for every health information system vendor as well as every health care organization. Data standards have matured, and linkages between vendor systems are demanded by informed purchasers of health information systems. Furthermore, producers of software, databases, and information systems and network providers are delivering generic products that can more quickly be implemented in the health care information systems environment. And the fruits of the UMLS developments of the past ten years are being realized as institutional data dictionaries are being built and utilized.
Today, unlike the situation in the 1980s, we have the tools and the information resources to more rapidly create an integrated regional health information infrastructure. However, the organizational side of the enterprise, that is, people and workflow processes, still has a long way to go. 10,11 Clinical staff are scrambling to meet the demands for cost reduction and increased productivity while trying to adjust to each new wave of technology. Librarians and developers of information systems are likewise hard-pressed to deliver needed tools and information resources rapidly as the organization creates new affiliation agreements monthly or even weekly. The support staff of information systems cannot keep up with the demand for training and user support. Telemedicine applications, especially real-time consultations, are not only costly in terms of telecommunications expenses, they consume large amounts of time of specialists and providers alike. And security issues continue to be of paramount concern as we move information and develop systems beyond the institutional boundaries.
What have we learned from the previous ten years of IAIMS planning and implementation processes at institutions across the United States and beyond ? In a word, the technology is the easy part—now more than ever. It is the way planning processes deal with people, both the users and the systems developers, that will result in success or failure of regional integrated health information systems.
What can we learn from institutional IAIMS processes as we build regional integrated information systems ? At the heart of all successful IAIMS institutions is a robust planning process, with the leadership of the institution committed to implementing the plan. While each IAIMS site has taken a slightly different path from the others and each has had a somewhat different view of what constituted “integration,” all had to develop comprehensive strategic plans and create enterprise-wide organizational structures to integrate activities across organizational and geographic boundaries. 12
Defining Integration—A Vital Component of IAIMS Planning
Integration as a concept has come to mean many things to many people and, in the absence of a precise institutional understanding, planning and implementation processes can easily lose their focus. From the earliest IAIMS planning at the University of Washington (UW), integration has been defined from the perspective of the user :
Single device
Single interface
Appearance of single database
Search strategy consistency
Small, portable device
User-definable options
Memory of user preferences
Easy, logical data entry and display
To do useful tasks
Likewise, a succinct statement of goal is useful as one begins to build a sense of community understanding among disparate components of the institution. This statement of unified purpose becomes paramount as one begins to build information-systems linkages to geographically distant sites. The UW IAIMS goal was seamless access to information resources, databases, and tools in support of the many roles that health sciences personnel (educators, students, researchers, administrators, and care-givers) play in response to the university mission of education, clinical care, and research in a geographically distributed environment.
The UW Institutional Environment
From early in the UW IAIMS planning process (1988), we recognized that, given our mission as a regional health care university, our information systems would need to meet the needs of UW faculty, staff, and administrators in the four-state WAMI (Washington, Alaska, Montana, Idaho) region we serve educationally and clinically. 13,14 In fact, recently the WAMI region has been expanded to include Wyoming as a partner in our regional medical programs. The WAMI region encompasses over 789,000 square miles, over 27% of the total area of the United States, and extends over three time zones. In addition to geographic size, these states also contain the nation's highest mountain chains. The climatic conditions vary greatly, with extremes of temperature and moisture. With the exception of Washington, the WAMI states are sparsely populated, with 50% or more of the populations living in small towns, in villages, and on ranches.
In the early IAIMS years, the UW identified the development of institutional information systems as a key priority. Support for our regional first-year medical school sites and clinical clerkship and residency sites was focused on library and academic resources and not on clinical systems and decision-support tools. Recently, however, we have begun the development of a regional telemedicine testbed to support the broad information needs of our affiliated clinical sites around the Seattle area as well as throughout the WAMI states.
Technical Infrastructure
Early in the institutional IAIMS development process, getting the technical infrastructure “right” was vital, and it is equally important in the regional environment. The UW was fortunate in the late 1980s to have forged technically sophisticated, coherent and collaborative alliances among the key information agencies. We adopted common networking standards across the university and the medical centers and collaborated in the development of academic information resources, clinical decision-support tools, and common user interface(s). 15,16,17,18
Figure 1 shows the key campus information agencies that have collaborated over the years to create the campus infrastructure, information systems, resources, and databases that support our institutional IAIMS, as well as the additional organizational entities that are joining with the original group to ensure that a coherent framework emerges to support our regional clinical and educational system. The new participants in our various planning groups include hospitals marketing, our regional clinical and educational partners, and our telemedicine project staff. A variety of telemedicine projects have been undertaken at the UW over the years to support clinical care and education over distances. Including departmental telemedicine activities in the planning of our over-all regional information systems is vital.
Figure 1.
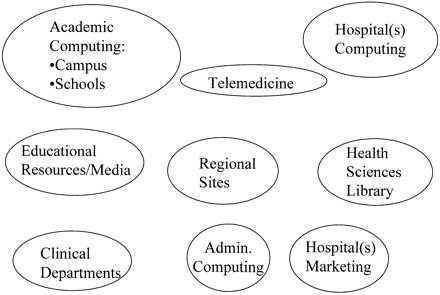
Key players in regional IAIMS development.
Telemedicine—From Demonstration Projects to Integrated System
Telemedicine can be described as the use of electronic information and communication technologies to provide and support health care when distance separates the participants. Telemedicine efforts on campus often begin within a single department (e.g., radiology) for a single purpose, and are likely to be grant-funded. Multiple uncoordinated telemedicine efforts may be undertaken within a single institution. Such efforts frequently lack linkages to other campus information resources, focus on “proof of concept,” and end when the funds end. The IAIMS planning process provides an opportunity to link these disparate telemedicine efforts and bring them into the overall fabric of enterprise information systems with a goal of creating an enduring telemedicine service to support the broad institutional needs for multimedia communications with the institution's geographically distributed sites.
The lack of a coordinated institutional approach to telemedicine activities can potentially result in present and future problems working with off-campus primary care sites and potential clinical and educational partners. From systems with multiple interfaces and passwords to an absence of a coherent message regarding institutional relationships to a lack of access to key academic medical center information resources, the end result is frustration on the part of off-campus health care providers.
Components of a Regional Health Information System
As is true of institutional information systems, the components of a successful comprehensive regional health information system include, in addition to a robust technical infrastructure that will support multimedia as well as high-speed data transmission, highquality, secure, patient-focused information sharing, provision of efficient means of communication among providers and with their patients, academic information resources, decision-support tools, and training and support services. The challenges of aligning the various components in support of a regional health information system are complex, but the potential rewards in efficacy, quality, and cost savings are enormous. Beyond the actual benefits realized from linking disparate information systems, resources, services, and databases is the value to the regional partners in clinical care and training, which benefit from having more coherent linkages with the academic medical center.
Organizational Models and IAIMS Roles : Getting to Integrated
Over the years, institutions have used a variety of organizational models, ranging from anarchy (extreme individual autonomy) to feudalism (management by individual units) to monarchy (single leader—all information agencies report to single individual) to federalism (consensus, negotiation, symbiosis, commensualism). 19 IAIMS institutions have tended to adopt combinations of these models, in particular, variations on federalism. The IAIMS role can be described as that of the manager of the federation, the catalyst for development and maintainer of a “level playing field” where various information groups, departments, administrators, and faculty can plan for the future in a relatively neutral environment. IAIMS programs leverage resources and link faculty informatics research efforts with real institutional information systems problems. A key question is whether a federalistic approach to regional integrated systems development will work or whether, over time, most institutions will move toward a more formal organizational information structure with a single leader in charge of regional information systems, services, and databases.
Conclusion
The IAIMS as an organizational change tool has been extraordinarily powerful in bringing about integrated information systems within a number of institutions. As we build regional health care systems, it is imperative that comprehensive, technically robust, integrated information systems be a core goal. Providing new ways of looking at old problems has been a key feature of IAIMS initiatives to date. The IAIMS, as a process with its focus on comprehensive institutional planning, has proven its worth over the years and is likely to be ever more useful as we build complex regional health information systems for the future.
Acknowledgments
The author thanks Dr. Jim LoGerfo, Ms. Debra Ketchell, Dr. Jim Barrett and Dr. Peter Tarczy-Hornoch for their leadership in furthering the IAIMS vision and Ms. Jennifer Kerr for valuable editorial assistance.
Presented at the IAIMS Consortium Symposium, Vanderbilt University, Nashville, TN, September 27, 1996. Supported in part by contracts and grants from the National Library of Medicine, 5G08-LM05620, N01-LM-63545 and N01-LM-3520.
References
- 1.Healthcare Financial Management Association. Cost benefits of integrated systems. Health Management Technology. 1995. ; 10.
- 2.Council on Competitiveness. Highway to Health : Transforming U.S. Health Care in the Information Age. Washington, DC, 1996.
- 3.Babbage C. On the Economy of Machinery and Manufacturers. London, Charles Knight, 1832.
- 4.Matheson NW, Cooper JAD. Academic information in the health sciences center : roles for the library in information management. J Med Educ. 1982. ; 57(Part 2) : 1-93. [DOI] [PubMed] [Google Scholar]
- 5.Association of American Medical Colleges. The Management of Information in Academic Medicine : An Assessment of the Application of Technology, Policy Consequences, and Needed Changes in the Present System. 2 vols. Washington, DC : AAMC, 1982.
- 6.Barnett GO, Greenes RA, Zielstorff RD. IAIMS development at Harvard Medical School. Bull Med Libr Assoc. 1988. ; 76 : 226-30. [PMC free article] [PubMed] [Google Scholar]
- 7.Ball MH, Douglas JV. Part II. Planning and implementing integrated information services. Integration and outreach : Integrated Academic Information Management Systems (IAIMS) at Maryland. J Am Soc Info Sci. 1988. ; 39 : 107-12. [DOI] [PubMed] [Google Scholar]
- 8.West RT. The National Library of Medicine's IAIMS grant program : experiences and futures. J Am Soc Info Sci. 1988. ; 39 : 142-5. [DOI] [PubMed] [Google Scholar]
- 9.Lindberg DAB, West RT, Corn M. IAIMS : an overview from the National Library of Medicine. Bull Med Libr Assoc. 1992. ; 80 : 244-6. [PMC free article] [PubMed] [Google Scholar]
- 10.Lorenzi, NM. Organizational Aspects of Health Informatics. Managing Technological Change. New York : Springer-Verlag, 1995.
- 11.Fuller S, Braude RM, Florance V, Frisse ME. Managing information in the academic medical center : building an integrated information environment. Acad Med. 1995. ; 70 : 887-91. [DOI] [PubMed] [Google Scholar]
- 12.Stead WW, Borden R, Bourne J, et al. The Vanderbilt University fast track to IAIMS : transition from planning to implementation. J Am Med Informat Assoc. 1996. ; 3 : 308-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adkins RJ, Anderson GR, Cullen TJ, Myers WW, Newman FS, Schwarz MR. Geographic and specialty distributions of WAMI Program participants and nonparticipants. J Med Educ. 1987. ; 62 : 810-7. [DOI] [PubMed] [Google Scholar]
- 14.Osborn EHS, O'Neil EH. Biomodal medical schools : excelling in research and primary care. Acad Med. 1996. ; 71 : 941-9. [DOI] [PubMed] [Google Scholar]
- 15.Fuller S. Creating the integrated information infrastructure for the 21st century at the University of Washington Magnuson Health Sciences Center. Proceedings of the Annual Symposium on Computer Applications in Medical Care. 1993. ; 529-33. [PMC free article] [PubMed]
- 16.Tarczy-Hornoch P, Fuller S. Design and implementation of integrated encrypted email for clinicians. Proc AMIA Annu Fall Symp. JAMIA. 1996. ; 3, September-October suppl : 850.
- 17.Ketchell DS, Ibrahim KN, Murri NA, Wareham PS, Bell DM, Jankowski TA. Architecture for a federated drug reference in a managed care environment. Proc AMIA Ann Fall Symp. JAMIA. 1996. ; 3, September-October suppl : 413-7. [PMC free article] [PubMed]
- 18.Ketchell DS, Freedman MM, Jordan WE, Lightfood EM, Heyano S, Libbey PA. Willow : a uniform search interface. JAMIA. 1996. ; 3 : 27-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davenport TH, Eccles RG, Prusak L. Information politics. Sloan Management Review. 1992. ; 34 : 53-65. [Google Scholar]


