Abstract
BACKGROUND AND OBJECTIVE:
Stroke is the second leading cause of death worldwide and the number of stroke cases has increased remarkably over the last 20 years. This study aimed at identifying predictors of with 6-month mortality of first-ever stroke patients and the factors contributing to it in East Azerbaijan province.
MATERIALS AND METHODS:
A closed cohort study was carried out from April 2014 to December 2014. All cases of first-ever diagnosed stroke were included in the study. Any transient ischemic attack, silent brain infarctions, and the stroke cases which were neither associated with trauma, blood disease nor with malignancy were excluded from the study. The variables of this study include participants' demographic characteristics, stroke severity National Institutes of Health Stroke Scale (NIHSS), and stroke risk factors. Patients were followed up within 6 months. To determine the survival time, the log-rank method was applied to compare intergroup differences. The tests include the univariate and multivariate analysis Cox regression. P < 0.05 were considered as statistically significant.
RESULTS:
A total of 576 cases of stroke were included in this study. Average age of ischemic and hemorrhagic stroke was 70.15 ± 13.0 and 67.79 ± 12.69, respectively. Case-fatality rate (CFR) of stroke patients was 49.2 and 21.7% in hemorrhagic and ischemic stroke types, respectively. Factors contributing to stroke mortality events include the severity of stroke (NIHSS categories 15–19 and ≥20), age over 65, being female, high body mass index and hyperlipidemia. In the final model, the severity of stroke (with NIHSS 15–19 with hazard ratio (HR) 4.22 (95% confidence interval [CI] 2.36–7.56) and NIHSS ≥20 with HR 5.34 (95% CI: 2.81–10.12) and age above 65 with HR 1.61 (95% CI: 1.02–2.51) were the most important predictors of 6-month mortality.
CONCLUSION:
Severity of stroke by NIHSS was the most prominent factor in stroke patients' mortality. By increasing the follow-up time, a better evaluation of the predictors of mortality after stroke can be achieved.
Keywords: Case-fatality rate, intracranial hemorrhages, Iran, ischemic stroke, mortality
Introduction
First-ever stroke is defined as a stroke occurring for the first time during a patient's lifetime. Stroke as the second leading cause of death worldwide is the main cause of functional disability in most areas.[1] The number of stroke cases in the world doubled to 33 million between 1990 and 2010.[2] Burden of the stroke is increasing due to population growth as well as the increasing average age in communities.[3] The prevalence of stroke in Iran is high compared to Western countries, especially in young age group.[4]
Mortality of stroke varies across different regions of the world.[5] It has decreased in high-income countries (due to lifestyle changes in the past decade), but this is not evident in low- and-middle-income countries.[6] According to the World Bank classification, Iran is an upper middle-income country.[7]
In previous studies, the average survival rate of stroke is estimated to be 5–10 years which is dependent on factors such as severity of stroke and the hosts' characteristics.[8] One-month stroke mortality rate varies from 13.2% to 27.4% in Europe.[9] After follow-up, the annual survival rate was estimated to be close to 10%. However, the corresponding value for annual mortality was between 8% and 32% among centers in Poland.[5]
Considering that there is no national registration of stroke in Iran, there is a significant difference between reported rates in different regions of Iran from 22 to 140 strokes/100,000 population.[10] Mortality after a stroke is reported differently in different studies. For instance, in a study in Shiraz province of Iran, it was reported to be 20.5%, with higher mortality among elderly people and lower socioeconomic classes.[11]
Several modifiable and nonmodifiable risk factors have been identified in relation to stroke mortality: Old age, type of stroke and its severity, history of previous stroke or Transient Ischemic Attack (TIA), diabetes, smoking, obesity, physical inactivity, diet high in cholesterol and salt, alcohol use, arterial fibrillation, consumption of contraceptive pills, and a history of heart disease.[12]
In addition, gender is one of the important determinants of stroke. In general, stroke is more common among men. However, because of high life expectancy of women and high incidence of stroke at older ages, the number of cases of stroke is higher among women rather than men.[13]
In the INTERSTROKE study which included 22 countries, it has been shown that there are ten risk factors which are responsible for more than 90% of the stroke risk encountered by the population.[14]
So far, there is no considerable reliable information about the severity of the mid-term (6 months) stroke mortality and its determinants in East Azerbaijan province, Iran. Therefore, the present study was conducted with the aim of calculating case-fatality rate (CFR) of 6 months after the stroke as well as identifying the factors affecting the mortality rate-based type of stroke in East Azerbaijan province-Iran.
Materials and Methods
This study was conducted using a closed prospective cohort design. It was carried out as a one-group survival analysis in two large hospitals in the city of Tabriz, Iran (Razi and Imam Reza hospitals) from April 2014 to December 2014 for 9 months. East Azerbaijan Province is the fifth largest province in the northwest of Iran, with a population of 3,909,652 in the census carried out in 2016 (Iranian Statistics Center). This province has a young population and about 50% of the population of the province is under 25 years of age.[15]
Inclusion and exclusion criteria (selection and description of participants)
All cases of first-ever diagnosed ischemic stroke (IS) or intracerebral hemorrhage by neurologists, residing in East Azerbaijan province for at least 1 month, being over 16, and being treated in the special stroke ward were included in the study. However, any TIA, silent brain infarctions and the stroke cases which were neither associated with trauma, blood disease nor with malignancy were excluded from the present study.[16]
The variables in this study include demographic characteristics such as age, sex, level of education, occupation, body mass index (BMI), and marital status; some risk factors of stroke including fasting blood sugar, cholesterol, triglyceride, high-density lipoprotein, low-density lipoprotein, systolic and diastolic blood pressure at the time of admission, passive smoking, hookah and alcohol, diabetes, and heart disease.
Definition of stroke and diagnostic criteria
“Two stroke definitions were considered: (1) A new focal neurological deficit with symptoms and signs lasting for >24 h coherent with the stroke definition of the World Health Organization (WHO); patients who died within the first 24 hours with a focal neurological deficit and (2) all neurological focal deficits lasting at least 1 h or resolving within 1 h, but with an abnormal brain imaging associated with a clinically relevant picture.”[17]
A definitive diagnosis of stroke was performed by a neurologist based on computed tomography (CT) scan and magnetic resonance imaging (MRI) scan.
In this study, hypertension meant patients with previous medical history, use of antihypertensive drugs, or average blood pressure >140/90 mmHg.[18]
By diabetes mellitus (DM), we meant patients with fasting blood glucose >126 mg/dl, patient with the previous history of DM or patients receiving a drug for DM treatment.[19]
Hypercholesterolemia was defined as serum total cholesterol level >200 mg/dl or use of lipid-lowering treatment.
Follow-up
A telephone-based follow-up was carried out with close relatives about the patient's conditions after 180 days from the first stroke.
Medical history associated with cardiovascular diseases, family history of stroke, and TIA were obtained from medical records of the patients or through face-to-face interviews.
Demographic information was completed using a questionnaire. Patient's relatives were asked about their patient's conditions if the patients themselves were not able to respond.
Records of stroke patients hospitalized at Razi and Imam Reza hospitals of Tabriz (admitted in neurology or other departments) were monitored by neurologists for signs and symptoms and risk factors of stroke. Stroke types were classified through using MRI and CT scan. Then, the National Institutes of Health Stroke Scale (NIHSS) was completed by a specialist to determine stroke severity.
Statistical analysis
Descriptive statistics (mean and standard deviation [SD]) were used with normally distributed quantitative variables, while median and interquartile ranges were used with nonnormally distribution. For qualitative variables, however, frequency and relative frequency were used.
To test the possible relationship between risk factors and event (mortality/survival), Chi-square test was used. In case of limitations in expected frequency or sample size, Fisher's exact test was used.
To determine the survival time, the Kaplan–Meier method was used and if the assumption of proportionality was met during the period of study, the log-rank method was applied to compare intergroup differences.
Other tests performed in this study include the univariate and multivariate Cox proportional hazards (CPH) regression models which are a method for investigating the effect of several variables on the time of a specified event (time-to-event) happens. Variables were entered with the BACKWARD method, that is, only significant variables retained in the final model.
The two assumptions of CPH regression models, that is, the censoring assumption (the censoring of the patients is random and is not related to the event), and the constant hazard risk (constant hazard risk over time in the compared groups) were considered and met. Data were analyzed by Stata software version 14. P < 0.05 were considered statistically significant.
The study protocol was reviewed and approved by the Ethics Committee of Tabriz University of Medical Sciences, No. IR.TBZMED.REC.1393.217.
The procedure of study was in accordance with the ethical standards of the Tabriz University of Medical Sciences Ethics committee on human experimentation. All patients voluntarily contributed after being notified of the objectives, methods, benefits, and disadvantages of the study. Informed consent was given by all patients before the interview. If the patient was not alert (lack of consciousness), his/her family agreed with fingerprints to participate in the study. The patients ensured the confidentiality of information by desisting from mentioning participants' names, initials, or hospital numbers, especially in illustrative material.
Results
A total of 576 eligible first-ever stroke patients were included in the study (53.5% were male). Male-to-female ratio was 1:15. Table 1 shows the distribution of some demographic characteristics of the cases.
Table 1.
Distribution of some demographic characteristics based on stroke type for first cases, East Azerbaijan-Iran
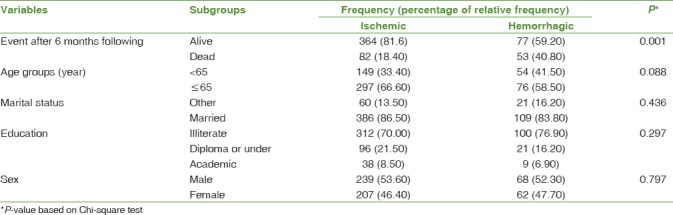
The mean age of ischemic stroke patients was 70.15 which ranged from 25 to 94 years. The mean age for hemorrhagic stroke patients was 67.99 years ranging from 33 to 90 years. There was no significant difference in the mean age of the two groups (P = 0.826).
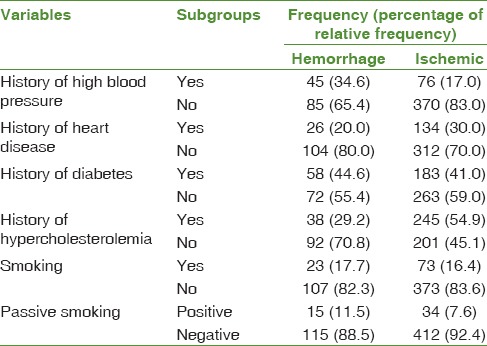
Distribution of major risk factors of stroke, based on type of stroke, is shown in [Table 2].
Table 2.
Distribution of major risk factors of first-ever stroke by type of stroke, East Azerbaijan-Iran
Distribution of stroke type in men and women was not significantly different (P = 0.797).
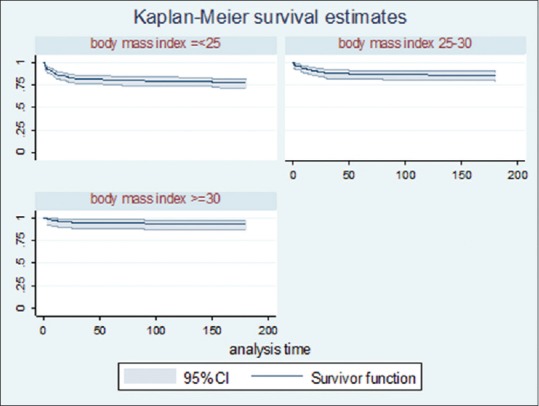
The relationship between risk factors and the 180-day follow-up event are presented in Table 3. The 180 days survival after stroke was lower in hemorrhagic type than ischemic which was statistically significant (P < 0.001) was [Figure 1].
Table 3.
Distribution of major risk factors based on 6 months survival for first-ever stroke cases, East Azerbaijan-Iran
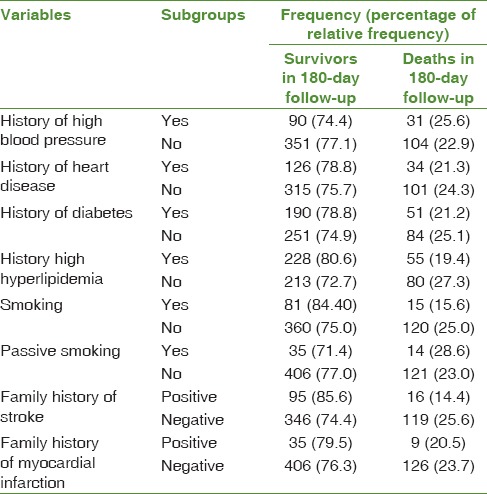
Figure 1.
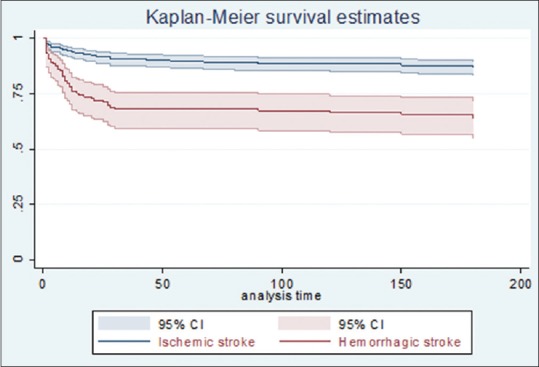
Comparison of estimated probability of mortality among types of stroke based on Kaplan–Meier method for first-ever stroke patients, East Azerbaijan Province, Iran
The mean of 6-month survival time of ischemic stroke was 155.15 days with an SD of 56.66 days, and these values for hemorrhagic stroke were 115.93 days with SDs of 160.29 of days.
The 6-month mortality increased with stroke severity. The lowest and highest survival rate belonged to NIHSS ≥20 and NIHSS below 5, respectively (P < 0.001).
Case-fatality rate of hemorrhagic and ischemic strokes were 49.2% and 21.7%, respectively. There was a statistically significant difference between the stroke types, with patients of hemorrhagic type having a higher mortality risk than ischemic (P < 0.001).
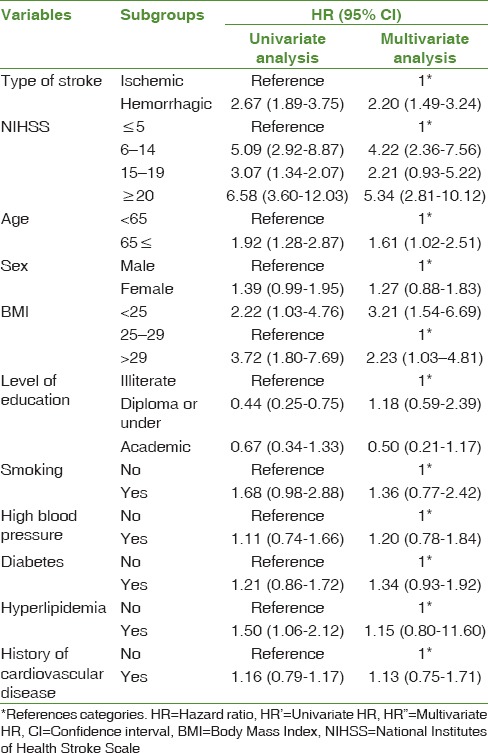
Based on the results of univariate Cox model analysis, among factors predicting mortality after 6-month follow-up for the first-ever strokecases, (with an HR above 1 on death events), hemorrhagic stroke, severity of NIHSS stroke, age over 65, female gender, high BMI, and hyperlipidemia were significant ones [Figure 2].
Figure 2.
Comparison of estimated probability of mortality between body mass index categories based on Kaplan–Meier method for first-ever stroke patients, East Azerbaijan Province, Iran
In the final multivariate Cox model, hemorrhagic stroke type, severity of stroke by NIHSS, and age ≥65 years were the most important determinant factors in the 180 days mortality event [Table 4].
Table 4.
Univariate and multivariate analysis of Cox model in predicting death event (6 months) for cases of first-time stroke, East Azerbaijan-Iran
Discussion
In this study, 23.3% of the patients died during the 6-month follow-up time. Six-month CFR was 51.2% in the hemorrhagic and 21.6% in the ischemic stroke. one-month CFR in Isfahan, Iran population was 32.0%, whereas in Senegal and Gambia, the corresponding values were 38.0%, and 27.0%, respectively.[20,21] The CFR in the ischemic stroke with a range of 14.4%–24.0% is lower than hemorrhagic type (37.6%–68.6%). The cumulative CFR 28 days after stroke is reported to be 11.8% in Iran.[22] In one study, one-year survival rate of patients was 78.3%.[23] In another study, the total CFR for FES was 20.6% for 28 days and 30.2% for 180 days after stroke.[24] In Khorasan, Iran, the in-hospital mortality rate for ischemic stroke was 30.7%.[25] Lack of structures such as specialized units for stroke and underutilization of thrombolysis considerably affect the management of acute stroke patients.
According to the present study, ischemic stroke comprised 77.0% of all stroke cases. In a study done by Delbari et al., ischemic stroke accounted for 75% of cases.[26] In other studies in Iran, for example, Daneshfard et al. reported that the ischemic type comprises 57.9%–87.0% of all stroke patients.[11] In Isfahan, Iran, 68.4% and 23.9% of all patients were ischemic and intracerebral hemorrhagic, respectively.[20]
In the present study, both types of stroke were more prevalent among men than women. In the univariate Cox model, 6-month mortality risk after stroke was 39% higher in women than men. This finding is consistent with the study done in Ardabil Province by Aminisani et al.[27] Nonsignificant difference in gender can be resulted from short observation time and younger age of the patients. The fact that the prevalence of stroke in men is more than women is related to the preventative effect of estrogen hormone against cardiovascular disease events.[28] In a study in South of Iran, higher in-hospital stroke mortality was seen in women and children.[29] In population-based studies in Iran, stroke rate was higher in women.[30] However, stroke in the age group of 15–45 years is 52% more prevalent in men than women.[31] However, the reason for the difference in incidence rates between Iran and the rest of the world is unknown.
The Stroke Severity Index NIHSS was one of the strongest predictors of 6-month mortality in both univariate and multivariate models. A significant increase in the 6-month mortality was observed with increase in NIHSS index. In the multivariate regression model, after adjusting for other variables, 65 years and above had 61% higher risk of mortality compared to the reference age (<65). Its sensitivity and specificity for prediction of 30-day fatality were 81% and 90%, respectively.[32] Level of consciousness, speech, and gaze were among the independent determinants of mortality (P = 0.030).[22] Patients with NIHSS ≥20 had a 90-day mortality rate of 50.5%, but all survivors were severely suffering from disability. Moreover, patients with NIHSS of 5 or less did not have any fatal event. Furthermore, 30% of the survivors had moderate disability and 70% of them recovered and discharged.[33]
Underweight patients had 3.21 (95% CI: 3.16–0.51) times HR for 6-month mortality in comparison with normal BMI patients. More mortality of low BMI results from pneumonia, nutritional deficiency, and less resistance to infections.[34,35] Overweight and obese patients had 2.23 (95% CI: 1.53–4.81) times more HR 6-month mortality than patient with normal BMI. In a study done in Japan, the Jichi Medical School cohort study, it was found that underweight (BMI below 18.5) men with an HR of 2.11; 95% CI: 1.17–3.82 were significantly at a greater risk of mortality. However, women with BMI of 30 and beyond (HR 2.25, 95% CI: 1.28–5.08) were significantly at a greater risk of mortality.[34]
In univariate analysis, among the important effective comorbidities of stroke (i.e., high blood pressure, diabetes, hyperlipidemia, and a history of cardiovascular disease), only hyperlipidemia had a significant correlation with 6-month mortality. In the multivariate analysis, however, none of the comorbidities had a significant correlation with 6-month mortality. Hypertension and history of ischemic heart disease were the most important risk factors contributing to stroke in Khorasan, Iran.[25] In fact, 53.1% and 22.3% of stroke patients were suffering from hypertension and history of ischemic heart disease, respectively. Hypertension, heart disease, and DM were among the most important stroke risk factors in Babol, Iran.[35] In a recent review in Iran, hypertension was one of the most important avoidable risk factors in ischemic type (54% of patients) and in (70.7% of hemorrhagic cases). In a study done in Shiraz by Daneshfard et al. 2015 (South of Iran), hypertension was identified as one of the most important risk factors and cigarette smoking ranked the fourth-factor causing stroke risk.[11]
Conclusion
Severity of stroke by NIHSS was the most prominent factor in stroke patients' mortality. A better evaluation of the predictors of mortality after stroke can be achieved by increasing the follow-up time. Determining the underlying causes of death was a difficult issue in which medical staff is faced with. In this study, the underlying cause of death was inquired from patients' relatives by telephone (telephone-based follow-up). Only those cases whose underlying cause of death was stroke were included in our analysis. The fact that the present study is a hospital based rather than population based may invite criticism regarding the accuracy of its findings. Although the confounding factors of this study were controlled in the regression model during the analysis phase by adjusting method, we were not able to measure the severity of the other comorbidities in the present study. Strengths of this study comprise the use of two hospitals sources to find cases of stroke, including revisiting all cases. Furthermore, our study provides unique data, being the first population-based study of stroke in our province with middle-term outcome after stroke.
Because of the high frequency of stroke in this province, policy shall focus on promoting stroke care interventions, as well as, raising awareness about the risk factors.
Financial support and sponsorship
The study was reviewed and approved by the Ethics Committee of Tabriz University of Medical Sciences (TBZMED. REC.1393.512). Informed consent was obtained from all participants. This study was funded by the Research Department of Tabriz University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This article is the result of a research project approved and sponsored by Health Faculty of Tabriz University of Medical Sciences. The authors appreciate the authorities and all colleagues and people participating in this study.
References
- 1.Ghandehari K. Epidemiology of stroke in Iran. Galen Med J. 2016;5:3–9. [Google Scholar]
- 2.Towfighi A, Saver JL. Stroke declines from third to fourth leading cause of death in the United States: Historical perspective and challenges ahead. Stroke. 2011;42:2351–5. doi: 10.1161/STROKEAHA.111.621904. [DOI] [PubMed] [Google Scholar]
- 3.Béjot Y, Daubail B, Giroud M. Epidemiology of stroke and transient ischemic attacks: Current knowledge and perspectives. Rev Neurol (Paris) 2016;172:59–68. doi: 10.1016/j.neurol.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 4.Feigin VL, Norrving B, Mensah GA. Global burden of stroke. Circ Res. 2017;120:439–48. doi: 10.1161/CIRCRESAHA.116.308413. [DOI] [PubMed] [Google Scholar]
- 5.Sienkiewicz-Jarosz H, Głuszkiewicz M, Pniewski J, Niewada M, Członkowska A, Wolfe C, et al. Incidence and case fatality rates of first-ever stroke-comparison of data from two prospective population-based studies conducted in Warsaw. Neurol Neurochir Pol. 2011;45:207–12. doi: 10.1016/s0028-3843(14)60073-6. [DOI] [PubMed] [Google Scholar]
- 6.Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: A review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003;2:43–53. doi: 10.1016/s1474-4422(03)00266-7. [DOI] [PubMed] [Google Scholar]
- 7.Bank World. Data for Iran, Islamic Rep. Upper Middle Income. 2017. Available date 2018 Jun 30. Available from: https://www.data.worldbank.org/country/iran-islamic-rep .
- 8.Sidney S, Rosamond WD, Howard VJ, Luepker RV. The “heart disease and stroke statistics-2013 update” and the need for a national cardiovascular surveillance system. Circulation. 2013;127:21–3. doi: 10.1161/CIRCULATIONAHA.112.155911. [DOI] [PubMed] [Google Scholar]
- 9.Di Carlo A, Lamassa M, Baldereschi M, Pracucci G, Consoli D, Wolfe CD, et al. Risk factors and outcome of subtypes of ischemic stroke. Data from a multicenter multinational hospital-based registry. The European community stroke project. J Neurol Sci. 2006;244:143–50. doi: 10.1016/j.jns.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 10.Hosseini AA, Sobhani-Rad D, Ghandehari K, Benamer HT. Frequency and clinical patterns of stroke in Iran – Systematic and critical review. BMC Neurol. 2010;10:72. doi: 10.1186/1471-2377-10-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daneshfard B, Izadi S, Shariat A, Toudaji MA, Beyzavi Z, Niknam L, et al. Epidemiology of stroke in Shiraz, Iran. Iran J Neurol. 2015;14:158–63. [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson M, Bakas T. A review of barriers to thrombolytic therapy: Implications for nursing care in the emergency department. J Neurosci Nurs. 2010;42:88–94. [PubMed] [Google Scholar]
- 13.Appelros P, Stegmayr B, Terént A. Sex differences in stroke epidemiology: A systematic review. Stroke. 2009;40:1082–90. doi: 10.1161/STROKEAHA.108.540781. [DOI] [PubMed] [Google Scholar]
- 14.O'Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): A case-control study. Lancet. 2010;376:112–23. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 15.Center Iranian Statistics. East Azerbaijan Province. 2016. [Available date 2018 Jun 30]. Available from: https://www.amar.org.ir/
- 16.Thorvaldsen P, Asplund K, Kuulasmaa K, Rajakangas AM, Schroll M. Stroke incidence, case fatality, and mortality in the WHO MONICA project. World Health Organization monitoring trends and determinants in cardiovascular disease. Stroke. 1995;26:361–7. doi: 10.1161/01.str.26.3.361. [DOI] [PubMed] [Google Scholar]
- 17.Timsit S, Nowak E, Rouhart F, Goas P, Merrien FM, Tirel-Badet A, et al. High completeness of the brest stroke registry evidenced by analysis of sources and capture-recapture method. Neuroepidemiology. 2014;42:186–95. doi: 10.1159/000358802. [DOI] [PubMed] [Google Scholar]
- 18.Bethesda (MD): National Heart, Lung, and Blood Institute (US); 2004. National High Blood Pressure Education Program. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. [PubMed] [Google Scholar]
- 19.Zimmet P, Alberti K, Shaw J. International diabetes federation: the IDF consensus worldwide definition of the metabolic syndrome. Diabetes Voice. 2005;50:31–3. [Google Scholar]
- 20.Oveisgharan S, Sarrafzadegan N, Shirani S, Hosseini S, Hasanzadeh P, Khosravi A. Stroke in Isfahan, Iran: Hospital admission and 28-day case fatality rate. Cerebrovasc Dis. 2007;24:495–9. doi: 10.1159/000110418. [DOI] [PubMed] [Google Scholar]
- 21.Sagui E, M'Baye PS, Dubecq C, Ba Fall K, Niang A, Gning S, et al. Ischemic and hemorrhagic strokes in Dakar, Senegal: A hospital-based study. Stroke. 2005;36:1844–7. doi: 10.1161/01.STR.0000177864.08516.47. [DOI] [PubMed] [Google Scholar]
- 22.Zandieh A, Kahaki ZZ, Sadeghian H, Fakhri M, Pourashraf M, Parviz S, et al. A simple risk score for early ischemic stroke mortality derived from national institutes of health stroke scale: A discriminant analysis. Clin Neurol Neurosurg. 2013;115:1036–9. doi: 10.1016/j.clineuro.2012.10.034. [DOI] [PubMed] [Google Scholar]
- 23.Karnik R, Valentin A, Ammerer HP, Hochfelner A, Donath P, Slany J. Outcome in patients with intracerebral hemorrhage: Predictors of survival. Wien Klin Wochenschr. 2000;112:169–73. [PubMed] [Google Scholar]
- 24.Janes F, Gigli GL, D'Anna L, Cancelli I, Perelli A, Canal G, et al. Stroke incidence and 30-day and six-month case fatality rates in Udine, Italy: A population-based prospective study. Int J Stroke. 2013;8(Suppl A100):100–5. doi: 10.1111/ijs.12000. [DOI] [PubMed] [Google Scholar]
- 25.Ghandehari K, Izadi Z Khorasan Stroke Registry. The Khorasan stroke registry: Results of a five-year hospital-based study. Cerebrovasc Dis. 2007;23:132–9. doi: 10.1159/000097050. [DOI] [PubMed] [Google Scholar]
- 26.Delbari A, Salman Roghani R, Tabatabaei SS, Lökk J. A stroke study of an urban area of Iran: Risk factors, length of stay, case fatality, and discharge destination. J Stroke Cerebrovasc Dis. 2010;19:104–9. doi: 10.1016/j.jstrokecerebrovasdis.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 27.Amini Sani N, Oscoie S, Shamshirgaran SM, Dastgiri S. One month mortalty rate of storke in Ardabil. J Ardabil Univ Med Sci. 2007;7:353–6. [Google Scholar]
- 28.Zhang C, Lan T, Zhe Y, Hu B, Zhang G, He J, et al. Epidemiology investigation of stroke among Mongolian and Han population aged over 45 in inner Mongolia. Sci Rep. 2017;7:45710. doi: 10.1038/srep45710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Borhani-Haghighi A, Safari R, Heydari ST, Soleimani F, Sharifian M, Yektaparast Kashkuli S, et al. Hospital mortality associated with stroke in Southern Iran. Iran J Med Sci. 2013;38:314–20. [PMC free article] [PubMed] [Google Scholar]
- 30.Azarpazhooh MR, Etemadi MM, Donnan GA, Mokhber N, Majdi MR, Ghayour-Mobarhan M, et al. Excessive incidence of stroke in Iran: Evidence from the Mashhad stroke incidence study (MSIS), a population-based study of stroke in the Middle East. Stroke. 2010;41:e3–10. doi: 10.1161/STROKEAHA.109.559708. [DOI] [PubMed] [Google Scholar]
- 31.Ghandehari K, Moud ZI. Incidence and etiology of ischemic stroke in Persian young adults. Acta Neurol Scand. 2006;113:121–4. doi: 10.1111/j.1600-0404.2005.00515.x. [DOI] [PubMed] [Google Scholar]
- 32.Cheung CM, Tsoi TH, Hon SF, Au-Yeung M, Shiu KL, Lee CN, et al. Using the national institutes of health stroke scale (NIHSS) to predict the mortality and outcome of patients with intracerebral haemorrhage. Hong Kong Med J. 2008;14:367–70. [PubMed] [Google Scholar]
- 33.Dawodu CO, Danesi MA. Relationship of national institute of health stroke scores [NIHSS] to 90 days mortality in Africa. Niger Postgrad Med J. 2008;15:259–63. [PubMed] [Google Scholar]
- 34.Kawate N, Kayaba K, Hara M, Kotani K, Ishikawa S Jichi Medical School Cohort Study Group. Body mass index and stroke incidence in Japanese community residents: The Jichi medical school (JMS) cohort study. J Epidemiol. 2017;27:325–30. doi: 10.1016/j.je.2016.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ahangar AA, Ashraf Vaghefi SB, Ramaezani M. Epidemiological evaluation of stroke in Babol, northern Iran (2001-2003) Eur Neurol. 2005;54:93–7. doi: 10.1159/000088643. [DOI] [PubMed] [Google Scholar]


