Abstract
Intravascular ultrasound (IVUS)-guided guidewire manipulation technique is often useful to cross the lesion of chronic total occlusion (CTO) antegradely and solve retrograde CTO failure cases. However, this technique is usually complex because we need many devices and it requires many steps. Some steps usually take time and/or sometimes create a large dissection space which cause the procedure to fail. To overcome a weakness in this technique, we introduce the new IVUS-guided wiring technique with double lumen catheter named “Slipstream technique” here. This technique is simple, easy, and associated with less injury. It will be helpful for penetrating into the true lumen from the subintimal space with a guidewire correctly and safely.
<Learning objective: IVUS-guided wiring technique in the treatment of chronic total occlusion is usually complex. The key point of new IVUS-guided wiring technique is to put both the IVUS catheter and double lumen catheter on the same wire. This manner is simple. Moreover, it will increase the stability of double lumen catheter and be helpful to manipulate the second guidewire effectively.>
Keywords: Intravascular ultrasound-guided wiring, Double lumen catheter, Chronic total occlusion
Introduction
After the introduction of the retrograde approach [1], the success rate of percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) increased by up to 80–90% [2]. However, there are some situations in which it is difficult to advance the guide wire and microcatheter into the CTO lesion, even though the guide wire and microcatheter can pass through the collateral channel retrogradely [3]. Although intravascular ultrasound (IVUS)-guided guidewire manipulation is often useful to cross the lesion [4], [5], [6] and solve retrograde CTO-PCI failure cases, this technique is usually complex because we need many devices and it requires many steps.
In addition, the performance of guidewires is sometimes reduced by instability or entanglement. Here, we introduce a more simple and effective IVUS-guided wiring technique with a double lumen catheter for the treatment of CTOs.
Case report
A 64-year-old male with stable angina was admitted to a hospital. Coronary angiography showed severe stenosis in the distal part of the right coronary artery (RCA) and a CTO in the proximal left anterior descending artery (LAD). The first attempt at recanalization of the LAD-CTO was performed in September 2015 after the treatment of RCA, but unfortunately it failed. The doctor who performed the procedure consulted us about the 2nd attempt for the LAD-CTO, so we decided to try again after some discussion.
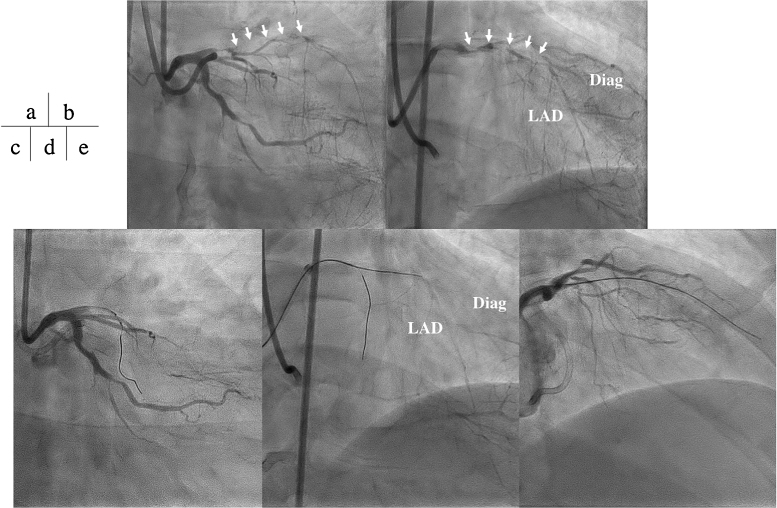
In May 2016, the 2nd attempt for PCI was performed. Angiography revealed a CTO of the proximal LAD (Fig. 1a, b), confirming that nothing changed in comparison to the prior session. With an 8-Fr guiding catheter, a SION blue (Asahi Intec, Nagoya, Japan) was inserted into a septal branch to check the entry point by IVUS (NavifocusWR; Terumo Corp., Tokyo, Japan) (Fig. 1c). Gaia 1st (Asahi Intec, Nagoya, Japan) was inserted into the CTO lesion first, and subsequently exchanged for Gaia 2nd (Asahi Intec) inside the lesion because of tissue stiffness. Gaia 2nd advanced gradually and passed into the diagonal branch (Fig. 1d, e). After passing Gaia 2nd into the diagonal branch, we changed it to floppy guidewire (SION blue) to avoid the coronary perforation. We tried to insert another guidewire (SION blue) into the LAD with a double lumen catheter (SASUKE; Asahi Intec), but it could not advance. To understand the reason why, we observed the bifurcation between the LAD and the diagonal branch by IVUS. After the dilation with 1.5 mm balloon catheter, we advanced IVUS catheter to the distal part of diagonal branch. The IVUS image showed that there was a single-layered wall between LAD and the diagonal branch (Fig. 2). To puncture this wall correctly, we decided to use an IVUS-guided wiring technique.
Fig. 1.
Baseline coronary angiography in the right oblique caudal projection (a) and the right oblique cranial projection (b). CTO begins from the proximal of LAD to the bifurcation between LAD and diagonal branch (Diag) (arrow). (c) Intravascular ultrasound catheter was inserted in septal branch to identify the entrance of occluded LAD (arrow). (d) Guidewire (Gaia 2nd) advanced close to the end of CTO (arrow). (e) Gaia 2nd passed into diagonal branch.
CTO, Chronic total occlusion; LAD, left anterior descending artery.
Fig. 2.
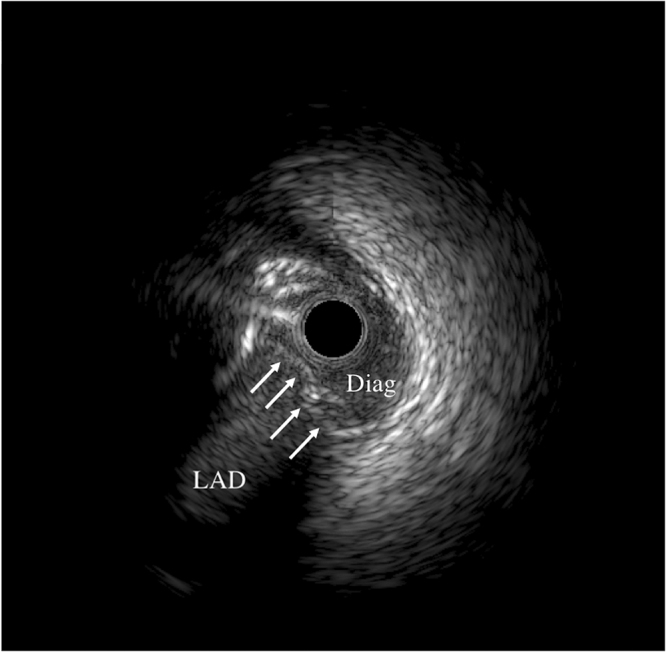
Intravascular ultrasound image showed that there was a barrier between diagonal branch (Diag) and the left anterior descending artery (LAD) (arrow).
In the case of usual IVUS-guided wiring techniques, we insert another guidewire and microcatheter along the IVUS catheter. This process sometimes takes a lot of time. Moreover, this step may make a large dissection space and cause the procedure to fail. To avoid this situation, we evolved a new method named the “Slipstream” technique.
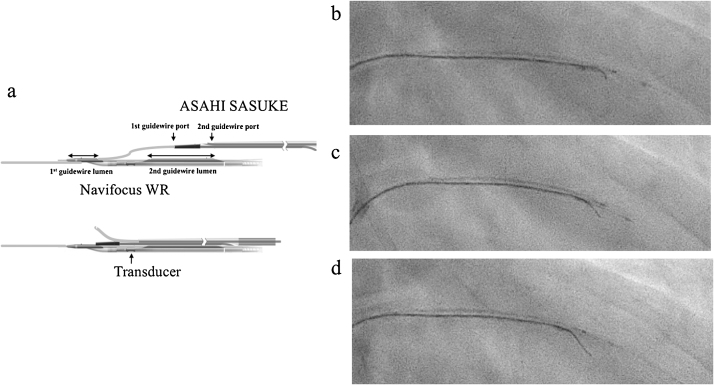
After pulling out the IVUS catheter once, we inserted it again using only the 1st guidewire lumen. Afterwards, we put the double lumen catheter on the same guidewire which was used in the IVUS catheter and advanced it to the tip of the IVUS catheter. By using the 1st guidewire lumen only, the double lumen catheter reaches closer to the tip of IVUS catheter (Fig. 3a), thereby significantly increasing the stability. In addition, the 2nd guidewire port of SASUKE is close to the transducer of NavifocusWR in this system. This makes it helpful and easy to identify the tip of the guidewire on the IVUS image during the procedure.
Fig. 3.
(a) The scheme of “Slipstream” technique. Although, we usually pass the guidewire through both 1st and 2nd guidewire lumen to get strong support during the procedure when we used NavifocusWR intravascular ultrasound (IVUS) catheter, guidewire is passed through 1st guidewire lumen only in this technique. And then, ASAHI SASUKE was put on the same guidewire and advances up to the tip of IVUS catheter.
The picture shows before (b) and immediately after (c) puncture and passing into left anterior descending artery (d).
Using this system, we could puncture the barrier with the new Gaia 2nd as the 2nd guidewire and advance it into the LAD correctly (Fig. 3b–d and Movie 1). Finally, we put a stent in the LAD and finished the procedure.
Discussion
We introduced a new IVUS-guided wiring technique with double lumen catheter in this report. The advantage of this technique is simple and more atraumatic in comparison to the previous one. In traditional methods [4], [5], [6], the 2nd guidewire alone or both guidewire and microcatheter have to be inserted along the IVUS catheter up to the transitional site between the true limen and subintimal space. This step in the procedure usually takes time and/or sometimes creates a large dissection space which causes the procedure to fail. To prevent a waste of time and a risk like this, it is effective to put and advance the double lumen catheter on the 1st guidewire which was used for insertion of the IVUS catheter. In most cases, it is easy and safe to advance both the IVUS catheter and the double lumen catheter in a gentle manner after the dilation with small-sized balloon catheter. In addition, the stability of the double lumen catheter is better than a usual microcatheter in the vessel when manipulating the guidewire. In our experiment, a double lumen catheter was able to retain its position in the center of the phantom vessel when we rotated the 2nd guidewire from the side port, because of an anchor effect of the 1st guidewire. In contrast, a usual microcatheter would not be able to keep its position during the guidewire manipulation (Movies 2 and 3).
We named this technique “Slipstream” technique. Although “Slipstream” is one of the technical terms of hydrodynamics, this term is often used in the field of motor sports. By using this phenomenon, the following car or motorcycle just behind the former one can easily overtake it.
The situation where a double lumen catheter and IVUS catheter are very close and the 2nd guidewire can easily penetrate the distal fibrous cap or the barrier between the true lumen and subintimal space is similar to the “Slipstream” technique in the field of motor sports. This is the reason why we named this technique “Slipstream” technique.
For this technique, various double lumen catheters and IVUS catheters are available. Currently, we use 2 double lumen catheters in Japan (SASUKE and Crusade; KANEKA, Osaka, Japan). Although both catheters are high-spec, a thinner and lubricious tip is better in this technique as it reduces the risk of injury. The tip of SASUKE is the same as that of Corsair (Asahi Intec), making it thinner (1.5 Fr vs 2.2–2.4 Fr) and more lubricious than Crusade. In our personal opinion, the SASUKE is better suited for this technique, although it is also possible to use Crusade.
In addition, there are also some limitations regarding the selection of IVUS catheters. When we need to puncture from the subintimal space into the true lumen, we have to insert the IVUS catheter into the subintimal space once [4], [5], [6]. Inserting as short a section of the catheter as possible is important in order to minimize vessel damage. Therefore, the IVUS catheter which has the shortest distance from the tip to transducer and a small shaft profile is optimal in this technique. Several IVUS catheters are available in Japan. As NavifocusWR has the shortest distance from the tip to transducer (9 mm) and a small shaft profile (2.5 Fr), we usually use this catheter in this technique. In our personal experience, Opticross (Boston Scientific Corporation, Fremont, CA, USA) and Eagle Eye (Volcano Corporation, San Diego, CA, USA) are also possible for this technique.
In most cases, we need strong penetration force to penetrate the barrier between the main branch and side branch. As the selection of the 2nd guidewire, the tapered stiff wire like Gaia family or Conquest family (Asahi Intec) is recommended.
We usually use an 8-Fr guiding catheter in this technique. As both the double lumen catheter and IVUS catheter are inserted into a guiding catheter at the same time, an 8 Fr-guiding catheter is usually recommended except for the combination of Opticross and SASUKE. This combination is only available in a 7-Fr guiding catheter. In the future, if the profile size of the double lumen catheter and/or IVUS catheter becomes smaller, we will be able to use a small-sized guiding catheter.
Conclusion
We report on a case in which a new IVUS-guided wiring technique that involves a double lumen catheter named “Slipstream” technique was used for the treatment of a CTO. This technique makes the 2nd guidewire more stable and facilitates the penetration of the guidewire from the subintimal space into the true lumen.
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jccase.2017.04.007.
Appendix A. Supplementary data
The following are Supplementary data to this article:
Movie showed the motion of the tip of guidewire. Guidewire penetrated the barrier between diagonal branch and LAD (scene 6–10 s).
Movie showed the motion of double lumen catheter during the manipulation of 2nd guidewire. Upper panel showed cross-sectional view and lower panel showed overview of phantom vessel.
Movie showed the motion of usual microcatheter during the manipulation of guidewire. Upper panel showed cross-sectional view and lower panel showed overview of phantom vessel. When the guidewire rotated, position of microcatheter changed its position to various direction.
References
- 1.Surmely J.F., Tsuchikane E., Katoh O., Nishida Y., Nakayama M., Nakamura S. New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J Invasive Cardiol. 2006;18:334–338. [PubMed] [Google Scholar]
- 2.Habara M., Tsuchikane E., Muramatsu T., Kashima Y., Okamura A., Mutoh M. Comparison of percutaneous coronary intervention for chronic total occlusion outcome according to operator experience from the Japanese retrograde summit registry. Catheter Cardiovasc Interv. 2016;87:1027–1035. doi: 10.1002/ccd.26354. [DOI] [PubMed] [Google Scholar]
- 3.Suzuki Y., Muto M., Yamane M., Muramatsu T., Okamura A., Igarashi Y. Independent predictors of retrograde failure in CTO-PCI after successful collateral channel crossing. Catheter Cardiovasc Interv. 2016;(September (21)) doi: 10.1002/ccd.26785. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Matsubara T., Murata A., Kanyama H., Ogino A. IVUS-guided wiring technique: promising approach for the chronic total occlusion. Catheter Cardiovasc Interv. 2004;61:381–386. doi: 10.1002/ccd.10796. [DOI] [PubMed] [Google Scholar]
- 5.Okamura A., Iwakura K., Fujii K. ViewIT improves intravascular ultrasound-guided wiring in coronary intervention of chronic total occlusion. Catheter Cardiovasc Interv. 2010;75:1062–1066. doi: 10.1002/ccd.22427. [DOI] [PubMed] [Google Scholar]
- 6.Ito S., Suzuki T., Ito T., Katoh O., Ojio S., Sato H. Novel technique using intravascular ultrasound-guided guidewire cross in coronary intervention for uncrossable chronic total occlusions. Circ J. 2004;68:1088–1092. doi: 10.1253/circj.68.1088. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Movie showed the motion of the tip of guidewire. Guidewire penetrated the barrier between diagonal branch and LAD (scene 6–10 s).
Movie showed the motion of double lumen catheter during the manipulation of 2nd guidewire. Upper panel showed cross-sectional view and lower panel showed overview of phantom vessel.
Movie showed the motion of usual microcatheter during the manipulation of guidewire. Upper panel showed cross-sectional view and lower panel showed overview of phantom vessel. When the guidewire rotated, position of microcatheter changed its position to various direction.