Abstract
An 82-year-old woman with symptomatic severe aortic stenosis (AS) developed an obstructive ileus caused by colon cancer. Colectomy was considered a high-risk surgery due to both the severe AS and obstructive ileus. Therefore, we planned placement of a colonic stent for the obstructive ileus. After stenting, we performed transcatheter aortic valve implantation (TAVI) instead of surgical aortic valve replacement (SAVR), because of the risk of bleeding during extracorporeal circulation and the perioperative risk of AVR (Society of Thoracic Surgery predicted risk of mortality: 7.4%). Successful colonic stenting and TAVI allowed a safer colectomy. The period from TAVI to colectomy was 12 days. TAVI could be useful for symptomatic severe AS in high-risk patients prior to non-cardiac surgery, especially for malignant tumors.
<Learning objective: In patients with symptomatic severe aortic stenosis, aortic valve replacement is recommended prior to non-cardiac surgery. However, in patients with a malignancy, the complications due to the tumor and the risk of extracorporeal circulation remain a challenge in surgical aortic valve replacement. In such cases, transcatheter aortic valve implantation may be a useful option to reduce the incidence of complications and the time to surgery for the malignancy.>
Keywords: Aortic stenosis, Transcatheter aortic valve implantation, Non-cardiac surgery, Colon cancer, Obstructive ileus
Introduction
Severe aortic stenosis (AS) is a known risk factor for mortality and morbidity in patients undergoing non-cardiac surgery [1]. In patients with symptomatic severe AS, surgical aortic valve replacement (SAVR) prior to non-cardiac surgery is recommended [2]. However, SAVR is considered a high-risk procedure in patients with frailty, history of coronary artery bypass grafting, porcelain aorta, or history of chest irradiation. For these patients, balloon aortic valvuloplasty (BAV) could be a therapeutic option [3]. Recently, transcatheter aortic valve implantation (TAVI) has emerged as an alternative for patients with intermediate or high surgical risk [4], but the usefulness of TAVI prior to non-cardiac surgery remains unclear.
We report a case in which preceding SAVR was difficult due to complex medical problems, and multiple therapies including TAVI were effective prior to non-cardiac surgery.
Case report
An 85-year-old woman without significant past medical history was referred to our hospital due to severe AS. She presented with symptoms of dyspnea on exertion and leg edema (New York Heart Association class III) for one month.
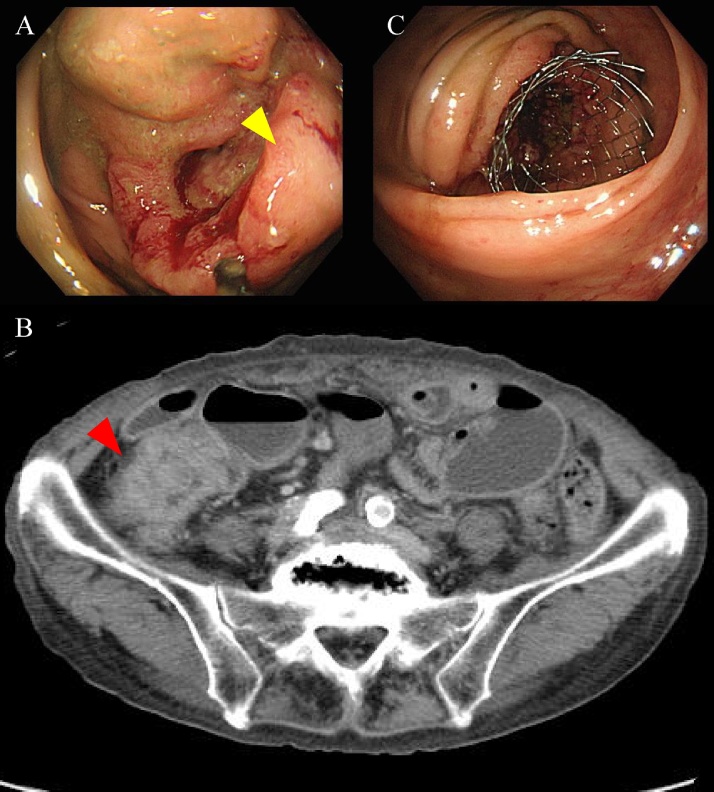
Echocardiography revealed severe AS (aortic valve area, 0.5 cm2; maximum jet velocity, 4.5 m/s; and mean aortic pressure gradient, 52 mmHg). She was found to have anemia (hemoglobin level: 8.9 mg/dl), and fiber optic colonoscopy confirmed advanced colon cancer in the ascending colon (Fig. 1A). On the 5th day after colonoscopy, the patient developed vomiting and was diagnosed with obstructive ileus due to ascending colon cancer (Fig. 1B). The patient was admitted with severe AS, obstructive ileus, and colon cancer.
Fig. 1.
(A) Colonoscopy showing advanced colon cancer (yellow arrowhead) and obstruction. (B) Contrast-enhanced computed tomography demonstrating colon cancer (red arrowhead) and obstructive ileus. (C) Colonic stenting resolved the obstruction caused by advanced colon cancer.
Colectomy for ascending colon cancer and obstructive ileus was recommended. However, the perioperative risk was high because the patient had symptomatic severe AS. Although preceding AVR was warranted based on European Society of Cardiology (ESC) guidelines [2], SAVR was high-risk because of potential bleeding during extracorporeal circulation and the perioperative risk of AVR (Society of Thoracic Surgery predicted risk of mortality: 7.4%). Furthermore, extracorporeal circulation during SAVR might increase the risk of cancer dissemination by immunosuppression [5]. The fluid therapy to maintain normovolemia for obstructive ileus was difficult due to severe AS. Considering the perioperative management of fluid therapy, obstructive ileus was also associated with an increased risk of both SAVR and colectomy.
A multidisciplinary cardiology team including interventional cardiologists and surgeons decided to place a colonic stent under endoscopic guidance to relieve colonic obstruction. After stenting on the 5th hospital day (Fig. 1C), we planned TAVI for severe AS.
Relief of obstructive ileus allowed the patient to undergo contrast-enhanced computed tomography (CT) and invasive coronary angiography (ICA). ICA revealed moderate stenosis in the midleft anterior descending artery and obtuse marginal artery.
Dual antiplatelet therapy for 6 months is recommended following an implantation of Sapien XT valve (Edwards Lifesciences, Irvine, CA, USA), but the patient had only been treated with aspirin in anticipation of colorectal surgery.
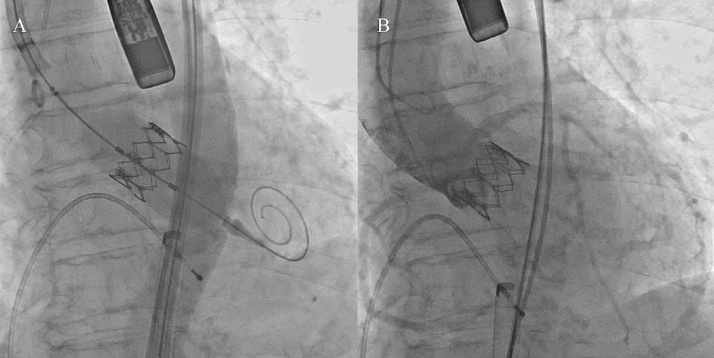
The patient underwent TAVI through the right femoral artery on the 23rd hospital day. A 23-mm Sapien XT valve was placed under fluoroscopic guidance (Fig. 2A). Complete correction of the transaortic pressure gradient from 63 mmHg to 11 mmHg was confirmed, and grade I aortic regurgitation was observed by angiography after valve replacement (Fig. 2B).
Fig. 2.
Fluoroscopy during transcatheter aortic valve implantation. (A) Implantation of 23-mm Sapien XT valve. (B) Aortography after valve deployment.
After successful TAVI, the patient remained on aspirin and underwent ileocecal resection and three-field lymph node dissection on the 35th hospital day. There were no complications, including bleeding, ischemic stroke, or valve thrombosis, after surgery. The pathological diagnosis was T3, N1, M0 tubular adenocarcinoma, pathological Stage IIIb. The patient was discharged on the 53rd hospital day.
Discussion
Severe AS is considered a high-risk indicator of cardiac complications during non-cardiac surgery [1]. Hypotension and tachycardia due to anesthesia and surgical stress can reduce coronary perfusion and may ultimately lead to myocardial infarction or death.
The ESC guidelines recommend SAVR in symptomatic patients with severe AS prior to intermediate-risk or high-risk non-cardiac surgery [2]. However, SAVR is considered a high-risk or ineligible procedure for several reasons, including frailty, history of coronary artery bypass grafting, porcelain aorta, and history of chest irradiation. The presence of cancer is often considered a contraindication to surgical intervention for severe AS. In patients with advanced cancer, bleeding events are also a serious concern because of extracorporeal circulation during cardiac surgery [6].
Recently, TAVI has emerged as a valid option for intermediate-risk or high-risk patients [4]. Previous studies reported that BAV was an effective option prior to non-cardiac surgery [3], whereas several limitations of BAV therapy were also reported. The improvement in transaortic pressure gradient was limited, and severe complications such as stroke, myocardial infarction, and aortic regurgitation, occurred in approximately 25% of the patients [7]. Considering the clinical outcome and the complication rate, TAVI can be an alternative option to BAV in patients with severe AS prior to non-cardiac surgery. In addition, compared with SAVR, TAVI is less invasive, avoiding sternotomy and extracorporeal circulation [4], and may reduce the risk of bleeding and enable faster recovery to facilitate non-cardiac surgery, especially in patients with malignant tumors.
In patients with obstructive ileus, the bowel becomes dilated proximal to the site of obstruction and fluid is sequestered due to impaired absorption. Since major fluid shifts into bowel occurs, patients require adequate fluid therapy to avoid hypovolemic shock [8]. In our case, the patient had obstructive ileus in addition to severe AS, and the management of fluid therapy was difficult. Therefore, we first performed colonic stenting to relieve colonic obstruction. Colonic stents are useful not only for palliation, but also for bridging to elective surgery for colonic obstruction. A previous randomized trial showed that colonic stent insertion for bridging to elective surgery reduced postoperative complications likely to result from emergent surgery [9].
After colonic stenting, the patient underwent TAVI and received aspirin alone. In a recent randomized controlled trial [4], all patients continued to take aspirin indefinitely and clopidogrel for a minimum of one month. The dual antiplatelet therapy after TAVI was aimed to avoid ischemic complications such as myocardial infarction and ischemic stroke. In contrast, it can also increase the risk of major bleeding. A recent report demonstrated that single antiplatelet therapy, aspirin alone, was associated with a tendency toward a lower rate of adverse events following TAVI compared to dual antiplatelet therapy [10]. Single antiplatelet therapy, aspirin alone, might sufficiently prevent ischemic events after TAVI. In patients before non-cardiac surgery, single antiplatelet therapy could reduce the perioperative risk during non-cardiac surgery and shorten the term between TAVI and non-cardiac surgery. Indeed, we did not prescribe dual antiplatelet therapy to reduce the risk of bleeding during colectomy, and we could perform colectomy without any complications including major bleeding, ischemic events, and valve thrombosis. Furthermore, the time between TAVI and colectomy was 12 days.
Conclusion
TAVI can be a useful option for symptomatic severe AS patients with high surgical risk prior to non-cardiac surgery. The colectomy with aspirin alone could be performed for colon cancer without any complications following TAVI. Furthermore, the time between diagnosis and colon surgery was relatively short. However, further studies are required to confirm the safety and efficacy of this strategy.
Conflict of interest
Dr Tanabe receives honoraria from Edwards Lifesciences and Medtronic. Dr Yokozuka receives honorarium from Edwards Lifesciences. Other authors report no conflicts of interest.
References
- 1.Skinner J.F., Pearce M.L. Surgical risk in the cardiac patient. J Chron Dis. 1964;17:57–72. doi: 10.1016/0021-9681(64)90039-6. [DOI] [PubMed] [Google Scholar]
- 2.Kristensen S.D., Knuuti J., Saraste A., Anker S., Botker H.E., Hert S.D. 2014 ESC/ESA guidelines on non-cardiac surgery: cardiovascular assessment and management: the Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA) Eur Heart J. 2014;35:2383–2431. doi: 10.1093/eurheartj/ehu282. [DOI] [PubMed] [Google Scholar]
- 3.Roth R.B., Palacios I.F., Block P.C. Percutaneous aortic balloon valvuloplasty: its role in the management of patients with aortic stenosis requiring major noncardiac surgery. J Am Coll Cardiol. 1989;13:1039–1041. doi: 10.1016/0735-1097(89)90258-1. [DOI] [PubMed] [Google Scholar]
- 4.Leon M.B., Smith C.R., Mack M.J., Makkar R.R., Svensson L.G., Kodali S.K. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016;374:1609–1620. doi: 10.1056/NEJMoa1514616. [DOI] [PubMed] [Google Scholar]
- 5.Yamamoto S., Yoshimasu T., Nishimura Y., Uchita S., Toguchi K., Honda K. In vitro evaluation of the effect of cardiac surgery on cancer cell proliferation. Ann Thorac Cardiovasc Surg. 2011;17:260–266. doi: 10.5761/atcs.oa.10.01585. [DOI] [PubMed] [Google Scholar]
- 6.Ascione R., Williams S., Lloyd C.T., Sundaramoorthi T., Pitsis A.A., Angelini G.D. Reduced postoperative blood loss and transfusion requirement after beating-heart coronary operations: a prospective randomized study. J Thorac Cardiovasc Surg. 2001;121:689–696. doi: 10.1067/mtc.2001.112823. [DOI] [PubMed] [Google Scholar]
- 7.Percutaneous balloon aortic valvuloplasty. Acute and 30-day follow-up results in 674 patients from the NHLBI Balloon Valvuloplasty Registry. Circulation. 1991;84:2383–2397. doi: 10.1161/01.cir.84.6.2383. [DOI] [PubMed] [Google Scholar]
- 8.Jackson P.G., Raiji M.T. Evaluation and management of intestinal obstruction. Am Fam Physician. 2011;83:159–165. [PubMed] [Google Scholar]
- 9.Ghazal A.H., El-Shazly W.G., Bessa S.S., El-Riwini M.T., Hussein A.M. Colonic endolumenal stenting devices and elective surgery versus emergency subtotal/total colectomy in the management of malignant obstructed left colon carcinoma. J Gastrointest Surg. 2013;17:1123–1129. doi: 10.1007/s11605-013-2152-2. [DOI] [PubMed] [Google Scholar]
- 10.Rodes-Cabau J., Masson J.B., Welsh R.C., Garcia Del Blanco B., Pelletier M., Webb J.G. Aspirin versus aspirin plus clopidogrel as antithrombotic treatment following transcatheter aortic valve replacement with a balloon-expandable valve: the ARTE (Aspirin Versus Aspirin + Clopidogrel Following Transcatheter Aortic Valve Implantation) randomized clinical trial. JACC Cardiovasc Interv. 2017;10:1357–1365. doi: 10.1016/j.jcin.2017.04.014. [DOI] [PubMed] [Google Scholar]