Abstract
Management of in-stent restenosis (ISR) remains challenging even in the drug-eluting stent era. We report the case of a Japanese female with repeated ISR after primary percutaneous coronary intervention (PCI) for acute coronary syndrome. We observed ISR tissue with “black hole” on intravascular ultrasound, which appeared to be heterogeneous tissue on optical frequency-domain imaging (OFDI). Paclitaxel-coated balloon dilatation of the ISR lesion with “black hole” was ineffective. The morphological assessment of ISR tissue using OFDI might be important to treat ISR lesions by PCI. OFDI is a novel tool to observe the difference in the in-stent tissue characteristics.
<Learning objective: In-stent restenosis (ISR) remains a clinical problem even in the drug-eluting stent (DES) era. The morphological assessment of ISR tissue using optical frequency-domain imaging (i.e. homogeneous, heterogeneous, and layered types) might be important to treat ISR lesions by percutaneous coronary intervention since the reaction to DES and drug-coating balloon seems to be different according to the in-stent tissue characteristics.>
Keywords: Black hole, Restenosis, Second-generation drug-eluting stent, Intravascular ultrasound, Optical frequency-domain imaging
Introduction
In-stent restenosis (ISR) remains a clinical problem, although drug-eluting stents (DES) reduced the rate of restenosis through inhibition of cell proliferation compared with bare-metal stents (BMS) [1]. Progress in intracoronary imaging modalities has enabled the morphological assessment of ISR tissue. Optical frequency-domain imaging (OFDI) findings of ISR tissue structure were classified into several types: homogeneous, heterogeneous, and layered types [2]. The morphological assessment of ISR tissue might be important to treat ISR lesions [3]. We report the case of a Japanese female with repeated ISR after primary percutaneous coronary intervention (PCI) for acute coronary syndrome, in whom we evaluated the restenotic tissue over time using intravascular ultrasound (IVUS) and OFDI.
Case report
A 63-year-old woman with a history of dyslipidemia was admitted to our hospital with acute coronary syndrome. Coronary angiography (CAG) showed significant stenosis of the mid left anterior descending artery (LAD) (Fig. 1a). A 3.0 × 16 mm platinum–chromium everolimus-eluting stent was implanted directly (Fig. 1b). Routine follow-up angiography 7 months later showed ISR [OFDI-derived minimal lumen area (MLA): 0.72 mm2] (Fig. 1c). The appearance of ISR on IVUS (OptiCross, Boston Scientific, Natick, MA, USA) included homogeneous echo-lucent intraluminal tissue, the so called “black hole” (Fig. 2 upper and middle panels) [4], [5]. On OFDI (FastView, Terumo, Tokyo, Japan), it appeared to be heterogenic low-intensity smooth sponge-like tissue (Fig. 2, lower panels). The restenotic “black hole” lesion was dilated from segment “B” through segment “C” with a 3.0 × 15 mm paclitaxel-coated balloon (PCB) after dilatation with a 3.0-mm scoring balloon (Fig. 2, right panel), whereas segment “A” was not dilated since the stenosis was not considered significant (angiographic % diameter stenosis was 50%). Follow-up angiography 11 months later showed ISR with “black hole” on IVUS again (OFDI-derived MLA: 1.21 mm2). In segment “A”, which was not dilated with PCB, progression and abundant bright punctate structures with backward attenuation were observed in the smooth heterogeneous sponge-like tissue on OFDI (Fig. 3, middle panels). Bright puncta in the heterogeneous tissue on OFDI developed in the proximal stent segment without PCB dilatation, whereas these were not observed in the distal stent segment with PCB dilatation. These bright puncta were not observed at 7 months follow-up (Fig. 2, lower panels; Fig. 3, upper panels). The lesion of repeated restenosis with “black hole” was dilated with a 3.0 mm scoring balloon including segment “A”. Follow-up angiography 16 months later also showed ISR (OFDI-derived MLA: 1.59 mm2). However, the FFR value was 0.93 for LAD and PCI was not performed. The appearance of ISR on IVUS included “black hole” again, where the same appearance was found on OFDI (Fig. 3, lower panels). Progression of heterogeneous tissue with bright puncta was observed around the proximal stent edge.
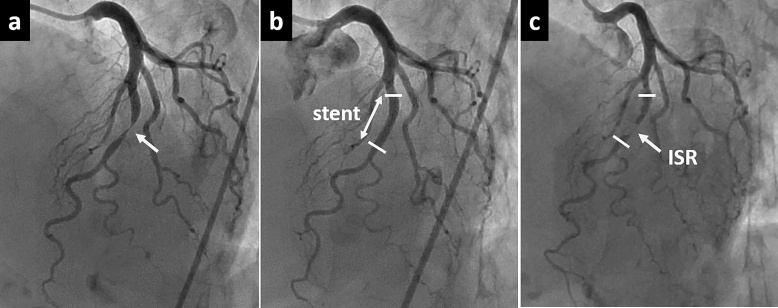
Fig. 1.
(a) Immediate coronary angiography for acute coronary syndrome showed a significant stenosis atmid left anterior descending artery. (b) A 3.0 × 16 mm platinum–chromium everolimus-eluting stent was implanted directly. (c) Follow-up angiography 7 months later showed in-stent restenosis (ISR).
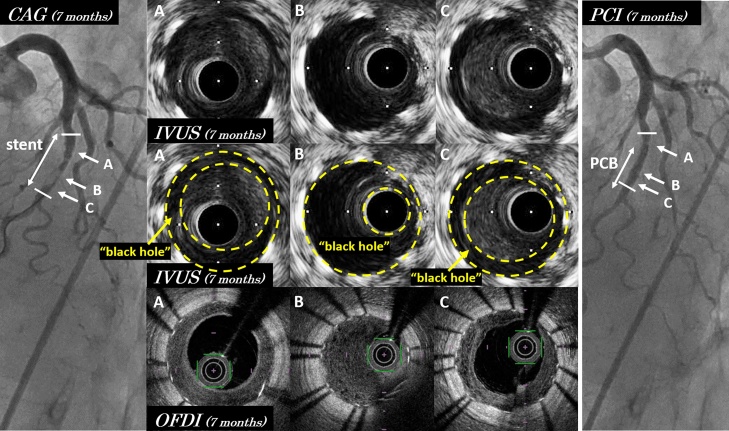
Fig. 2.
Coronary angiography, intravascular ultrasound (IVUS), and optical frequency-domain imaging (OFDI) 7 months later. IVUS images of in-stent restenosis (upper and middle panels) showed homogeneous echo-lucent intraluminal tissue, the so-called “black hole”. “Black hole” is the tissue surrounded with yellow lines. In-stent restenosis on OFDI (lower panels) showed low-intensity smooth heterogeneous sponge-like tissue. Segment “B” and “C” was dilated with paclitaxel-coated balloon (PCB), whereas segment “A” was not dilated with PCB (right panel).
PCI, percutaneous coronary intervention; CAG, coronary angiography.
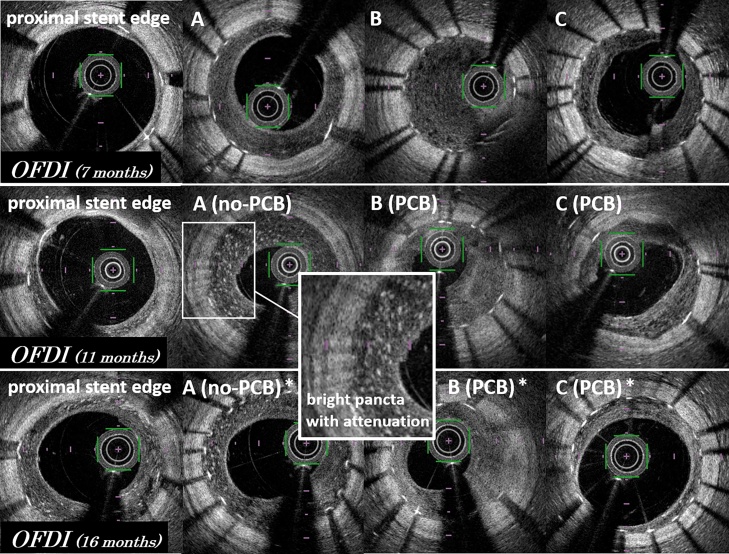
Fig. 3.
Time course of restenotic tissue characteristics on optical frequency-domain imaging (OFDI). Upper panels show OFDI images 7 months later. OFDI images of segment “A” 11 months later (middle panel) showed abundant bright puncta with backward attenuation. Bright puncta developed in the proximal stent segment without paclitaxel-coated balloon (PCB) dilatation, not in the distal stent segment with PCB dilatation. These were not observed on the intravascular ultrasound. On OFDI 16 months later (lower panels), heterogeneous tissue with bright puncta had progressed around the proximal stent edge.
*The restenotic lesion including segment “A” was dilated with a 3.0 mm scoring balloon 11 months later.
Discussion
“Black hole” on IVUS is defined as homogeneous echo-lucent intraluminal tissue. Histopathological assessment of “black hole” tissue showed hypocellular tissue with proteoglycan- or fibrin-rich extracellular matrix (ECM), lacking connective tissue [1], [6]. The hypocellular tissue may look echo-lucent on IVUS. It is thought that “black hole” may be associated with brachytherapy [5], [7] or sirolimus-eluting stent (SES) implantation [6], [8]. Since the bare-metal stent era, neointimal formation is well-known to involve not only cell proliferation but also ECM accumulation [9]. The use of DES has reduced the occurrence of ISR through inhibition of cell proliferation. However, DES-ISR tissue contains abundant proteoglycan/fibrin-rich ECM compared with BMS-ISR tissue [1]. “Black hole” tissue is similar to DES-ISR tissue, and could be related to the polymer or drug of DES.
OFDI findings of ISR tissue structure were classified into several types: homogeneous, heterogeneous, and layered types [2]. In our case, we observed the time course of “black hole” on IVUS using OFDI. “Black hole” appeared as low-intensity heterogeneous smooth sponge-like tissue on OFDI. Bright puncta in the heterogeneous tissue on OFDI 11 months later developed in the proximal stent segment without PCB dilatation, whereas these were not observed in the distal stent segment with PCB dilatation. Therefore, we presume that the appearance of numerous bright puncta represents the natural time course of heterogeneous tissue. Histopathological examination of “black hole” tissue was reported to include organized fibrin with a few mononuclear giant cells, indicating macrophage infiltration [10]. Macrophages detected by OFDI are seen as high reflective puncta with attenuation, whereas IVUS cannot detect the presence of macrophages. Although bright puncta look like macrophages, it is unknown whether bright puncta on OFDI represent infiltrated macrophages.
PCB dilatation of the restenotic tissue with “black hole” was ineffective in our case. Tada et al. [3] showed that the re-ISR rate after PCB for ISR lesions with heterogeneous tissue on optical coherence tomography was higher compared with the re-ISR rate after plain old balloon angioplasty (POBA) or DES (PCB: 38.5%, POBA: 20.0%, DES: 18.8%). Various drugs, such as paclitaxel, may have little effect on the hypocellular tissue. However, it is unclear from our case that POBA with scoring balloon was superior to PCB in ISR lesions with heterogeneous tissue on OFDI. Progression of heterogeneous tissue with bright puncta on OFDI was observed around the proximal stent edge. The appearance of bright puncta might be inhibited by PCB because these were not observed in the segment with PCB dilatation. The reaction to DES and drug-coating balloon seems to be different according to the in-stent tissue characteristics. The morphological assessment of ISR tissue using OFDI might be important to treat ISR lesions by PCI. OFDI is a novel tool to observe the difference in the in-stent tissue characteristics.
Conflict of interest
All authors do not have any conflict of interest.
References
- 1.Alfonso F., Byrne R.A., Rivero F., Kastrati A. Current treatment of in-stent restenosis. J Am Coll Cardiol. 2014;63:2659–2673. doi: 10.1016/j.jacc.2014.02.545. [DOI] [PubMed] [Google Scholar]
- 2.Gonzalo N., Serruys P.W., Okamura T., van Beusekom H.M., Garcia-Garcia H.M., van Soest G. Optical coherence tomography patterns of stent restenosis. Am Heart J. 2009;158:284–293. doi: 10.1016/j.ahj.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Tada T., Kadota K., Hosogi S., Miyake K., Ohya M., Amano H. Association between tissue characteristics assessed with optical coherence tomography and mid-term results after percutaneous coronary intervention for in-stent restenosis lesions: a comparison between balloon angioplasty, paclitaxel-coated balloon dilatation, and drug-eluting stent implantation. Eur Heart J Cardiovasc Imaging. 2015;16:1101–1111. doi: 10.1093/ehjci/jev031. [DOI] [PubMed] [Google Scholar]
- 4.Kay I.P., Wardeh A.J., Kozuma K., Sianos G., Regar E., Knook M. The pattern of restenosis and vascular remodelling after cold-end radioactive stent implantation. Eur Heart J. 2001;22:1311–1317. doi: 10.1053/euhj.2000.2542. [DOI] [PubMed] [Google Scholar]
- 5.Castagna M.T., Mintz G.S., Weissman N., Maehara A., Finet G., Waksman R. “Blackhole”: echolucentrestenotic tissue after brachytherapy. Circulation. 2001;103:778. doi: 10.1161/01.cir.103.5.778. [DOI] [PubMed] [Google Scholar]
- 6.Costa Jde R., Jr., Mintz G.S., Carlier S.G., Fujii K., Sano K., Kimura M. Frequency and determinants of black holes in sirolimus-eluting stent restenosis. J Invasive Cardiol. 2006;18:348–352. [PubMed] [Google Scholar]
- 7.Kay I.P., Ligthart J.M., Virmani R., van Beusekom H.M., Kozuma K., Carter A.J. The black hole: echolucent tissue observed following intracoronary radiation. Int J Cardiovasc Interv. 2003;5:137–142. doi: 10.1080/14628840310007673. [DOI] [PubMed] [Google Scholar]
- 8.Ratore S., Matsuo H., Suzuki T. Black hole phenomenon observed on IVUS after late restenosis following sirolimus-eluting stent implantation. J Invasive Cardiol. 2009;21:426–427. [PubMed] [Google Scholar]
- 9.Chung I.M., Gold H.K., Schwartz S.M., Ikari Y., Reidy M.A., Wight T.N. Enhanced extracellular matrix accumulation in restenosis of coronary arteries after stent deployment. J Am Coll Cardiol. 2002;40:2072–2081. doi: 10.1016/s0735-1097(02)02598-6. [DOI] [PubMed] [Google Scholar]
- 10.Suzuki N., Angiolillo D.J., Monteiro C., Shuja S., Futamatsu H., Kawaguchi R. Variable histological and ultrasonic characteristics of restenosis after drug-eluting stents. Int J Cardiol. 2008;130:444–448. doi: 10.1016/j.ijcard.2007.08.143. [DOI] [PubMed] [Google Scholar]