Abstract
A 45-year-old man presented with fatigue for the previous two days. Because of severe hypoxemia and chest radiograph showing severe consolidation only in the right lung field, he was admitted to a near-by district hospital under the diagnosis of acute pneumonia. Since his respiratory condition rapidly deteriorated, he was transferred to our hospital. The diagnosis of unilateral cardiogenic pulmonary edema was made based upon the echocardiographic examination which showed severe mitral regurgitation secondary to chordal rupture of the posterior mitral valve leaflet (P2). After successful intensive medical treatment with diuretics and extracorporeal membrane oxygenation, mitral valve repair was performed with quadrangular resection of the posterior mitral leaflet (P2) and insertion of 28 mm Cosgrove ring.
It is important to recognize acute and severe mitral regurgitation as a main cause of unilateral cardiogenic pulmonary edema. Prompt differentiation from acute pneumonia is critical to save lives of the patients.
<Learning objective: Unilateral cardiogenic pulmonary edema is an unusual condition and may often be misdiagnosed as acute pneumonia, resulting in an increased risk of mortality. A correct differentiation from pneumonia is critical to save lives of the patients. It is important to recognize acute and severe mitral regurgitation as a main cause of this unusual condition.>
Keywords: Unilateral cardiogenic pulmonary edema, Acute mitral regurgitation, Differentiation from pneumonia
Introduction
Unilateral cardiogenic pulmonary edema is an unusual condition [1] and therefore may often be misdiagnosed initially as respiratory diseases such as pneumonia. Initiation of appropriate treatment may be delayed [2], resulting in an increased risk of mortality. Acute mitral regurgitation due to chordal rupture of the posterior mitral valve leaflet has been thought as a main cause of unilateral cardiogenic pulmonary edema [1]. Prompt differentiation from pneumonia is critical to save lives of the patients.
Case report
A 45-year-old man presented with fatigue and mild fever for two days. Because of severe hypoxemia and chest radiograph showing diffuse consolidation only in the right lung field, he was admitted to a near-by district hospital under the diagnosis of acute pneumonia (Fig. 1A). An electrocardiogram showed sinus tachycardia (130 beats/min) without any abnormal Q waves or ST-T changes. The blood test showed elevated white blood cells (16,730/μL), elevated C-reactive protein (17.5 mg/dL) but negative procalcitonin. He was intubated on the next day because of rapid deterioration in his condition with severe hypoxemia despite treatment with antibiotics and steroids. Since his respiratory condition further deteriorated, he was transferred to our hospital six days later. Upon arrival, he was in severe respiratory failure (pO2 55 mmHg, pCO2 50 mmHg, FiO2 1.0). Repeat physical examination revealed apical 3/6 pansystolic murmur. The blood test again showed insignificant procalcitonin level (0.24 ng/mL). Plasma levels of B-type natriuretic peptide (330 pg/mL) and A-type natriuretic peptide (192 pg/mL) were both elevated. Blood cultures were all negative and sputum cultures also revealed no pathologic organisms. Chest radiograph showed severe consolidation in the entire right lung field and left upper lung field (Fig. 1B). Transthoracic echocardiogram showed frail posterior mitral leaflet with severe mitral regurgitation secondary to chordal rupture of the posterior mitral valve leaflet (P2) (Fig. 2). The left atrium (LA) was mildly dilated (anteroposterior diameter 40 mm, LA volume 65 mL, LA volume index 34.8 mL/m2). Hyperdynamic left ventricular (LV) wall motion was noted (LV diastolic dimension 50 mm, systolic dimension 32 mm). Transesophageal echocardiogram again showed large frail posterior leaflet with chordal rupture of the posterior mitral valve leaflet (P2) (Fig. 3A). A large acceleration flow was seen within the LV around the mitral valve. From there a massive regurgitant flow went through frail P2 leaflet, first anterolaterally to the middle area of the LA and then was redirected toward the right side of the pulmonary veins (Fig. 3B), which was thought to be the cause of his unilateral cardiogenic pulmonary edema. Pulsed-wave Doppler examination showed systolic reverse flow, which may indicate the possibility of severe mitral regurgitation, not only in the right superior pulmonary vein but also in the left superior pulmonary vein as well at this point. However, a plain computed tomography scan taken at the time when he was admitted to the near-by district hospital showed engorged right superior (Fig. 3C) and right inferior pulmonary veins (Fig. 3D)without significant engorgement of the left pulmonary veins, indirectly indicating the mechanism of unilateral pulmonary edema. Moreover, engorged right superior and interior pulmonary veins were directly connected to probable perihilar pulmonary alveolar shadow. The patient was put on extracorporeal membrane oxygenation together with non-invasive positive pressure ventilation, although intra-aortic balloon pump was not used. The following surgery confirmed the diagnosis of chordal rupture of the posterior mitral valve leaflet (P2). The P2 leaflet was found to be unusually large with prolapsed width of 20 mm. There was also large tear of the P2 leaflet near the P3 leaflet down to the mitral ring. Mitral valve was repaired with quadrangular resection of the posterior leaflet and insertion of 28 mm Cosgrove ring. The resected specimen showed slight thinning in the mid portion of the P2 leaflet due to mild myxomatous changes. Post-operative course was uneventful and the patient remained asymptomatic one year after surgery.
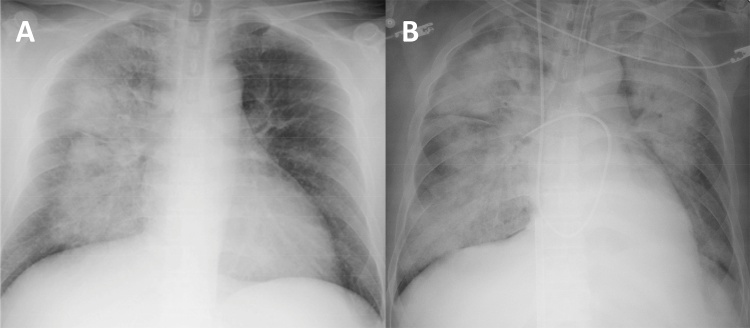
Fig. 1.
(A) Chest radiograph on admission at the district hospital showing unilateral consolidation of the right lung field. (B) Chest radiograph at transfer six days later showing bilateral severe consolidation resembling “butterfly shadow”.
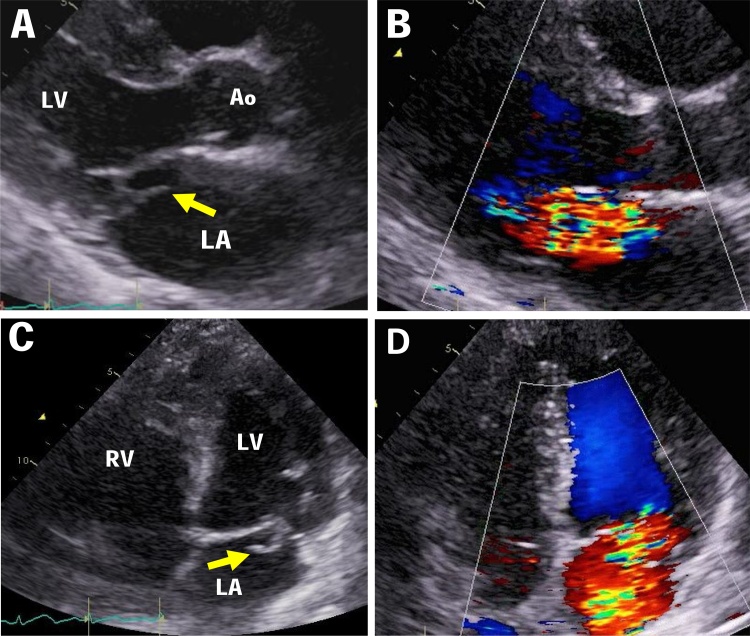
Fig. 2.
Transthoracic echocardiograms in the long-axis view (upper panel) and apical four-chamber view (lower panel). Chordal rupture of the posterior mitral valve P2 leaflet is shown (A,C: arrow). Severe mitral regurgitation was first directed anterolaterally and then to the right side of the LA (B,D).
Ao, aorta; LA, left atrium; LV, left ventricle; RV, right ventricle.
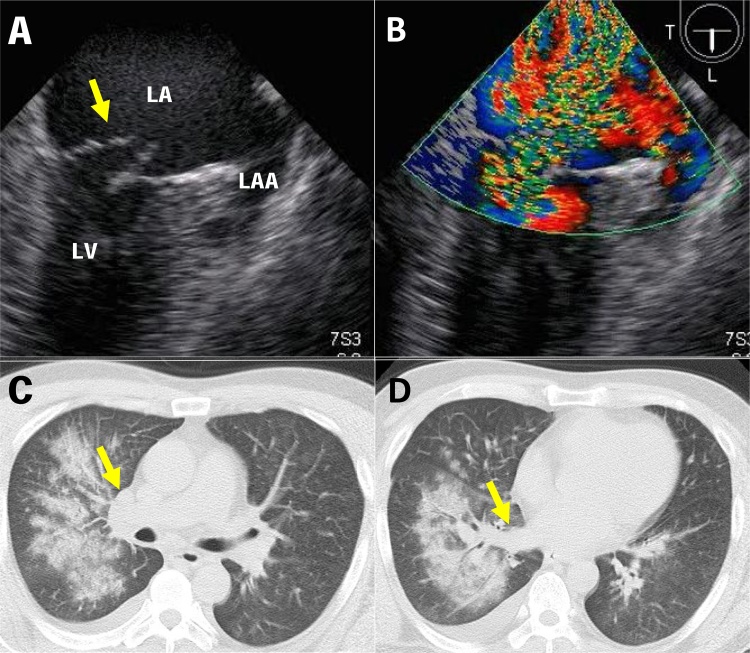
Fig. 3.
Upper panel: Transesophageal echocardiograms showing chordal rupture of the posterior mitral valve leaflet (A, arrow) and massive mitral regurgitant flow toward the right side of the pulmonary veins (B). Lower panel: Plain computed tomography scan on admission at the district hospital showing prominent right superior pulmonary vein (C, arrow) and engorged right inferior pulmonary vein (D, arrow) without significant engorgement of the left pulmonary veins. Engorged right pulmonary veins were directly connected to the perihilar consolidation.
LA; left atrium, LLA; left atrial appendage, LV; left ventricle.
Discussion
In order to differentiate unilateral cardiogenic pulmonary edema from acute pneumonia, it is helpful to obtain information such as sudden onset of symptoms, perihilar unilateral “bat wing” consolidation in the right lung field, and significantly elevated plasma level of B-type natriuretic peptide in the absence of positive procalcitonin level (Table 1). Physical examination attempting to detect a murmur is most important but it may at times be misleading since the systolic murmur of acute mitral regurgitation may be soft, early in systole, and even be absent because of rapid equilibration of LA and LV pressures. At the same time it is also problematic in a patient presenting with respiratory distress. The key examination is therefore bedside echocardiography which will guide us to a correct diagnosis of unilateral cardiogenic pulmonary edema. The early initiation of appropriate treatment may then reduce the risk of mortality of the patients.
Table 1.
Different presentations between unilateral cardiogenic pulmonary edema and pneumonia.
| Unilateral cardiogenic pulmonary edema | Pneumonia | ||
|---|---|---|---|
| Symptom | Sudden onset/mostly afebrile | Gradual onset/febrile | |
| Physical examination | Early systolic ∼pansystolic murmur | No murmur | |
| Chest X-ray | Unilateral “bat wing” consolidation with peripheral field spared, mostly in the right lung | Diffuse, lobar, or multifocal consolidation | |
| Gram staining (sputa) | Negative | Often positive | |
| Biomarkers | PCT | Negative | Positive |
| BNP | Elevated | WNL | |
| ANP | Elevated | WNL | |
| Echocardiography | Acute and severe mitral regurgitation | – | |
| Chordal rupture |
ANP, atrial natriuretic peptide; BNP, B-type natriuretic peptide; PCT, procalcitonin; WNL, within normal limits.
This cardiogenic unilateral pulmonary edema should also be differentiated from noncardiogenic unilateral permeability pulmonary edema which may be caused by lesions ipsilateral to the edema such as aspiration, reexpansion, contusion, pulmonary vein occlusion, and prolonged decubitus positioning, and by lesions contralateral to the edema such as pulmonary embolism, lobectomy, and denervation [3].
Unilateral pulmonary edema has been reported to represent 2.1% of cardiogenic pulmonary edema [1]. Several mechanisms of unilateral pulmonary edema caused by acute and severe mitral regurgitation have been suggested. The regurgitant flow may be directed toward the right pulmonary veins, frequently the superior right pulmonary vein, in the patients with severe mitral regurgitation from the posterior leaflet [4], [5]. Anatomic position of pulmonary veins in the left atrium and anatomic drainage of pulmonary veins may also contribute to the development of this unusual condition [6]. However, the cause of severe mitral regurgitation has not well been discussed. As shown in this case and also in other reports [1], [5], the main cause of severe mitral regurgitation in unilateral pulmonary edema seems to be acute chordal rupture rather than chronic mitral valve prolapse, although acute mitral regurgitation due to chordal rupture may often occur in the presence of chronic conditions such as mitral valve prolapse. Thus, it is important to perform bedside echocardiography with the understanding of the concept that unilateral cardiogenic pulmonary edema is mainly caused by acute mitral regurgitation most often due to chordal rupture of the posterior mitral valve leaflet. This is critical to save lives of the patients who carry increased risk of mortality.
Conflict of interest
All authors have no conflict of interest.
Acknowledgment
We thank Dr Hiroyuki Irie for his participation with excellent surgery in the treatment of the patient.
Contributor Information
Satoshi Inotani, Email: jm-s-inotani@kochi-u.ac.jp.
Yoshinori Doi, Email: ydoi@chikamori.com.
References
- 1.Attias D., Mansencal N., Auvert B., Vieillard-Baron A., Delos A., Lacombe P. Prevalence, characteristics, and outcomes of patients presenting with cardiogenic unilateral pulmonary edema. Circulation. 2010;122:1109–1115. doi: 10.1161/CIRCULATIONAHA.109.934950. [DOI] [PubMed] [Google Scholar]
- 2.Choi H.S., Choi H., Han S., Kim H.S., Lee C., Kim Y.Y. Pulmonary edema during pregnancy: unilateral presentation is not rare. Circ J. 2002;66:623–626. doi: 10.1253/circj.66.623. [DOI] [PubMed] [Google Scholar]
- 3.Calenoff L., Kruglik G.D., Woodruff A. Unilateral pulmonary edema. Radiology. 1978;126:19–24. doi: 10.1148/126.1.19. [DOI] [PubMed] [Google Scholar]
- 4.Miyatake K., Nimura Y., Sakakibara H., Kinoshita N., Okamoto M., Nagata S. Localisation and direction of mitral regurgitation flow in mitral orifice studied with combined use of ultrasonic pulsed Doppler technique and two dimensional echocardiography. Br Heart J. 1982;48:449–458. doi: 10.1136/hrt.48.5.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raman S., Pipavath S. Asymmetric edema of the upper lung due to mitral valvular dysfunction. N Engl J Med. 2009;361:e6. doi: 10.1056/NEJMicm0801147. [DOI] [PubMed] [Google Scholar]
- 6.Marom E.M., Herndon J.E., Kim Y.H., McAdams H.P. Variations in pulmonary venous drainage to the left atrium: implications for radiofrequency ablation. Radiology. 2004;230:824–829. doi: 10.1148/radiol.2303030315. [DOI] [PubMed] [Google Scholar]