Abstract
Brugada syndrome is typically an autosomal dominant genetic disorder with variable expression, characterized by three specific electrocardiogram (ECG) patterns. While Type I Brugada ECG pattern is used as a classic marker for the disease, it is generally masked from ECG except in special cases such as malaria-induced fever. This vignette highlights a unique clinical scenario that can lead to the unmasking of Brugada type 1 pattern.
<Learning objective: Brugada syndrome is associated with ventricular arrhythmias which if left untreated can result in syncope or premature death. Early intervention involving lifestyle modifications and recommendation of implantable defibrillator is based on diagnosis. Yet, Brugada syndrome is hard to detect from an electrocardiogram (ECG) alone. Still there are certain circumstances that unmask the Brugada syndrome ECG pattern. This case report provides one clinical scenario leading to the incidental unmasking of Brugada syndrome.>
Keywords: Brugada syndrome, Genetics, Cardiac disease
Introduction
Brugada syndrome is typically an autosomal genetic disorder that is often transmitted in an autosomal dominant pattern. While there are varying degrees of phenotypic expression of the condition, the hallmark is ST–T segment elevation in the precordial electrocardiogram (ECG) leads. It carries an increased risk of ventricular tachyarrhythmia and sudden cardiac death. Type I Brugada ECG pattern is used as a classic marker for the disease and is characterized by a pseudo-right bundle branch block and persistent ST–T segment elevation in leads V1 to V3 [1]. Mutations most commonly in the genes coding for sodium or potassium voltage channels result in reduced duration of normal action potentials, and predisposition to local re-entry and ventricular arrhythmias [2]. Fever is a trigger for ECG changes and cardiac arrest in these patients [3]. While asymptomatic Brugada patients have a low risk of adverse cardiac events, patients with aborted sudden cardiac death and unexplained syncope have the highest risk of sudden death [4].
Case report
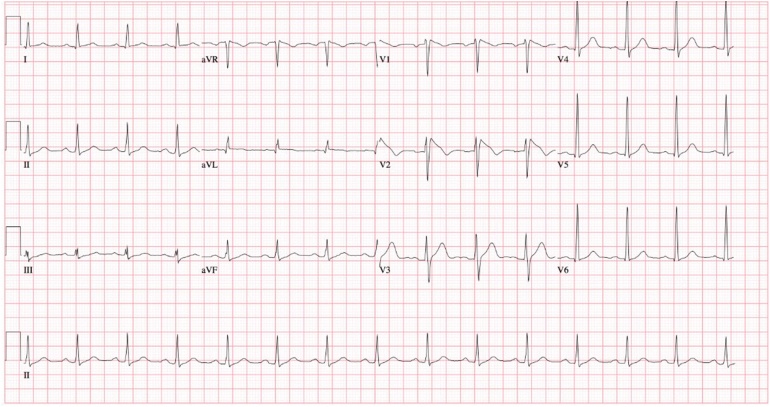
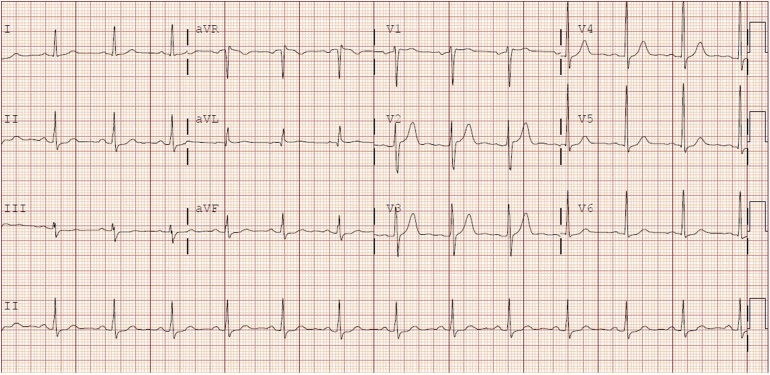
A 52-year-old previously healthy South Asian male presented to the emergency room with recurrent fevers up to 40 °C after travel to South Asia. He was diagnosed with Plasmodium vivax malaria and was incidentally found to have type I Brugada pattern (Fig. 1) on his 12-lead ECG. Electrolytes were normal at the time of admission and during the course of the hospitalization. After administration of chloroquine and antipyretic treatments, he defervesced and a normal ECG pattern was observed as indicated by his 12-lead ECG (Fig. 2). To confirm the diagnosis, procainamide testing was performed which revealed type I Brugada pattern. Additionally, genetic testing demonstrated a D1370G mutation in the SCN5A sodium channel gene. The patient had no prior history of ventricular arrhythmias or syncope and no family history of sudden cardiac death. Given that the risk of sudden death in asymptomatic Brugada pattern patients is exceptionally low, defibrillator implantation was not recommended. Instead lifestyle modifications were advised including avoiding and promptly treating fevers, and consulting with a pharmacist prior to using new medications.
Fig. 1.
Type 1 Brugada pattern on 12-lead electrocardiogram.
Fig. 2.
Normal ECG pattern on 12-lead electrocardiogram.
Discussion
This case is a good example of how the diagnosis of Brugada syndrome would have been missed if the patient were perfectly healthy. In this report, the occurrence of fever was necessary for the unmasking of type 1 Brugada pattern on an ECG, which can often remain concealed. In conclusion, this vignette highlights one of the many possible unique clinical scenarios that can lead to the unmasking of Brugada pattern.
Conflict of interest
The authors declare there are no conflicts of interest.
References
- 1.Alings M., Wilde A. “Brugada” syndrome: clinical data and suggested pathophysiological mechanism. Circulation. 1999;99:666–673. doi: 10.1161/01.cir.99.5.666. [DOI] [PubMed] [Google Scholar]
- 2.Zhang J., Sacher F., Hoffmayer K., O'Hara T., Strom M., Cuculich P. Cardiac electrophysiological substrate underlying the ECG phenotype and electrogram abnormalities in Brugada syndrome patients. Circulation. 2015;131:1950–1959. doi: 10.1161/CIRCULATIONAHA.114.013698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amin A.S., Meregalli P.G., Bardai A., Wilde A.A., Tan H.L. Fever increases the risk for cardiac arrest in the Brugada syndrome. Ann Intern Med. 2008;149:216–218. doi: 10.7326/0003-4819-149-3-200808050-00020. [DOI] [PubMed] [Google Scholar]
- 4.Probst V., Veltman C., Eckardt L., Meregalli P.G., Gaita F., Tan H.L. Long-term prognosis of patients diagnosed with Brugada syndrome: results from the FINGER Brugada syndrome registry. Circulation. 2010;121:635–643. doi: 10.1161/CIRCULATIONAHA.109.887026. [DOI] [PubMed] [Google Scholar]