ABSTRACT
Vaccines are an established means of preventing and eliminating communicable diseases. Whilst their efficacy in some settings is well studied, the impact of multi-dose vaccinations programmes in elderly populations is not well documented. A literature review was conducted in order to collate and analyse existing publications to provide a summary of current thinking and support identification of key factors that impact on the success of vaccination programmes. Having returned little information to provide a comprehensive understanding of the subject area, two short surveys were undertaken to supplement the findings and further examine the attitudes and opinions of the elderly and healthcare professionals. Combining the results from all three research methodologies suggests that vaccination programmes with fewer doses are associated with improved course completion rates and a lower logistical and economic burden. Whilst it is acknowledged that this study has limitations, it provides relevant insights in a space where there is little research to inform the work programmes of vaccines in development and support optimisation of ongoing programmes. It also highlights the need for further research to fully understand the factors influencing successful vaccination programmes in this specific patient population.
KEYWORDS: adherence, dosing schedules, elderly, Vaccine, vaccination programme
Introduction
It is generally accepted that multi-dose vaccination programmes are an effective means of immunising infants and children. This is supported by a wealth of clinical papers that describe the benefits of these programmes and detail their successes in preventing and in some cases eliminating communicable diseases. Although eradication may be the ultimate goal of a vaccination programme, to achieve this requires high coverage rates amongst the target populations in order to develop immunity and reduce infection / mortality rates. In the developed world, participation in childhood vaccination programmes is largely the norm and, with some exceptions, there are good rates of coverage that are contributing to the elimination of diseases such as measles, mumps, rubella and polio.1-3
Overall, the prevalence of illness attributable to vaccine-preventable diseases is greater in adults than children but vaccination coverage rates in this population are considerably lower, particularly amongst the elderly.4 Despite having similar, robust guidelines and recommendations for vaccinations in at-risk groups, most European countries fail to meet the 75% coverage target set by the WHO for single-dose influenza vaccinations in over 65s.5 In the UK only 72.6% of over 65s received flu vaccinations in the six months from September 2017 to January 2018. Vaccination rates are even lower in other national programmes targeting the elderly; 69.8% for over 65′s in the pneumococcal polysaccharide vaccine and only 48.3% for over 70′s in the shingles vaccine.6,7,8 These figures are for single dose vaccinations yet evidence reviewed in this report suggests that rates are even lower for multi-dose vaccination programmes.9-11
Whilst vaccination may seem like an obvious and necessary measure to promote public health, there are many and varied reasons why programmes fail to meet their coverage targets and why some people do not want to be vaccinated. These reasons and their impact have been explored in detail for some single-dose programmes delivered in elderly populations.12 However; there is little published information when it comes to multi-dose vaccinations in this group. In developing successful vaccination programmes for the elderly and implementing strategies to improve coverage, it is important to understand the impact of dosing schedules on both this population and the associated healthcare resources. This short report aims to contribute to current understanding by investigating the impact of multi-dose formulations on three key aspects of vaccination programmes: logistics and economics (including course completion) and humanistic (patient quality of life) outcomes. It collates the results of three pieces of research including a review of published literature, quantitative / qualitative research with individuals aged 65–89 and a group of primary healthcare professionals.
Results
Of 252 studies identified, only three met the defined inclusion criteria for the literature review: two relevant to course completion and one related to cost and resource use. No studies were returned that provided any insight into how multi-dose programmes impact on the quality of life of participants (Table 1). This shows that the literature review had returned little relevant information on the logistical, economic and humanistic impact of multi-dose vaccination programmes in the elderly. Thereby confirming suspicions that there are few resources to which practitioners can refer for guidance on optimising vaccination programmes for this population.
Table 1.
Papers included in the literature review.
| Sourced from | Author | Title | Reference | Published date | Location | Study date |
|---|---|---|---|---|---|---|
| EMBASE | Nelson et al. | Compliance With Multiple-Dose Vaccine Schedules Among Older Children, Adolescents, and Adults: Results From a Vaccine Safety Datalink Study | Supplement 2, 2009, Vol 99, No. S2 | American Journal of Public Health | 2009 | USA | 1996–2004 |
| Backwards from Nelson | Macdonald et al. | Predictors of completion of a hepatitis B vaccination schedule in attendees at a primary health care centre | Sexual Health, 2007, 4, 27–30 | 2007 | Australia | 1992–2003 |
| Forwards from Nelson | Kuan et al. | Cost-effectiveness of hepatitis B vaccination using HEPLISAVTMin selected adult populations compared to Engerix-B®vaccine | Vaccine 31 (2013) 4024– 4032 | 2013 | USA | 2011 |
Overall the report highlight that completion of multi-dose vaccination programmes is particularly poor in the elderly age group.9-11 Course completion is influenced by a wide range of factors associated with programme design and an individual's ability and willingness to adhere to the programme but in most cases vaccination programmes with fewer doses result in greater completion rates.9-11
MacDonald et al concurred that factors found to have a statistically significant impact on improving adherence in a hepatitis B vaccination programme were not sufficient to overcome the challenges associated with administering three doses.10 However, this was not always the case and in an extensive US study of adherence with different vaccine dosing programmes across multiple age groups, Nelson et al found that full adherence with a three-dose hepatitis B vaccine programme was better than that of a two-dose hepatitis A programme (43.6% vs. 61.1%).11 In this instance, adherence was found to be greater in the over-50 age group but course completion was still low across both vaccination groups.11 In the multi-variate analyses of the study, the authors demonstrated that a number of factors associated with increases in adherence were statistically significant and that these factors had a stronger effect on the relative risk of completing the vaccination programme for the three-dose hepatitis B vaccine than the two-dose hepatitis A programme.11 Gender (female); older age; longer duration of enrolment in a managed care organisation; a higher number of medical visits prior to first dose; and not being a recipient of Medicaid were all predictors of increased adherence.11
The Healthcare Professional (HCP) survey revealed strong opinions, with 84% of respondents agreeing that course completion would reduce with a multi-dose vaccination programme. Groups within the elderly population who often struggle to access vaccinations and who would be at greater risk of poor outcomes with multi-dose rather than single dose schedules were identified as: housebound and nursing home residents; the frail, infirm and less mobile; people with learning disabilities, mental health, dementia or cognitive issues; people from ethnic or cultural minorities or with language barriers and those with transportation difficulties.
One factor that appeared to improve completion of multi-dose programmes was an accelerated dosing schedule.10 In MacDonald's study of a hepatitis B vaccination programme an accelerated dosing schedule (0, 7 and 21 days and a booster at 12 months) led to increased adherence over a traditional dosing schedule (0, 1 and 6 months).10 A shorter period between the first appointment and the start of the vaccination programme and the intention to deliver an accelerated dosing programme were both statistically significant predictors of course completion.10 As observed with other studies, course completion rates were still low for both programmes.10
With limited data available from the literature review on the impact of multi-dose programmes on the elderly, the elderly population survey provided a useful indicator of participants' views and the factors influencing their willingness and ability to complete the scheduled course. The results showed a high level of GP surgery attendance, with 89% of individuals having visited in the last year. While few respondents (10%) reported difficulties accessing their surgery, for those who did cite challenges, lack of available appointments was the most common reason (60%). Respondents indicated a good level of attendance at vaccination appointments with 83% having received a vaccination within the last two years; including travel, flu and other preventative vaccinations. Approximately 93% of those interviewed had never had to rearrange or cancel a vaccination appointment and, of those that did cancel appointments, 80% rearranged, suggesting a strong willingness to attend.
Perhaps unsurprisingly, there was strong support for vaccines to be delivered in as few doses and appointments as necessary, with 84% indicating a preference for single doses and 79% a preference for receiving multiple vaccinations in one visit rather than over several appointments. However, in contrast to the views of HCPs and at odds with the course completion rates seen in the literature review, 68% of respondents stated that they would be unconcerned if vaccinations had to be delivered over multiple appointments. When respondents were stratified by age, 70% of 65–69 year olds were unconcerned about multiple appointments, falling to 61% in those aged 80–89 years, indicating that course completion for multi-dose programmes may be more challenging with increasing age. Of greater concern to this particular population were adverse events; 63% stated that they would not be willing to return for a subsequent dose if they had suffered an adverse effect to the first dose of a vaccination.
With regard to the economics of vaccination programmes, the literature review found that vaccination programmes with fewer doses were associated with greater cost effectiveness.9 As described earlier, fewer doses result in greater course completion rates and good adherence was a significant factor in driving cost effectiveness9
Kuan et al carried out a cost effectiveness analysis of a two doses versus a 3 dose vaccine for the prevention of hepatitis B in US healthcare workers, international travellers and patients with diabetes, chronic pain or end stage renal disease.9 Outcomes of interest were the total quality adjusted life years (QALYs) and total costs associated with the two approaches across the different patient subgroups. The analysis determined that the vaccine requiring fewer doses was cost-effective; with adherence, vaccine cost and duration of protection all influencing total cost effectiveness.9
HCPs were clear that multi-dose vaccination programmes would lead to extra cost and resource burdens on medical practices already strained under a substantial workload. Approximately 83% of nurses and 60% of GPs were certain that any additional costs incurred would not be met by existing reimbursement schemes. And, whilst 87% of immunisation leads (responsible for co-ordinating vaccination services provided by the NHS within a specific region) and 50% of practice managers were confident that funding would be sufficient, they agreed that cost would become a greater issue if payment on completion or reduced payments for multi-dose schemes were introduced; and practices may deprioritise these vaccinations versus other paid-for nursing services.
Although few of the studies analysed the logistical impact of multi-dose vaccination programmes, the views expressed in the HCP and elderly population surveys suggest that multi-dose programmes are associated with a greater logistical burden. Having a negative impact on resources and being a driver of increased costs, this factor significantly affects healthcare providers' ability to deliver vaccination programmes as well as impacting on the willingness and ability of an individual to attend.
The vast majority of respondents to the elderly population survey (84%) indicated a preference for single dose vaccines. Although a reasonably high percentage also suggested that they would be unconcerned if required to attend multiple appointments (64%), in practice factors such as illness, needing accompaniment, travel difficulties and the inability to get an appointment, may become more significant for multiple appointments, contributing to poor course completion rates as seen in the literature review. HCPs were in agreement with this last statement, believing that the ability of the elderly population to access the surgery is one of the most significant factors in a delivering a successful vaccination programme. They anticipated that multiple doses would amplify the challenges anticipated in a single-dose programme, particularly amongst the groups already identified as having difficulty accessing vaccinations. In addition, communication challenges in explaining the need for a multi-dose schedule and ensuring patients attend subsequent appointments would present further challenges.
In terms of the logistical impact on medical practices, an increased burden on nursing resources and costs were a concern to nearly all HCPs (Fig. 1). They also anticipated additional workload for administration staff in scheduling extra appointments and following up individuals who do not attend; 73% felt that practices would struggle to schedule extra appointments needed for a multi-dose programme. Additionally, whilst some single-dose vaccinations can be conveniently scheduled to take place in the same appointment and reduce administrative burden e.g. flu and pneumococcal injections, multi-dose formulations would not benefit from similar efficiencies. A further concern cited by HCP respondents was vaccine wastage as a result of both unpredictable numbers returning to complete the full course of vaccinations, and cold chain problems due to ordering and fridge capacity issues.
Figure 1.
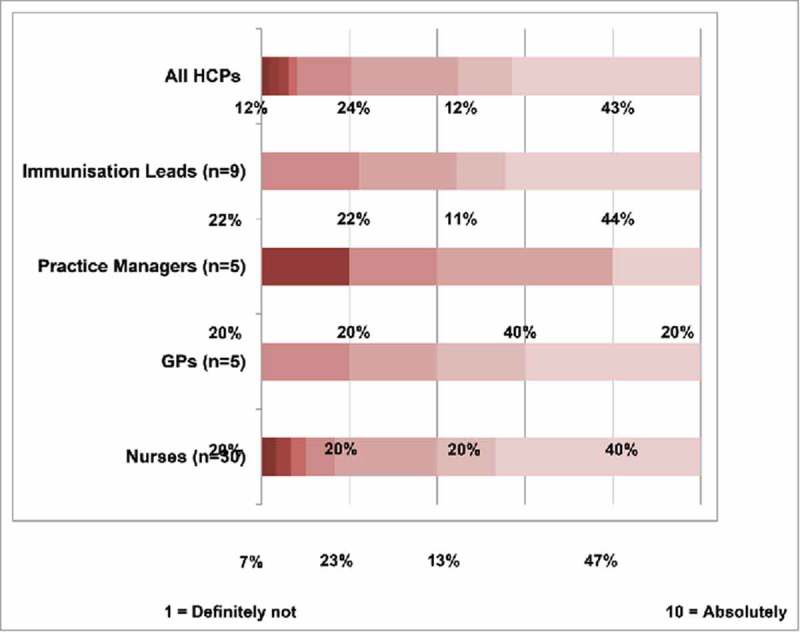
Likelihood that an increased number of doses would place additional burden on the surgery.
Conclusions
The results of the studies compiled in this report indicate that vaccination programmes with fewer doses are typically associated with better rates of course completion and a lower economic and logistical burden on healthcare providers and practitioners.9-12 They also highlight that coverage rates for multi-dose vaccination programmes in the elderly are lower compared to multi-dose vaccinations in young age groups and single-dose vaccinations within the same group.9-11
Whilst a low number of doses is significant in achieving good levels of course completion, other factors such as population demographics and engagement with healthcare systems also appear to play a role.10,11 The severity of the disease being vaccinated against and the consequences of subsequent illness may also impact on willingness to take part in multi-dose programmes, as seen in Nelson's comparison of a three-dose hepatitis B versus a two-dose hepatitis A programme.11 However, further research is needed to confirm the significance of this factor. Accelerated dosing regimens do appear to offer advantages over traditional regimens in terms of course completion and may have a role to play where multi-dose formulations are required in order to achieve sufficient immune response.10
Good adherence is a significant factor in maximising the cost-effectiveness of vaccination programmes, and improved adherence/course completion rates are associated with regimens with fewer doses.9 This confirms the importance of including strategies to support adherence within programme design and the value further research would add to current understanding of the factors influencing vaccine adherence within elderly populations. Further study may also help to clarify why the elderly population in this research cite a preference for single dose vaccination schedules while also indicating that attending multiple vaccination appointments would not be a significant concern. Course completion rates found in the literature review demonstrate that this indifference to multiple vaccination appointments does not translate into practice with a much lower uptake observed for each subsequent dose in multi-dose vaccination programmes.9-11 Tolerability may be a factor here, representing a particular adherence challenge for multi-dose programmes if issues with the first dose prevent subsequent attendances. However, the impact of adverse events on course completion was not covered in the literature review or HCP survey so it is not possible to comment further on the extent to which this may account for the discrepancy between intention to attend and actual attendance.
Multi-dose vaccination programmes were found to increase costs and resourcing concerns for medical practices.9 With many UK practices already under pressure, there is a danger that complex and resource-intensive, multi-dose programmes may be deprioritised if HCPs feel that reimbursement does not cover the additional resources and running costs required to implement them.
These findings indicate that the success of a vaccination programme relies on a number of interdependent factors and cannot be estimated solely on the clinical efficacy of the vaccination itself. Multi-dose vaccinations are found to impact negatively on cost, logistics and completion of vaccination courses and as such would need to demonstrate high levels of clinical efficacy or address a specific unmet need in order to justify the additional burden on medical practices and target populations.
Limitations of this research are due to the paucity of data returned in the literature review as well as the low numbers and restricted questions in the surveys. It is acknowledged that the results of the elderly population survey may be impacted by the participants physical and cognitive ability to complete the survey and that barriers to course completion may vary between countries and their health systems. However, the report does provide a valuable summary of the currently available data on key factors influencing the success of multi-dose vaccination programmes in the elderly. It offers relevant insights that merit consideration in the development of current and future vaccination programmes, having shown that single-dose regimens are more acceptable for both patients and healthcare systems and that there are opportunities for optimising course completion when multi-dose regimens must be implemented.
The report's findings also bear relevance to current practise where implementing strategies such as accelerated dosing regimens or improving communications with patients may be useful in improving the efficacy of existing multi-dose vaccination programmes, such as those for hepatitis A. This report also aims to prompt wider research amongst larger elderly populations across a variety of vaccination programmes as well as research in other countries. Of particular concern is the absence of data on the quality of life impact of different vaccination schedules. Further understanding in this area would support optimisation of vaccination programmes to ensure course completion.
Methods
This report compiles the results of three pieces of research including a review of the published literature along with quantitative / qualitative research with individuals aged 65–89 and a group of primary healthcare professionals.
The literature review applied robust and established methods to identify and evaluate papers relevant to two research questions defined using PICOS (Participant, Intervention, Comparison, Outcome Study) criteria: what are the logistical and economic implications of multi-dose vaccination schedules (including impact on vaccine course completion) and what are the humanistic outcomes associated with multi-dose vaccination schedules? Studies of interest were identified by simultaneously searching the Embase, Medline and Medline (R) In-Process electronic databases, within the date range 1966 – 2015, using a defined set of research terms and eligibility criteria. A grey literature search, using google, and a further search of the bibliographies of review papers were also performed to include any other studies that may not have been identified in the search strategy (Fig. 2). Duplicates were removed for all records obtained in the searches and a manual review of the titles and abstracts conducted using the defined inclusion/exclusion criteria to determine papers to include at this stage (known as the first pass). The first pass was performed by one independent reviewer with uncertainties between included papers resolved by a second independent reviewer. Full-text papers identified at the first pass were then evaluated and included for review based on the inclusion/exclusion criteria (also known as the second pass). Data were extracted from eligible publications into a pre-defined spreadsheet following strategies similar to the PRISMA / CONSORT guidelines.13,14 An update of the literature review was conducted within the date range 2016–17 but returned no relevant new publications.
Figure 2.
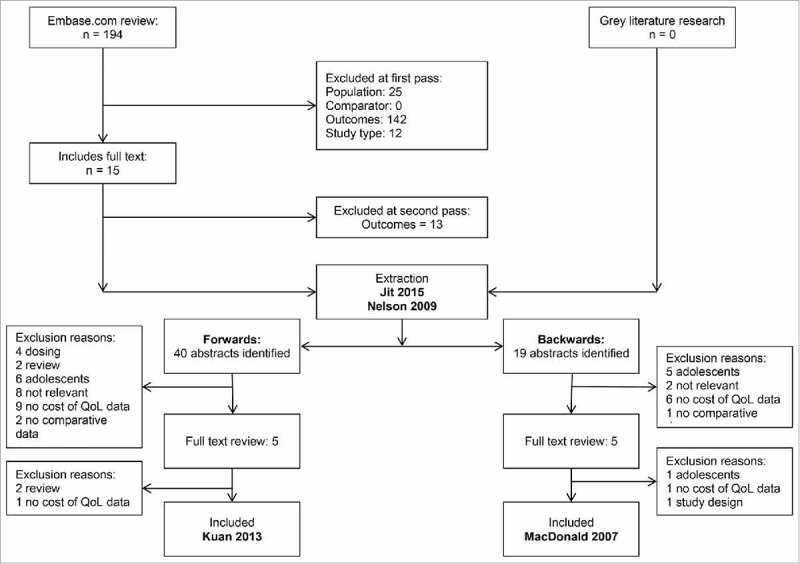
Summarised search methodology for targeted literature review.
Due to the limited number of publications meeting the criteria for the literature review, a further two surveys were conducted to provide fuller understanding of the cost, logistical and quality of life impacts of multi-dose vaccines within elderly populations. The HCP survey, involved comprehensive telephone interviews with 30 nurses, five GPs, five practice managers, and nine immunisation leads from across Great Britain. The second survey, amongst a group of 1,000 UK residents aged 65–89, examined the incidence and nature of problems faced by the elderly when accessing their GP surgery, attending vaccination appointments and their preferences for receiving vaccinations in single or multiple appointments (Fig. 3). Fourteen survey questions were asked during seven-minute telephone interviews conducted in October 2016 w`ith participants randomly selected from across the UK, with quotas set by age, gender, socioeconomic status and region in order to reflect a nationally representative sample of adults.
Figure 3.
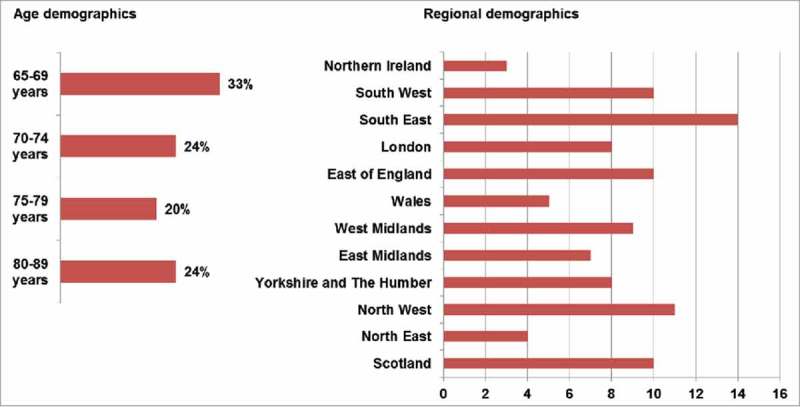
Demographics of the elderly population survey.
Funding Statement
This work was supported by the Merck Sharp and Dohme.
Disclosure of potential conflicts of interest
Ian Matthews and Hazel Dawson are employees of Merck Sharp & Dohme Limited.
References
- 1.Andre FE, Booy R, Bock HL, Clemens J, Datta SK, John TJ, Lee BW, Lolekha S, Peltola H, Ruff TA, et al.. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. 2008;86(2):140–6. doi: 10.2471/BLT.07.040089. PMID:18297169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muller CP, Kremer JR, Best JM, Dourado I, Triki H, Reef S. WHO Steering Committee for Measles and Rubella. Reducing global disease burden of measles and rubella: report of the WHO Steering Committee on research related to measles and rubella vaccines and vaccination, 2005. Vaccine. 2007;25(1):1–9. doi: 10.1016/j.vaccine.2006.07.039. PMID:17262908. [DOI] [PubMed] [Google Scholar]
- 3.Peltola H, Davidkin I, Paunio M, Valle M, Leinikki P, Heinonen OP. Mumps and rubella eliminated from Finland. JAMA. 2000;284(20):2643–7. doi: 10.1001/jama.284.20.2643. PMID:11086376. [DOI] [PubMed] [Google Scholar]
- 4.Williams WW, Lu P, O'Halloran A, Kim DK, Grohskopf LA, Pilishvili T, Skoff TH, Nelson NP, Harpaz R, Markowitz LE, et al.. Surveillance of vaccination coverage among adult populations — United States, 2014. MMWR Surveill Summ. 2016;65(1):1–36. doi: 10.15585/mmwr.ss6501a1. PMID:26844596. [DOI] [PubMed] [Google Scholar]
- 5.Palachea A, Oriol-Mathieub V, Finoc M, Xydia-Charmantad M. Seasonal influenza vaccine dose distribution in 195 countries (2004–2013): Little progress in estimated global vaccination coverage. Vaccine. 2015;33:5598–5605. doi: 10.1016/j.vaccine.2015.08.082. PMID:26368399. [DOI] [PubMed]
- 6.Public Health England Seasonal influenza vaccine uptake amongst GP patients in England. Provisional monthly data for 1 September 2017 to 31 January 2018 by NHS England Local Team. [Accessed 2018 March 27]. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/684553/Seasonal_flu_vaccine_uptake_GP_patients_2017_2018_01_September_31_January_Local_Team.pdf.
- 7.Public Health England Pneumococcal Polysaccharide Vaccine (PPV) coverage report, England, April 2016 to March 2017. Health Protection Report Volume 11 Number 23 [Accessed 2018 March 27]. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/624133/hpr2317_PPV.pdf.
- 8.Public Health England Herpes zoster (shingles) immunisation programme: September 2016 to August 2017. Report for England. [Accessed 2018 March 27]. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/667636/Annual_shingles_report_2016-2017_.pdf.
- 9.Kuan RK, Janssen R, Heyward W, Bennett S, Nordyke R. Cost-effectiveness of hepatitis B vaccination using HEPLISAV™ in selected adult populations compared to Engerix-B® vaccine. Vaccine. 2013;31(37):4024–32. doi: 10.1016/j.vaccine.2013.05.014. PMID: 23707166. [DOI] [PubMed] [Google Scholar]
- 10.Macdonald V, Dore GJ, Amin J, van Beek I. Predictors of completion of a hepatitis B vaccination schedule in attendees at a primary health care centre. Sex Health. 2007;4(1):27–30. doi: 10.1071/SH06008. PMID:17382034. [DOI] [PubMed] [Google Scholar]
- 11.Nelson JC, Bittner RC, Bounds L, Zhao S, Baggs J, Donahue JG, Hambidge SJ, Jacobsen SJ, Klein NP, Naleway AL, et al.. Adherence with multiple-dose vaccine schedules among older children, adolescents, and adults: results from a vaccine safety datalink study. Am J Public Health. 2009;99(Suppl.2):S389–97. doi: 10.2105/AJPH.2008.151332. PMID:19797753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kohlhammer Y, Schnoor M, Schwatz M, Raspe H, Schäfer T. Determinants of influenza and pneumococcal vaccination in elderly people: a systematic review. Public Health. 2007;121(10):742–51. doi: 10.1016/j.puhe.2007.02.011. PMID:17572457. [DOI] [PubMed] [Google Scholar]
- 13.CONSORT Group The CONSORT statement. [Accessed 2017December11]. http://www.consort-statement.org/.
- 14.PRISMA. PRISMA Checklist [Accessed 2017December11]. http://prisma-statement.org/PRISMAStatement/Checklist.aspx.


