Abstract
Objectives
The aim of this study was to compare clinical and radiological results of proximal crescentic osteotomy (PCO) and rotational scarf osteotomy performed in the treatment of hallux valgus.
Methods
A total of 57 consecutive patients (60 feet) with symptomatic hallux valgus deformity were randomly assigned to one of two groups. The PCO group consisted of 22 women and 5 men (30 feet) and the mean age was 43(±14.5) years. The scarf group consisted of 23 women and 7 men (30 feet) and the mean age was 40.9(±12.6) years. Outcomes were assessed by using of preoperative and postoperative American Orthopaedic Foot and Ankle Society (AOFAS) scores and visual analogue scale (VAS). Weight bearing X-rays were used for radiological evaluation.
Results
The mean AOFAS scores improved from 42(±16.2) to 66.7(±13.4) points in PCO group and from 36.2(±16.1) to 73.2(±13.5) points in scarf group. The mean pain score improved from 6.3(±1.3) to 2.4(±2) in PCO group and from 6.5(±1.9) to 2.5(±1.3) in scarf group. The mean hallux valgus angle (HVA) decreased from 38.1°(±7.1) preoperatively to 23.8°(±8.5) at postoperative first year in PCO group, and from 36.1°(±7.5) preoperatively to 22.2°(±7.5) at postoperative first year in scarf group. The mean intermetatarsal angle (IMA) decreased from 17.3°(±3.8) preoperatively to 11.8°(±3.3) at postoperative first year in PCO group, and from 16.2°(±2.6) preoperatively to 9.3°(±2.4) at postoperative first year in scarf group.
When all the patients were assessed together, the relations between preoperative DMAA values and postoperative first year HVA (r = 0,327) and IMA (r = 0,399) values were positive but had low significance. The HVA and IMA values were increased in both groups at the end of the first year when compared to the postoperative sixth week values (p < 0.01 for both groups for both values).
Conclusion
The PCO and the rotational scarf osteotomy in the treatment of hallux valgus deformity provides a satisfactory correction. The clinical and radiological results of both methods are similar. Especially in patients with high preoperative DMAA, an increase in the HVA and the IMA values may occur in the first postoperative year when compared to the postoperative sixth week values.
Level of evidence
Level II, therapeutic study.
Keywords: Hallux valgus, Scarf osteotomy, Proximal crescentic osteotomy, Surgical treatment, Foot
Introduction
Hallux valgus is a common pathology in the society, which impair quality of life.1, 2 Surgical treatment is usually recommended for symptomatic patients with moderate or severe deformity. Due to the variety of the components of hallux valgus deformity, different surgical methods can be used. Particularly in moderate or severe deformities, metatarsal osteotomies carried out with distal soft tissue procedures are frequently applied surgical methods.3
Several proximal first metatarsal osteotomies have been defined with distal soft tissue procedures, especially in the treatment of severe hallux valgus deformities. Previous studies have reported that PCO, which is one of these osteotomies, has led to clinical and radiographic healing with over 90% patient satisfaction in the medium and long term.3, 4 On the other hand, dorsiflexion malunion of the first metatarsal bone has been recorded following PCO with a ratio of 16–28%.5, 6 In addition, metatarsalgia and hallux varus transfer are possible complications that can occur.3, 6
Scarf osteotomy is suggested for the treatment of mild or moderate hallux valgus deformity and is defined as an osteotomy that translates the distal fragment laterally.7 Scarf osteotomy has gone through several modifications in time. In one of these modifications, the distal plantar fragment was rotated laterally and a more efficient correction effect was targeted in the IMA without much impact on the DMAA.8 Thus, rotational scarf osteotomy was became a surgical option that could be performed in severe deformities as well. Several studies have reported high patient satisfaction and important improvement in functional outcomes together with favorable radiographic results as a result of scarf osteotomy.8, 9, 10 Following scarf osteotomy, through (an impaction of the two osteotomy fragments resulting in loss of metatarsal height and pronation of the distal fragment) reaching a 35%11 and postoperative stiffness in the metatarsophalengeal joint have been recorded.12 It has also been reported that a rotational scarf osteotomy helps to prevent complications like through.8
Both osteotomies can be expected to have a significant corrective effect on IMA. But due to the rotation as well as translation with rotational scarf osteotomy, there can be expected a less adverse effect on DMMA compared to PCO. The present study aimed to evaluate and compare the clinical and radiological results and the complications of PCO and the rotational scarf osteotomy which are frequently preferred techniques in recent years in the treatment of moderate and severe hallux valgus deformity.
Materials and methods
The prospective randomized study was performed at a single center between 1st October 2012 and 1st September 2014. The study was approved by the local medical ethics committee and an informed consent was provided for all patients. The inclusion criteria were the patients older than 18 years of age, HVA >30°, IMA>13° and symptomatic hallux valgus deformity. Patients with degenerative osteoarthritis of the first metatarsophalangeal joint, diabetes mellitus, rheumatoid arthritis, neurological diseases, vascular diseases, previous forefoot surgery and body-mass index >30 were excluded. A total of 57 consecutive patients (60 feet) with hallux valgus deformity were randomly assigned to one of the two groups (Fig. 1). The allocation was done double blinded. The PCO group consisted of 22 women and 5 men (30 feet) and the mean age was 43 years (±14.5). The scarf group consisted of 23 women and 7 men (30 feet) and the mean age was 40.9 years (±12.6). Demographic data (mean age and sex ratio) were statistically similar between the two groups.
Fig. 1.
Flow diagram.
Clinical evaluation was made using the AOFAS Score (100 points) and the VAS score (10 points) which were performed preoperatively and at the end of the first year after surgery.
The dorsoplantar and lateral weight-bearing radiographs of the foot13 were obtained from all patients preoperatively, and at the sixth week, third month and first year after surgery. All the radiographic images were taken using a picture archiving and communication system (PACS) workstation. Radiographic measurements were made using the PACS software. The radiographic imaging and measuring system was digital. All the radiological evaluations and measurements were made by one orthopedic resident (OT). The following 6 radiographic measurements and evaluations were performed: HVA, IMA, DMAA, first metatarsal length, metatarsophalangeal joint congruence and the lateral sesamoid position14 in relation to the first metatarsal neck. While measuring HVA, IMA, and DMAA, first and second metatarsal axes were determined according to Coughlin et al.15 The lateral sesamoid subluxation level was evaluated at three grade as mild (%0–25), moderate (%25–50) and severe (%50–100).
Surgical technique
The spinal block was performed for all patients as anesthesia protocol. All surgical procedures were performed in the supine position and under pneumatic tourniquet application. Surgeries were performed by one of the two orthopedic surgeons (NŞ, GC) with the same surgical protocol. Distal lateral release and bunionectomy were made using the same technique prior to the osteotomy in both groups. After a dorsal incision was made between the first and second intermetatarsal space, attachment of the adductor hallucis muscle, transverse intermetatarsal ligament, lateral collateral ligament and capsule with lateral metatarsosesamoid suspensory ligament were released. The second incision was made dorsomedially for both surgical technique, from the proximal end of the first metatarsal up to the distal of the metatarsophalangeal joint. After the longitudinal capsular exposure, the bunion was resected in a standard fashion. Both medial capsulorrhaphy and osteotomies were made through the same incision.
A PCO about 10 mm distal to the proximal end of the first metatarsal was made using a crescentic blade. The concavity of the osteotomy was proximally pointed. The correction of the deformity was checked with an intraoperative fluoroscopy to reduce the IMA angle until the desired alignment was achieved, then fixation was made using two 2 mm Kirschner wires.
For the scarf osteotomy, z-shaped standard osteotomy cuts were made along the first metatarsal. The plantar-distal part of the osteotomy was translated and rotated laterally under fluoroscopic control to reduce the IMA angle until the desired alignment was achieved. Provisional fixation was made with two Kirschner wires. The final position of the osteotomy was secured with two 3.5 mm headless titanium screws (A-spire, Sanatmetal, Budapest, Hungary). The proximal and distal residual prominences were cut out to provide a flush medial border.
After the osteotomies and fixations were completed, the congruence of the metatarsophalangeal joint and reduction of the sesamoids was evaluated. In combination with a lateral release, medial capsular reefing was performed to realign metatarso-sesamoid complex and to correct hallux valgus deformity and aim to restore a physiological ligamentous situation on the medial side. The first suture on metatarso-sesamoid ligament to reposition the metatarsal head back onto the sesamoid apparatus and the other sutures following medial collateral ligament and capsule were performed. Medial capsular repair completed the procedure. Before the wound closure, the tourniquet was released and the hemostasis was secured.
Postoperative treatment
The same postoperative regime was applied to both groups. Below knee splint was used for three weeks. The patients were allowed 20 kg weight-bearing in the first three weeks and then allowed to ambulate as tolerated. The crutches were allowed for six weeks. The sutures were removed 14 days after the operation. The toe alignment splint was used 6 weeks after the removal of the splint.
Statistical analysis
Based on the study carried out by Mahadevan et al,16 sample size suggested that 30 patients per group would be sufficient to detect the differences 0.66 (SD = 7) as significant at p < 0.05 with at least 80% power in this study.
All statistical analyses were performed with the IBM SPSS version.23.0. Shapiro–Wilk test was used as a normality test. Continuous variables were compared using t-test and Mann–Whitney U test when the data were not normally distributed. Wilcoxon signed rank test was used for dependent variables. Post measurements were compared according to percent change (percent change=(post value-pre value)/pre value). Categorical variables were compared using Pearson's chi-squared test and Fisher-Freeman-Halton test. Also, McNemar test was used for dependent categorical variables. GEE was used for analysis of dependent categorical variables. Correlations between variables were tested using Pearson and Spearman correlation coefficients. A p-value <0.05 was considered as significant.
Results
In the clinical assessment, both methods resulted in significant improvement in the AOFAS and VAS scores at the end of the first year. The AOFAS and the VAS scores were similar both preoperative and first year postoperative evaluations between two groups (Table 1).
Table 1.
Clinical evaluation.
| Clinical parameters | PCO Group | Scarf Group | p value |
|---|---|---|---|
| AOFAS Score | |||
| Preoperative | 42 (±16.2) | 36.2 (±16.1) | p = 0.168 |
| 12 months postoperative | 66.7 (±13.4) | 73.2 (±13.5) | p = 0.076 |
| change (%) | 0.89 (±1.12) | 1.66 (±2.02) | |
| p value | p < 0.01 | p < 0.01 | |
| VAS | |||
| Preoperative | 6.3 (±1.3) | 6.5 (±1.9) | p = 0.546 |
| 12 months postoperative | 2.4 (±2) | 2.5 (±1.3) | p = 0.811 |
| change (%) | −3.9 (±2.02) | −4 (±2.49) | |
| p value | p < 0.01 | p < 0.01 | |
PCO: proximal crescentic osteotomy.
In the radiological evaluation, improvements were observed in the HVA and IMA values in both groups at the end of the first postoperative year in comparison to the preoperative period. DMAA did not change in the PCO group at the first postoperative year compared to the preoperative values whereas an improvement was observed in the scarf group (Table 2) (see Fig. 2, Fig. 3). For the metatarsal length, an average 2.6 mm (±3.8) shortening was observed in the PCO group at the first postoperative year (p < 0.01) whereas no change occurred in the scarf group (p > 0.05). The ratios of the patients with congruent joints were observed to improve at the first postoperative year in both groups (p < 0.01 for both groups) (Table 3). The rates of healing at the fibular sesamoid position in the PCO group did not change, but p-value was found to be close to the critical value (p = 0,053). On the other hand, in the scarf group, an improvement was observed at the fibular sesamoid position at the first postoperative year, in comparison to the preoperative period (p < 0.01) (Table 4).
Table 2.
Radiographic evaluation.
| Radiological parameters | PCO Group | Scarf Group | p value |
|---|---|---|---|
| HVA | |||
| Preoperative | 38.1 (±7.1) | 36.1 (±7.5) | p = 0.301 |
| 12 months postoperative | 23.8 (±8.5) | 22.2 (±7.5) | |
| change (%) | −0.37 (±0.21) | −0.39 (±0.14) | p = 0.656 |
| p value | p < 0.01 | p < 0.01 | |
| IMA | |||
| Preoperative | 17.3 (±3.8) | 16.2 (±2.6) | p = 0.215 |
| 12 months postoperative | 11.8 (±3.3) | 9.3 (±2.4) | |
| change (%) | −0.31 (±0.17) | −0.42 (±0.17) | p = 0.017 |
| p value | p < 0.01 | p < 0.01 | |
| DMAA | |||
| Preoperative | 17.1 (±4.8) | 15 (±6.7) | p = 0.182 |
| 12 months postoperative | 15.4 (±7.6) | 9.8 (±4.9) | |
| change (%) | −0.11 (±0.36) | −0.31 (±0.32) | p = 0.028 |
| p value | p > 0.05 | p < 0.01 | |
PCO: proximal crescentic osteotomy, IMA: intermetatarsal angle, DMAA: distal metatarsal articular angle.
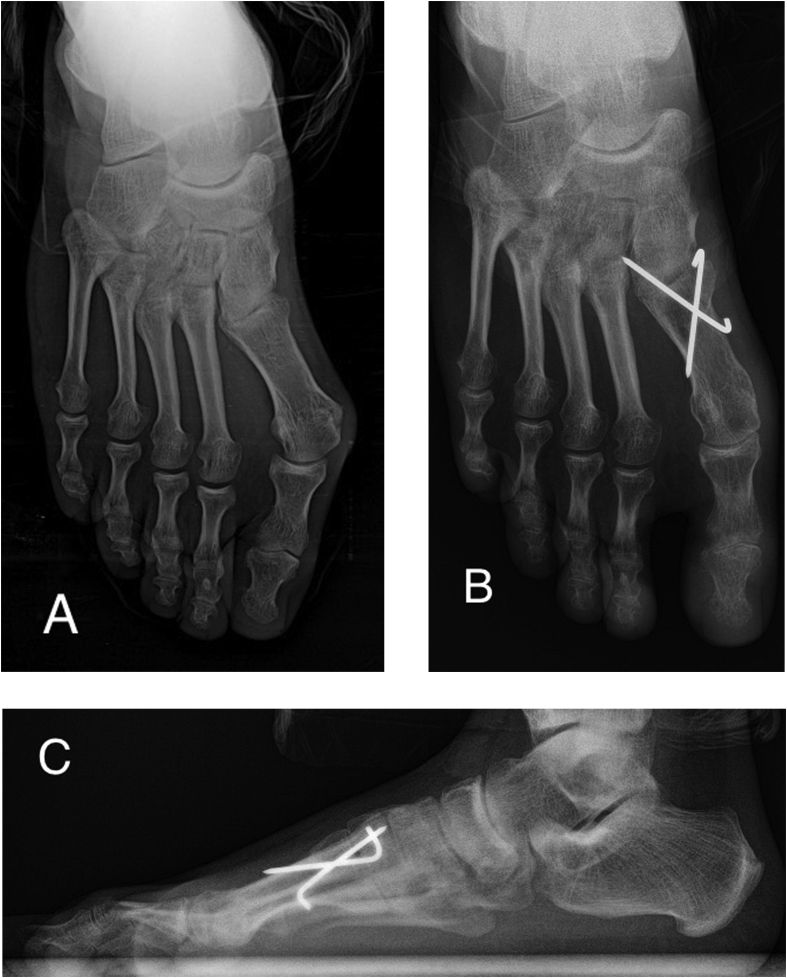
Fig. 2.
Preoperative antero-posterior (A), postoperative anteroposterior (B) and lateral (C) weight bearing X-rays of a patient who has undergone proximal crescentic osteotomy.
Fig. 3.
Preoperative antero-posterior (A), postoperative anteroposterior (B) and lateral (C) weight bearing X-rays of a patient who has undergone rotational scarf osteotomy.
Table 3.
Evaluation of the joint congruency.
| MTP joint congruency n (%) | PCO Group | Scarf Group | p value |
|---|---|---|---|
| Preoperative | |||
| congruent | 5 (16.7) | 8 (26.7) | p = 0.347 |
| incongruent | 25 (83.3) | 22 (73.3) | |
| 12 months postoperative | |||
| congruent | 24 (80) | 26 (86.7) | p = 0.893 |
| incongruent | 6 (20) | 4 (13.3) | |
| p value | p < 0.01 | p < 0.01 | |
PCO: proximal crescentic osteotomy, MTP: metatarsophalangeal joint.
Table 4.
Evaluation of the lateral sesamoid subluxation percent.
| Lateral sesamoid subluxation | PCO Group n (%) | Scarf Group n (%) | p value |
|---|---|---|---|
| Preoperative | |||
| %0-25 | 2 (6.7) | 0 (0) | p = 0.582 |
| %25-50 | 5 (16.7) | 6 (20) | |
| %50-100 | 23 (76.7) | 24 (80) | |
| 12 months postoperative | |||
| %0-25 | 7 (23.3) | 7 (23.3) | p = 0.167 |
| %25-50 | 7 (23.3) | 14 (46.7) | |
| %50-100 | 16 (53.3) | 9 (30) | |
| p = 0.053 | P < 0.001 | ||
PCO: proximal crescentic osteotomy.
The HVA and IMA values were increased in both groups at the end of the first year when compared to the postoperative sixth week values. HVA values increased from 18 (±5.4) to 23.8 (±8.5) in the PCO group (p < 0.01) and from 16.9 (±5) to 22.2 (±7.5) (p < 0.01) in the scarf group. IMA values went up from 9.2 (±3) to 11.8 (±3.3) in the PCO group and from 8.1 (±2.6) to 9.3 (±2.4) in the scarf group (p < 0.01 for both groups).
In the comparison between the groups in terms of change percentages, while changing percentage of HVA values were similar between the two groups, the changing percent in the IMA value in the scarf group was bigger than the PCO group (Table 2). The amount of shortening in the metatarsal length in the PCO group was significantly higher than that of the scarf group (Table 2) (p < 0.01). Improvements in the rates of fibular sesamoid position (subluxation percentage) and joint congruency percentages were found to be similar in both groups (Table 3, Table 4).
When all the patients were assessed together, the relations between preoperative DMAA values and postoperative first year HVA and IMA values were positive but had low significance (r = 0,327; p = 0,011 for HVA and r = 0,399; p = 0,002 for IMA). A positive relation of low significance was found between the preoperative DMAA values and the first postoperative year HVA values of the scarf group (r = 0,437; p = 0,016), whereas no significant correlation was found with IMA values (r = 0,319; p = 0,085). As for the PMO group, no significant correlation was found between the preoperative DMAA values and the postoperative first-year HVA values (r = 0,195; p = 0,302), but a positive relation of low significance was observed with IMA values (r = 0,451; p = 0,012).
Discussion
Good results have been recorded concerning both of the two methods implemented in the treatment of moderate and severe hallux valgus in the literature.4, 8, 9, 11 However, it is not possible to make a certain statement as to which osteotomy is better than the other in the surgical treatment of moderate and severe hallux valgus. Proximal metatarsal osteotomies provide a more effective correction in IMA compared to distal procedures. But due to the long lever arm of the first metatarsal, too much dorsiflexion forces are exerted on the osteotomy line. On the other hand the adding of a rotational component in the scarf osteotomy has increased the utility of this method in severe deformities. The negative impact of rotational scarf osteotomy on DMMA may be less than the PCO. How this conditions would be reflected in the clinical and radiological outcomes of the patients was of interest to this study. But as a result, this prospective study has shown that the PCO and the scarf osteotomies led to similar results in clinical and radiological parameters in the surgical treatment of moderate and severe hallux valgus.
In their prospective comparative study, Wester et al4 compared the open wedge metatarsal osteotomy to the crescentric osteotomy in patients with severe hallux valgus and found similar radiological and clinical results. In this study, they found average improvements of 11.3° in the HVA and 6.3° in the IMA with PCO at the end of the first year and stated that the improvement in AOFAS score was comparable to other studies despite the suboptimal radiological correction. In another meta-analysis,17 average IMA correction obtained with scarf osteotomy was found at 5.33°. In the study we carried out, unlike the study conducted by Wester et al,4 although first-year-end AOFAS and VAS scores were satisfactory, they remained low when compared to some other study results.4, 18, 19 This may be due to the increase we observed in the HVA and the IMA values at the end of the first postoperative year. The number of patients whose joint congruence and fibular sesamoid position recovered were improved at the postoperative first year in both groups, similar to other studies.5, 20
The radiological correction obtained on the sixth postoperative week was observed to have been partially lost in the first year. It could be the correction loss that occurs in time as seen in other studies.4, 21 A consideration was made that the high preoperative DMAA values may be a possible cause for recurrence after hallux valgus surgery. A correlation, albeit weak, was observed between the preoperative DMAAs and postoperative first-year HVA and IMA angles in our study. Therefore, in patients with high DMAA in the preoperative evaluations, combining metatarsal osteotomies with distal metatarsal or proximal phalanx osteotomies may reduce the rate of recurrence.
Although the DMAA measurement is frequently used in hallux valgus evaluations, it is reported to have low reliability by observers.22, 23 On the other hand, it is among the commonly used parameters in measuring the lateral slope of the distal metatarsal joint surface. The preoperatively measured DMAA values showed no change in the first postoperative year in the PCO group while we found an improvement in the scarf group. Since the first metatarsal is rotated from proximal in PCO, it is an expected result that the relationship between the metaphyseal axis and joint surface would not change. Likewise, because of the deformation in the metatarsal bone, particularly after scarf-like diaphysis osteotomies, measurement of the angle gets harder and its reliability decreases. After all, considering the direction of the foot as a whole, an increase in the DMAA angle is an expected outcome after both osteotomies. Perhaps, it would be more beneficial to define a new measurement method that can evaluate the first distal metatarsal joint direction according to the axis of the whole foot instead of the metatarsal axis.
First metatarsal bone shortness is a possible complication that could be seen after first metatarsal osteotomies performed in hallux valgus treatment.3, 24 Carr and Boyd25 stated a shortness of 4 mm as acceptable. Schemitsch and Horne26 reported that it is important that the relative length of the first metatarsal bone in comparison to the second is lower than 0.825%. In this study, an average 2.6 mm shortness was found in the first metatarsal in the PCO group whereas no shortness occurred in the scarf group. Medial displacement and impaction were observed in the osteotomy line in the follow-up of one patient in PCO group. This patient developed 15 mm shortness in the first metatarsal bone. This may have been caused by the high rate of shortness observed in the PCO group. Three patients had wound site complications due to the Kirschner wires and one patient had a medial displacement and impaction in the PCO group. The superficial infection at the wound site was corrected with wound care and antibiotic treatment. In the scarf group, however, no complication was observed (malunion, fracture, and loss of motion in the metatarsophalangeal joint) except for the increase in HVA and IMA values at the end of the first year like PCO.
One of the limitations of our study is that, even if power analysis is performed, the results may not be generalized due to the limited number of patients. However, the prospective randomized design increases the study's strength. Another limitation is that the follow-up time was insufficient, especially for the detection of long-term complications such as metatarsophalangeal joint osteoarthritis. In addition, the fact that metatarsal osteotomies performed additionally to soft tissue procedures in severe cases as well were carried out in isolation in this study may be controversial in terms of indications. This may explain the increase in the HVA and IMA at the end of the first year and the relatively low clinical scores. Finally, the fact no patient-reported outcome tool was used in our study disabled evaluating the procedures in terms of patients.
In conclusion, PCO and rotational scarf osteotomy in the treatment of moderate and severe Hallux valgus deformity provides a satisfactory clinical and radiological correction when combined with the distal soft tissue procedures. Clinical and radiological outcomes of both procedures are similar in the short term. Especially in patients with high preoperative DMAA, increases were observed in the HVA and IMA values in the first postoperative year in comparison with an early postoperative period.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Coughlin M.J., Jones C.P. Hallux valgus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007;28(7):759–777. doi: 10.3113/FAI.2007.0759. [DOI] [PubMed] [Google Scholar]
- 2.Roddy E., Zhang W., Doherty M. Prevalence and associations of hallux valgus in a primary care population. Arthritis Rheum. 2008;59(6):857–862. doi: 10.1002/art.23709. [DOI] [PubMed] [Google Scholar]
- 3.Schuh R., Willegger M., Holinka J., Ristl R., Windhager R., Wanivenhaus A.H. Angular correction and complications of proximal first metatarsal osteotomies for hallux valgus deformity. Int Orthop. 2013;37(9):1771–1780. doi: 10.1007/s00264-013-2012-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wester J.U., Hamborg-Petersen E., Herold N., Hansen P.B., Froekjaer J. Open wedge metatarsal osteotomy versus crescentic osteotomy to correct severe hallux valgus deformity-A prospective comparative study. Foot Ankle Surg. 2016;22(1):26–31. doi: 10.1016/j.fas.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 5.Easley M.E., Kiebzak G.M., Davis W.H., Anderson R.B. Prospective, randomized comparison of proximal crescentic and proximal chevron osteotomies for correction of hallux valgus deformity. Foot Ankle Int. 1996;17(6):307–316. doi: 10.1177/107110079601700603. [DOI] [PubMed] [Google Scholar]
- 6.Mann R.A., Rudicel S., Graves S.C. Repair of hallux valgus with a distal soft-tissue procedure and proximal metatarsal osteotomy. A long-term follow-up. J Bone Joint Surg Am. 1992;74(1):124–129. [PubMed] [Google Scholar]
- 7.Molloy A., Widnall J. Scarf osteotomy. Foot Ankle Clin. 2014;19(2):165–180. doi: 10.1016/j.fcl.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Murawski C.D., Egan C.J., Kennedy J.G. A rotational scarf osteotomy decreases troughing when treating hallux valgus. Clin Orthop Relat Res. 2011;469(3):847–853. doi: 10.1007/s11999-010-1647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crevoisier X., Mouhsine E., Ortolano V., Udin B., Dutoit M. The scarf osteotomy for the treatment of hallux valgus deformity: a review of 84 cases. Foot Ankle Int. 2001;22(12):970–976. doi: 10.1177/107110070102201208. [DOI] [PubMed] [Google Scholar]
- 10.Jeuken R.M., Schotanus M.G., Kort N.P., Deenik A., Jong B., Hendrickx R.P. Long-term follow-up of a randomized controlled trial comparing scarf to chevron osteotomy in hallux valgus correction. Foot Ankle Int. 2016;37(7):687–695. doi: 10.1177/1071100716639574. [DOI] [PubMed] [Google Scholar]
- 11.Coetzee J.C. Scarf osteotomy for hallux valgus repair: the dark side. Foot Ankle Int. 2003;24(1):29–33. doi: 10.1177/107110070302400104. [DOI] [PubMed] [Google Scholar]
- 12.Hammel E., Abi Chala M.L., Wagner T. Complications of first ray osteotomies: a consecutive series of 475 feet with first metatarsal Scarf osteotomy and first phalanx osteotomy. Rev Chir Orthop Reparatrice Appar Mot. 2007;93(7):710–719. doi: 10.1016/s0035-1040(07)73256-7. [DOI] [PubMed] [Google Scholar]
- 13.Smith R.W., Reynolds J.C., Stewart M.J. Hallux valgus assessment: report of research committee of American Orthopaedic Foot and Ankle Society. Foot Ankle. 1984;5(2):92–103. doi: 10.1177/107110078400500208. [DOI] [PubMed] [Google Scholar]
- 14.Agrawal Y., Desai A., Mehta J. Lateral sesamoid position in hallux valgus: correlation with the conventional radiological assessment. Foot Ankle Surg. 2011;17(4):308–311. doi: 10.1016/j.fas.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Coughlin M.J., Saltzman C.L., Nunley J.A., 2nd Angular measurements in the evaluation of hallux valgus deformities: a report of the ad hoc committee of the American Orthopaedic Foot & Ankle Society on angular measurements. Foot Ankle Int. 2002;23(1):68–74. doi: 10.1177/107110070202300114. [DOI] [PubMed] [Google Scholar]
- 16.Mahadevan D., Lines S., Hepple S., Winson I., Harries W. Extended plantar limb (modified) chevron osteotomy versus scarf osteotomy for hallux valgus correction: a randomised controlled trial. Foot Ankle Surg. 2016;22(2):109–113. doi: 10.1016/j.fas.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 17.Smith S.E., Landorf K.B., Butterworth P.A., Menz H.B. Scarf versus chevron osteotomy for the correction of 1-2 intermetatarsal angle in hallux valgus: a systematic review and meta-analysis. J Foot Ankle Surg. 2012;51(4):437–444. doi: 10.1053/j.jfas.2012.02.016. [DOI] [PubMed] [Google Scholar]
- 18.Giannini S., Cavallo M., Faldini C., Luciani D., Vannini F. The SERI distal metatarsal osteotomy and Scarf osteotomy provide similar correction of hallux valgus. Clin Orthop Relat Res. 2013;471(7):2305–2311. doi: 10.1007/s11999-013-2912-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones S., Al Hussainy H.A., Ali F., Betts R.P., Flowers M.J. Scarf osteotomy for hallux valgus. A prospective clinical and pedobarographic study. J Bone Joint Surg Br. 2004;86(6):830–836. doi: 10.1302/0301-620x.86b6.15000. [DOI] [PubMed] [Google Scholar]
- 20.Fuhrmann R.A., Zollinger-Kies H., Kundert H.P. Mid-term results of Scarf osteotomy in hallux valgus. Int Orthop. 2010;34(7):981–989. doi: 10.1007/s00264-010-0958-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Deveci A., Firat A., Yilmaz S., Oken O.F., Yildirim A.O., Ucaner A., Bozkurt M. Short-term clinical and radiologic results of the scarf osteotomy: what factors contribute to recurrence? J Foot Ankle Surg. 2013;52(6):771–775. doi: 10.1053/j.jfas.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 22.Lee K.M., Ahn S., Chung C.Y., Sung K.H., Park M.S. Reliability and relationship of radiographic measurements in hallux valgus. Clin Orthop Relat Res. 2012;470(9):2613–2621. doi: 10.1007/s11999-012-2368-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coughlin M.J., Freund E., Roger A., Mann Award The reliability of angular measurements in hallux valgus deformities. Foot Ankle Int. 2001;22(5):369–379. doi: 10.1177/107110070102200503. [DOI] [PubMed] [Google Scholar]
- 24.Easley M.E., Trnka H.J. Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int. 2007;28(6):748–758. doi: 10.3113/FAI.2007.0748. [DOI] [PubMed] [Google Scholar]
- 25.Carr C.R., Boyd B.M. Correctional osteotomy for metatarsus primus varus and hallux valgus. J Bone Joint Surg Am. 1968;50(7):1353–1367. [PubMed] [Google Scholar]
- 26.Schemitsch E., Horne G. Wilson's osteotomy for the treatment of hallux valgus. Clin Orthop Relat Res. 1989;240:221–225. [PubMed] [Google Scholar]