Abstract
Objective
The aim of this study was to assess and compare the effects of different electrotherapy methods and exercise therapy on pain, function and quality of life in shoulder impingement syndrome.
Methods
Eighty-three patients (66 females, 17 males; mean age: 48.2 ± 7.33 years) with shoulder impingement syndrome were selected and 79 of them were randomly allocated into four groups. Group 1 (n = 19, mean age: 47.89 ± 7.12 years) was given hot pack and exercises, Group 2 (n = 20, mean age: 47.70 ± 6.51 years) was given hot packs, exercises and interferential current, Group 3 (n = 20, mean age: 48.50 ± 8.34 years) was given hot packs, exercises and TENS and Group 4 (n = 20, mean age: 48.55 ± 7.89 years) was given hot packs, exercises and ultrasound three times a week for four weeks. Assessments were made before treatment, right after it and three months after that using the visual analog scale (VAS), Short Form-36 (SF-36) and the Disabilities of the Arm, Shoulder and Hand (DASH) outcome measures.
Results
At the fourth week and third month assessments, all groups showed significant improvements in terms of pain, DASH and SF-36 physical component scores (p < 0.05). In intragroup comparisons, a significant difference between pre- and post-treatment results was found only in SF-36 mental component scores of Group 2. No significant difference was observed between the groups in any stage of the study period (p > 0.05).
Conclusion
Application of ultrasound, interferential current and TENS in addition to exercise therapy in shoulder impingement syndrome treatment had similar improvements in terms of pain, function and physical component of quality of life. However, interferential current treatment showed significantly better outcomes for the mental component of quality of life.
Level of evidence
Level I, Therapeutic study.
Keywords: Electrotherapy, Exercises, Pain, Quality of life, Shoulder impingement syndrome
Shoulder pain is one of the most frequent type of musculoskeletal complaints.1, 2 Subacromial impingement syndrome, also known as shoulder impingement syndrome (SIS) is the most common cause of shoulder pain, with a prevalence of %44–65 among all shoulder pains.3, 4 It is defined as the mechanical compression of the rotator cuff and subacromial bursa between the humerus and coracoacromial arch.4, 5, 6 The condition is seen more frequently in women and with an increasing incidence by age. It causes painful movement limitation, functional deficit and restriction of daily living activities. As a result of overuse of the shoulder, especially in overhead positions, weakness of shoulder stability and various traumas occur.2, 5, 6
The treatment of SIS is mostly performed through conservative methods,7 in which the aim is to reduce the pain and joint stiffness, improve muscle strength, prevent progression of the problems, bring shoulder function to the highest level and bring the person back to daily activities as early as possible.5, 8, 9, 10, 11 These conservative methods include exercise programs for the rotator cuff and scapular muscles, a variety of medications, manual therapy techniques, modification of daily activities and a variety of physical therapy modalities.10, 11, 12 In general practice, physical therapy and rehabilitation usually begins with heat application to relieve soft tissue pain and continues with different electrotherapy modalities. Transcutaneous electrical nerve stimulation (TENS), interferential current and ultrasound are the most popular applications to control pain, increase blood circulation and prepare the patient for exercise.13 Yavuz et al. compared the ultrasound and the low-level laser therapy in treatment of SIS and showed improvement in terms of pain and disability with both treatments.11 Van der Heijden et al.14 compared the ultrasound and the exercise to placebo ultrasound and exercise, and then to exercise alone and found that the groups showed no difference in self-perceived recovery, pain or functional capacity. In addition, the authors compared bipolar interferential current in addition to exercise to placebo bipolar interferential current and exercise, and exercise alone and again observed no difference between groups in the short and long term. In a recent study, Page et al. reviewed 47 trials out of 3488 articles about electrotherapy modalities for rotator cuff disease and concluded that although these modalities were widely used as components of physical therapy interventions, the evidence levels of the studies were low and that high-quality placebo-controlled trials were needed to confirm the effects of electrotherapy.15 To our knowledge, additional effects of the applications have not been established and the comparison of different methods has not been researched yet. Furthermore, long-term results of the patients after the program are unknown.
Therefore, the aims of our study were to evaluate and compare the effectiveness of a four-week physical therapy and rehabilitation program with different electrotherapy applications on pain, quality of life and function in treatment of SIS and to investigate the three-month results after the program was over. We hypothesized that there might be positive effects of additional different electrotherapy applications on the quality of life, pain and functionality in SIS. Different electrotherapy applications are not superior to each other. All of the applications may maintain their effect after the third month of follow-up.
Patients and methods
In this prospective randomized controlled study, 95 volunteers who had a shoulder pain complaint lasting at least for four weeks and were diagnosed with SIS with clinical examinations and MRIs were selected.
The selection criteria were as follows: 1) patients aged between 18 and 55, 2) have continuous unilateral shoulder symptoms, 3) have a restriction of less than 30% in passive range of motion compared to the unaffected side and 4) haven't undergone any type of treatment for the past year at least. Twelve patients who had adhesive capsulitis or major rotator cuff tears, permanent loss of shoulder function, advanced muscle atrophy and weakness, sensory and muscular deficits rooted from neurological, inflammatory joint diseases or previous shoulder injury, a history of shoulder dislocation or surgery, have had steroid injections during the past six months and were using any steroids or NSAIDs were later excluded.
The patients were informed about the study and their written informed consent was obtained. This study was conducted in accordance with the rules of the Declaration of Helsinki and was approved by the Ethics Committee of the University (approval number: 75/1.04.2015).
Eighty-three patients (66 females, 17 males; mean age: 48.2 ± 7.33 years) with shoulder impingement syndrome were selected. Four of them dropped out of the study due to personal reasons. The remaining 79 patients were randomly allocated into four groups using the SPSS software (SPSS Inc., Chicago, IL, USA). Group 1 (n = 19, mean age: 47.89 ± 7.12 years) was given hot pack + exercises, Group 2 (n = 20, mean age: 47.70 ± 6.51 years) was given hot pack + exercises + interferential current, Group 3 (n = 20, mean age: 48.50 ± 8.34 years) was given hot pack + exercises + TENS and Group 4 (n = 20, mean age: 48.55 ± 7.89 years) was given hot pack + exercises + ultrasound for three days per week for four weeks. The patients were told not to use any pain-killer during treatment and they were evaluated before treatment, right after that and at the postoperative third month.
Patients' demographic data, previous treatments, height and weight were asked. A visual analog scale (VAS) was used for pain, the Short Form-36 (SF-36) for the quality of life, and the Disabilities of the Arm, Shoulder and Hand questionnaire (DASH) for shoulder function assessments.
In VAS assessment, the patients were asked to place a vertical mark along a horizontal line indicating their current degree of pain at rest and during activity, where 0 points indicated ‘no pain’ and 100 points indicated ‘worst pain’.16
The SF-36 scale is an indicator of a patient's overall health status and it consists of eight sections: vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, emotional role functioning, social role functioning and mental health.17 The physical and mental component summaries were used for this study. Scores range from 0 to 100. Lower scores indicate more disability, higher scores indicate less disability.
The DASH questionnaire is designed to measure the physical function and symptoms of people with musculoskeletal disorders in the upper limb. It consists of 30 items; 6 items about symptoms and 24 items about function. Patients answer the questions using a 5-point Likert system and the cumulative score is scaled from 0 to 100, with higher scores indicating more disability.18
To reduce muscle spasm, all patients received hot pack application on the upper trapezius muscle for 15 min. After this warm-up and relaxation period, a standardized exercise program was applied. The exercise program included Wand exercises for shoulder abduction, flexion, hyperextension and internal and external rotation, Codman exercises and isometric and resistive exercises of the shoulder girdle.5, 10, 19 The exercise program was performed under the supervision of an experienced physiotherapist and the patients were encouraged to exercise at home on daily basis. The exercises were adjusted according to the patient's tolerance. The isometric exercises were used during the painful period, and the resistance exercises were added after the pain began to relieve. In addition to the routine hot pack and exercise program, different electrotherapy modalities were used for the groups except the controls. Group 2 patients were given interferential current at 50–120 Hz frequency for 20 min around the effected shoulder. Group 3 patients were given TENS in conventional mode for 20 min. Group 4 patients had a 1 MHz ultrasound at an intensity of 1.5 W/cm2 for 5 min.14 All electrotherapy applications were performed using the Enraf-Nonius 492 Sonopuls (Enraf-Nonius BV, Rotterdam, the Netherlands) combined device.
The G × Power software v.3.0.10 (Franz Faul, Kiel University, Germany) was used to determine the necessary sample size of at least 76 subjects, including at least 19 individuals of each group. The power of the test in this series was estimated to be approximately 80.48%. The SPSS software v.20 (SPSS Inc., Chicago, IL, USA) was used for calculations. All values were presented in mean and standard deviation and in percentage. The repeated measures ANOVA test was used in comparison of the means of the repeated measures. The results of the repeated measures ANOVA were analyzed by Mauchly's sphericity test and Box's M Test. If the parametric tests (factorial design for repeated measures analysis) did not provide the preconditions, the Greenhouse-Geisser (1959) or Huynh-Feldt (1976) correction was used for corrections to the degrees of freedom or Friedman's Test. The Bonferroni correction was used for multiple comparisons. P values of < 0.05 and < 0.01 was considered statistically significant.
Results
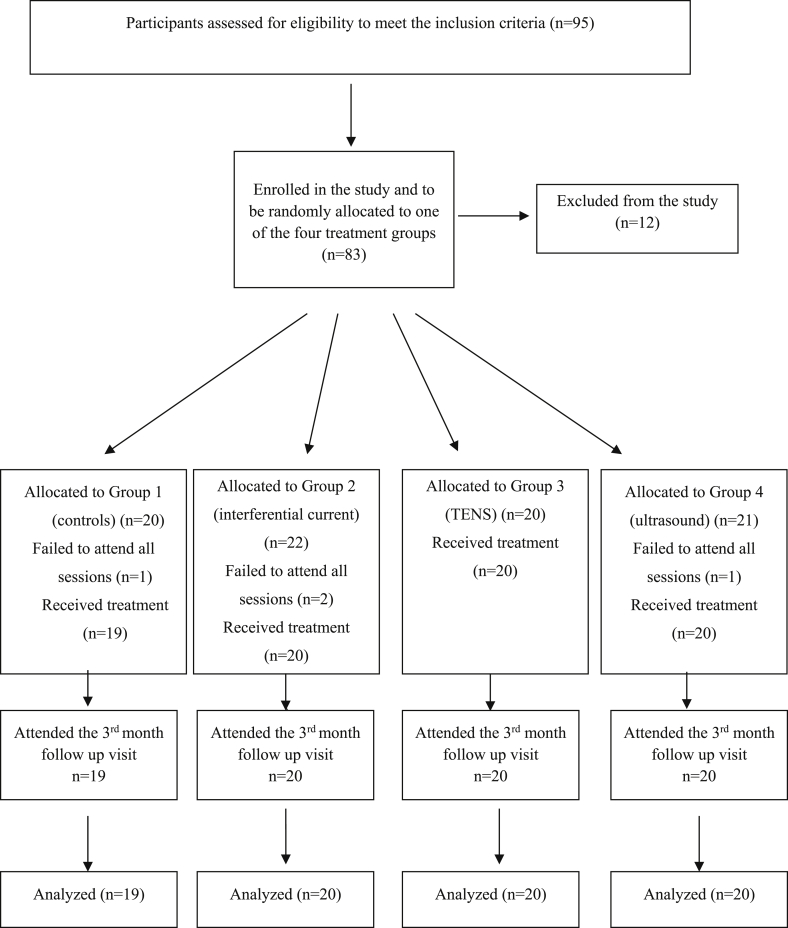
Details of participant selection and analyses are shown in Fig. 1. Physical characteristics among the groups were similar for all variables (p > 0.05), except the affected side (p < 0.05) as displayed in Table 1.
Fig. 1.
Flow-chart of participant selection and analysis.
Table 1.
Demographic characteristics of the groups.
| Group 1 (control) (n = 19) Mean ± SD |
Group 2 (interferential current) (n = 20) Mean ± SD |
Group 3 (TENS) (n = 20) Mean ± SD |
Group 4 (ultrasound) (n = 20) Mean ± SD |
Total (n = 79) Mean ± SD |
p | |
|---|---|---|---|---|---|---|
| Year | 47.89 ± 7.12 | 47.70 ± 6.51 | 48.50 ± 8.34 | 48.55 ± 7.89 | 48.2 ± 7.33 | 0.978 |
| BMI (kg/m2) | 28.93 ± 5.79 | 27.80 ± 3.60 | 29.77 ± 6.55 | 27.67 ± 5.16 | 28.6 ± 5.33 | 0.582 |
| Gender | ||||||
| Female | 17 (89.5%) | 14 (70%) | 15 (75%) | 19 (95%) | 65 (82.3%) | 0.130 |
| Male | 2 (10.5%) | 6 (30%) | 5 (25%) | 1 (5%) | 14 (17.7%) | |
| Dominant side | ||||||
| Right | 19 (100%) | 20 (100%) | 19 (95%) | 19 (95%) | 77 (97.5%) | 0.586 |
| Left | 1 (5%) | 1 (5%) | 2 (2.5%) | |||
| Affected side | ||||||
| Right | 9 (47.4%) | 14 (70%) | 18 (90%) | 15 (75%) | 56 (70.9%) | 0.030∗ |
| Left | 10 (52.6%) | 6 (30%) | 2 (10%) | 5 (25%) | 23 (29.1%) | |
| Educational status | ||||||
| Illiterate | 1 (5.3%) | 0 | 0 | 2 (10%) | 3 (3.8%) | 0.360 |
| Primary school | 11 (57.9%) | 13 (65%) | 9 (45%) | 10 (50%) | 43 (54.4%) | |
| Middle school | 2 (10.5%) | 2 (10%) | 2 (10%) | 2 (10%) | 8 (10.1%) | |
| High school | 4 (20.1%) | 3 (15%) | 5 (25%) | 4 (20%) | 16 (20.3%) | |
| University | 1 (5.3%) | 2 (10%) | 4 (20%) | 2 (10%) | 9 (11.4%) | |
∗p< 0.05.
Significant differences were observed in Groups 1, 2 and 4 in intragroup comparisons of pain at rest before the treatment, at the end of fourth week and postoperative third month (p < 0.05). Intergroup comparisons exhibited significant differences between pain at rest before and after the treatment. Before the treatment, Group 1 significantly differed from Group 3 and Group 3 significantly differed from Group 4. After the treatment, Group 3 significantly differed from Group 4 (p < 0.05). No significant differences were detected among the groups at the postoperative third month measurements (Table 2). There was no difference between the groups in terms of activity pain before the treatment. Significant differences were detected within each group before the treatment, after the treatment and at the postoperative third month results. However, no significant differences were detected among the groups (Table 2).
Table 2.
Pre-treatment, post-treatment and postoperative 3rd month VAS scores.
| VAS | Group 1 (control) Mean ± SD |
Group 2 (interferential current) Mean ± SD |
Group 3 (TENS) Mean ± SD |
Group 4 (ultrasound) Mean ± SD |
p (intergroup comparisons) |
|
|---|---|---|---|---|---|---|
| VAS at rest | Pre-treatment | 3.05 ± 3.08 | 3.00 ± 2.79 | 1.25 ± 2.12 | 3.45 ± 3.14 | 0.001∗ |
| Post-treatment | 2.21 ± 2.86 | 1.40 ± 2.64 | 0.65 ± 1.46 | 2.20 ± 2.61 | 0.001∗ | |
| 3rd month | 1.58 ± 2.36 | 1.05 ± 1.85 | 0.35 ± 1.08 | 1.30 ± 2.51 | 0.056 | |
| p (intragroup comparisons) |
0.001∗ | 0.001∗ | 0.46 | 0.001∗ | ||
| VAS during activity | Pre-treatment | 7.84 ± 1.26 | 7.85 ± 1.56 | 7.45 ± 0.99 | 7.30 ± 1.69 | 0.999 |
| Post-treatment | 5.84 ± 1.86 | 5.50 ± 2.31 | 5.00 ± 1.68 | 5.45 ± 2.04 | 0.999 | |
| 3rd month | 4.58 ± 2.57 | 4.00 ± 2.67 | 4.60 ± 2.64 | 4.05 ± 2.37 | 0.999 | |
| p (intragroup comparisons) |
0.001∗ | 0.001∗ | 0.001∗ | 0.001∗ |
∗p<0.01.
When we compared the quality of life via physical component of the SF-36 questionnaire among patients of the same group, the results showed significant differences before the treatment, after the treatment and at the third postoperative month (p < 0.05). However, no significant differences were detected among the groups (Table 3). When patients in Group 2 were compared among themselves, the mental component score showed significant differences between pretreatment and post-treatment measurements (p < 0.05). Measurements of the mental component at the three time points showed no significant differences among the groups (Table 3).
Table 3.
Pre-treatment, post-treatment and postoperative 3rd month quality of life scores.
| Quality of Life | Group 1 (control) Mean ± SD |
Group 2 (interferential current) Mean ± SD |
Group 3 (TENS) Mean ± SD |
Group 4 (ultrasound) Mean ± SD |
p (intergroup comparisons) |
|
|---|---|---|---|---|---|---|
| SF-36 Physical Component |
Pre-treatment | 30.22 ± 4.64 | 31.24 ± 8.62 | 34.17 ± 6.24 | 31.39 ± 6.77 | 0.741 |
| Post-treatment | 36.10 ± 6.75 | 37.10 ± 9.85 | 39.58 ± 7.50 | 35.80 ± 7.73 | 0.741 | |
| 3rd month | 39.61 ± 9.13 | 41.07 ± 11.92 | 39.69 ± 10.27 | 40.06 ± 9.31 | 0.741 | |
| p (intragroup comparisons) |
0.001∗ | 0.001∗ | 0.001∗ | 0.001∗ | ||
| SF-36 Mental Component |
Pre-treatment | 42.77 ± 9.49 | 37.99 ± 9.75 | 39.71 ± 12.48 | 37.07 ± 11.96 | 0.851 |
| Post-treatment | 43.16 ± 8.53 | 41.29 ± 9.64 | 40.92 ± 11.25 | 38.26 ± 12.56 | 0.851 | |
| 3rd month | 45.60 ± 7.54 | 44.03 ± 8.10 | 41.45 ± 11.66 | 39.49 ± 10.89 | 0.851 | |
| p (intragroup comparisons) |
0.054 | 0.001∗ | 0.374 | 0.174 |
∗p<0.01.
The DASH scores did not exhibit any significant differences among the groups before the treatment. However, in intragroup evaluations the DASH scores showed significant decrease among the three time points in all groups (p < 0.05) (Table 4). Comparison of the groups on the other hand displayed no significant differences among the groups.
Table 4.
Pre-treatment, post-treatment and postoperative 3rd month DASH scores.
| DASH scores |
Group 1 (control) Mean ± SD |
Group 2 (interferential current) Mean ± SD |
Group 3 (TENS) Mean ± SD |
Group 4 (ultrasound) Mean ± SD |
p (intergroup comparisons) |
|---|---|---|---|---|---|
| Pre-treatment | 58.28 ± 13.27 | 56.00 ± 15.53 | 51.78 ± 15.29 | 57.41 ± 17.52 | 0.346 |
| Post-treatment | 46.72 ± 18.60 | 43.12 ± 21.64 | 37.84 ± 16.33 | 45.96 ± 17.51 | 0.346 |
| 3rd month | 39.88 ± 22.13 | 31.89 ± 21.53 | 38.21 ± 22.28 | 35.50 ± 21.48 | 0.346 |
| p (intragroup comparisons) |
0.001∗ | 0.001∗ | 0.001∗ | 0.001∗ |
∗p<0.01.
Discussion
Subacromial impingement syndrome is the most widespread cause of shoulder pain. The aim of conservative treatment of SIS is to decrease the pain and subacromial inflammation, to provide opportunity for recovery and increase function and the quality of life. Many treatment alternatives are available such as: anti-inflammatory drugs, superficial thermal applications (cold pack and hot pack), exercise therapy and electrotherapeutic modalities. However, the optimal treatment of SIS is still controversial.12 Exercises are the most important part of treatment. Blume et al. compared the eccentric versus concentric progressive resistance exercises and found that both programs resulted in improved function, active range of motion and strength in patients with SIS.20 Granviken and Vasseljen demonstrated that both home exercises and supervised exercises are similarly effective for people with SIS.21 Moezy et al. investigated the effect of a six-week supervised scapular stabilization exercise therapy on pain, scapular position, head and back posture and shoulder mobility in comparison to physical therapy in SIS patients22 and achieved similar results to ours, indicating that exercise significantly decreased the pain and that no significant difference was found in the VAS score, thus the shoulder pain of the subjects. Numerous studies have shown the matching effect of exercise therapy alone in reducing pain versus those combined with other treatments.23, 24, 25 Similarly, we detected a significant improvement in pain, quality of life and function in the group that received exercise therapy as controls.
While therapeutic exercises are currently considered as an effective treatment method,26, 27, 28 a lot of electrotherapeutic agents are used for the treatment of SIS in conventional therapy in daily routine to decrease pain, improve mobility and prepare the tissue to exercise; additional effects of the agents are unclear.29, 30, 31, 32 Ultrasound, interferential current and TENS were used in this study as different electrotherapeutic agents.
The efficacy of ultrasound as a commonly used electrophysiological agent in the treatment of SIS was discussed in many studies. Yavuz et al. compared ultrasound with low-level laser and found significant improvement in terms of pain, the quality of life and shoulder disability in both groups.11 Calis et al. also demonstrated that ultrasound and laser therapy were effective in terms of pain and function but not superior over the other.10 Yazmalar et al. compared sham ultrasound and continuous ultrasound therapy and found no differences between the groups in terms of pain and function and asserted that both modalities proved to have no benefits on SIS.33 Van der Heijden et al. compared bipolar interferential electrotherapy and pulsed ultrasound therapy and found no differences between groups in terms of pain and function and suggested that neither modalities were effective as adjuvants to exercise therapy.14 We found significant improvement in pain, quality of life and function in the group that received ultrasound therapy but in comparison with the other groups, the effect of ultrasound was not superior over others.
Interferential current therapy is another widespread electrotherapeutic technique. However, the information about its effectiveness is limited.34, 35 In Van der Heijden et al.’s study,14 the patients were divided into three groups: (1) those who received bipolar interferential current and exercises (active and passive ROM of the shoulder), (2) those who received placebo bipolar interferential current and exercises, and (3) those who received exercises alone. There were no differences in terms of pain and functional capacity among the groups at the short and long-term follow-up. While some studies showed the effectiveness of interferential current therapy in different diseases,35, 36 some others demonstrated that neither active nor sham interferential current therapy was superior over the other.37, 38, 39 In a systematic review and meta-analysis conducted by Fuentes et al.,34 adjuvant interferential current seemed to be more effective in reducing pain than a control treatment, and that it was more effective than a placebo treatment at the third month follow-up. However, interferential current alone was not significantly better than placebo or other therapy at discharge or during the follow-up period.34 In our study, we observed a significant improvement in terms of pain, function and quality of life in the group that received interferential current therapy, but when compared to the other groups, no superiority was observed. However, an improvement in the mental component of quality of life was observed only in this group. Electrotherapeutic techniques have a wide area of use for mental improvements and physiological effects. This study also investigated the mental components of the treatments. Some patients might have been affected by the use of different machines. We used three different electrotherapeutic methods with the same machine. The duration of interferential current application was similar to TENS and longer than the ultrasound. However, interferential current may have deeper penetration than TENS and ultrasound and cause less discomfort than TENS. All these situations may have affected the patient's perception and cause a mental well-being which may also be important for the patient's expectations regarding the treatment.
Transcutaneous electrical nerve stimulation was another modality we used for the study. TENS has a widespread use for pain-control according to the gate control theory in which ‘peripheral’ inhibition of pain can be obtained as a result of stimulating the large non-nociceptive afferent (Aβ) fibers.40 Despite its common use for pain, the evidence for TENS's efficacy is scarce. Kocyiğit et al. compared the immediate effect of TENS and found no significant differences in comparison to sham application.41 In Shehab and Adham's study, TENS showed superiority over ultrasound therapy.42 On the other hand, Herrera-Lasso et al. found no significant differences between TENS and ultrasound.43 We demonstrated that there is a significant improvement in pain, function and quality of life in the group that received TENS, but when compared to the other groups, there was no superiority.
Our study had some limitations. First, the affected sides in patients were different. However, the affected side was the dominant side in most cases. Dominant side may be effective for functional outcomes, especially in daily activities. Second, VAS scores at rest were different before treatment, where Group 3 had the lowest score. Therefore, no statistically significant difference was observed in this group after the treatment. However, the scores for pain during activity were similar for all groups. Taking the pain characteristics of SIS into account, we realized that focusing on the results of activity pain might be more essential than focusing on the pain at rest. Moreover, although improvements were observed in all groups, the pain did not subside totally at the third month follow-up. Third, although the patients were told to carry on with their exercises after treatment, we could not properly follow up on the patients in their homes, thus, we could not conclude from the results based on exercise continuum after the supervised program. Fourth, we only used three different electrotherapeutic methods with the same machine. We did not use any placebo application as per the hypothesis of the study. Placebo applications may be investigated in further studies. Finally, a control group with no treatment could not be used due to ethical issues.
In conclusion, the application of ultrasound, interferential current or TENS as different electrotherapeutic agents in addition to exercise therapy in the treatment of SIS exhibited similar improvements in terms of pain, function and the physical component of quality of life at fourth week after the treatment and at the postoperative third month. Interferential current treatment provided significantly better outcomes in the mental component of quality of life. Further studies with long-term follow-ups are needed to investigate the effects of different electrotherapy agents.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Akman S., Küçükkaya M. Subacromial impingement syndrome: pathogenesis, clinical features, and examination methods. Acta Orthop Traumatol Turc. 2003;37(Suppl 1):27–34. [PubMed] [Google Scholar]
- 2.Thornton L.A., McCarty C.M., Burgess M.J. Effectiveness of low-level laser therapy combined with an exercise program to reduce pain and increase function in adults with shoulder pain: a critically appraised topic. J Sport Rehabil. 2013;22(1):72–78. doi: 10.1123/jsr.22.1.72. [DOI] [PubMed] [Google Scholar]
- 3.Huang H., Lin J., Guo Y.L., Wang W.T.J., Chen Y.J. EMG biofeedback effectiveness to alter muscle activity pattern and scapular Kinematics in subjects with and without shoulder impingement. J Electromyogr Kinesiol. 2013;23(1):267–274. doi: 10.1016/j.jelekin.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 4.Chester R., Smith T.O., Hooper L., Dixon J. The impact of Subacromial Impingement Syndrome on muscle activity patterns of the shoulder complex: a systematic review of electromyographic studies. BMC Musculoskelet Disord. 2010;11(45):1–12. doi: 10.1186/1471-2474-11-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cakmak A. Conservative treatment of subacromial impingement syndrome. Acta Orthop Traumatol Turc. 2003;37(Suppl 1):112–118. [PubMed] [Google Scholar]
- 6.Cools M.A., Johansson F.R., Borms D., Maenhout A. Prevention of shoulder injuries in overhead athletes: a science-based approach. Braz J Phys Ther. 2015;19(5):331–339. doi: 10.1590/bjpt-rbf.2014.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Celik D., Sirmen B., Demirhan M. The relationship of muscle strength and pain in subacromial impingement syndrome. Acta Orthop Traumatol Turc. 2011;45(2):79–84. doi: 10.3944/AOTT.2011.2425. [DOI] [PubMed] [Google Scholar]
- 8.Morrison D.S., Greenbaum B.S., Einhorn A. Shoulder impingement. Orthop Clin North Am. 2000 Apr;31(2):285–293. doi: 10.1016/s0030-5898(05)70148-6. [DOI] [PubMed] [Google Scholar]
- 9.Aytar A. Subakromial Sıkışma Sendromu Konservatif Tedavi. In: Baltacı G., editor. Omuz Yaralanmalarında Rehabilitasyon. Pelikan Yayıncılık; Ankara: 2015. [Google Scholar]
- 10.Calis H.T., Berberoglu N., Calis M. Are ultrasound, laser and exercise superior to each other in the treatment of subacromial impingement syndrome? Randomized clinical trial. Eur J Phys Rehabil Med. 2011;47(3):375–380. [PubMed] [Google Scholar]
- 11.Yavuz F., Duman I., Taskaynatan M.A., Tan K.A. Low-level laser therapy versus ultrasound therapy in the treatment of subacromial impingement syndrome: a randomized clinical trial. J Back Musculoskelet Rehabil. 2014;27(3):15–320. doi: 10.3233/BMR-130450. [DOI] [PubMed] [Google Scholar]
- 12.Dong W., Goost H., Lin X.B. Treatments for shoulder impingement syndrome. Medicine. 2015;94(10):1–17. doi: 10.1097/MD.0000000000000510. e510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yuruk O. Omuz Rehabilitasyonunda Kullanılan Fiziksel Ajanlar ve Elektroterapi Yöntemleri. In: Baltacı G., editor. Omuz Yaralanmalarında Rehabilitasyon. Pelikan Yayıncılık; Ankara: 2015. [Google Scholar]
- 14.Van Der Heijden G.J., Leffers P., Wolters P.J. No effect of bipolar interferential electrotherapy and pulsed ultrasound for soft tissue shoulder disorders: a randomised controlled trial. Ann Rheum Dis. 1999;58(9):530–540. doi: 10.1136/ard.58.9.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page M.J., Green S., Mrocki M.A. Electrotherapy modalities for rotator cuff disease. Cochrane Database Syst Rev. 2016;10(6):1–254. doi: 10.1002/14651858.CD012225. CD012225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boonstra A.M., Schiphorst Preuper H.R., Reneman M.F., Posthumus J.B., Stewart R.E. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res. 2008;31(2):165–169. doi: 10.1097/MRR.0b013e3282fc0f93. [DOI] [PubMed] [Google Scholar]
- 17.Koçyiğit H., Aydemir Ö., Fişek G. Kısa Form-36’nın Türkçe versiyonunun güvenilirliği ve geçerliliği. İlaç ve Tedavi Dergisi. 1999;12(2):102–106. [Google Scholar]
- 18.Düger T., Yakut E., Öksüz Ç. Kol-omuz ve el sorunları anketi: Türkçe uyarlamasının geçerlik ve güvenirliği. Fizyoter Rehabil. 2006;17(3):99–107. [Google Scholar]
- 19.Kisner C., Colby L.A. The shoulder and shoulder girdle. In: Kısner C., Colby L.A., editors. Therapeutic Exercises. 5th ed. Philadelphia; 2007. [Google Scholar]
- 20.Blume C., Wang price S., Trudelle jackson E., Ortiz A. Comparison of eccentric and concentric exercise interventions in adults with subacromial impingement syndrome. Int J Sports Phys Ther. 2015;10(4):441–455. [PMC free article] [PubMed] [Google Scholar]
- 21.Granviken F., Vasseljen O. Home exercises and supervised exercises are similarly effective for people with subacromial impingement: a randomised trial. J Physiother. 2015;61(3):135–141. doi: 10.1016/j.jphys.2015.05.014. [DOI] [PubMed] [Google Scholar]
- 22.Moezy A., Sepehrifar S., Dodaran M.S. The effects of scapular stabilization based exercise therapy on pain, posture, flexibility and shoulder mobility in patients with shoulder impingement syndrome: a controlled randomized clinical trial. Med J Islam Repub Iran. 2014;28(87):1–15. [PMC free article] [PubMed] [Google Scholar]
- 23.Celik D., Akyuz G., Yeldan I. Comparison of the effects of two different exercise programs on pain in subacromial impingement syndrome. Acta Orthop Traumatol Turc. 2004;43(6):504–509. doi: 10.3944/AOTT.2009.504. [DOI] [PubMed] [Google Scholar]
- 24.Kromer T.O., Tautenhahn U.G., de Bie R.A., Staal J.B., Bastiaenen C.H. Effects of physiotherapy in patients with shoulder impingement syndrome: a systematic review of the literature. J Rehabil Med. 2009;41(11):870–880. doi: 10.2340/16501977-0453. [DOI] [PubMed] [Google Scholar]
- 25.Bang M.D. Comparison of supervised exercise with and without annual physical therapy for patients with shoulder impingement syndrome. J Orthop Sports Phys Ther. 2000;30(3):126–137. doi: 10.2519/jospt.2000.30.3.126. [DOI] [PubMed] [Google Scholar]
- 26.Rabini A., Piazzini D.B., Bertolini C. Effects of local microwave diathermy on shoulder pain and function in patients with rotator cuff tendinopathy in comparison to subacromial corticosteroid injections: a single-blind randomized trial. J Orthop Sports Phys Ther. 2012;42(4):363–370. doi: 10.2519/jospt.2012.3787. [DOI] [PubMed] [Google Scholar]
- 27.Brantingham J.W., Cassa T.K., Bonnefin D. Manipulative therapy for shoulder pain and disorders: expansion of a systematic review. J Manip Physiol Ther. 2011;34(5):314–346. doi: 10.1016/j.jmpt.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 28.Ginn K.A., Cohen M.L. Exercise therapy for shoul-der pain aimed at restoring neuromuscular control: a randomized comparative clinical trial. J Rehabil Med. 2005;37(2):115–122. doi: 10.1080/16501970410023443. [DOI] [PubMed] [Google Scholar]
- 29.Jain T.K., Sharma N.K. The effectiveness of physiotherapeutic interventions in treatment of frozen shoulder/adhesive capsulitis: a systematic review. J Back Musculoskelet Rehabil. 2014;27(3):247–273. doi: 10.3233/BMR-130443. [DOI] [PubMed] [Google Scholar]
- 30.Desmeules F., Boudreault J., Roy J.S., Dionne C.E., Frémont P., MacDermidg J.C. Efficacy of transcutaneous electrical nerve stimulation for rotator cuff tendinopathy: a systematic review. Physiotherapy. 2016;102(1):41–49. doi: 10.1016/j.physio.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 31.Lindsay D.M., Dearness J., McGinley C.C. Electrotherapy usage trends in private physiotherapy practice in Alberta. Physiother Can. 1995;47(1):30–34. [PubMed] [Google Scholar]
- 32.Chipchase L.S., Williams M.T., Robertson V.J. A national study of the availability and use of electrophysical agents by Australian Physiotherapists. Physiother Theory Pract. 2009;25(4):279–296. doi: 10.1080/09593980902782611. [DOI] [PubMed] [Google Scholar]
- 33.Yazmalar L., Sarıyıldız M.A., Batmaz İ. Efficiency of therapeutic ultrasound on pain, disability, anxiety, depression, sleep and quality of life in patients with subacromial impingement syndrome: a randomized controlled study. J Back Musculoskelet Rehabil. 2016 Nov 21;29(4):801–807. doi: 10.3233/BMR-160692. [DOI] [PubMed] [Google Scholar]
- 34.Fuentes J.P., Olivo S.A., Magee D.J., Gross D.P. Effectiveness of interferential current therapy in the management of musculoskeletal pain: a systematic review and meta-analysis. Phys Ther. 2010;90(9):1219–1238. doi: 10.2522/ptj.20090335. [DOI] [PubMed] [Google Scholar]
- 35.Quirk A.S., Newman R.J., Newman K.J. An evaluation of interferential therapy, shortwave diathermy and exercise in the treatment of osteoarthrosis of the knee. Physiotherapy. 1985;71(2):55–57. [Google Scholar]
- 36.Adedoyin R.A., Olaogun M.O., Fagbeja O.O. Effect of interferential current stimulation in management of osteoarthritic knee pain. Physiotherapy. 2002;88(8):493–499. [Google Scholar]
- 37.Cheing G.L., So E.M., Chao C.Y. Effectiveness of electroacupuncture and interferential electrotherapy in the management of frozen shoulder. J Rehabil Med. 2008;40(3):166–170. doi: 10.2340/16501977-0142. [DOI] [PubMed] [Google Scholar]
- 38.Almeida T.F., Roizenblatt S., Benedito-Silva A.A., Tufik S. The effect of combined therapy (ultrasound and interferential current) on pain and sleep in fibromyalgia. Pain. 2003;104(3):665–672. doi: 10.1016/S0304-3959(03)00139-8. [DOI] [PubMed] [Google Scholar]
- 39.Taylor K., Newton R.A., Personius W.J., Bush F.M. Effects of interferential current stimulation for treatment of subjects with recurrent jaw pain. Phys Ther. 1987;67(3):346–350. doi: 10.1093/ptj/67.3.346. [DOI] [PubMed] [Google Scholar]
- 40.Sluka K.A., Walsh D. Transcutaneous electrical nerve stimulation: basic science mechanism and clinical effectiveness. J Pain. 2003;4(3):109–121. doi: 10.1054/jpai.2003.434. [DOI] [PubMed] [Google Scholar]
- 41.Kocyigit F., Akalin E., Gezer N.S., Orbay O., Kocyigit A., Ada E. Functional magnetic resonance imaging of the effects of low frequency transcutaneous electrical nerve stimulation on central pain modulation: a double blind, placebo controlled trial. Clin J Pain. 2012;28(7):581–588. doi: 10.1097/AJP.0b013e31823c2bd7. [DOI] [PubMed] [Google Scholar]
- 42.Shehab D., Adham N. Comparative effectiveness of ultrasound and transcutaneous electrical stimulation in treatment of periarticular shoulder pain. Physiother Can. 2000;52(3):208–214. [Google Scholar]
- 43.Herrera-Lasso I., Mobarak L., Fernandez-Dominguez L., Cardiel M.H., Alarcon-Segovia D. Comparative effectiveness of packages of treatment including ultrasound or transcutaneous electrical nerve stimulation in painful shoulder syndrome. Physiotherapy. 1993;79(4):251–253. [Google Scholar]