Abstract
Osteochondromas (OC) are the most common benign tumors of the bones. They are most frequently found near the knee joint and are typically asymptomatic. The presence of OC near the hip joint is rare. In addition, OC is an extremely uncommon cause of sciatica. We present a rare case of OC of the proximal femur. The patient presented with left hip pain and manifestations of sciatic nerve compression. Surgical excision was performed. The diagnosis was confirmed postoperatively by histopathology.
Osteochondromas (OC) are hamartomatous proliferations of both bone and cartilage that are thought to arise from trapped growth-plate cartilage, extend through the cortex, and grow via endochondral ossification beneath the periosteum.1 This process of OC development may explain the tendency of OC to involve long bones, such as the distal femur, the proximal tibia, and the proximal humerus.2 Typically, OC arise within the first three decades of life and affect children and adolescents. The majority of OC are asymptomatic and are found incidentally.3,4 The main purpose of this study is to illustrate a rare cause of sciatic nerve compression and how this compression was treated.
CASE
A 25-year-old female not known to have any medical illness presented to our clinic complaining of left hip and buttock pain, limitation of left hip joint movement, numbness and mild tingling in the plantar and dorsal aspects of the left foot and a palpable mass in the posterior aspect of the left thigh for the prior 6 months. Examination of the patient revealed an immobile mass measuring approximately 10 cm×6 cm in the left buttock, left hip flexion limited to 60° due to pain, and weakness of both ankle plantar flexion and dorsiflexion. Radiographs of the left hip revealed a pedunculated osseous mass measuring approximately 7.5 cm×6 cm attached to the posteromedial aspect of the femoral neck just above the lesser trochanter (Figures 1–3).
Figure 1.
Preoperative anteroposterior (AP) radiograph of the left hip reveals an osteochondroma (OC) projected over the proximal femur.
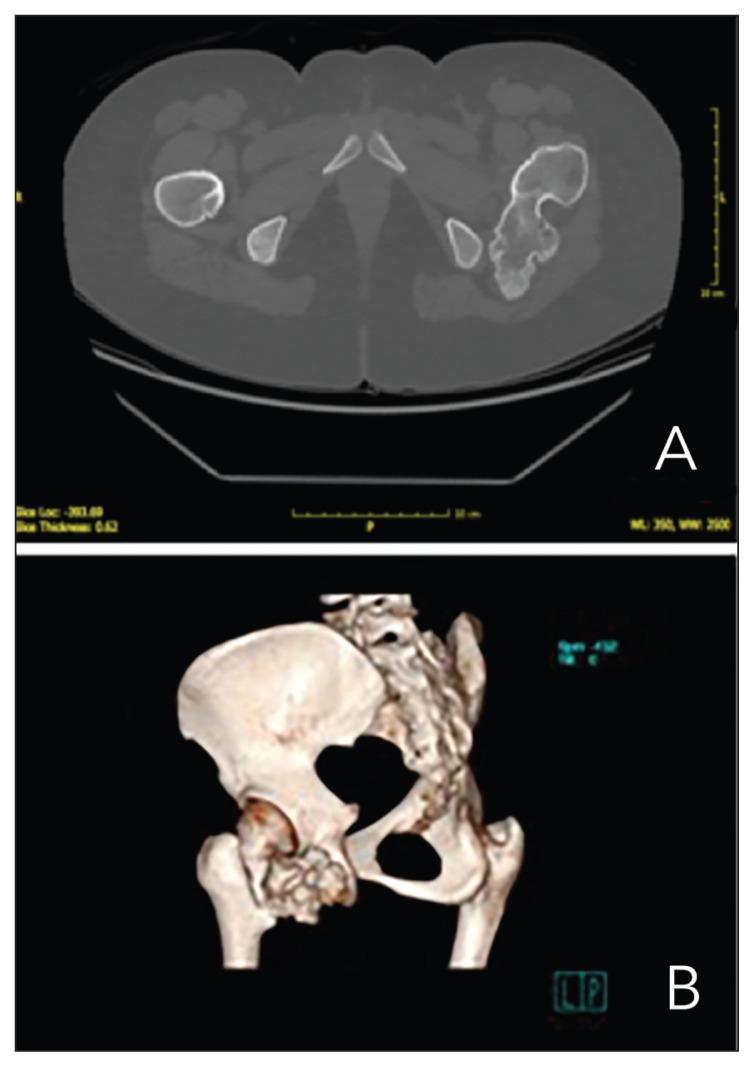
Figure 2.
Computed tomography (CT) scan, axial cut . Three-dimensional (3D) CT.
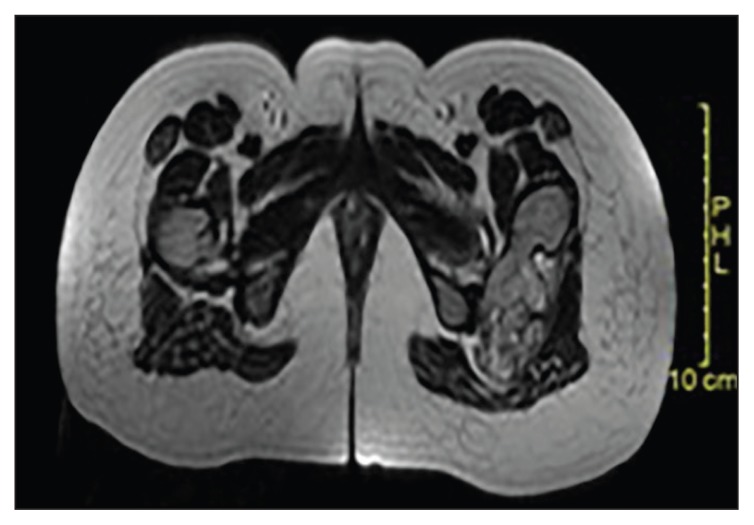
Figure 3.
Magnetic resonance imaging (MRI) of the hip confirmed that the mass was an OC with a cartilaginous cap of less than 1 cm. Adjacent soft tissue compression without extension or malignant degeneration was evident.
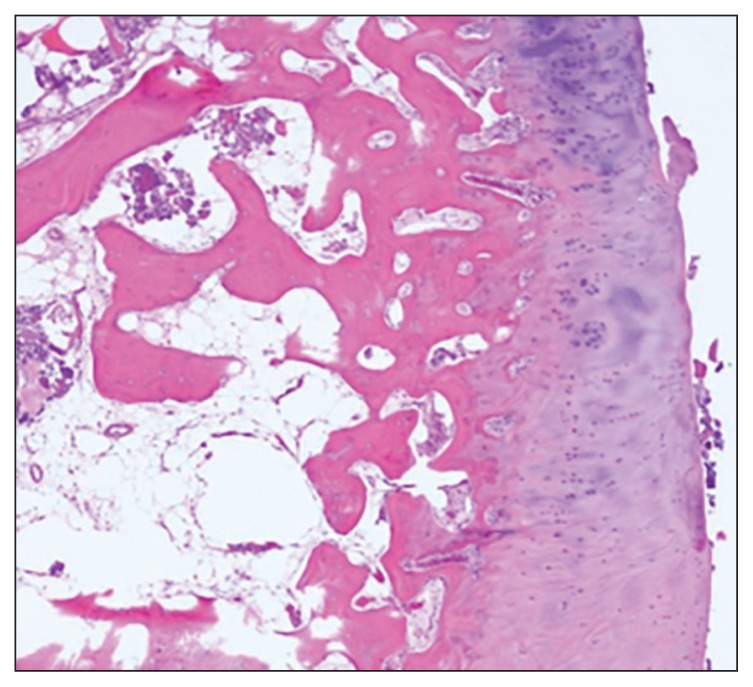
The mass was excised through a posterior approach with the patient in the right lateral decubitus position, as described by Yu et al.5 The sciatic nerve was dissected and isolated from the OC. An osteotome was used to excise the tumor (Figure 4). The femoral neck was examined intraoperatively, and there were no cracks or defects to be fixed. A histopathological report indicated that the tumor was an OC with a cartilaginous cap of less than 1 cm (Figure 5). Postoperatively, the patient reported improvement in numbness and tingling sensation in the foot, but continued to experience mild buttock pain. At 10-month follow-up, the patient had full resolution of the sensory and motor function of the sciatic nerve. Radiographs of the hip revealed no evidence of heterotrophic ossification or avascular necrosis of the hip Figure 6.
Figure 4.
Intraoperative photograph notable for the multifaceted cartilaginous cap of the OC.
Figure 5.
Decalcified haematoxylin-eosin stained section of the cartilaginous cap that demonstrates the paucicellular matrix of the cap (bar=1000 microns).
Figure 6.
X-ray at 10-month follow-up revealing no evidence of AVN or recurrence of the lesion.
DISCUSSION
Differential diagnosis for sciatic nerve compression in non-traumatic young adult patients may be divided into intraspinal and extraspinal categories of anatomical etiology.6 Lumbar disk herniation and spinal stenosis are the most common causes of this compression. Piriformis syndrome is an example of an extraspinal cause of sciatica.7 A pelvic bone tumor such as an OC is another example of an extraspinal pathology.5 Other relatively uncommon causes of sciatic nerve compression include vascular malformations, infectious diseases,5 hereditary multiple exostoses,8 and tumors of the bone and soft tissue.9–11
Typically, spinal causes of sciatic nerve compression are associated with a history of low back pain and lifting heavy objects and exacerbated by bending, axial loading, or sitting. Piriformis syndrome, which occurs due to hypertrophy of the piriformis muscle that compresses the sciatic nerve, presents with signs and symptoms of sciatica that are exacerbated by activity, prolonged sitting, or walking. The diagnosis of piriformis syndrome is clinical and is a diagnosis of exclusion.7 Myositis ossificans, which typically occurs after a traumatic event or neurological insult, can be differentiated by radiographic characteristics such as mature circumferential calcification, immature radiolucent centers, and radiolucent clefts that separate the abnormal ossification from the cortex of the adjacent bone.12
One of the most important differential diagnoses that should be excluded is a secondary chondrosarcoma that arises from a solitary OC, particularly near the pelvis. In this study, computed tomography (CT) and magnetic resonance imaging (MRI) revealed no cortical destruction and no bone marrow involvement, respectively. Histologically, the cartilaginous cap was less than 1 cm. Given these findings, secondary chondrosarcoma was unlikely.13
Yu et al5 and Turan Ilica et al14 reported cases of femoral neck OC involving a 39-year-old man and a 34-year-old man, respectively. CT and MRI were used to determine the size, origin, and extent of each OC and plan strategies for surgery.14 In these cases, similarly to our described case, the patients demonstrated signs of sciatic nerve compression, including weakness of toe and ankle dorsiflexion and a diminished Achilles tendon reflex. As observed using CT and MRI, the OC in the currently described case had a sessile structure and extended broadly outward in the region of the lesser trochanter.
Despite the similar diagnoses in the case presented by Yu et al5 and our case, the former case was treated with prophylactic internal fixation, whereas our case was successfully treated without prophylactic fixation. Prophylactic fixation of the femoral neck after the excision of a large OC is not mandatory and depends on the presence of a defect in the femur neck, such as a cyst, a fissure, or another defect. Although we took fixation into consideration during preoperative planning, we preferred to keep the patient on partial weight bearing for six weeks and then allow for full weight bearing.
Based on our case, OC should be considered a potential, though extremely rare, extraspinal cause of sciatic nerve compression. An OC can be treated surgically with good results and high patient satisfaction. In addition, the use of prophylactic internal fixation is not mandatory.
Footnotes
SIMILAR CASES PUBLISHED: 1
REFERENCES
- 1.Rains HA, Mann CV. Tumours of bones and joints. In: Baily H, Rains AJH, Mann CV, McNeill Love RJ, editors. Bailey and Love’s short practice of surgery. 20th ed. London: HK Lewis; 1988. pp. 372–9. [Google Scholar]
- 2.Panagiotis K, Vassiliki G, Kalliopi S, Georgios P, Georgios K, Niki A, et al. Osteochondromas: review of the clinical, radiological and pathological features. In Vivo. 2008;(5):633–46. [PubMed] [Google Scholar]
- 3.Giudici MA, Moser RP, Jr, Kransdorf MJ. Cartilaginous bone tumors. Radiol Clin North Am. 1993;31(2):237–59. [PubMed] [Google Scholar]
- 4.Scarborough MT, Moreau G. Benign cartilage tumors. Orthop Clin North Am. 1996;27(3):583–9. [PubMed] [Google Scholar]
- 5.Yu K, John P, Anto F, Amir A. Osteochodroma of femoral neck: a rare cause of sicatic nerve compression. Orthopedics. 2010;33(8) doi: 10.3928/01477447-20100625-26. [DOI] [PubMed] [Google Scholar]
- 6.Kulcu DG, Naderi S. Differential diagnosis of intraspinal and extraspinal non-discogenic sciatica. J Clinneurosci. 2008;15(11):1246–52. doi: 10.1016/j.jocn.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 7.Kirschner JS, Foye PM, Cole JL. Piriformis syndrome, diagnosis and treatment. Muscle Nerve. 2009;40(1):10–8. doi: 10.1002/mus.21318. [DOI] [PubMed] [Google Scholar]
- 8.Paik NJ, Han TR, Lim SJ. Multiple peripheral nerve compressions related to malignantly transformed hereditary multiple exostoses. Muscle Nerve. 2000;23(8):1290–4. doi: 10.1002/1097-4598(200008)23:8<1290::aid-mus23>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 9.Bickels J, Kahanovitz N, Rubert CK, Henshaw RM, Moss DP, Meller I, et al. Extraspinal bone and soft-tissue tumors as a cause of sciatica. Clinical diagnosis and recommendations: analysis of 32 cases. Spine. 1999;24(15):1611–6. doi: 10.1097/00007632-199908010-00017. [DOI] [PubMed] [Google Scholar]
- 10.Zonenshayn M, Edgar MA, Lavyne MH. Removal of a lumbar melanotic schwannoma via the far-lateral approach in a patient with Carney complex. Case report. J Neurosurg. 2000;92(2 Suppl):241–5. doi: 10.3171/spi.2000.92.2.0241. [DOI] [PubMed] [Google Scholar]
- 11.Lin PP, Moussallem CD, Deavers MT. Secondary chondrosarcoma. J Am Acad Ortho Surg. 2010;18(10):608–15. doi: 10.5435/00124635-201010000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Kransdorf MJ, Meis JM. From the archives of the AFIP. Extraskeletal osseous and cartilaginous tumors of the extremities. Radiographics. 1993;13(4):853–84. doi: 10.1148/radiographics.13.4.8356273. [DOI] [PubMed] [Google Scholar]
- 13.Siebenrock KA, Ganz R. Osteochondroma of the femoral neck. Clin Orthop Relat Res. 2002;394(394):211–8. doi: 10.1097/00003086-200201000-00025. [DOI] [PubMed] [Google Scholar]
- 14.Turan Ilica A, Yasar E, Tuba Sanal H, Duran C, Guvenc I. Sciatic nerve compression due to femoral neck osteochondroma: MDCT and MR findings. Clin Rheumatol. 2008;27(3):403–4. doi: 10.1007/s10067-007-0761-4. [DOI] [PubMed] [Google Scholar]