Abstract
BACKGROUND
Previous studies have demonstrated that asthma might be associated with an increase in cardiovascular disease (CVD) and death. However, this relationship differs by gender.
OBJECTIVES
To systematically evaluate the association of asthma on the incidence of CVD and death in cohort studies.
DESIGN
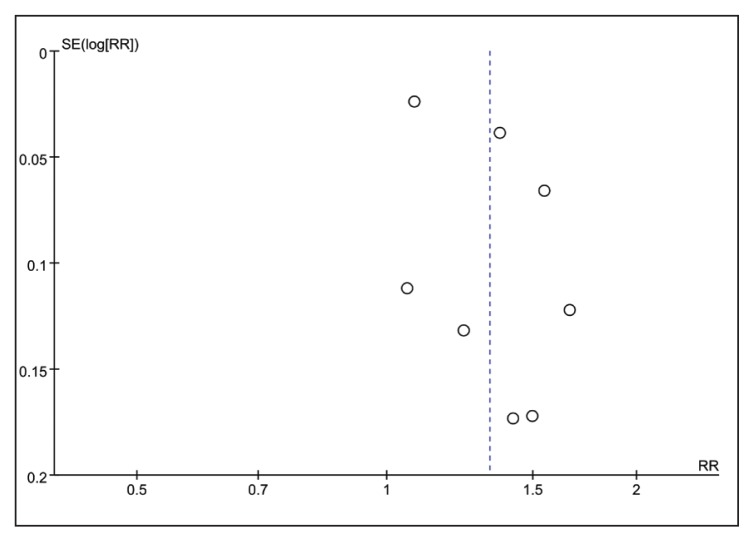
Fixed and random effects models were used to calculate risk estimates in a meta-analysis. Potential publication bias was calculated using a funnel plot, Begg’s rank correlation test, and Egger’s linear regression test.
SEARCH STRATEGY
We searched the PubMed and Embase databases for studies that examined the relationship between asthma and CVD or all-cause mortality.
SELECTION CRITERIA
Prospective and retrospective cohort studies.
RESULTS
Ten studies containing 406 426 participants were included. The summary relative risk (95% confidence interval, CI) for patients with asthma was 1.33 (95% CI: 1.15–1.53), for CVD in women, it was 1.55 (95% CI: 1.20–2.00), for CVD in men it was 1.20 (95% CI: 0.92–1.56), and for all-cause mortality in both genders it was 1.36 (95% CI: 1.01–1.83). These findings remained consistent after sensitivity analysis.
CONCLUSION
The results indicate that asthma was associated with an increased risk of CVD and all-cause mortality.
Asthma is a global health problem that is increasing worldwide and affects people of all ages. The main characteristics of asthma include hyper-responsiveness of the airway to stimuli and reversible airflow obstruction. Typical symptoms of asthma include chest tightness, breathlessness, recurrent episodes of wheezing, and coughing that changes in intensity over time.1 Asthma is a heterogeneous disease that is usually characterized by chronic airway inflammation.2 It is also associated with chronic systemic inflammatory diseases beyond the airways.3,4 Several studies have demonstrated that inflammatory processes are likely participants in the pathophysiology of asthma, atherosclerosis and endothelial dysfunction.5–7 Besides, our knowledge of the involvement and interaction of coagulation, anticoagulant pathways, the fibrinolytic system, and platelets in the pathophysiology of asthma has increased considerably.7 Therefore, various studies have already demonstrated that asthma is related to an increased incidence of cardiovascular disease (CVD).8–10 Recently, several large cohort studies were published that provide more evidence that asthmatic individuals have a higher CVD event rates and an increased risk of death than non-asthmatics.9,11,12 However, there were discrepancies within the findings on the role of age and gender in the relationship between asthma and the risk of CVD.13–15 These discrepancies encouraged us to study the relationships in depth.
The burden of CVD events and all-cause deaths has considerably increased concerns about the absolute number of susceptible asthma patients around the world. To our knowledge, there have been no systematic evaluations nor meta-analyses on the association of asthma and the incidence of cardiovascular events or concerning asthma prognosis. Therefore, we systematically reviewed studies on the relationship between asthma and CVD or all-cause mortality and performed a meta-analysis.
METHODS
The Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines were used to perform the meta-analysis.16
Search strategy
We performed a systematic search in June of 2015 using PubMed and Embase databases. We searched searched for published articles that examined the association between asthma and the risk of CVD, coronary heart disease (CHD), stroke, and death or all-cause mortality. The following search terms were used: 1) asthma, bronchial asthma, allergic airway inflammation, 2) coronary artery disease, CHD, coronary arteriosclerosis disease, CVD, cerebrovascular disease, peripheral vessel disease, stroke, and 3) prospective cohort and retrospective cohort study. Reference lists, conference abstracts, and bibliographies of pertinent articles were searched and reviewed. The literature search was limited to the English language.
Selection criteria
Two investigators independently evaluated the eligibility of the studies that had been retrieved from the databases on the basis of predetermined selection criteria. After an initial review, studies were included if they satisfied the following criteria: (1) a cohort study design (2) the exposure of interest was asthma; (3) the outcomes were CVD, CHD, stroke, death, or all-cause mortality; (4) the relative risk (RR), or equivalent ratio-type indices, for instance, hazard ratio (HR), odds ratio (OR) and the corresponding 95% confidence intervals (CIs), or the event numbers in each category were reported; (5) in cases where multiple reports covered the same cohort study data, only the study containing the larger sample size and more detailed outcomes was selected to avoid analysis of overlapping data; (6) studies were included if they satisfied six or more Newcastle-Ottawa Scale (NOS) criteria, as recommended by the Cochrane Non-Randomized Studies Methods Working Group.17
Data extraction
Two reviewers independently extracted the data using a standardized data extraction form. Any differences of opinion about the inclusion of studies or interpretations of data were resolved through an internal discussion among the reviewers. The following characteristics were recorded for the identified studies: name of the first author, year of publication, country of publication, length of follow-up in years, study design, ascertainment of asthma, assessments of outcomes, the ages, characteristics, and total number of participants, outcome numbers of CVD events and incidences of all-cause mortality, and statistical adjustments for potential confounding factors.
Outcome measures
The definition of CVD includes CHD, stroke, peripheral vessel disease, coronary artery disease, cerebrovascular disease and coronary arteriosclerosis disease. All-cause mortality is defined as death for any reason, including but not limited to stroke, heart failure, sudden death, arrhythmia, malignant tumor, or myocardial infarction.
Quality assessment
A quality assessment was performed for the cohort studies in this meta-analysis using the NOS criteria. These studies were judged using three broad perspectives on the basis of the NOS: selection of the study groups (four items, one star each), comparability of the study groups (one item, up to two stars), and attaining the outcome of interest (three items, one star each). Given the variable quality of observational studies, studies were considered high quality if they satisfied six or more NOS criteria.
Statistical analyses
We used adjusted relative risks (RRs) and 95% confidence intervals (CIs) as measures for the link between asthma and CVD events and all-cause mortality. If multivariate RRs were provided, they were used for statistical analyses and preferred over univariate RRs. Before pooling the data, we converted the adjusted RRs from each study to their log for variance stabilization and to normalize the distribution. A RR>1 reflected an increased risk in patients with asthma as compared to subjects without asthma, or it indicated a higher mortality rate.
A test for heterogeneity was used to assess between-study variability.18 Tests were conducted using the Cochrane Q statistic (P<.10 as the significance level) and I2 statistic. A value of I2<50% meant that “heterogeneity might be acceptable” and I2>75% indicated “considerable heterogeneity”, based on the suggestions of the Cochrane Handbook for Systematic Reviews of Interventions.19 Moreover, if the I2≤50%, the Mantel-Haenszel fixed-effect model was used to calculate the RRs. If I2>50%, the DerSimonian and Laird random-effect model was applied to obtain the RRs.
Potential publication bias was estimated using a funnel plot. Asymmetric funnel plots were assessed using Begg’s rank correlation test and Egger’s linear regression test (P<.10 was considered statistically significant).20 We also performed further analyses to examine potential sources of heterogeneity by evaluating the incidence of CVD risk in male or female asthmatic patients. Sensitivity analyses were additionally used to examine the influence of a single study on the overall risk estimate. These analyses were carried out by sequentially omitting one study each time.
All statistical analyses were performed using Review Manager (version 5.2 for Windows, Cochrane Collaboration, Oxford, UK, 2008).
RESULTS
Literature search
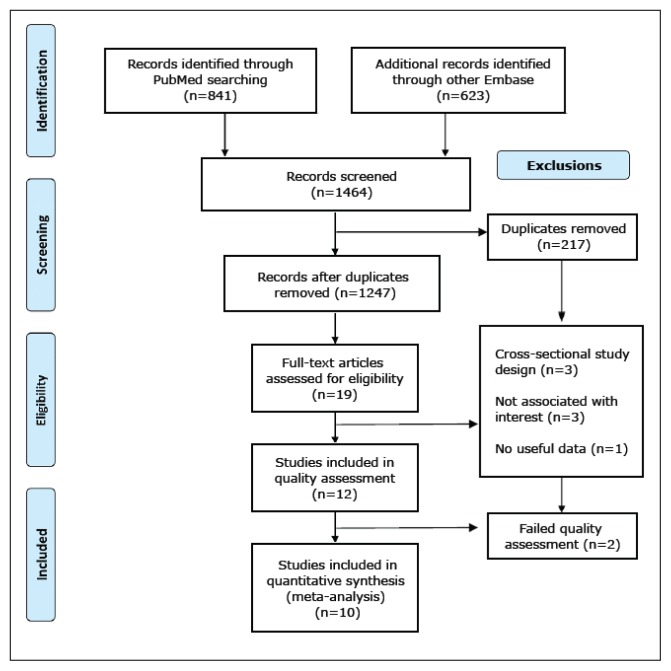
Our search strategy generated a total of 1464 citations: 841 from PubMed, and 623 from Embase. After screening the titles or abstracts, the majority of articles were excluded, largely because they were reviews, duplicate articles, case-control studies, cross-sectional studies, or not relevant to our topic. After these exclusions, 19 articles remained (Figure 1). Nine articles were then excluded for various reasons after further reviewing the full texts. Of these nine, three studies were excluded because the design was cross-sectional. An additional three articles were excluded because they did not evaluate the association of interest. Another article was excluded because it did not provide useful data. Finally, two articles were excluded as a result of low quality assessment scores. This left a total of ten eligible studies3,9–15,21,22 for the meta-analysis.
Figure 1.
Flow chart of study selection process.
Characteristics and quality assessment
The characteristics of the studies that were included are summarized in Table 1. These studies were published between 2004 and 2015. Five studies were conducted in the USA, three were conducted in Europe and two were conducted in Taiwan. Four studies were retrospective cohort studies and six studies were prospective studies. The length of follow-up ranged from 4.5 to 27 years. The sample sizes of the cohorts ranged from 1233 to 151 620 (a total of 406 426). The ascertainment of asthma varied among studies: eight studies were based on self-reported doctor diagnoses or inpatient admission for asthma, one used a respiratory questionnaire and one was from an epidemiology project. Among the ten studies, seven reported CVD events, six reported CHD events, four reported stroke events, and four reported all-cause deaths. All studies were adjusted for age with the exception of one study. Some studies identified and adjusted for conventional risk factors, including race/centre,9,13–15,21 education,10,13,21 body mass index,9,13,21 smoking habits,9–11,13,15,22 alcohol consumption,10,12,13 blood pressure levels,11–13,21 cholesterol levels9,10,13,15,21 and diagnosis of diabetes.3,9–11,13,15,21 Four studies reported that the risk of CVD was different in male and female asthmatic individuals.10,11,13,21 With the use of the NOS, ten studies3,9–15,21,22 were classified as high quality as they satisfied more than six NOS criteria. The NOS checklists are listed in Table 2.
Table 1.
Baseline characteristics of the ten cohort studies of asthma and cardiovascular diseases and all-cause mortality.
| First author, year | Location | Study design | Participant | Age | CVD event | Assessment of asthma | Duration (years) | Adjustment for covariates |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Iribarren, 200413 | USA | Retrospective | M 70047 W 81573 |
18–85 | CHD | Self-reported doctor diagnosis or inpatient admission for asthma | 27 | Age, race/ethnicity, education level, smoking status, alcohol consumption, BMI, TC, WBC, HTN, diabetes, parental history of CHD, and occupational exposures |
| Marco, 200514 | Italy | Prospective | 6031 | 20–44 | CVD and all-cause mortality | Self-reported doctor diagnosis | 7 | Age, sex and centre |
| Schanen, 200515 | USA | Prospective | 13501 | 45–64 | CVD | Self-reported doctor diagnosis | 14 | Age, sex, race/centre, HDL-C, LDL-C, SBP, hypertension medication use, smoking status, pack years, W/H ratio, diabetes diagnosis, sport score |
| Bellia, 200722 | Italy | Prospective | 1233 | ≥65 | CVD and all-cause mortality | Respiratory questionnaire | 5 | Smoking, comorbidity, and underweight |
| Onufrak, 200821 | USA | Prospective | 14567 | 45–64 | CVD | Self-reported doctor diagnosis | 13 | Age, BMI, black race, diabetes, HTN, education level, LDL-C, HDL-C, physical activity |
| Hyun, 20123 | USA | Retrospective | 7176 | - | CHD | Rochester epidemiology project | Asthma 7 Non-asthma 5–8 |
Race, diabetes, RA and IBD |
| Chung (ACS), 201412 | Taiwan | Retrospective | 38840 | ≥18 | ACS | Physicians | 16 | Age, sex, HTN, diabetes, hyperlipidemia, Stroke, heart failure, COPD and smoking |
| Chung (Stroke), 201411 | Taiwan | Retrospective | 72587 | ≥18 | Stroke | Physicians | Asthma 7.21 Non-asthma 7.35 |
Age, sex, AF, HTN, hyperlipidemia, heart failure, alcoholism, obesity, COPD, DVT, CAD |
| Matthew, 20159 | USA | Prospective | 6792 | 62 | CVD and all-cause mortality | Self-reported doctor diagnosis | 5 | Age, race, sex, TC, HDL-C, SBP, smoking, diabetes, antihypertensive and lipid-lowering medication used at baseline, BMI, family history of CVD, income |
| Yunus, 201510 | Denmark | Prospective | 94079 | 20–100 | CVD and all-cause mortality | Self-reported doctor diagnosis | 4.5 | Age, BMI, physical activity in leisure-time, education, income, alcohol consumption, smoking, SBP, DBP, TC, LDL-C, HDL-C, TG, diabetes, use of cholesterol-lowing medication, presence of diabetes |
BMI:body mass index; TC: total cholesterol; WBC: white blood cell; HTN: hypertension; CHD: coronary heart disease; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; SBP: systolic blood pressure; RA: rheumatoid arthritis; IBD: inflammatory bowel disease; COPD: chronic obstructive pulmonary disease; DVT: deep vein thrombosis; CAD: coronary artery disease;
Table 2.
Study quality of included studies based on the Newcastle-Ottawa scale.
| Author | Represent activeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Comparability of cohorts on the basis of the design or analysis | Ascertainment of outcome | Was follow-up long enough for outcomes to occur | Adequacy of follow up of cohort | Total scores |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Iribarren, 2004 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ★ | 9 |
| Marco, 2005 | ★ | ★ | ★ | ⋆ | ★⋆ | ★ | ★ | ★ | 7 |
| Schanen, 2005 | ★ | ★ | ★ | ⋆ | ★★ | ★ | ★ | ★ | 8 |
| Bellia, 2007 | ★ | ★ | ★ | ⋆ | ★⋆ | ★ | ★ | ★ | 7 |
| Onufrak, 2008 | ★ | ★ | ★ | ⋆ | ★★ | ★ | ★ | ⋆ | 7 |
| Hyun, 2012 | ★ | ★ | ★ | ★ | ★⋆ | ★ | ★ | ★ | 8 |
| Chung(ACS), 2014 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ⋆ | 8 |
| Chung(Stroke)m 2014 | ★ | ★ | ★ | ★ | ★★ | ★ | ★ | ⋆ | 8 |
| Matthew, 2015 | ★ | ★ | ★ | ⋆ | ★★ | ★ | ★ | ★ | 8 |
| Yunus, 2015 | ★ | ★ | ★ | ⋆ | ★★ | ★ | ★ | ★ | 8 |
See quality assessment in methods for explanation of ratings.
Primary results of the meta-analysis
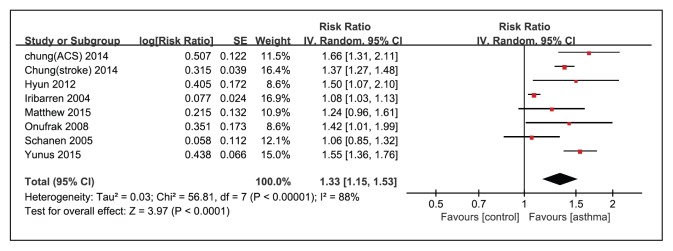
Eight cohort studies3,9–13,15,21 were included in the meta-analysis linking asthma with the risk of CVD. Figure 2 shows the results from the random effects model and combines RRs for CVD. Across eight studies, six studies reported a positive association between asthma and CVD events (RRs ranged from 1.08 to 1.66). Overall, subjects with asthma experienced a remarkably increased risk of CVD events (RR: 1.33; [95% CI: 1.15–1.53]; P<.0001) as compared to the reference group (Figure 2). However, heterogeneity was large (I2=88%, P<.00001).
Figure 2.
Forest plot for random-effect analysis of the association between asthma and cardiovascular diseases for eight studies.
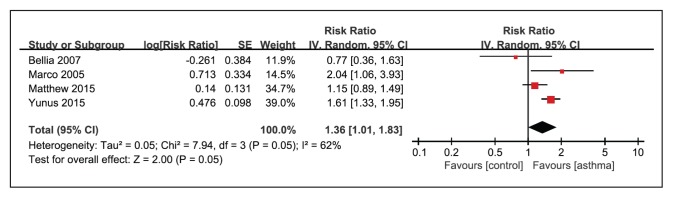
Asthma was associated with an increased risk of all-cause mortality in a random effects model as compared to reference subjects without asthma (RR 1.36; [95% CI: 1.01–1.83]; P=.05) (Figure 3). However, there were incidences of substantial heterogeneity between studies (I2=62%; P=.05).
Figure 3.
Forest plot for random-effect analysis of the association between asthma and all-cause mortality from four studies.
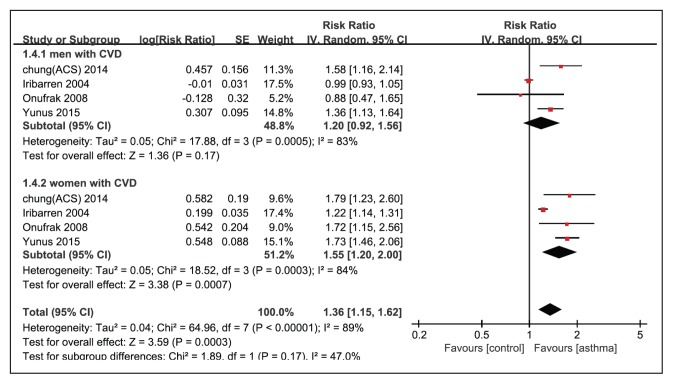
We further explored whether there were different effects on the incidence of CVD between male and female asthmatic patients using a random effects model. Women with asthma had a significantly higher risk of CVD as compared to the reference group (RR: 1.55; I2=84%; [95% CI: 1.20–2.00]; P=.0007), whereas no significant association was found in men (RR: 1.20; I2=83%; [95% CI: 0.92–1.56]; P=.17). However, the combined RR value was 1.36 ([95% CI: 1.15–1.62]; P=.0003). To further explore the interaction between gender and asthma on CVD risk, the “Test for subgroup differences” at the bottom of Figure 4 were examined and gave a P=.17, which suggested that the influence of gender on the association between asthma and CVD risk was not statistically significant. Therefore, we cannot confirm or refute a significant difference in the incidence of CVD between male and female asthmatic patients.
Figure 4.
Forest plot for random-effect analysis of association between cardiovascular diseases and men and women with asthma.
Sensitivity analyses
We evaluated the risk estimates for asthma and risk of CVD for the remaining studies by omitting one study each time. This produced a RR value with a range from 1.29 ([95% CI: 1.12–1.49]; P<.001) to 1.39 ([95% CI: 1.26 –1.54; P<.001) which did not alter the overall combined RRs.
Publication bias
Publication bias was assessed among studies concerning asthma and CVD risk using a funnel plot (Figure 5). The funnel plot appeared asymmetric, but was difficult to interpret because of the small number of studies. To further examine the publication bias, we used Begg’s rank correlation test and Egger’s linear regression, which indicated no evidence of publication bias (Begg’s, P=1.000; Egger’s linear regression, P=.150).
Figure 5.
Funnel plot to examine publication bias in eight studies.
DISCUSSION
This meta-analysis concludes that there is an association between asthma and an increased risk of CVD and all-cause mortality. Further subgroup analyses showed that women with asthma experienced a higher risk of CVD than men with asthma. Importantly, asthmatics of both genders had a high risk for all-cause mortality.
There have been numerous studies on the etiology of asthma and CVD events. Chronic inflammatory disease is considered a link between asthma and the onset of increased CVD. Chronic airway inflammation might contribute to systemic inflammation and increase vulnerability to vascular diseases. Established inflammatory biomarkers are increased in atherogenesis, such as high-sensitivity C-reactive protein (Hs-CRP), interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-a), interleukin-8 (IL-8), and fibrinogen, which are also known to be elevated in asthmatics.23,24 One possible theory is that asthmatic patients display signs of enhanced coagulation activation in their airways, impaired functions of the anticoagulant protein C system, attenuated fibrinolysis, and increased platelet activation.7 Moreover, it was clearly demonstrated that allergic asthma accelerated atherosclerosis by adjusting the balance of effector T cells and regulatory T-cells in apolipoprotein E deficient mice, which is associated with an increase in Th2 and Th17 cells but not Th1 cells.25 Medicines used in the treatment of asthma, such as beta-adrenoceptor agonists and oral or inhale glucocorticoids, could increase the occurrence of CVD events.26,27
Our findings demonstrate that asthma was uniformly associated with an increased overall risk of CVD. Further analysis indicates that gender might influence the impact of asthma on CVD risk. Combined with previous findings, the data indicate a positive association between asthma and the incidence of CVD that varies according to several factors including gender, smoking status, asthma severity, and age of the onset of asthma. Further analysis is needed to understand why asthmatic women might be at a higher risk than asthmatic men for CVD. Perhaps women engage in less physical activity, have more weight gain, obesity and metabolic disorders.
Another study of a large multiethnic cohort found that persistent asthmatics had a higher CVD event rate compared to intermittent and non-asthmatics.9 In a study conducted by Bellia et al, asthma was associated with a higher mortality rate in the elderly, but it was not an independent risk factor.22 After systematically analyzing four studies in our investigation, the results indicate that asthma was an increased risk factor for all-cause mortality.9,10,14,22
Given differences in asthma treatments, patient characteristics, the definitions of asthma, the varying severity of asthma, the age and gender of subjects, we observed substantial heterogeneities in the relationship between asthma and CVD.
The greatest strength of our analysis is that we used cohort studies, six of which were prospective. They were highly effective evidence-based studies with large sample sizes. Assessments about asthma were reasonable and probably accurate. Consequently, our results accurately represent the association between asthma, CVD incidences, and all causes of death.
There are several potential limitations in our meta-analysis. First, we only selected studies published in English, which could lead to selection bias. Second, significant heterogeneity was detected although sensitivity analyses indicated that the conclusions were unaffected by the heterogeneity. Otherwise, heterogeneity could have led to overestimating or underestimating the association of asthma on CVD events. Third, we could not conduct further analyses using factors like age, body mass index, smoking, and asthma treatments, because of insufficient data. Also, publication bias is difficult to show conclusively by funnel plot when the number of studies is small.
In summary, this meta-analysis provided strong evidence that asthma is significantly associated with future cardiovascular risk among asthmatic patients. Furthermore, asthmatics have an increased risk of all-cause mortality. These data indicate a need for early detection and intervention during general outpatient visits in asthmatics who may have potential CVD complications or mortality.
Footnotes
Conflict of interest
The authors declared no conflicts of interest.
SYSTEMATIC REVIEW REGISTRATION NUMBER: Systematic review was not registered.
REFERENCES
- 1.FitzGerald JM, Reddel HK, Bateman ED, et al. Global Strategy for Asthma Management and Prevention (2015 update) 2015 Global initiative for asthma [Internet] 2015. Available from: www.ginashma.org.
- 2.Pin I, Gibson P, Kolendowicz R, et al. Use of induced sputum cell counts to investigate airway inflammation in asthma. Thorax. 1992;47:25–9. doi: 10.1136/thx.47.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yun HD, Knoebel E, Fenta Y, et al. Asthma and proinflammatory conditions: a population-based retrospective matched cohort study. Mayo Clin Proc. 2012;87:953–60. doi: 10.1016/j.mayocp.2012.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fenta YA, Tello N, Jung JA, et al. Inflammatory bowel disease and asthma: A population?based, case?control study. Inflammatory bowel diseases. 2010;16:1957–62. doi: 10.1002/ibd.21277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yildiz P, Oflaz H, Cine N, et al. Endothelial dysfunction in patients with asthma: the role of polymorphisms of ACE and endothelial NOS genes. Journal of Asthma. 2004;41:159–66. doi: 10.1081/jas-120026073. [DOI] [PubMed] [Google Scholar]
- 6.Onufrak S, Abramson J, Vaccarino V. Adult-onset asthma is associated with increased carotid atherosclerosis among women in the Atherosclerosis Risk in Communities (ARIC) study. Atherosclerosis. 2007;195:129–37. doi: 10.1016/j.atherosclerosis.2006.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Boer JD, Majoor CJ, van’t Veer C, et al. Asthma and coagulation. Blood. 2012;119:3236–44. doi: 10.1182/blood-2011-11-391532. [DOI] [PubMed] [Google Scholar]
- 8.Prosser R, Carleton B, Smith A. The comorbidity burden of the treated asthma patient population in British Columbia. Chronic Diseases and Injuries in Canada. 2010;30 [PubMed] [Google Scholar]
- 9.Tattersall MC, Guo M, Korcarz CE, et al. Asthma Predicts Cardiovascular Disease Events The Multi-Ethnic Study of Atherosclerosis. Arteriosclerosis, thrombosis, and vascular biology. 2015;35:1520–5. doi: 10.1161/ATVBAHA.115.305452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Çolak Y, Afzal S, Nordestgaard BG, Lange P. Characteristics and Prognosis of Never Smokers and Smokers with Asthma in the Copenhagen General Population Study: a Prospective Cohort Study. Am J Respir Crit Care Med. 2015;192:172–81. doi: 10.1164/rccm.201502-0302OC. [DOI] [PubMed] [Google Scholar]
- 11.Chung WS, Shen TC, Lin CL, et al. Adult asthmatics increase the risk of acute coronary syndrome: A nationwide population-based cohort study. Eur J Intern Med. 2014;25:941–5. doi: 10.1016/j.ejim.2014.10.023. [DOI] [PubMed] [Google Scholar]
- 12.Chung WS, Lin CL, Chen YF, et al. Increased stroke risk among adult asthmatic patients. Eur J Clin Invest. 2014;44:1025–33. doi: 10.1111/eci.12336. [DOI] [PubMed] [Google Scholar]
- 13.Iribarren C. Are patients with asthma at increased risk of coronary heart disease? International Journal of Epidemiology. 2004;33:743–8. doi: 10.1093/ije/dyh081. [DOI] [PubMed] [Google Scholar]
- 14.de Marco R, Locatelli F, Cazzoletti L, et al. Incidence of asthma and mortality in a cohort of young adults: a 7-year prospective study. Respir Res. 2005;6:95. doi: 10.1186/1465-9921-6-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schanen JG, Iribarren C, Shahar E, et al. Asthma and incident cardiovascular disease: the Atherosclerosis Risk in Communities Study. Thorax. 2005;60:633–8. doi: 10.1136/thx.2004.026484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Jama. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 17.Wells G, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000 [Google Scholar]
- 18.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ: British Medical Journal. 2003;327:557. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] The Cochrane Collaboration; 2011. Available from www.handbook.cochrane.org. [Google Scholar]
- 20.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315:629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Onufrak SJ, Abramson JL, Austin HD, et al. Relation of adult-onset asthma to coronary heart disease and stroke. Am J Cardiol. 2008;101:1247–52. doi: 10.1016/j.amjcard.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bellia V, Pedone C, Catalano F, et al. Asthma in the elderly: mortality rate and associated risk factors for mortality. Chest. 2007;132:1175–82. doi: 10.1378/chest.06-2824. [DOI] [PubMed] [Google Scholar]
- 23.Wu TL, Chang PY, Tsao KC, et al. A panel of multiple markers associated with chronic systemic inflammation and the risk of atherogenesis is detectable in asthma and chronic obstructive pulmonary disease. Journal of clinical laboratory analysis. 2007;21:367–71. doi: 10.1002/jcla.20197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bjermer L. Asthma is a systemic inflammation--not a local disease. Broad anti-inflammatory treatment is necessary. L kartidningen. 2009;106:1905. [PubMed] [Google Scholar]
- 25.Wang L, Gao S, Xu W, et al. Allergic asthma accelerates atherosclerosis dependent on Th2 and Th17 in apolipoprotein E deficient mice. Journal of molecular and cellular cardiology. 2014;72:20–7. doi: 10.1016/j.yjmcc.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 26.Au DH, Curtis JR, Every NR, et al. Association between inhaled beta-agonists and the risk of unstable angina and myocardial infarction. Chest. 2002;121:846–51. doi: 10.1378/chest.121.3.846. [DOI] [PubMed] [Google Scholar]
- 27.Wolf G. Glucocorticoids in adipocytes stimulate visceral obesity. Nutr Rev. 2002;60:148–51. doi: 10.1301/00296640260093823. [DOI] [PubMed] [Google Scholar]