Abstract
Structural barriers to HIV care are particularly challenging in the US South, which has higher HIV diagnosis rates, poverty, uninsurance, HIV stigma, and rurality, and fewer comprehensive public health programs versus other US regions. Focusing on one structural barrier, we examined geographic accessibility to comprehensive, coordinated HIV care (HIVCCC) in the US South. We integrated publicly available data to study travel time to HIVCCC in 16 Southern states and District of Columbia. We geocoded HIVCCC service locations and estimated drive time between the population-weighted county centroid and closest HIVCCC facility. We evaluated drive time in aggregate, and by county-level HIV prevalence quintile, urbanicity, and race/ethnicity. Optimal drive time was ≤30 minutes, a common primary care accessibility threshold. We identified 228 service locations providing HIVCCC across 1,422 Southern counties, with median drive time to care of 70 minutes (IQR 64 minutes). For 368 counties in the top HIV prevalence quintile, median drive time is 50 minutes (IQR 61 minutes), exceeding 60 minutes in over one-third of these counties. Among counties in the top HIV prevalence quintile, drive time to care is six-fold higher for rural versus super-urban counties. Counties in the top HIV prevalence quintiles for non-Hispanic Blacks and for Hispanics have >50% longer drive time to care versus for non-Hispanic Whites. Including another potential care source—publicly-funded health centers serving low-income populations—could double the number of high-HIV burden counties with drive time ≤30 minutes, representing nearly 35,000 additional people living with HIV with accessible HIVCCC. Geographic accessibility to HIVCCC is inadequate in the US South, even in high HIV burden areas, and geographic and racial/ethnic disparities exist. Structural factors, such as geographic accessibility to care, may drive disparities in health outcomes. Further research on programmatic policies, and evidence-based alternative HIV care delivery models improving access to care, is critical.
Background
Of the estimated 1.2 million Americans living with HIV, 40% are engaged in care, with fewer receiving effective antiretroviral therapy and achieving viral suppression (Bradley et al., 2014). In addition to receipt of comprehensive, coordinated HIV care (HIVCCC), system-level factors, or the structural and policy-related aspects of health care delivery, influence health outcomes (ONAP, 2015). Geographic accessibility to health care—i.e., travel time or distance to services—is an important structural determinant of effective care for chronic diseases (Brundisini et al., 2013). Inadequate geographic accessibility to care disproportionately affects racial/ethnic minorities (Onega et al., 2008; Peipins, Graham, Young, Lewis, & Flanagan, 2013), who may face additional barriers like poverty (Macartney, Bishaw, & Fontenot, 2013) and lack of car ownership (Raphael, Berube, & Deakin, 2006). However, scant evidence exists on geographic accessibility to HIV care, including disparities.
Structural barriers to health care remain challenging in the US South (Adimora, Ramirez, Schoenbach, & Cohen, 2014), which claims the highest HIV diagnosis rates nationally (CDC, 2015) and where poverty, uninsurance, and rurality are disproportionate relative to other regions (Desilver, 2014; Stephens, Artiga, & Paradise, 2014). These barriers contribute to striking racial/ethnic disparities: nearly 70% of HIV-positive Southerners are Hispanic or non-Hispanic Black (CDC, 2015; Prejean, Tang, & Hall, 2013), who, once diagnosed, are less likely to be linked to care (Tripathi et al., 2011), retained in care (Mugavero et al., 2009), or receive treatment (Johnson et al., 2013). HIV-positive Southerners are less likely to achieve virologic suppression (Hanna et al., 2013), and Southern states have some of the highest HIV case fatality rates (Hanna, Selik, Tang, & Gange, 2012).
In this context, we estimate drive time to HIVCCC in the US South, detailing disparities in drive time by urbanicity and race/ethnicity. We also describe how disparities might decrease when implementing an illustrative policy solution—publicly-funded health centers serving low-income populations as a potential source of HIV care.
Methods
Data
Service locations
We identified service locations providing HIVCCC in 16 Southern states plus the District of Columbia (DC) using four publicly available data sources: Tracking Accountability in Government Grants (DHHS, 2015), Health Resources and Services Administration (HRSA) Find Grants (HRSA, 2015b), HRSA Data Portal (HRSA, 2015a), and the federal HIV Testing Sites & Care Services Locator database (DHHS, 2016) (Figure 1). Service locations were defined as providing HIVCCC if HIV-related core medical services (e.g., antiretroviral prescriptions) and support services (e.g., case management) were offered.
Figure 1.
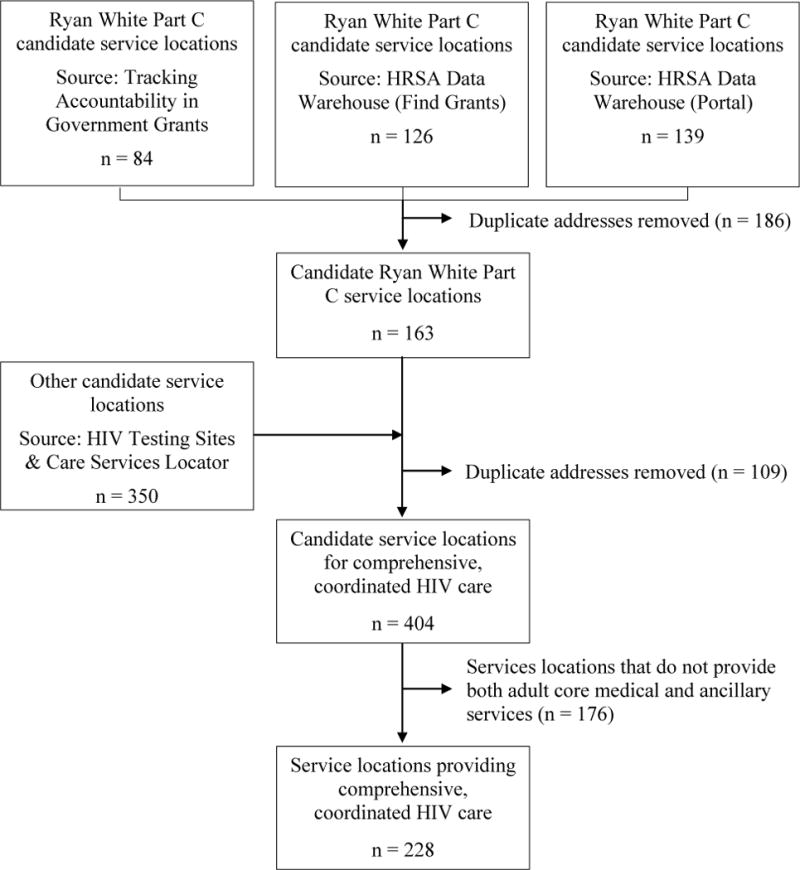
Algorithm to identify service locations providing HIVCCC
This figure shows the process by which service addresses of facilities providing HIVCCC in the US South were identified. We began by identifying candidate service locations (versus administrative locations) of federally funded Ryan White Part C facilities from three public databases, since these clinics represent a national model for HIVCCC. After eliminating duplicate addresses, we integrated potential addresses of non-Ryan White Part C-funded service locations, eliminating service locations not providing both adult core medical and ancillary HIV services. This process resulted in 228 service locations providing comprehensive, coordinated HIV care across the region. Abbreviation: HIVCCC = comprehensive, coordinated HIV care
Using federal grant numbers, we identified in the analytic database those clinics funded by the federal Ryan White Part C, Early Intervention Services program, since they represent a national model for providing HIVCCC. The US Ryan White HIV/AIDS program offers comprehensive treatment and care to approximately 500,000 HIV-positive Americans annually, providing clinical, support, and related services for vulnerable HIV-positive populations (e.g., racial/ethnic minorities) without adequate health insurance.
In sensitivity analysis, we included service locations of federally qualified health centers (FQHCs), which are federally funded outpatient clinics offering comprehensive primary care and support services to underserved communities. Eligible to receive Ryan White Part C funding, FQHCs serve patient populations similar to those seen in Ryan White Part C clinics (Weddle, Twilbeck, Toomey, Mincey, & McNamara, 2015), with nearly one-third of Ryan White clinics nationally also designated as FQHCs (HRSA, 2011).
Other data
We included publicly available HIV surveillance data from 2013 (AIDSVu). County-level adult and adolescent HIV diagnosed cases and diagnosed cases per population were reported for 1,270 Southern counties (of 1,422 total) and by race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic). We focused on counties in the top HIV prevalence quintile, or counties with ≥264–3,442 HIV cases per 100,000 population (Box 1), for all diagnosed HIV cases regardless of race/ethnicity. To identify potential racial and ethnic disparities, we separately identified counties in the top HIV prevalence quintiles for non-Hispanic Whites, for non-Hispanic Blacks, and for Hispanics and examined drive time from counties in the top HIV prevalence quintile for each racial/ethnic group, but emphasize wide variation (≥131–1,437 cases per 100,000 population (non-Hispanic Whites); ≥1,141–10,049 (non-Hispanic Blacks); ≥603–15,785 (Hispanics)).
Box 1. County-level classifications of HIV prevalence and urbanicity*.
| Quintile | HIV prevalence† (cases per 100,000) | Urban status | Definition |
|---|---|---|---|
| 5th‡ | ≥264–3442 | Super-urban | “Central” & “fringe” counties in metropolitan statistical areas§ ≥1 million |
| 4th | 144–263 | ||
| 3rd | 88–143 | Urban | Counties in metropolitan statistical areas of 50,000–999,999 |
| 2nd | 57–87 | Peri-urban | Counties in micropolitan statistical areas¶ |
| 1st | 17–56 | Rural | Counties not in micropolitan statistical areas |
Based on the 2013 National Center for Health Statistics urban-rural classification scheme.
Reflects adult and adolescent cases per 100,000 population.
In addition to aggregate estimates, we also report HIV prevalence in the top HIV prevalence quintile for different races and ethnicities: 131–1,437 (non-Hispanic Whites); 1,141–10,049 (non-Hispanic Blacks); and 603–15,785 (Hispanics).
Metropolitan statistical areas are federally defined geographic areas with high population density, typically consisting of a core city (minimum population 50,000) and multiple adjacent counties which have strong social and economic ties. There are currently 157 metropolitan statistical areas represented in the South, or approximately 40% of all metropolitan statistical areas nationally.
Micropolitan statistical areas are federally defined geographic areas with lower population density, typically consisting of towns and communities with populations greater than 10,000 but less than 50,000. There are currently 213 micropolitan statistical areas in the US South, or approximately 40% of micropolitan statistical areas nationally.
We used additional data on urbanicity, centers of population, and street networks. We adapted the US National Center for Health Statistics urban-rural classification (Ingram and Franco, 2014) to define a four-level measure of urbanicity (Box 1). We used county-level population-weighted centroids, defined as the latitude and longitude of the arithmetic center point of each county’s population (Census Bureau, 2010). Finally, we included street network data from StreetMap Premium for ArcGIS. In sensitivity analysis, we incorporated bus transit data into the network, selecting urban bus transit networks with low (1 bus transit network serving 1 county in Mississippi), medium (3 networks serving 4 counties in South Carolina), and high (9 networks serving 14 counties in North Carolina) levels of bus transit infrastructure.
Analytic approach
We estimated the fastest one-way drive time between each population-weighted county centroid and the closest HIVCCC service location using ArcGIS 10.3.1 and summarized data using Stata 14. We reported median drive time with interquartile ranges (IQR). Tests of statistical significance were not performed since analyses apply to the entire population of HIV-positive adults in the South. We evaluated the results using a 30-minute threshold for primary care accessibility, per a HRSA criterion for defining geographic health professional shortage areas (Government Publishing Office, 2016). This threshold is also used for state access standards for primary and specialty care in Medicaid managed care plans (Murrin, 2014).
We conducted two sensitivity analyses. First, we examined the impact of using bus transit time (bus time) on our findings. In the analytic database, we replaced drive time with bus time for those counties served by bus transit networks. Second, we performed an illustrative analysis examining how provision of HIVCCC at FQHCs might influence findings. While the analytic approach used was similar to baseline analyses, we restricted this sensitivity analysis to counties in the top HIV prevalence quintile to examine only counties with the highest HIV burden.
Results
Service locations
We identified 228 service locations providing HIVCCC in 134 (of 1,422) counties across the South (Figure 2). Of the 228 service locations, 61 (27%) are federally funded Ryan White Part C clinics, and almost half (110) are in four states (Florida, Texas, Virginia, North Carolina). Nearly 90% (204) are in super-urban or urban counties; over three-quarters (185) are in counties in the top HIV quintile.
Figure 2.
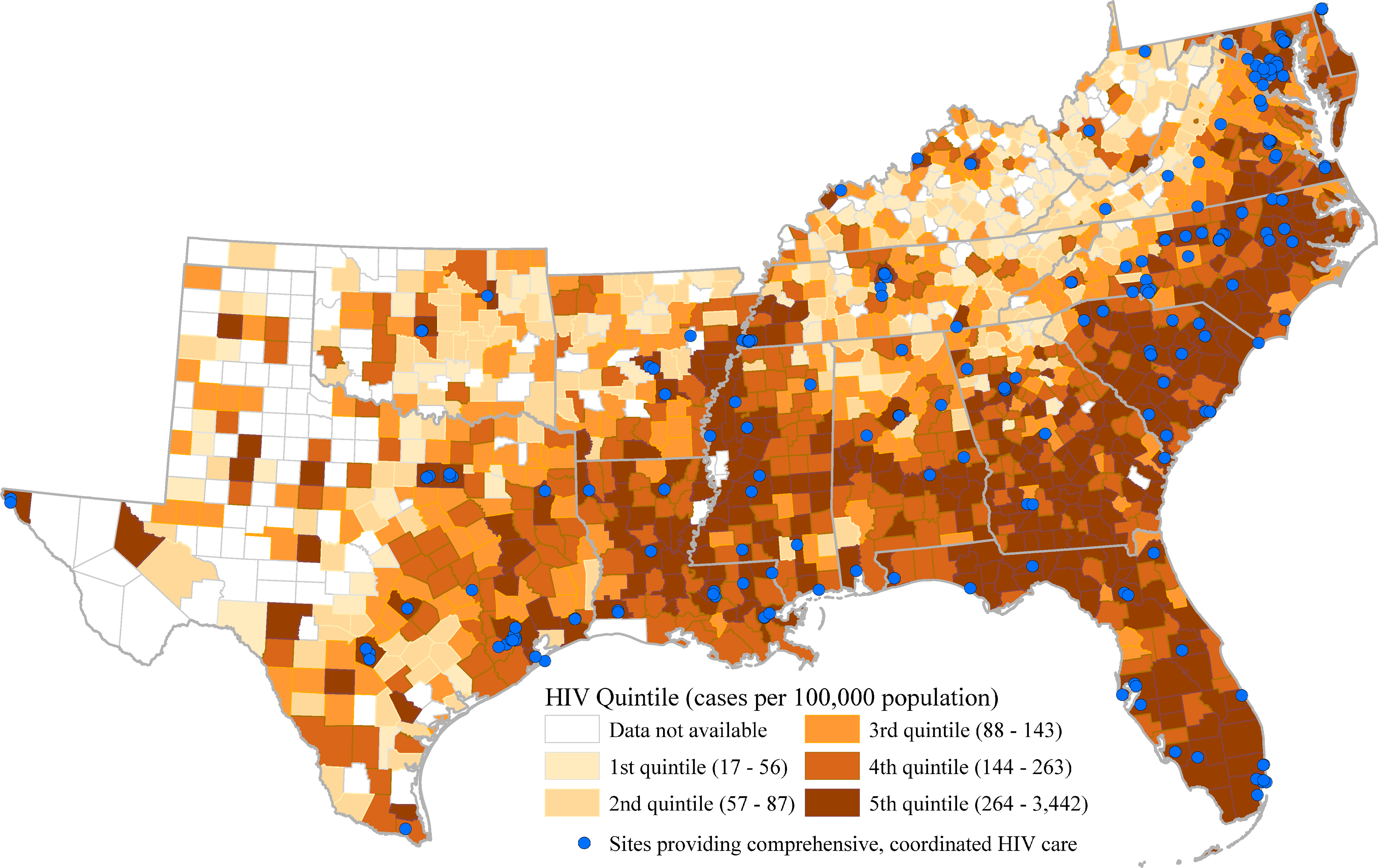
County-level HIV prevalence and service locations providing HIVCCC
Abbreviation: HIVCCC = comprehensive, coordinated HIV care
Disparities in travel time
All counties
Median drive time across all 1,422 counties is 70 minutes (IQR 64 minutes) (Table 1), with drive time >30 minutes for over 80% (1,197) of all Southern counties. Excluding DC, median drive time is <40 minutes for only 1 state (South Carolina) and <50 minutes for three additional states (Maryland, North Carolina, Virginia). Rural counties have drive times more than double that of super-urban counties (median 95 (IQR 63) minutes versus 35 (IQR 34), respectively). Among 1,270 counties having HIV prevalence data, median drive time doubles between counties in the bottom and top HIV prevalence quintiles.
Table 1.
Travel time from population-weighted county centroids to service locations providing comprehensive, coordinated HIV care in the Southern United States
| Median travel time (IQR), min | Number of counties, by travel time category (N (%*))
|
|||||
|---|---|---|---|---|---|---|
| ≤30 min | >0.5 – ≤1 h | >1 – ≤2 h | >2 – ≤4 h | >4 h | ||
| All counties | 70 (64) | 225 (16) | 356 (25) | 571 (40) | 212 (15) | 58 (4) |
| HIV prevalence quintile† | ||||||
| 5th | 50 (61) | 127 (35) | 96 (26) | 126 (34) | 16 (4) | 3 (1) |
| 4th | 62 (57) | 45 (14) | 108 (34) | 128 (40) | 39 (12) | 2 (1) |
| 3rd | 66 (60) | 41 (15) | 77 (29) | 106 (40) | 33 (12) | 10 (4) |
| 2nd | 88 (63) | 7 (4) | 50 (25) | 93 (47) | 44 (22) | 4 (2) |
| 1st | 90 (47) | 3 (3) | 16 (14) | 66 (58) | 23 (20) | 5 (4) |
| Urbanicity‡ | ||||||
| Super-urban | 35 (34) | 88 (40) | 100 (46) | 30 (14) | – | – |
| Urban | 50 (61) | 108 (29) | 108 (29) | 113 (30) | 34 (9) | 11 (3) |
| Peri-urban | 77 (55) | 19 (7) | 60 (23) | 138 (53) | 34 (13) | 10 (4) |
| Rural | 95 (63) | 10 (2) | 88 (15) | 290 (51) | 144 (25) | 37 (7) |
| State | ||||||
| Alabama | 64 (50) | 9 (13) | 20 (30) | 30 (45) | 8 (12) | – |
| Arkansas | 99 (77) | 5 (7) | 15 (20) | 28 (38) | 26 (35) | – |
| Delaware | 71 (90) | 1 (33) | – | 2 (67) | – | – |
| DC§ | 2 (–) | 1 (100) | – | – | – | – |
| Florida | 54 (53) | 17 (25) | 20 (30) | 29 (43) | 1 (1) | – |
| Georgia | 68 (50) | 21 (13) | 42 (26) | 84 (53) | 12 (8) | – |
| Kentucky | 79 (58) | 12 (10) | 27 (23) | 60 (50) | 21 (18) | – |
| Louisiana | 58 (40) | 16 (25) | 20 (31) | 27 (42) | 1 (2) | – |
| Maryland | 46 (57) | 8 (33) | 5 (21) | 8 (33) | 3 (13) | – |
| Mississippi | 57 (43) | 14 (17) | 32 (39) | 34 (41) | 2 (2) | – |
| North Carolina | 44 (45) | 29 (29) | 35 (35) | 31 (31) | 5 (5) | – |
| Oklahoma | 101 (81) | 5 (6) | 11 (14) | 32 (42) | 26 (34) | 3 (4) |
| South Carolina | 35 (28) | 13 (28) | 24 (52) | 9 (20) | – | – |
| Tennessee | 84 (49) | 6 (6) | 17 (18) | 56 (59) | 16 (17) | – |
| Texas | 129 (157) | 20 (8) | 29 (11) | 71 (28) | 79 (31) | 55 (22) |
| Virginia | 41 (45) | 44 (33) | 47 (35) | 39 (29) | 4 (3) | – |
| West Virginia | 76 (53) | 4 (7) | 12 (22) | 31 (56) | 8 (15) | – |
Abbreviations: IQR = interquartile range; min = minutes; h = hours; DC = District of Columbia
Percentages may not add up to 100% due to rounding. We represent the number of counties with a zero percentage contribution to the distribution with dashes (–).
Travel time is reported for those counties with reported HIV prevalence estimates; counties with missing prevalence estimates are excluded. HIV prevalence quintiles are defined as follows: 5th, ≥264–3,442 cases per 100,000 population. 4th, 144–263 cases per 100,000 population. 3rd, 88–143 cases per 100,000 population. 2nd, 57–87 cases per 100,000 population. 1st, 17–56 cases per 100,000 population.
Urbanicity: Super-urban, counties in metropolitan statistical areas (MSAs) ≥1 million people. Urban, counties in MSAs of 50,000–999,999. Peri-urban, counties in micropolitan statistical areas. Rural, counties not in micropolitan statistical areas.
For DC, state-level HIV prevalence estimates were used in the analysis.
Counties in the top HIV prevalence quintile
We identified 368 counties in the top HIV prevalence quintile for all races and ethnicities. Median drive time to HIVCCC is 50 minutes (IQR 61), exceeding 30 minutes in two-thirds of these counties and 60 minutes in over one-third.
We found large differences in drive time when stratifying by urbanicity (Figure 3). Median drive time from rural counties in the top HIV prevalence quintile is >1 hour—nearly 700% the drive time in super-urban areas. In most states, drive time increases with increasing rurality, at times with wide variation: In Alabama, median drive time for rural counties is 71 minutes, >20 times longer than for super-urban counties.
Figure 3.
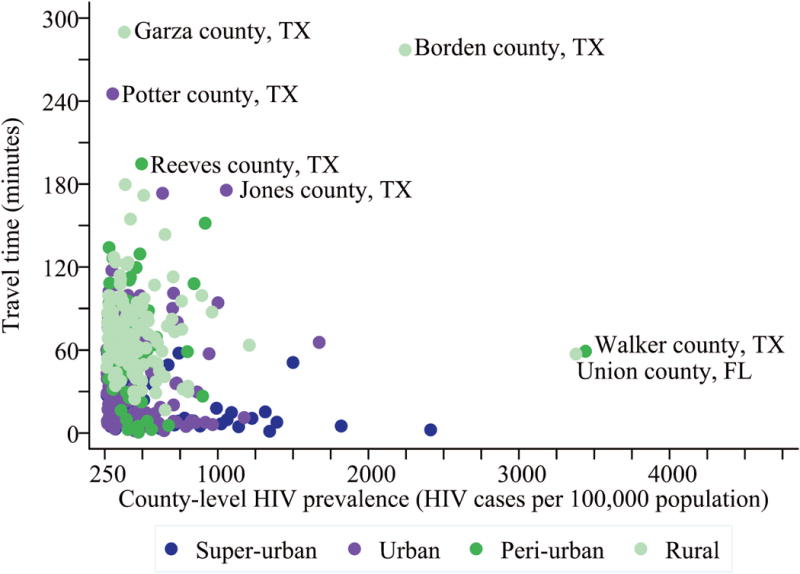
Travel time from the population-weighted county centroid to HIVCCC in the top HIV prevalence quintile, by county urbanicity
This figure shows travel time by urbanicity in the top HIV prevalence quintile. On the horizontal axis is HIV prevalence, while travel time in minutes is shown on the vertical axis. Super-urban counties are shown in dark blue (◆), urban counties in purple (◆), peri-urban counties in green (◆), and rural counties in light green (◆). Less urban counties in the top HIV prevalence quintile have lower HIV prevalence but much higher travel time to HIV care, compared to more urban counties. Some of the highest HIV prevalence peri-urban and rural counties (labeled)—e.g., Union county, FL, Walker county, TX—have travel times to care exceeding 60 minutes. Some counties (also labeled) with lower HIV prevalence, but still in the top HIV prevalence quintile—such as Potter county, TX, and Garza county, TX—have travel time of over three hours. Most outliers are in Texas, due to the relative geographic clustering of clinics compared to the geographic dispersion of HIV cases across this large state. Abbreviation: HIVCCC = comprehensive, coordinated HIV care
We also evaluated drive time from counties in the top HIV prevalence quintile for different races and ethnicities, although underscore wide differences in HIV prevalence estimates in the top quintile by racial/ethnic group, complicating direct comparisons (≥131–1,437 (non-Hispanic Whites, n=233 counties); ≥1,141–10,049 (non-Hispanic Blacks, n=154 counties); ≥603–15,785 (Hispanics, n=70 counties)). Some counties (e.g., Miami-Dade, Florida) were in the top HIV prevalence quintile across multiple racial/ethnic groups.* Drive time in the top HIV prevalence quintile for non-Hispanic Whites is 32 minutes (IQR 60), increasing over 50% (+18 minutes) in the top HIV prevalence quintile for non-Hispanic Blacks and nearly doubling in the top HIV prevalence quintile for Hispanics (+26 minutes). Across urban counties, this drive time disparity increases to 70% longer for non-Hispanic Blacks and almost triples for Hispanics, although attenuates for peri-urban and rural counties. The disparity begins to reverse for super-urban counties: drive time from counties in the top HIV prevalence quintile for Hispanics (7 minutes) is nearly 30% less than that for other racial/ethnic groups.
Bus transit transportation
We examined changes in travel time to HIVCCC when bus transit was available. In Mississippi, South Carolina, and North Carolina, overall median travel time increases from 47 minutes (IQR 43) for drive time only to 51 minutes (IQR 45) for drive time or bus time. While median travel time increases by 5 minutes for both South Carolina and North Carolina, there are no differences in median travel time for Mississippi. However, when restricting to counties with bus transit networks, overall median travel time increases from 11 minutes drive time (IQR 19) to 91 minutes bus time (IQR 197), ranging from 6-fold (North Carolina) to 15-fold (Mississippi) increases in median travel time due to use of bus transit.
An illustrative policy solution
We identified 1,567 Southern FQHCs that were not providing HIVCCC. Drive time from counties in the top HIV prevalence quintile decreases 80% (from median 50 minutes to median 10 minutes) when including FQHCs as a potential source of HIV care. This illustrative policy solution for counties in the top HIV prevalence quintile results in 170 additional counties (+235%) and 34,815 more diagnosed HIV cases (from 279,106 to 313,921, or +12%) meeting the 30-minute travel time threshold (Figure 4).
Figure 4.
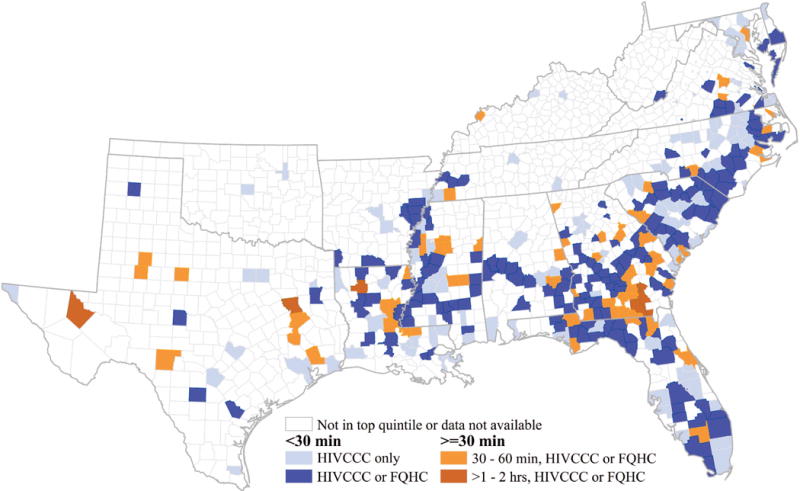
Reductions in travel time if federally qualified health centers (FQHCs) could offer HIVCCC in high-HIV burden Southern counties: an illustrative example
This county-level map of the US South shows changes in travel time when including federally qualified health centers, or FQHCs, as a potential source of HIV care for counties in the top HIV prevalence quintile. If comprehensive, coordinated HIV care were available at all FQHCs in the top HIV prevalence quintile either directly or through an alternative care model (e.g., telepartnership with an existing Ryan White clinic), an additional 170 counties in the top HIV prevalence quintile (shown in bright blue, ■) would have travel times to care under 30 minutes, a commonly used threshold. This represents a more than 230% increase in the number of counties (shown in light blue, ■) meeting the 30-minute travel time threshold. However, even when FQHCs are a potential source of HIV care, a small number of counties still have travel times that do not meet the optimal threshold, with travel times between 30 and 60 minutes shown in light orange (■) and >60 minutes shown in dark orange (■). Abbreviations: FQHC = federally qualified health center; HIVCCC = comprehensive, coordinated HIV care.
For counties in the top HIV prevalence quintile, including FQHCs as a potential source of HIVCCC could reduce geographic disparities in travel time. Similar to analyses without FQHCs, travel time increases with rurality. However, when including FQHCs as a potential source of HIVCCC in high-burden counties, rural and peri-urban counties across the region see the greatest benefits, with drive time decreases of more than 50 minutes (versus –15 minutes and –4 minutes, for urban and super-urban locales).
Racial/ethnic disparities in travel time to HIV care could diminish if HIVCCC were offered either directly from or through partnerships with FQHCs. Median drive time to care decreases approximately 40 minutes from counties in the top HIV quintile for both non-Hispanic Blacks and Hispanics. The disparity in median drive time across counties in the top HIV prevalence quintile for different racial/ethnic groups narrows substantially to 2 minutes (for non-Hispanic Blacks) and 4 minutes (for Hispanics) compared to non-Hispanic Whites.
Discussion
Structural barriers to health care, particularly geographic proximity to care, remain challenging for persons living with HIV. We find that drive time to HIVCCC exceeds common thresholds for care accessibility in most Southern counties, including high HIV burden counties. We also find notable disparities by county urbanicity and race/ethnicity. When including an alternative care source, FQHCs, both overall drive time and disparities in drive time diminish markedly, although disparities still exist.
The current study highlights nuances in geographic proximity to care. In the highest prevalence quintile, drive time to care from rural counties greatly exceeds that of urban counties, with some states showing particularly wide variation by urbanicity. Several Texas counties, for example, have excessively high travel times due to the more urban clustering of clinics versus the wider geographic dispersion of HIV cases across this large state. Drive time is longer from counties in the top prevalence quintile for non-Hispanic Blacks and for Hispanics compared to those for non-Hispanic Whites. These disparities point to structural barriers to care, systematically disadvantaging rural residents and racial/ethnic minorities. While overall median travel time increases only modestly when including bus time estimates, for those counties with bus transit systems, bus transit availability substantially increases travel time, confirming previous work (Dasgupta et al., 2015).
Study findings highlight the need for targeted solutions that decrease disparities in geographic access to HIV care. If FQHCs were an additional source of HIVCCC in high-burden areas, drive time decreases markedly, with reductions in drive time disparities by urbanicity and race/ethnicity. This presents an optimistic, best-case scenario, given that generalist clinicians at FQHCs may not have the same HIV care expertise as those at specialty HIV clinics. However, generalist clinicians can develop expertise in HIV management through clinical experience and education, and expert generalists can provide high-quality HIV care (Landon et al., 2003; Landon et al., 2002). Further, evidence-based alternative care delivery models may make FQHC-based HIV care possible. Telemedicine allowing HIV specialists to remotely partner with generalist clinicians has shown promise for rural veterans living with HIV (Ohl et al., 2013); specialist tele-support for primary care providers through the Project ECHO model has expanded care for vulnerable populations with complex, chronic conditions (Arora et al., 2011) and is cost-effective in populations with hepatitis C (Rattay, Dumont, Heinzow, & Hutton, 2017). Yet real-world financial and operational challenges may limit the widespread feasibility of FQHCs as a policy solution. Ongoing federal funding for community health centers is uncertain (NACHC, 2017), and Southern FQHCs, particularly in non-Medicaid expansion states, may have more uninsured and underinsured individuals, lower revenue per patient, lower medical staffing ratios, and higher workforce recruitment and retention challenges (Paradise et al., 2017).
This study’s findings contribute to an emerging literature on geographic proximity to HIV care in the US. Existing knowledge comes mainly from studies in select urban populations (Goswami et al., 2016). While geographic proximity is one of many factors influencing choice of service location (Eberhart et al., 2014), travel distance is a considerable barrier for some (Sutton, Anthony, Vila, McLellan-Lemal, & Weidle, 2010). The current study builds on this evidence by estimating travel time to care across an entire region and evaluating state-level variation, as well as racial/ethnic disparities in geographic accessibility to HIV care, which—like other structural barriers—could contribute to disparities in health outcomes.
Our findings contribute to a broader literature on geographic proximity to care for individuals with complex, chronic diseases. While trends in geographic and racial/ethnic disparities are similar, absolute drive time to HIV care appears far greater. Median travel time to specialized cancer care in the South (17 minutes) (Onega, et al., 2008) is nearly one-third that for high HIV prevalence Southern counties; mean travel distance nationally to dialysis facilities is approximately 8 miles (Stephens et al., 2013), likely with a far lower travel time than for even the highest HIV burden counties. Ultimately, longer travel time or distance to receive HIV care may be associated with poorer quality of care and health outcomes, as reported for cancer treatment (Lin et al., 2015) and diabetes management (Strauss, MacLean, Troy, & Littenberg, 2006), potentially exacerbating disparities.
Limitations
First, the data did not capture individual travel time to HIVCCC. Instead we relied on county travel time, capitalizing on publicly available data to glean broad insights on travel time to HIV care and disparities regionally. Second, baseline data did not include public transport networks, a realistic source of transportation in metropolitan areas. If we had fully incorporated public transportation data, estimated travel time would likely increase for counties with public transit (Eberhart, Share, Shpaner, & Brady, 2015); sensitivity analysis confirmed a substantial increase in travel time for counties served by bus transit networks but a modest overall increase. Further, while limited data inhibited our evaluation of the impact of public transit on disparities, disparities by urbanicity in travel time to HIV care would likely attenuate, while disparities by race/ethnicity would likely increase, since racial/ethnic minorities are more likely to use public transportation (Anderson, 2016). Third, the nature of the county-level HIV prevalence data made direct comparisons of travel time for different racial/ethnic groups in the top HIV prevalence quintile challenging, since prevalence thresholds varied by race/ethnicity. While we detected striking racial/ethnic disparities in drive time, future research should determine whether disparities persist at the individual level. Fourth, the data did not allow reliable identification of Ryan White Part B-funded sites, which receive federal funding indirectly (as allocated by US states and territories) to provide HIV core and support services. However, we identify and highlight Ryan White Part C clinics since there is substantial overlap between Part B and Part C clinics and they are a national model for the provision of a comprehensive suite of HIV services. Finally, the definition of HIVCCC not only included provision of two service classes, but required their co-location at a single facility. In reality, individuals may access medical and support services at different facilities. While the data did not allow for identification of facilities that partner in providing HIVCCC, future research can leverage individual-level data to examine the role of non-co-located services in geographic access to HIVCCC.
Conclusions
Geographic accessibility is an important, but often overlooked, structural barrier to HIV care and a potential contributor to disparities in accessing care. This study underscores its importance in future research, including on regional disparities, racial/ethnic disparities in access, and the relationship between travel time to care and HIV care quality. This evidence is timely as the current US health policy debate leaves the future of many federal programs uncertain, possibly limiting health care resources and intensifying geographic inaccessibility for vulnerable and minority populations, especially Southerners with HIV (Adimora, et al., 2014). Maintaining and expanding medical transportation services, implementing evidence-based telehealth solutions with primary care clinics, and investigating the acceptability of local nurse-managed care are critical next steps to addressing geographic barriers to care. Doing so promises further forward movement toward increasing access to care, reducing health disparities, and eliminating new HIV infections in the US.
Supplementary Material
Acknowledgments
FUNDING
This research was supported in part by the National Institutes of Health (CTSA award number KL2TR000057 from the National Center for Advancing Translational Sciences and R01 MD011277 from the National Institute on Minority Health and Health Disparities) and the Blick Scholars Program at Virginia Commonwealth University. The funding sources played no role in the study, including study design; collection, analysis, and/or interpretation of data; the writing of the manuscript; and the decision to submit the manuscript for publication.
Footnotes
Preliminary results for this manuscript were presented in part at the 8th IAS Conference on HIV Pathogenesis, Treatment, and Prevention [abstract A-729-0310-03361], July 19–22, 2015, Vancouver, Canada, and the AcademyHealth Annual Research Meeting [abstract 10924], June 26–28, 2016, Boston, USA.
Fewer counties are in the top HIV prevalence quintile for racial/ethnic minorities, since more Hispanic and non-Hispanic Black than non-Hispanic White county estimates for HIV prevalence are suppressed due to low numbers of cases.
COMPETING INTERESTS
The authors have no competing interests, financial or otherwise, to declare.
References
- Adimora AA, Ramirez C, Schoenbach VJ, Cohen MS. Policies and politics that promote HIV infection in the Southern United States. AIDS. 2014;28(10):1393–1397. doi: 10.1097/qad.0000000000000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AIDSVu. Emory University, Rollins School of Public Health; www.aidsvu.org. Retrieved March 13, 2018. [Google Scholar]
- Anderson M. Who relies on public transit in the US Fact Tank: News In the Numbers. Pew Research Center; 2016. Retrieved March 13, 2018 from http://www.pewresearch.org/fact-tank/2016/04/07/who-relies-on-public-transit-in-the-u-s/ [Google Scholar]
- Arora S, Kalishman S, Dion D, Som D, Thornton K, Bankhurst A, Yutzy S. Partnering urban academic medical centers and rural primary care clinicians to provide complex chronic disease care. Health Affairs. 2011;30(6):1176–1184. doi: 10.1377/hlthaff.2011.0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley H, Hall HI, Wolitski RJ, Van Handel MM, Stone AE, LaFlam M, Valleroy LA. Vital Signs: HIV diagnosis, care, and treatment among persons living with HIV–United States, 2011. MMWR Morbidity and Mortality Weekly Report. 2014;63(47):1113–1117. [PMC free article] [PubMed] [Google Scholar]
- Brundisini F, Giacomini M, DeJean D, Vanstone M, Winsor S, Smith A. Chronic disease patients’ experiences with accessing health care in rural and remote areas: a systematic review and qualitative meta-synthesis. Ontario Health Technology Assessment Series. 2013;13(15):1–33. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] Diagnoses of HIV Infection in the United States and Dependent Areas, 2014. 2015 Retrieved from http://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-us.pdf.
- Dasgupta S, Kramer MR, Rosenberg ES, Sanchez TH, Reed L, Sullivan PS. The effect of commuting patterns on HIV care attendance among men who have sex with men (MSM) in Atlanta, Georgia. JMIR Public Health and Surveillance. 2015;1(2):e10. doi: 10.2196/publichealth.4525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desilver D. Who’s poor in America? 50 years into the ‘War on Poverty,’ a data portrait. Pew Research Center; 2014. Retrieved March 13, 2018 from http://www.pewresearch.org/fact-tank/2014/01/13/whos-poor-in-america-50-years-into-the-war-on-poverty-a-data-portrait/ [Google Scholar]
- Eberhart MG, Share AM, Shpaner M, Brady KA. Comparison of geographic methods to assess travel patterns of persons diagnosed with HIV in Philadelphia: How close is close enough? Journal of Biomedical Informatics. 2015;53:93–99. doi: 10.1016/j.jbi.2014.09.005. [DOI] [PubMed] [Google Scholar]
- Eberhart MG, Voytek CD, Hillier A, Metzger DS, Blank MB, Brady KA. Travel distance to HIV medical care: a geographic analysis of weighted survey data from the Medical Monitoring Project in Philadelphia, PA. AIDS and Behavior. 2014;18(4):776–782. doi: 10.1007/s10461-013-0597-7. [DOI] [PubMed] [Google Scholar]
- Goswami ND, Schmitz MM, Sanchez T, Dasgupta S, Sullivan P, Cooper H, Waller LA. Understanding local spatial variation along the care continuum: The potential impact of transportation vulnerability on HIV linkage to care and viral suppression in high-poverty areas, Atlanta, Georgia. Journal of Acquired Immune Deficiency Syndromes. 2016;72(1):65–72. doi: 10.1097/qai.0000000000000914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government Publishing Office. 42 CFR Part 5, Appendix A to Part 5, Criteria for Designation of Areas Having Shortages of Primary Medical Care Professional(s) 2016 [Google Scholar]
- Hanna DB, Buchacz K, Gebo KA, Hessol NA, Horberg MA, Jacobson LP, Gange SJ. Trends and disparities in antiretroviral therapy initiation and virologic suppression among newly treatment-eligible HIV-infected individuals in North America, 2001-2009. Clinical Infectious Diseases. 2013;56(8):1174–1182. doi: 10.1093/cid/cit003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna DB, Selik RM, Tang T, Gange SJ. Disparities among US states in HIV-related mortality in persons with HIV infection, 2001-2007. AIDS. 2012;26(1):95–103. doi: 10.1097/QAD.0b013e32834dcf87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources and Services Administration [HRSA] National HIV/AIDS Strategy: Improving HIV/AIDS Care in the Health Center Community. Summary of a HRSA/BPHC Grantee TA Call - Held January 31, 2011. 2011 Retrieved March 13, 2018 from https://bphc.hrsa.gov/technicalassistance/taresources/nhascallnotes040111.pdf.pdf.
- Health Resources and Services Administration [HRSA] Data Warehouse - Data Portal. 2015a Retrieved March 13, 2018 from https://datawarehouse.hrsa.gov/tools/dataportal.aspx.
- Health Resources and Services Administration [HRSA] Data Warehouse - Find Grants. 2015b Retrieved March 13, 2018 from https://datawarehouse.hrsa.gov/Tools/FindGrants.aspx.
- Ingram DD, Franco SJ. 2013 NCHS urban–rural classification scheme for counties. Vital and Health Statistics Series 2, Data evaluation and methods research. 2014;166:1–73. [PubMed] [Google Scholar]
- Johnson AS, Beer L, Sionean C, Hu X, Furlow-Parmley C, Le B, Dean HD. HIV infection - United States, 2008-2010. MMWR Morbidity and Mortality Weekly Report Surveillance Summaries. 2013;62(Suppl 3):112–119. [PubMed] [Google Scholar]
- Landon BE, Wilson IB, Cohn SE, Fichtenbaum CJ, Wong MD, Wenger NS, Cleary PD. Physician specialization and antiretroviral therapy for HIV. Journal of General Internal Medicine. 2003;18(4):233–241. doi: 10.1046/j.1525-1497.2003.20705.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landon BE, Wilson IB, Wenger NS, Cohn SE, Fichtenbaum CJ, Bozzette SA, Cleary PD. Specialty training and specialization among physicians who treat HIV/AIDS in the United States. Journal of General Internal Medicine. 2002;17(1):12–22. doi: 10.1046/j.1525-1497.2002.10401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin CC, Bruinooge SS, Kirkwood MK, Olsen C, Jemal A, Bajorin D, Hershman DL. Association Between geographic access to cancer care, insurance, and receipt of chemotherapy: Geographic distribution of oncologists and travel distance. Journal of Clinical Oncology. 2015;33(28):3177–3185. doi: 10.1200/jco.2015.61.1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macartney S, Bishaw A, Fontenot K. American Community Survey Briefs. US Census Bureau; Washington, DC: 2013. Poverty Rates for Selected Detailed Race and Hispanic Groups by State and Place: 2007-2011. https://www.census.gov/prod/2013pubs/acsbr11-17.pdf. [Google Scholar]
- Mugavero MJ, Lin HY, Allison JJ, Giordano TP, Willig JH, Raper JL, Saag MS. Racial disparities in HIV virologic failure: Do missed visits matter? Journal of Acquired Immune Deficiency Syndromes. 2009;50(1):100–108. doi: 10.1097/QAI.0b013e31818d5c37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murrin S. State Standards for Access to Care in Medicaid Managed Care. U.S. Department of Health and Human Services, Office of the Inspector General; 2014. https://oig.hhs.gov/oei/reports/oei-02-11-00320.pdf. [Google Scholar]
- National Association of Community Health Centers [NACHC] Appropriations. 2017 Retrieved March 13, 2018 from http://www.nachc.org/policy-matters/federal-issues/appropriations/
- Office of National AIDS Policy [ONAP] National HIV/AIDS Strategy for the United States: Updated to 2020. 2015 Jul; Retrieved March 13, 2018. [Google Scholar]
- Ohl M, Dillon D, Moeckli J, Ono S, Waterbury N, Sissel J, Kaboli P. Mixed-methods evaluation of a telehealth collaborative care program for persons with HIV infection in a rural setting. Journal of General Internal Medicine. 2013;28(9):1165–1173. doi: 10.1007/s11606-013-2385-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onega T, Duell EJ, Shi X, Wang D, Demidenko E, Goodman D. Geographic access to cancer care in the US. Cancer. 2008;112(4):909–918. doi: 10.1002/cncr.23229. [DOI] [PubMed] [Google Scholar]
- Paradise J, Rosenbaum S, Markus A, Sharac J, Tran C, Reynolds D, Shin P. Community Health Centers: Recent Growth and the Role of the ACA. 2017 Retrieved from https://www.kff.org/report-section/community-health-centers-recent-growth-and-the-role-of-the-aca-issue-brief/
- Peipins LA, Graham S, Young R, Lewis B, Flanagan B. Racial disparities in travel time to radiotherapy facilities in the Atlanta metropolitan area. Social Science and Medicine. 2013;89:32–38. doi: 10.1016/j.socscimed.2013.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prejean J, Tang T, Hall HI. HIV diagnoses and prevalence in the Southern region of the United States, 2007-2010. Journal of Community Health. 2013;38(3):414–426. doi: 10.1007/s10900-012-9633-1. [DOI] [PubMed] [Google Scholar]
- Raphael S, Berube A, Deakin E. (University of California Transportation Center, Working Paper).Socioeconomic differences in household automobile ownership rates: Implications for evacuation policy. 2006 Retrieved March 13, 2018 from https://escholarship.org/uc/item/7bp4n2f6.
- Rattay T, Dumont IP, Heinzow HS, Hutton DW. Cost-effectiveness of access expansion to treatment of Hepatitis C virus infection through primary care providers. Gastroenterology. 2017;153(6):1531–1543. doi: 10.1053/j.gastro.2017.10.016. [DOI] [PubMed] [Google Scholar]
- Stephens J, Artiga S, Paradise J. Health coverage and care in the South in 2014 and beyond. 2014 Retrieved March 13, 2018 from https://kaiserfamilyfoundation.files.wordpress.com/2014/04/8577-health-coverage-and-care-in-the-south-in-2014-and-beyond-june-2014-update.pdf.
- Stephens JM, Brotherton S, Dunning SC, Emerson LC, Gilbertson DT, Harrison DJ, Gitlin M. Geographic disparities in patient travel for dialysis in the United States. Journal of Rural Health. 2013;29(4):339–348. doi: 10.1111/jrh.12022. [DOI] [PubMed] [Google Scholar]
- Strauss K, MacLean C, Troy A, Littenberg B. Driving distance as a barrier to glycemic control in diabetes. Journal of General Internal Medicine. 2006;21(4):378–380. doi: 10.1111/j.1525-1497.2006.00386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton M, Anthony MN, Vila C, McLellan-Lemal E, Weidle PJ. HIV testing and HIV/AIDS treatment services in rural counties in 10 Southern states: Service provider perspectives. Journal of Rural Health. 2010;26(3):240–247. doi: 10.1111/j.1748-0361.2010.00284.x. [DOI] [PubMed] [Google Scholar]
- Tripathi A, Gardner LI, Ogbuanu I, Youmans E, Stephens T, Gibson JJ, Duffus WA. Predictors of time to enter medical care after a new HIV diagnosis: A statewide population-based study. AIDS Care. 2011;23(11):1366–1373. doi: 10.1080/09540121.2011.565032. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Centers of Population by County. 2010 Retrieved March 13, 2018 from https://www.census.gov/geo/reference/centersofpop.html.
- U.S. Department of Health and Human Services [DHHS] Tracking Accountability in Government Grants System. 2015 Retrieved March 13, 2018 from https://taggs.hhs.gov/
- U.S. Department of Health and Human Services [DHHS] HIV Testing Sites & Care Services Locator. 2016 Retrieved March 13, 2018 from https://www.hiv.gov/locator/
- Weddle A, Twilbeck N, Toomey B, Mincey V, McNamara K. Strategies for Ryan White providers to partner/transition to community health centers in a post-Affordable Care Act world. HIV Prevention Justice Alliance. 2015 Retrieved March 13, 2018 from http://www.preventionjustice.org/wp-content/uploads/2015/01/HIV-PJA-Ryan-White-Webinar-1.14.15.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


