Introduction
Racial and ethnic differences in pain management have been documented in children 0–17 years of age [1]. Previous studies have noted consistent racial discrepancies in opioid use during emergency department visits involving pain management where white, non-Hispanic children are consistently more likely to be administered opioids as compared to minority groups [22; 23; 6]. In contrast, data from ambulatory surgery settings are inconsistent, with some studies showing differences in opioid administration based on race [16], and others showing no differences [20] However, race and ethnic differences in opioid prescriptions to children have not yet been identified in outpatient health care settings, although this is a frequently occurring context for children to receive opioids. This is an important gap in knowledge that may inform the development and evaluation of interventions to reduce differences in pain management for children and adolescents, based on context of health care visits [10].
Minority individuals are often undertreated for pain relative to white individuals[2] and recent evidence in adults show that health care providers’ race may play a significant role in these observed disparities[7; 11]. Indeed, white health care providers often endorse the belief that white individuals are more pain sensitive than black individuals, which in turn affects their treatment of pain in minorities [26; 12]. Because 75% of the physician workforce in the United States is white, non-Hispanic, it stands to reason that differences in opioid prescribing among children may be strongly associated with health care providers’ race and ethnic status. However, there is no published literature on the association between health care providers’ race and ethnic status and opioid prescribing to children. This is also an important gap in knowledge that would significantly influence systemic interventions to address racial disparities in pain management among children in the United States.
Thus, the primary aim of this study is to examine differences in opioid prescribing by child race in a representative sample of children in the United States receiving health care from outpatient healthcare providers. The context of outpatient settings is different from emergency department and surgery visits in that we expect providers and patients to be familiar with each other, thereby reducing some of the bias associated with treating unfamiliar patients. We hypothesized that no differences would be found in rates of opioid prescribing between white children as compared to minority (black, Hispanic, other racial groups) children. We also examined non-opioid analgesic prescribing to children based on race and ethnicity. The second aim of this study was to examine associations between health care providers’ race and ethnic status and differences in opioid prescribing to children. This aim was accomplished in a subsample of 33% of participants who reported that their usual source of health care provider was a person (e.g. MD, nurse practitioner, physician assistant, other provider). Specifically, we hypothesized that children who have a race-concordant relationship with their usual source of health care provider would be more likely to receive opioid prescriptions as compared to children who were of different race/ethnicity to their provider.
Methods
Survey design and population
This study involves secondary analyses of data from all children 0–17 years of age who participated in the 2003–2014 Medical Expenditure Panel Surveys (MEPS). MEPS are a set of large-scale surveys of individuals, households, and their medical providers, including pharmacies, across the United States. MEPS is aimed at providing comprehensive estimates of health care use, including prescription medication use among the noninstitutionalized civilian population of the USA. Surveys are conducted by the National Centre for Health Statistics and the Agency for Healthcare Research and Quality. In-person interviews are conducted with parents of child participants during which sociodemographic information is gathered and all medical encounters, including prescribed medications, are documented. Data are then summarized to provide annual health care utilization for each child participant. Please see the MEPS website http://meps.ahrq.gov/mepsweb/ for further information on design, sampling, and methodology. The sample used in our study includes all children 0–17 years of age who participated in the 2003–2014 MEPS. Approximately 8500–10000 children participated in MEPS each year from 2003–2014 and our final sample included 113,929 children. For this study we used a cross-sectional design to characterize the association between children’s racial and ethnic category and analgesic prescribing, including both opioids and non-opioid analgesics.
Study variables
Race and ethnicity
MEPS collects detailed information about self-reported race including whether participants identify as white, black, American Indian/Alaskan native, and Asian/Native Hawaiian/Pacific Islanders. Ethnic data collected includes whether participants report being Hispanic versus non-Hispanic. We collapsed race and ethnic categories to create a variable containing 6 categories: white non-Hispanic, black non-Hispanic, Hispanic, American Indian/Alaskan Native, Asian/Native Hawaiian/Pacific Islander and a category of children who reported multiple races. In this manuscript “white” refers to white, non-Hispanic individuals; “black” refers to black, non-Hispanic individuals; and “Hispanic” to white or black Hispanic individuals. We also refer to the Asian/Native Hawaiian/Pacific Islanders as “Asian” because Asian individuals formed the majority of this category. We were unable to further to classify the Asian/Native Hawaiian/Pacific Islander category because of changes in the MEPS survey in year 2012. We excluded multiple race children from analysis (3.2% of participants). Our categorization of race and ethnicity is consistent with the 2010 United States census categorization.
Usual source of care provider
MEPS collects data on whether each child participant has a particular doctor’s office, clinic, health center, or other place that the child goes to if he/she is sick or needs advice about his/her health (usual source of health care). In our sample >90% of children had a usual source of health care. About 33% (n=35,707) of children’s usual source of care was a specific health care provider (including MD’s, nurses, nurse practitioners, physician assistants, and other providers). Participants whose usual source of care was identified as a person reported the perceived race and ethnicity of their usual source of care providers. We collapsed health care provider’s race and ethnicity into 3 categories: white non-Hispanic, black non-Hispanic, and Hispanic. We did not include the other racial categories because of small sample sizes. To determine race-concordant relationships, we matched patients’ and providers’ race and ethnicity. Those assigned to the same race and ethnicity category were categorized as having a race concordant relationship, while patient and providers whose race and ethnicity differed from each other were considered to not have a race concordant relationship. Children who did not have a usual source of care provider listed several reasons, including seldom being sick (most common reason), recently moved to the area, don’t know where to go, changed insurance plans, goes to different providers for different needs, and other reasons.
Sociodemographic and health status covariates
We extracted the following data for each child participant, age (categories: <6 years, 6–11 years, and 12–17 years), sex (male/female), geographic region (Northeast, Midwest, South, and West), and insurance coverage (private, public, or uninsured). Parents also reported on their child’s physical and mental health status during the preceding year on a Likert type scale with the following categories: excellent, very good, good, fair, or poor.
Health care use variables
In order to control for health care use, we extracted data on all outpatient health care visits and prescription medications used by child participants over the past year. Outpatient health care visits consisted of a sum of the number of office visits and hospital outpatient clinic visits made by participants over the past year. Office visits consisted of medical encounters, with both physicians and non-physicians, that took place in office-based settings and clinics. Hospital outpatient visits consisted of medical encounters, with both physicians and non-physicians that took place in hospital-based outpatient clinic departments. The prescribed medications variable was a sum of the number of medications prescribed to children at all outpatient health care visits.
Identification and classification of analgesics
MEPS collected data on medications prescribed to participants during the past year. MEPS surveyors then contacted participants’ dispensing pharmacies and collected additional data about prescribed medications used, including Cerner’s Multum Lexicon therapeutic class and medicine name. This included data on all medications associated with outpatient visits (e.g., hospital outpatient clinic visits, office-based visits, and dental office visits); however, no information was collected on medications prescribed during hospital inpatient visits nor were data collected on over-the-counter medications. We also excluded from analysis any opioids received by children following emergency department visits and hospital stays (both day and overnight stays). We identified analgesic prescriptions using Cerner’s Multum Lexicon therapeutic drug class classification system as captured in MEPS. We then classified prescription medications into 2 categories: 1) opioids, which included both “narcotic analgesics” and “narcotic analgesic combinations” (e.g. oxycodone/acetaminophen combinations); and 2) non-opioid analgesics, which included: non-steroidal anti-inflammatory (NSAID) medications and NSAID combination medications, and acetaminophen and acetaminophen combination medications. We did not include data on antimigraine mediations. Tramadol was classified as an opioid in our study.
Statistical Analysis
Analyses were conducted using the survey package of Stata version 14.2 (StataCorp, College Station, TX); α level was set at 0.05. We adjusted for the complex probability survey design of MEPS using sampling weights, stratification, and clustering to provide nationally representative estimates.
Our first aim was to determine whether racial and ethnic differences exist in rates of analgesic prescriptions to children in the USA in outpatient health care settings. To address this aim we first summarized unadjusted weighted rates of analgesic prescribing to children based on racial and ethnic categories over time between 2003 and 2014. In order to better visually present changes in analgesic use over time, each year between 2003 and 2014 was collapsed into one of 4 categories: 2003–2005; 2006–2008; 2009–2011, and 2012–2014. We then performed multivariate logistic regression analyses, controlling for age, sex, insurance coverage, region of the United States, parent-reported child mental and physical health, total number of outpatient health service visits, and number of medication prescriptions received, to estimate the association between child race and ethnicity and analgesic prescriptions. Separate logistic regression models were conducted for opioid and non-opioid analgesics.
Our second aim was to determine the associations between patient-provider race and ethnic concordance and opioid prescribing among children in the United States in the outpatient setting. To address this aim we first examined unadjusted weighted rates of opioid prescribing among children based on their provider’s race and ethnicity between 2003 and 2014. Bivariate analyses were conducted using chi-2 testing for equality of proportions between samples. We then performed multivariate logistic regression analyses to test associations controlling for age, sex, insurance, region, parent reported child mental and physical health, total number of outpatient health service visits, and number of medication prescriptions received. Separate multivariable logistic regressions were conducted for each of the 3 racial groups of children. In each of the 3 regression analyses, opioid prescribing by white providers were held as reference and compared with the child’s race-concordant health care provider, with the primary objective of determining whether race concordant providers were more likely to prescribe opioids to similar race child participants.
Results
Data from 113,929 children 0–17 years of age were available for analysis in the 2003–2014 Medical Expenditure Panel Survey database. Sociodemographic and parent-reported physical and mental health status characteristics of child participants are presented in Table 1. Race and ethnic status of children in the United States has changed between 2003 and 2014. In 2003 60% of children were white while in 2014 50% of children were white. The proportion of Hispanic children increased from 2003–2014, while the proportion of black children remained stable.
Table 1.
Sample characteristics: All children 0–18 years of age participating in MEPS (2003–2014). Source: Medical Expenditure Panel Surveys 2003–2014. *
| n (number of observations) | Weighted percentage (%) | Standard Error (se) | |
|---|---|---|---|
|
|
|||
| n (number of observations) | 113,929 | 100 | |
| Race and ethnicity | |||
| White, non-Hispanic | 38654 | 55.8 | 0.9 |
| Black, non-Hispanic | 23407 | 14.3 | 0.6 |
| Hispanic | 42113 | 22.0 | 0.9 |
| American Indian/Alaskan Native | 597 | 0.6 | 0.1 |
| Asian/Pacific Islander | 5447 | 4.5 | 0.3 |
| Multiple races reported | 3711 | 3.2 | 0.2 |
| Age category | |||
| < 6 year | 33217 | 29.0 | 0.3 |
| 6–11 years | 40658 | 34.8 | 0.2 |
| 12–17 years | 40054 | 36.1 | 0.3 |
| Sex | |||
| Male | 58139 | 51.0 | 0.3 |
| Female | 55790 | 49.0 | 0.3 |
| Insurance | |||
| Any private | 49942 | 60.9 | 0.7 |
| Public only | 55746 | 33.2 | 0.7 |
| Uninsured | 8241 | 5.8 | 0.2 |
| Region | |||
| Northeast | 16019 | 16.8 | 0.6 |
| Midwest | 21633 | 21.5 | 0.6 |
| South | 43577 | 37.3 | 0.8 |
| West | 32700 | 24.3 | 0.8 |
| Physical Health | |||
| Excellent | 54730 | 52.1 | 0.4 |
| Very Good | 33778 | 29.6 | 0.3 |
| Good | 21882 | 16.0 | 0.3 |
| Fair | 2987 | 2.0 | 0.1 |
| Poor | 383 | 0.3 | 0.0 |
| Missing | 169 | 0.02 | 0.0 |
| Mental Health | |||
| Excellent | 59133 | 55.3 | 0.5 |
| Very Good | 30731 | 26.8 | 0.3 |
| Good | 20594 | 15.3 | 0.3 |
| Fair | 2688 | 2.1 | 0.1 |
| Poor | 596 | 0.5 | 0.0 |
| Missing | 187 | 0.03 | 0.0 |
| Number of prescription medications received (mean, se) | 49877 | 2.5 | 0.0 |
| Number of outpatient healthcare visits (mean, se) | 76840 | 3.1 | 0.0 |
| Time period | |||
| 2003–2005 | 29242 | 24.8 | 0.6 |
| 2006–2008 | 27130 | 25.0 | 0.4 |
| 2009–2011 | 28053 | 25.2 | 0.4 |
| 2012–2014 | 29504 | 25.1 | 0.5 |
The sample contains 113,929 participants, which are weighted to represent 72 million children present in the United States annually.
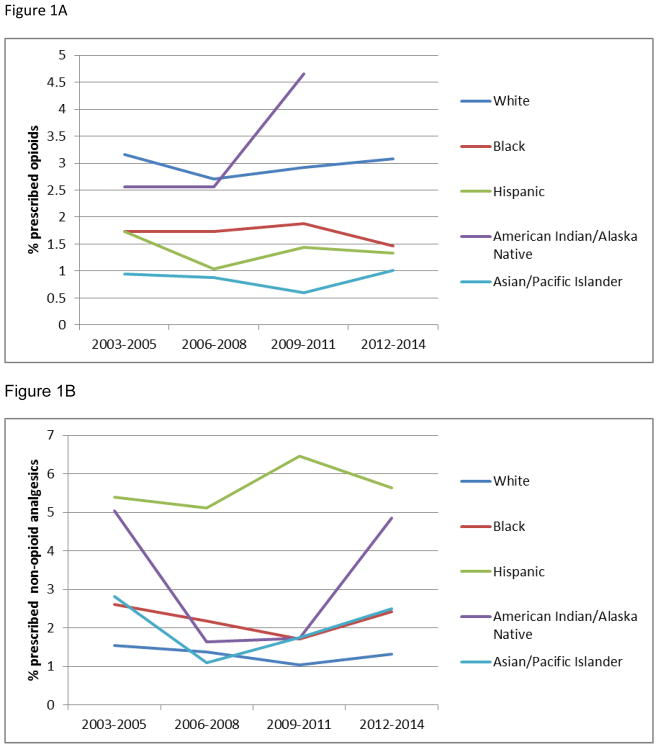
Analgesic prescribing over time by race and ethnicity
Rates of opioid and non-opioid analgesic prescribing over time, by each race and ethnic category, are presented in Figure 1. On average 2.3 % (95% confidence interval (CI), 2.2–2.5%) of children received an opioid prescription each year. We found higher rates of opioid prescribing to white children (annual average 3.0%; 95%CI, 2.7–3.2%) as compared to black children (annual average 1.7%; 95%CI, 1.5–2.0%), Hispanic children (annual average 1.4%; 95%CI, 1.2–1.6%) and Asian children (annual average 0.9%; 95%CI, 0.6–1.2%). Native American children had similar rates of opioid prescribing (2.6%; 95%CI, 1.5–4.3%) as compared to white children. In contrast, we found higher rates of non-opioid analgesic prescribing to minorities: black children (annual average 2.2%; 95%CI, 2.0–2.5%), Hispanic children (annual average 5.7%; 95%CI, 4.0–8.0%), Native American children (3.2%; 95%CI, 1.5–6.6%), and Asian children (annual average 2.0%; 95%CI, 1.5–2.7%), as compared to white children (annual average 1.3%; 95%CI, 1.2–1.5).
Figure 1.
Figure 1a. Rates of opioids prescribing to children 0–18 years of age by race and ethnic status in the United States. Source: MEPS 2003–2014. (*No opioids prescribed to American Indian/Alaskan Native children captured during 2012–2014)
Figure 1b. Rates of non-opioid analgesics prescribing to children 0–18 years of age by race and ethnic status in the United States. Source: MEPS 2003–2014.
Data from the multivariate logistic regression examining the association between race and ethnicity and analgesic prescribing to children are presented in Tables 2 and 3. Black children (adjusted OR (AOR)=0.6; 95%CI, 0.5–0.72), Hispanic children (AOR=0.5; 95%CI, 0.42–0.6), and Asian children (AOR=0.3; 95%CI, 0.21–0.46) had significantly lower odds of receiving opioids as compared to white children, after controlling for covariates. In contrast, black children (AOR=1.26; 95%CI, 1.01–1.56), Hispanic children (AOR=3.21; 95%CI, 2.27–4.56), and Asian children (AOR=1.72; 95%CI, 1.26–2.34) all had increased odds of receiving non-opioid prescriptions as compared to white children, after controlling for covariates.
Table 2.
Multivariate logistic regression testing the association between sample characteristics and opioid prescribing to children aged 0 to 17 years in the United States, from 2003 to 2014. Source: Medical Expenditure Panel Surveys 2003–2014.*
| Adjusted Odds Ratioα | [95% Confidence Interval] | p-value | |
|---|---|---|---|
|
|
|||
| Child race and ethnicity | |||
| White, non-Hispanic | reference | ||
| Black, non-Hispanic | 0.60 | 0.50–0.72 | <.0001 |
| Hispanic | 0.50 | 0.42–0.60 | <.0001 |
| American Indian/Alaska Native | 0.75 | 0.44–1.30 | 0.31 |
| Asian/Pacific Islander | 0.30 | 0.21–0.46 | <0.001 |
| Age category | |||
| <6 years | reference | ||
| 6–11 years | 1.13 | 0.95–1.37 | 0.184 |
| 12–17 years | 3.14 | 2.65–3.71 | <.0001 |
| Sex | |||
| Male | reference | ||
| Female | 1.07 | 0.94–1.22 | 0.27 |
| Insurance | |||
| Any private | reference | ||
| Public only | 0.95 | 0.82–1.09 | 0.46 |
| Uninsured | 0.43 | 0.30–0.62 | <.0001 |
| Region | |||
| Northeast | reference | ||
| Midwest | 1.41 | 1.11–1.77 | <.005 |
| South | 1.65 | 1.31–2.07 | <.0001 |
| West | 1.71 | 1.33–2.22 | <.0001 |
| Physical Health | |||
| Excellent | reference | ||
| Very good | 1.43 | 1.18–1.75 | <.0001 |
| Good | 1.62 | 1.32–2.00 | <.0001 |
| Fair | 2.14 | 1.44–3.18 | <.0001 |
| Poor | 1.62 | 1.90–3.33 | 0.190 |
| Mental Health | |||
| Excellent | reference | ||
| Very good | 0.76 | 0.64–0.92 | 0.004 |
| Good | 0.76 | 0.61–0.96 | 0.02 |
| Fair | 0.65 | 0.41–1.03 | 0.07 |
| Poor | 0.45 | 0.23–0.90 | 0.03 |
| Period | |||
| 2003–2005 | reference | ||
| 2006–2008 | 0.85 | 0.72–1.00 | 0.06 |
| 2009–2011 | 0.95 | 0.80–1.12 | 0.54 |
| 2012–2014 | 0.91 | 0.74–1.11 | 0.36 |
| Outpatient visits | 1.02 | 1.02–1.03 | <.0001 |
| Prescribed medications | 1.03 | 1.03–1.04 | <.0001 |
The sample contains 113,929 participants, which are weighted to represent 72 million children present in the United States annually
Odds ratios adjusted for all characteristics appearing in this table: race& ethnicity, age, sex, insurance, region, physical health, mental health, period.
Table 3.
Multivariate logistic regression testing the association between sample characteristics and non-opioid (acetaminophen and NSAIDS) prescribing to children aged 0 to 17 years in the United States, from 2003 to 2014. Source: Medical Expenditure Panel Surveys 2003–2014.*
| Adjusted Odds Ratioα | [95% Confidence Interval] | p-value | |
|---|---|---|---|
|
|
|||
| Child race and ethnicity | |||
| White, non-Hispanic | reference | ||
| Black, non-Hispanic | 1.26 | 1.01–1.56 | 0.04 |
| Hispanic | 3.21 | 2.27–4.56 | <.0001 |
| American Indian/Alaska Native | 1.62 | 0.71–3.68 | 0.24 |
| Asian/Pacific Islander | 1.72 | 1.26–2.34 | <0.005 |
| Age category | |||
| <6 years | reference | ||
| 6–11 years | 0.55 | 0.50–0.62 | <.0001 |
| 12–17 years | 0.89 | 0.75–1.05 | 0.16 |
| Sex | |||
| Male | reference | ||
| Female | 1.17 | 1.06–1.30 | <0.005 |
| Insurance | |||
| Any private | reference | ||
| Public only | 2.87 | 2.40–3.40 | <.0001 |
| Uninsured | 0.99 | 0.78–1.26 | 0.98 |
| Region | |||
| Northeast | reference | ||
| Midwest | 1.03 | 0.83–1.30 | 0.80 |
| South | 1.30 | 0.84–2.01 | 0.23 |
| West | 1.31 | 1.01–1.70 | 0.04 |
| Physical Health | |||
| Excellent | reference | ||
| Very good | 1.29 | 1.11–1.50 | <0.005 |
| Good | 1.68 | 1.41–2.00 | <.0001 |
| Fair | 1.40 | 1.06–1.83 | 0.02 |
| Poor | 0.80 | 0.40–1.70 | 0.6 |
| Mental Health | |||
| Excellent | reference | ||
| Very good | 0.88 | 0.76–1.02 | 0.96 |
| Good | 0.93 | 0.76–1.13 | 0.45 |
| Fair | 0.99 | 0.70–1.42 | 0.97 |
| Poor | 0.71 | 0.40–1.32 | 0.28 |
| Period | |||
| 2003–2005 | reference | ||
| 2006–2008 | 0.86 | 0.73–1.03 | 0.10 |
| 2009–2011 | 0.86 | 0.61–1.20 | 0.39 |
| 2012–2014 | 0.87 | 0.67–1.21 | 0.27 |
| Outpatient visits | 1.01 | 1.01–1.02 | <.0001 |
| Prescribed medications | 1.04 | 1.04–1.05 | <.0001 |
The sample contains 113,929 participants, which are weighted to represent 72 million children present in the United States annually
Odds ratios adjusted for all characteristics appearing in this table: race& ethnicity, age, sex, insurance, region, physical health, mental health, period.
Opioid prescription by usual source of care provider race and ethnic category
Child and provider race and ethnic concordance for participants who reported having a usual source of care provider is presented in Table 4. Most white children had race/ethnic concordant relationships with their usual source of care providers (93.5%), while 34.3% of black children and 42.7% of Hispanic children had race/ethnic concordant relationships with their health care providers. Among usual source of care providers, white providers were not more likely to prescribe opioids (2.9%) as compared to black (2.2%) and Hispanic (2.2%) providers (p=0.06).
Table 4.
Patient and provider race and ethnic concordance.
| White provider | Black provider | Hispanic provider | Total | |
|---|---|---|---|---|
| White child | 93.5 | 2.0 | 4.5 | 100 |
| Black child | 57.4 | 34.3 | 8.3 | 100 |
| Hispanic child | 53.3 | 4.0 | 42.7 | 100 |
| Total | 81.3 | 6.5 | 12.2 | 100 |
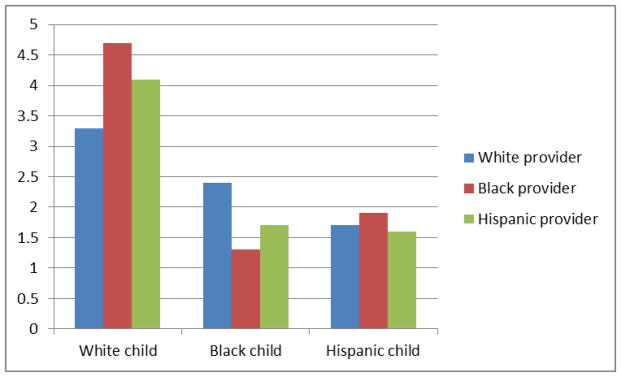
Unadjusted rates of opioid prescription to children based on patient and provider race and ethnicity are presented in Figure 2. We found that minority children who had a race-concordant relationship with their health care providers were no more likely to receive opioids than those with a non-concordant relationship. In fact, we found that minority children were less likely to receive opioids from minority providers. For example, as shown in the unadjusted rates presented in Figure 2, black children were less likely to receive opioids from black providers (1.3%) as compared to white providers (2.4%). Similarly, Hispanic children were also less likely to receive opioids from Hispanic providers (1.6%) as compared to white providers (1.7%). Of note, all providers were more likely to provide opioids to white children than black and Hispanic children.
Figure 2.
Unadjusted rates of opioid use by children based on provider race and ethnic status. Source: MEPS 2003–2014.
Multivariable logistic regression analyses examining associations between opioids and usual source of care provider characteristics, adjusting for covariates, are shown in Table 5. In the multivariate analysis of black children, we found that black children who had black providers were significantly less likely to receive opioids (AOR = 0.51; 95%CI, 0.30–0.87) as compared to black children who had white providers. The other two analyses involving white and Hispanic children did not reveal differences in opioid prescribing attributable to patient-provider concordance.
Table 5.
Multivariate logistic regression models examining associations between receipt of opioids and patient-provider race/ethnic concordance. (Source: Medical Expenditure Panel Surveys 2003–2014)
| Adjusted Odds Ratio¥ | 95% Confidence Interval | p-value | |
|---|---|---|---|
|
|
|||
| White, non-Hispanic child | |||
| White, non-Hispanic provider | (ref) | ||
| Black, non-Hispanic provider | 1.40 | 0.61–3.10 | 0.44 |
| Hispanic provider | 1.07 | 0.61–1.87 | 0.82 |
| Black, non-Hispanic child | |||
| White, non-Hispanic provider | (ref) | ||
| Black, non-Hispanic provider | 0.51* | 0.30–0.87 | 0.01 |
| Hispanic provider | 0.91 | 0.25–3.31 | 0.88 |
| Hispanic child | |||
| White, non-Hispanic provider | (ref) | ||
| Black, non-Hispanic provider | 1.26 | 0.34–4.66 | 0.72 |
| Hispanic provider | 1.14 | 0.77–1.70 | 0.51 |
Odds ratio’s adjusted for age, sex, insurance, region, physical health, mental health, period, number of outpatient visits, and number of prescribed medications.
p<0.05
Discussion
In this nationally representative cross-sectional analysis of outpatient visits of children in the United States, we found significant differences in opioid and nonopioid prescribing based on children’s race and ethnic status. We found that white children were more likely to receive opioid prescriptions as compared to minority groups, whereas minority children were more likely to receive non-opioid analgesic prescriptions, even after adjusting for important covariates including sociodemographic factors, physical and mental health, and healthcare use. The only minority group who received similar opioid prescriptions to white children was American Indian/Alaskan Native children.
Our data are consistent with published reports showing racial disparities in opioid prescribing during emergency department visits by children and adolescents in the United States [15; 17; 22]. Goyal et al. and Rasooly et al. found that black children were significantly less likely to receive opioid analgesics compared to white children, and this difference persisted after adjusting for pain severity and other demographic covariates. However, in these studies black children were more likely to receive non-opioid analgesia than white children [23; 6]. In contrast to emergency department findings, data from ambulatory surgery settings are inconsistent, with one study from the Pacific Northwest showing differences in opioid use based on race but a more recent study from the Midwest showing no difference in opioid use by race [16; 20]. However, both of these studies from ambulatory surgery centers were small, regional studies and not nationally representative. Our study is the first, to our knowledge, to document that race and ethnic differences in opioid prescribing to children exist in outpatient health care centers.
Potential reasons for differences in opioid prescription can be broadly categorized into those related to the patient and those related to health care providers. Patient-related factors include those related to clinical status and those related to patient preference. Many of the hypothesized patient-related clinical status risk factors related to opioids have not received empirical support. For example studies have demonstrated that non-white patients present to the ED with the same level of acuity as compared to white patients[3]. Patient preferences regarding analgesia have also been hypothesized to account for racial differences documented in analgesic prescriptions[13]. Recently, a study of adult patients in the ED found no significant difference by race in patients’ overall desire for analgesia[24], however race and ethnic differences exist for preference of type of analgesia. For example, Hispanic patients are more reluctant to use opioids as compared to white non-Hispanic patients because they are more concerned about risk for addiction, tolerance, and adverse treatment outcomes[21; 25; 19]. On the other hand, Hispanic and black patients are more likely to try over-the-counter medications (OTC) as compared to white patients[4; 25] Related, prescriptions for over-the-counter analgesics may be requested by families who have flexible spending accounts (FSA), which can be used to pay for OTC medications using pre-tax funds; however FSAs are much more likely to be utilized by white families compared to non-white families[9]. Thus, race and ethnic related preference for different types of analgesia could contribute to underlying racial differences in opioid use in outpatient settings.
Our findings also support the important role of healthcare provider factors in opioid differences among children. Some reasons for differences may include provider beliefs and implicit or explicit biases. For example, providers may believe that minorities are not able to obtain opioids because they are less likely to be carried by pharmacies in their areas[8]. Furthermore health care providers may have biases related to race. Hoffman et al. examined racial bias in pain assessment and treatment recommendations as a basis for disparities in pain treatment for black Americans relative to white Americans[12]. Their primary finding was that white individuals with at least some medical training hold and may use false beliefs about biological differences between black and white patients to inform medical judgments, which may contribute to racial disparities in pain assessment and treatment. Recently, Hollingshead et al. compared race-related stereotypes held by both white and black lay individuals[14]. They found that both white and black laypersons perceived the average white person to be more pain sensitive and more willing to report pain as compared to the average black person. Thus, their conclusion was that both white and black individuals hold similar racial stereotypes concerning pain and its management, which is consistent with previous studies [26; 5].
To better understand the effect of a provider factor in determining opioid disparities, the secondary aim of this study was to determine whether patient-provider race and ethnic concordance was associated with prescription of opioids to children. In contrast to our hypothesis, we did not find that children who have a race-concordant relationship with their health care provider were more likely to receive an opioid prescription as compared to children who were of different race/ethnicity than their provider. In fact, we found that, as a whole, minority children were less likely to receive opioids from minority healthcare providers. Given that minority persons are more reluctant to use opioids as a whole; our finding may indicate that minority health care providers are more perceptive to their minority patients preferring less opioids as compared to their white patients. On the other hand white patients may be more likely to request opioids from providers.Thus, our study contributes to understanding of health care provider related disparities in the United States by finding that race and ethnicity of health care providers may be a strong driver of opioid differences found among children in the United States These are novel findings that require further investigation to understand why provider racial concordance plays a role in differences related to opioid use.
Results should be considered within the context of several limitations of this study. First, we were unable to determine how many of the opioids prescribed to children actually came from their usual source of care providers since MEPS does not directly link providers to prescriptions. However, it is conceivable that most opioids given to children in outpatient settings would be from familiar providers (as opposed to opioids given following surgery or emergency department visits). Second, information was not available about children’s pain intensity, duration, and interference, or about the patient or parents’ desire for analgesia. Inclusion of those specifiers beyond just the presence or absence of a painful condition may have yielded additional information about the context for analgesia use. Third, because this is a secondary cross-sectional analysis of an existing database we are unable to causally link race, ethnicity, and opioid prescribing. Fourth, provider data to determine race and ethnic concordance were only available for a subsample of children and providers. Associations between race and opioid use were similar in the subsample as compared to the entire sample. Thus, we present data of the entire sample to address the first aim in this manuscript. Fifth, provider race was reported by the patient, thus there may be some imprecision related to patient’s ability to accurately perceive race. Despite these limitations, our study shows that there are significant racial and ethnic differences in opioid prescribing during outpatient health care visits among children and adolescents. These differences may be related to biases associated with patient-provider race and ethnic concordance, leading to differential pain management, and contributing to a wide gap in pain management provided to minorities. On the other hand, differences may be related to patient and provider preferences for opioid versus nonopioid medication use. Indeed, white individuals are much more likely to misuse opioids and have increased rates of opioid abuse and poisoning as compared to minorities [18]. This raises questions regarding whether, on a population level, opioids are over prescribed in white individuals or under prescribed in minority individuals. Our study was not designed to answer this fundamental question. However, for individual patients, we want to emphasize that health care providers should guard against inherent racial and ethnic biases and should personalize pain management decisions using best evidence practices. Furthermore, this study provides an important estimation of general analgesic prescribing among children in the United States that may guide future research and clinical service coordination for this vulnerable population.
Our study also has several strengths as compared to other epidemiological studies examining rates of opioid prescribing among children and adolescents: (1) we included a very large nationally representative sample spanning 2003–2014 rendering multiple years of data available for analysis, and (2) we analyzed prescriptions from the outpatient health care setting which has not been previously examined in children.
In summary, in a large, nationally representative database, we found differences in childhood opioid and nonopioid use based on race and ethnic differences. White children were significantly more likely to receive opioid prescriptions as compared to minorities. We also explored whether patient-provider race and ethnic concordance was associated with opioid prescribing. Overall, we found that providers were more likely to prescribe opioids to white children, while minority providers were less likely to prescribe opioids to minority children. Based on extant literature these findings may relate to minority patients’ known preference for using less opioid medications. Conversely, white patients may be more likely to request opioid medications for pain control. Future research should focus on understanding differences in preference for opioids based on race and ethnicity in the USA.
Acknowledgments
Jennifer Rabbitts was supported by National Institutes of Health K23HD078239. Tonya Palermo was partially supported by National Institutes of Health K24HD060068.
Footnotes
Conflict of interest statement
The authors report no conflict of interest
References
- 1. [[accessed] October 18, 2017];HealthPeople.gov. Available at: https://www.healthypeople.gov/
- 2.Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain. 2009;10(12):1187–1204. doi: 10.1016/j.jpain.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Ben-Isaac E, Schrager SM, Keefer M, Chen AY. National profile of nonemergent pediatric emergency department visits. Pediatrics. 2010;125(3):454–459. doi: 10.1542/peds.2009-0544. [DOI] [PubMed] [Google Scholar]
- 4.Carey TS, Freburger JK, Holmes GM, Jackman A, Knauer S, Wallace A, Darter J. Race, care seeking, and utilization for chronic back and neck pain: population perspectives. J Pain. 2010;11(4):343–350. doi: 10.1016/j.jpain.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dore RA, Hoffman KM, Lillard AS, Trawalter S. Children’s racial bias in perceptions of others’ pain. Br J Dev Psychol. 2014;32(2):218–231. doi: 10.1111/bjdp.12038. [DOI] [PubMed] [Google Scholar]
- 6.Goyal MK, Kuppermann N, Cleary SD, Teach SJ, Chamberlain JM. Racial Disparities in Pain Management of Children With Appendicitis in Emergency Departments. JAMA Pediatr. 2015;169(11):996–1002. doi: 10.1001/jamapediatrics.2015.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, Kalauokalani DA, Lasch KE, Myers C, Tait RC, Todd KH, Vallerand AH. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med. 2003;4(3):277–294. doi: 10.1046/j.1526-4637.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- 8.Green CR, Ndao-Brumblay SK, West B, Washington T. Differences in prescription opioid analgesic availability: comparing minority and white pharmacies across Michigan. J Pain. 2005;6(10):689–699. doi: 10.1016/j.jpain.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton BH, Marton J. Employee choice of flexible spending account participation and health plan. Health Econ. 2008;17(7):793–813. doi: 10.1002/hec.1296. [DOI] [PubMed] [Google Scholar]
- 10.Hirsh AT, Hollingshead NA, Ashburn-Nardo L, Kroenke K. The interaction of patient race, provider bias, and clinical ambiguity on pain management decisions. J Pain. 2015;16(6):558–568. doi: 10.1016/j.jpain.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirsh AT, Hollingshead NA, Bair MJ, Matthias MS, Wu J, Kroenke K. The influence of patient’s sex, race and depression on clinician pain treatment decisions. Eur J Pain. 2013;17(10):1569–1579. doi: 10.1002/j.1532-2149.2013.00355.x. [DOI] [PubMed] [Google Scholar]
- 12.Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci U S A. 2016;113(16):4296–4301. doi: 10.1073/pnas.1516047113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hollingshead NA, Ashburn-Nardo L, Stewart JC, Hirsh AT. The Pain Experience of Hispanic Americans: A Critical Literature Review and Conceptual Model. J Pain. 2016;17(5):513–528. doi: 10.1016/j.jpain.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hollingshead NA, Meints SM, Miller MM, Robinson ME, Hirsh AT. A comparison of race-related pain stereotypes held by White and Black individuals. J Appl Soc Psychol. 2016;46(12):718–723. doi: 10.1111/jasp.12415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hostetler MA, Auinger P, Szilagyi PG. Parenteral analgesic and sedative use among ED patients in the United States: combined results from the National Hospital Ambulatory Medical Care Survey (NHAMCS) 1992–1997. Am J Emerg Med. 2002;20(2):83–87. doi: 10.1053/ajem.2002.31578. [DOI] [PubMed] [Google Scholar]
- 16.Jimenez N, Seidel K, Martin LD, Rivara FP, Lynn AM. Perioperative analgesic treatment in Latino and non-Latino pediatric patients. J Health Care Poor Underserved. 2010;21(1):229–236. doi: 10.1353/hpu.0.0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson TJ, Weaver MD, Borrero S, Davis EM, Myaskovsky L, Zuckerbraun NS, Kraemer KL. Association of race and ethnicity with management of abdominal pain in the emergency department. Pediatrics. 2013;132(4):e851–858. doi: 10.1542/peds.2012-3127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCabe SE, West BT, Veliz P, McCabe VV, Stoddard SA, Boyd CJ. Trends in Medical and Nonmedical Use of Prescription Opioids Among US Adolescents: 1976–2015. Pediatrics. 2017;139(4) doi: 10.1542/peds.2016-2387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Monsivais DB, Engebretson JC. “I’m just not that sick”: pain medication and identity in Mexican American women with chronic pain. J Holist Nurs. 2012;30(3):188–194. doi: 10.1177/0898010112440885. [DOI] [PubMed] [Google Scholar]
- 20.Nafiu OO, Chimbira WT, Stewart M, Gibbons K, Porter LK, Reynolds PI. Racial differences in the pain management of children recovering from anesthesia. Paediatr Anaesth. 2017;27(7):760–767. doi: 10.1111/pan.13163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nguyen M, Ugarte C, Fuller I, Haas G, Portenoy RK. Access to care for chronic pain: racial and ethnic differences. J Pain. 2005;6(5):301–314. doi: 10.1016/j.jpain.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 22.Ortega HW, Vander Velden H, Lin CW, Reid S. Race, ethnicity, and analgesia provision at discharge among children with long-bone fractures requiring emergency care. Pediatr Emerg Care. 2013;29(4):492–497. doi: 10.1097/PEC.0b013e31828a34a8. [DOI] [PubMed] [Google Scholar]
- 23.Rasooly IR, Mullins PM, Mazer-Amirshahi M, van den Anker J, Pines JM. The impact of race on analgesia use among pediatric emergency department patients. J Pediatr. 2014;165(3):618–621. doi: 10.1016/j.jpeds.2014.04.059. [DOI] [PubMed] [Google Scholar]
- 24.Singer AJ, Garra G, Chohan JK, Dalmedo C, Thode HC., Jr Triage pain scores and the desire for and use of analgesics. Ann Emerg Med. 2008;52(6):689–695. doi: 10.1016/j.annemergmed.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 25.Townley S, Papaleontiou M, Amanfo L, Henderson CR, Jr, Pillemer K, Beissner K, Reid MC. Preparing to implement a self-management program for back pain in new york city senior centers: what do prospective consumers think? Pain Med. 2010;11(3):405–415. doi: 10.1111/j.1526-4637.2009.00783.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Trawalter S, Hoffman KM, Waytz A. Racial bias in perceptions of others’ pain. PLoS One. 2012;7(11):e48546. doi: 10.1371/journal.pone.0048546. [DOI] [PMC free article] [PubMed] [Google Scholar]