Abstract
Background
Hip fracture risk is high in young people with multiple sclerosis (MS), but has not been examined in an institutionalized aging population with MS.
Objective
We aimed to compare the hip fracture risk in nursing home (NH) residents with and without MS; and (2) examine risk factors for hip fracture in those with MS.
Methods
We conducted a retrospective cohort study using national NH clinical assessment and Medicare claims data. Participants included age-, sex- and race-matched NH residents with/without MS (2007–2008). Multivariable competing risk regression was used to compare 2-year hip fracture risk, and to examine risk factors.
Results
A total of 5,692 NH residents with MS were matched to 28,460 without MS. Approximately 80% of residents with MS vs. 50% of those without MS required extensive assistance in walking at NH admission. The adjusted incidence rate of hip fracture was 7.1 and 18.6 per 1,000 person-years in those with or without MS, respectively. Wandering and anxiolytic exposure were the main hip fracture risk factors in transfer independent residents with MS; while pneumonia and antidepressant use were the main factors in dependent residents with MS.
Conclusions
In contrast to prior comparisons from non-NH populations, the incidence of hip fracture was lower in NH residents with MS as compared with matched controls. Residents with MS were much more functionally dependent, which likely explains these findings. Fracture prevention strategies should focus on fall prevention in independent residents; and possibly improvement of health status and facility quality of care in dependent residents.
Introduction
Hip fractures are common in nursing home (NH) residents(1) and associated with functional dependence and elevated mortality.(2) Multiple sclerosis (MS) is a chronic, immune-mediated and degenerative disease of the central nervous system, characterized by disability progression over time.(3) People with MS typically experience early occurrence of fall and/or fracture risk factors, such as physical inactivity, impaired gait or balance, and lower bone mineral density;(4) and ‘accelerated aging’ through earlier presence of physical dependence and multiple comorbidities.(5) For these reasons, prior studies have reported that community dwellers with MS (mean age: <40 years) have a three-fold increase in hip fracture rates as compared to age- and sex-matched population without MS.(6, 7)
However, information remains limited regarding hip fracture incidence and risk factors in aging populations with MS, particularly those who are institutionalized. To date, only one study that was based on Danish national data concluded the incidence of hip fracture was >10 per 1,000 person years in persons 70-year-olds or older with MS.(8) Risk factors for hip fracture have been described in the general NH population, but have not been studied in NH residents with MS. Given the high burden of potentially long-term disability among institutionalized persons with MS, it is likely that unique risk factors for fracture exist in this frail population. Functional impairment has been shown to modify risk factors for injurious falls in general NH populations,(1) but it is unclear whether this is also true in residents with MS.
Efforts to reduce fracture risk among institutionalized aging populations with MS require a detailed understanding of the incidence of fracture and a better understanding of risk factors for fracture in this unique group. Therefore, we conducted this study to (1) compare the incidence of hip fracture between NH residents with and without MS; and (2) identify clinical characteristics associated with 2-year hip fracture risk in long-term NH residents with MS. Risk factor analyses were stratified by ability to transfer.
Methodology
Study design and data sources
This was a retrospective cohort study, linking 100% national Medicare fee-for-service (FFS) enrollment, Part A and Part D claims to the Minimum Data Set (MDS) version 2.0 between May 2007 and March 2010. The Part A claims data contain hospital admission and discharge dates, and diagnosis codes using International Classification of Diseases (ICD) ninth revision (ICD-9). The Medicare Part D file contains prescriptions dispensed at outpatient pharmacies. The MDS is a federally mandated needs assessment performed on all NH admissions and captures detailed clinical assessments for each resident at NH admission and quarterly thereafter, for as long as a resident remains in the NH.(9) Routinely collected data include demographics, physical and cognitive function, comorbid medical conditions, and health behaviors (e.g., use of tobacco). The reliability and validity of the MDS data is generally considered to be high.(10–12) Although MDS 2.0 currently has been replaced by version 3.0 throughout the U.S., version 2.0 is still used in many countries (e.g., Finland, Canada). The MDS was used to identify the study cohort with MS and risk factors for hip fractures. Ethical approval for this study was granted by the Institutional Review Board at Hebrew SeniorLife.
Study population
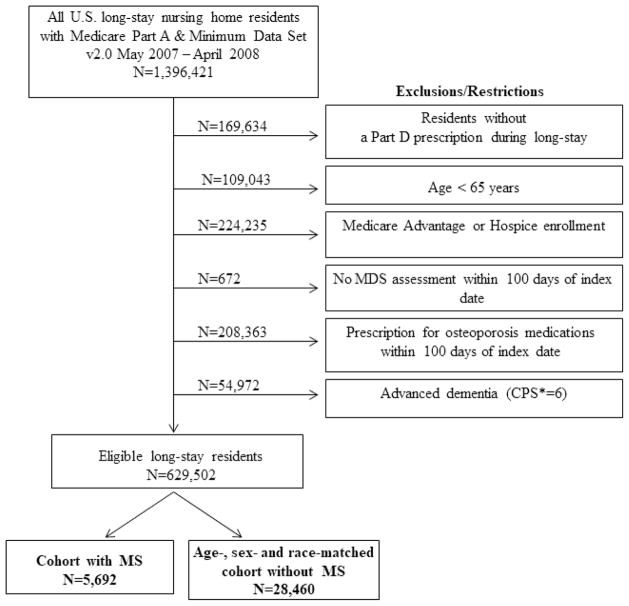
The study population included all newly admitted long-stay NH residents between May 2007 and April 2008. An individual qualified as a long-stay NH resident on day 100 (i.e., index date) after staying in the same nursing facility with no more than 10 consecutive days outside the facility. The 100-day period before the index date was referred as the baseline period. We required residents to have continuous enrollment in Medicare FFS Parts A and D, and at least one MDS assessment during the baseline period in order to permit assessment of risk factors for hip fractures. Approximately 3% of residents reported a hip fracture during the one year before the index date. We only counted the first hip fracture between the index date and the end of follow-up without a hospitalization for hip fracture in the previous 100 days, in order to be sure that we were excluding encounters for the follow-up care of a hip fracture (Figure 1).(13)
Figure 1.
Selection of study population
Residents with MS were identified using the medical condition checkbox of all available MDS assessments on or before the index date since 2000. The validity of using MDS to identify individuals with MS was well established, with a positive predictive value (PPV) of 0.65 and a negative predictive value of 1.(14) To account for differences in the demographics between NH residents with and without MS,(15) each resident with MS was matched to 5 residents without MS according to age, sex, and race on the index date.
The study population was followed from the index date, until the end of follow-up, defined as the first event of incident hip fracture, death, or March 31st, 2010 (end of the study period). All participants had the opportunity for 2-years of follow-up, but were censored on day 61 following a NH discharge.
Assessment of risk factors
Over 50 potential risk factors were selected based on prior literature and substantive clinical knowledge (4, 13) and categorized into 8 domains: demographic, cognitive/function, neuropsychiatric, falls, pain, nutrition, co-morbidities and prescription drugs. Potential risk factors under each domain are summarized in Table S1. This included, but was not limited to, the Cognitive Performance Scale (CPS), wandering, the Katz Activities of Daily Living (ADL) scale, walking in the room and self-transfer performance. Information from all domains except prescription drug use was obtained using the Medicare Enrollment File, Medicare Part A claims, or the MDS assessment closest to and preceding the index date. We considered prescription drugs that have been associated with an increased risk of falls or decreased bone mineral density (Table S1).(16) Drugs use was ascertained from Medicare Part D claims and defined as any dispensing during the baseline period.
Study outcomes
The outcome was presence of the first hospitalized hip fracture from the index date until the end of follow-up. A hospitalization for hip fracture was identified using a ICD-9 diagnosis code of 820.xx or 733.14 with or without an accompanying procedural code in the primary or secondary position on the Medicare Part A inpatient claims. The estimated PPV using a similar definition (without ICD-9 code 733.14) is 98%, with sensitivity of 97%.(17)
Statistical analysis
The incidence rates (IR) of hip fracture were calculated as the number of hip fractures divided by person-years of follow-up. We firstly calculated IR for hip fracture in our age-, sex- and race-matched cohort without adjusting for other covariates; then we calculated adjusted IR taking into account inverse probability weights estimated based on the presence of each of the characteristics described in the Risk Factors section above.(18) As physical function correlates with the disability of MS and may modify the relationships between other risk factors and hip fracture in MS,(19) we calculated the IR overall, as well as stratified by physical function indicated by self-transfer performance. The 95% confidence intervals (CI) were calculated based on the Gamma distribution.(20) Self-transfer performance is categorized in MDS version 2.0 as 5 categories according to performance in the past 7 days: no assistance required, requires setup help only, requires one person to physically assist, requires two or more persons to physically assist, and the activity did not occur (21). The first three categories were collapsed into the group of independent or mild assistance; while dependent was used to indicate the latter two categories.
Due to the high mortality following hip fracture events in NH, (22) we used the competing risk proportional hazards regression based on the Fine and Gray method(23) to compare the IR of hip fracture by MS status in the age-, sex- and race-matched cohort while accounting for the competing risk of death. We similarly used a Fine and Gray model to determine risk factors for hip fracture in the MS only cohort, adjusting for observed mortality. For both study aims, we initially used univariable models to examine the association between each characteristic and hip fracture risk. Characteristics associated with fracture (p≤0.05) in univariable models were entered into 8 domain-specific models (described above). Characteristics that were significant (p≤0.05) in domain-adjusted models were included in the final multivariable models that (1) compared hip fracture risk between MS and non-MS controls and (2) examined risk factors for hip fracture in residents with MS. These characteristics were also entered into a final stepwise selection model when examining the risk factors for hip fracture in MS. We used the same method to identify risk factors for residents with different level of self-transfer performance.
Stability analysis
A stability analysis was performed to test the robustness of our primary findings to decisions about the study design and analysis. We used an alternative hip fracture definition (Table S2) based on ICD diagnostic and procedural codes in both inpatient and outpatient (Part B) databases to identify hip fracture events that did not require hospitalization.
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS), Version 24.0., IBM Corp. Armonk, NY,(24) and SAS (v9.3).
Results
The study population included 5,692 long-stay NH residents with MS and 28,460 residents without MS. Baseline characteristics of the population are described in Table 1. Overall, 73.9% were female, 84.8% were white and 12.9% were black; the mean age was 76.5 years (SD 7.8). At baseline, a higher proportion of the MS cohort was physically dependent, but a lower proportion of the MS cohort exhibited wandering, was easily distracted, had a previous fall, Alzheimer’s Disease, dementia or schizophrenia as compared to those without MS (Table 1).
Table 1.
Summary of selected baseline characteristics
| Characteristics of study population | Persons with MS N=5,692 | Persons without MS N=28,460 | P value |
|---|---|---|---|
| Age, mean (SD), yrs | 76.5 (7.8) | 76.5 (7.8) | 0.96† |
| Sex, females, n (%) | 4,206 (73.9) | 21,030 (73.9) | 1.00§ |
| Race, n (%) | |||
| White | 4,827 (84.8) | 24,135 (84.8) | 1.00§ |
| Black or Hispanic | 732 (12.9) | 3,660 (12.9) | |
| Others | 133 (2.3) | 665 (2.3) | |
| * Duration of follow-up, yrs, mean (SD) | 1.7 (0.5) | 1.6 (0.6) | <0.001† |
| BMI, mean (SD), kg/m2 | 27.0 (6.2) | 28.0 (7.1) | <0.001† |
| Walking in the room, n (%) | <0.001§ | ||
| Independent/supervision | 713 (12.5) | 9,910 (34.8) | |
| Limited assistance | 401 (7.0) | 4,212 (14.8) | |
| Extensive assistance | 358 (6.3) | 2,949 (10.4) | |
| Dependent/total dependence | 4,220 (74.1) | 11,389 (40.0) | |
| Transfer performance, n (%) | <0.001§ | ||
| Independent/supervision | 746 (13.1) | 9,489 (33.3) | |
| Limited assistance | 588 (10.3) | 5,356 (18.8) | |
| Extensive assistance | 1,771 (31.1) | 8,832 (31.0) | |
| Total dependence | 2,587 (45.4) | 4,783 (16.8) | |
| || Presence of wandering, n (%) | 155 (2.7) | 2,400 (8.4) | <0.001§ |
| || Presence of easily distracted, n (%) | 633 (11.1) | 4,804 (16.9) | <0.001§ |
| || Presence of fall, 180 day before index, n (%) | 1,449 (25.5) | 10,815 (38.0) | <0.001§ |
| ¶ Presence of each comorbidity, n (%) | |||
| Pressure ulcer | 754 (13.2) | 1,934 (6.8) | <0.001§ |
| Anxiety | 1,001 (17.6) | 6,251 (22.0) | <0.001§ |
| Depression | 3,473 (61.0) | 16,998 (59.7) | 0.071§ |
| Schizophrenia | 235 (4.1) | 2,836 (10.0) | <0.001§ |
| Pneumonia | 582 (10.2) | 2,919 (10.3) | 0.96§ |
| Stroke | 1,385 (24.3) | 7,911 (27.8) | <0.001§ |
| Alzheimer’s disease | 423 (7.4) | 4,766 (16.7) | <0.001§ |
| Dementia, but not Alzheimer’s | 1,676 (29.4) | 10,922 (38.4) | <0.001§ |
| Prescription medication used, n (%) | |||
| Antidepressants | 3,326 (59.0) | 17,049 (61.0) | 0.006§ |
| Anxiolytics | 615 (10.9) | 3,519 (12.6) | <0.001§ |
| Anticonvulsants | 1,871 (33.2) | 8,571 (30.6) | <0.001§ |
| Antipsychotics | 1,133 (20.1) | 10,268 (36.7) | <0.001§ |
| Thyroid hormones | 1,133 (20.1) | 6,225 (22.3) | <0.001§ |
| Opioids | 1,963 (34.8) | 9,609 (34.4) | 0.52§ |
Study population was followed from the index date, until the first event of incident hip fracture, death, or March 31st, 2010 (end of the study period).
Comparison between MS and non-MS groups using Student’s t-test
Comparison between MS and non-MS groups using the Chi-square test
Missing<2% of observations. Study participants with missing values were coded as absence of a comorbidity.
Missing<1% of observations. Study participants with missing values were coded as absence of each condition.
A total of 90 residents with MS (1.6%) were hospitalized for hip fracture, and 1,405 (24.7%) died without hospitalized hip fracture during the follow-up. In the matched non-MS group, 917 (3.2%) had a hospitalization for hip fracture and 9,712 (34.1%) died without a hip fracture during the follow-up. The crude IR of hip fracture in residents with MS was 9.1 per 1,000 person-years (95% CI 7.3 – 11.2), and 19.9 per 1,000 person-years in those without MS (95% CI 18.6 – 21.2). The inverse probability weighting adjusted IRs for hip fracture was 7.1 per 1,000 person-years in MS (95% CI 5.6 – 9.1) as compared to 18.6 per 1,000 person-years in those without MS (95% CI 17.4 – 19.8, Table 2). IRs were higher in females, residents >75years, and in residents who were independent or requiring mild assistance in transfers in both residents with and without MS (Table 2). Within most subgroups, IRs were lower in residents with MS as compared with residents without MS. In residents requiring extensive or total dependence for transfers, IRs were similar regardless of MS status. When controlling for competing risk of mortality, hip fracture risk in MS residents was approximately 35% lower as compared with the non-MS group [adjusted hazard ratio (adjHR) 0.64; 95% confidence interval (CI) 0.51–0.80, Figure 1].
Table 2.
Two-year incidence rate of hip fracture in age-, sex- and race-matched MS and non-MS long-stay nursing home residents
| Persons with MS | Persons without MS | |||
|---|---|---|---|---|
| Hip fracture, n (%)1 | Adjusted IR2 (95% CI) | Hip fracture, n (%)1 | Adjusted IR2 (95% CI) | |
| Overall | 90 (1.6) | 7.1 (5.6 – 9.2) | 917 (3.2%) | 18.6 (17.4 – 19.8) |
| Age groups | ||||
| 65 – ≤75 years | 36 (1.3) | 6.8 (4.7 – 10.2) | 377 (2.8) | 15.5 (14.1 – 17.3) |
| >75 | 54 (1.8) | 9.3 (7.1 – 12.5) | 540 (3.6) | 22.0 (20.2 – 24.0) |
| Sex | ||||
| Women | 71 (1.7) | 8.2 (6.3 – 10.8) | 703 (3.3) | 19.3 (17.9 – 20.8) |
| Men | 19 (1.3) | 6.7 (4.2 – 11.5) | 214 (2.9) | 17.2 (15.1 – 19.8) |
| Self-transfer performance | ||||
| Independent/supervision | 23 (3.1) | 15.8 (10.5 – 24.8) | 423 (4.5) | 26.0 (23.6 – 28.7) |
| Limited assistance | 13 (2.2) | 12.5 (7.4 – 22.9) | 231 (4.3) | 26.5 (23.3 – 30.3) |
| Extensive assistance | 32 (1.8) | 10.2 (7.2 – 14.9) | 216 (2.4) | 15.4 (13.5 – 17.7) |
| Total dependence | 22 (0.9) | 5.0 (3.0 – 8.8) | 47 (1.0) | 5.4 (4.1 – 7.3) |
Percentages were calculated as the number of residents who had a hospitalization for hip fracture among each sex or self-transfer performance group.
IRs were calculated as the number of hospitalization for hip fracture per 1,000 person-years. Abbreviation: IR: incidence rate.
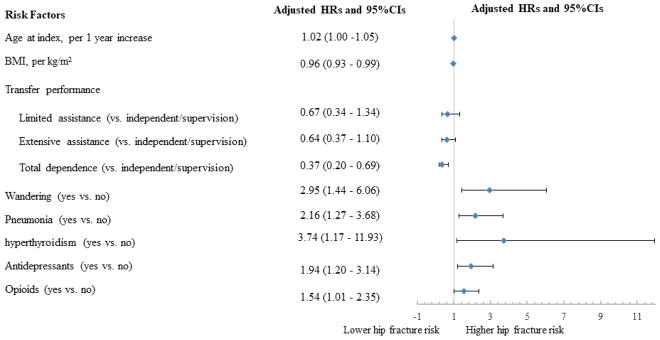
Eight characteristics were associated with hip fracture in the final multivariable model in the MS cohort: an increase in one-year of age [adjHR 1.02; 95% confidence interval (CI) 1.00–1.05)], transfer independence (e.g., adjHR 0.37; 95% CI 0.20–0.69), wandering (adjHR 2.95; 95% CI 1.44–6.06), pneumonia (adjHR 2.16, 95% CI 2.16; 1.27–3.68); hyperthyroidism (adjHR 3.74; 95% CI 1.17–11.93); antidepressant (adjHR 1.94; 95% CI 1.20–3.14) and opioid analgesic use (adjHR 1.54; 95% CI 1.01–2.35). Higher body mass index (BMI) was associated with lower hip fracture risk as compared to lower BMI (adjHR 0.96 per kg/m2; 95% CI 0.93–0.99), Figure 2).
Figure 2.
Factors associated with the 2-year risk of hip fracture among nursing home residents with multiple sclerosis in the final competing risk proportional hazard model (N=5,692)
Abbreviations: BMI, body mass index; kg, kilograms; m2, meters squared.
In the MS cohort independent or requiring mild assistance with transfers, low BMI, wandering and anxiolytic exposure were associated with elevated hip fracture risk in the final model (Table 3). In transfer dependent residents, hip fracture risk factors included macular degeneration, pneumonia, and the use of antidepressant and thyroid hormones (Table 3).
Table 3.
Patient characteristics associated with increased hip fracture risk by transfer performance in residents with MS: findings from final competing risk proportional hazard models
| Patient characteristics | Adjusted Hazard Ratios | 95% Confidence Intervals |
|---|---|---|
| Long-stay nursing home residents with MS with independent transfer performance | ||
| BMI, kg/m2 | 0.92 | 0.87 – 0.98 |
| Wandering | 3.24 | 1.42 – 7.40 |
| Alzheimer’s Disease | 2.75 | 1.33 – 5.71 |
| Anxiolytic drugs | 2.87 | 1.38 – 5.95 |
| Long-stay nursing home residents with MS with dependent transfer performance | ||
| Comorbid conditions | ||
| Hyperthyroidism | 8.65 | 2.70 – 27.73 |
| Pneumonia | 3.05 | 1.86 – 5.61 |
| Macular degeneration | 2.71 | 1.08 – 6.80 |
| Use of prescription drugs | ||
| Anticonvulsants | 1.73 | 1.01 – 2.96 |
| Antidepressants | 2.48 | 1.30 – 4.71 |
| Thyroid hormones | 2.44 | 1.40 – 4.24 |
| Systemic corticosteroids | 2.31 | 1.05 – 5.12 |
Abbreviation: BMI: body mass index.
Analyses based on the alternative hip fracture definition yielded results consistent with those of the primary analyses (Figure S1).
Discussion
This is the first study that examined hip fracture risk in an institutionalized older population with MS. In this population, the 2-year’s IR of hip fracture was found to be significantly lower as compared to the age-, sex-and race-matched population without MS. Older age, lower BMI, transfer dependence, wandering, comorbid pneumonia, and use of antidepressants or opioids were associated with increased hip fracture risk in MS. Risk factors varied by self-transfer dependence.
We reported an IR for hip fracture to be 7.1 per 1,000 person-years in our nursing home residents with MS. This incidence was lower than prior data from studies that examined fracture risk in younger patients with MS, in which hip fracture risk was three times higher in people with MS as compared those without MS.(6, 7) The IR of hip fracture in our study was also lower than the incidence (20 per 1,000 person years in females with MS over 70 years) reported in a Danish national MS registry study, the only previous study that described hip fracture risk in an aging population.(8) However, this Danish study also focused on community dwellers. This observed significant difference in hip fracture risk between our study and previous estimates is likely due to differences in patient characteristics at baseline. For instance, approximately 80% of residents with MS had significant functional impairment at the index date as compared to 50% of their matched counterparts. Less mobility may explain the lower prevalence of falls we observed in MS residents as compared with controls. Similarly, the prevalence of pressure ulcers in MS residents was twice a great as in the matched population without MS, again supporting the fact that the matched MS residents were considerably less mobile. However, a significantly larger proportion of residents without MS had a previous fall, schizophrenia or cognitive impairment, such as presence of Alzheimer’s Disease, dementia and wandering. These characteristics have been shown to elevate hip fracture risk in elderly admitted to nursing homes.(13) Our findings suggests that the increased opportunity for assistance with care and falls preventive strategies may reduce fracture risk in this institutionalized aging population with MS. Further studies are needed to evaluate whether similar assistance with care and falls preventive strategies as provided in NH facilities can be applied to community dwellers and the effectiveness of these interventions in younger people with MS.
Our study found that low BMI, transfer independence, wandering, and the use of antidepressants and opioids were found to be associated with increased hip fracture risk in long-stay NH residents with MS. Most of these factors have been implicated as risk factors for falls in previous studies involving non-MS NH populations.(25, 26) For instance, wandering was associated with a 7-fold increase in hip fracture risk in patients with Alzheimer’s disease.(27) Our findings further highlight the importance of applying fall prevention strategies in residents with MS who may already suffer from predisposed physical and cognitive impairment.
We found that fracture risk was highest in residents who were independent or requiring mild assistance with self-transfer. This is in contrast to findings from the Danish cohort study in which fracture risk was elevated in those who were disabled. In this study of community dwellers (mean age 36.9 years), disability, defined as Expanded Disability Status Scale (EDSS) scores between 6–10 as compared to with an EDSS score between 0 and 3, was associated with a nearly three-fold increased risk of fracture among incident MS patients.(8) Our study population was much older and supported in their activities of daily living by 24 hour NH staff which may explain the inverse association we observed. Further, our finding is consistent with the relationship between ADL dependence and hip fracture risk reported in the general NH population.(1)
Very few studies examined prescription drug use as risk factors for hip fracture in MS. Overall, our findings are consistent with previous studies based on national claims data in Dutch and United Kingdom populations with MS, in both of which, use of antidepressants was associated with increased hip fracture risk.(28, 29) Selective serotonin reuptake inhibitors, commonly used for depression, have been linked to disturbed sleep, insomnia, and daytime sleepiness.(30) We also found that residents with MS using an opioid medication were 1.5 times more likely to have hip fracture as compared to those without opioid use. This increased hip fracture risk may be attributable to the effects of chronic pain on falls risk,(31) and also the effects of the opioid medication.(32) Pain has been associated with elevated fall risk in elderly, due to pain-related muscle weakness and cognitive distraction.(31) Opioid exposure may result in sedative effects and reduced bone mineral density.(33) Over one-third of our study population received an opioid and approximately 60% received an antidepressant at baseline, and so these finding are of particular importance when considering fracture prevention in residents with MS.
A unique risk factor for hip fracture in our study population that was not shown in previous MS studies was pneumonia. Pneumonia has been associated with poor health status in older patients, which is further linked to greater hip fracture risk in elderly.(34) Additionally, as pneumonia is at least partially modifiable in NH residents due to vaccination, it has also been used as a quality of care indicator for long-term care facilities.(35) Thus the relationship we observed may be in part due to differences in the quality of care delivered to NH residents resulting in pneumonia. As pneumonia is more common in people with MS as compared to non-MS controls, and is one of the leading cause of death in MS,(36) our finding emphasizes the importance of pneumonia prevention in aging population with MS.
We found that risk factors for hip fracture varied depending on residents’ self-transfer performance. Lower BMI, wandering and anxiolytic use were associated with elevated hip fracture risk in those with more independence with self-transfer; while macular degeneration, pneumonia, antidepressant exposure and thyroid hormones were hip fracture risk factors in dependent residents. Our findings suggest that risk factors for falls may be the main factors driving hip fracture in independent residents; while risk in dependent residents may be influenced by poor health status and possibly facility quality of care factors.
Our study’s strengths include that it was a large, nationally representative sample of long-stay residents with MS and Medicare claims linked with the MDS. We examined a variety of potential clinical risk factors for hip fracture, such as physical and cognitive function, BMI, use of tobacco, which are typically unavailable in health claims database and have been rarely included in previous MS studies. There are also some limitations of our study. A number of factors were unavailable in our data, such as lifetime exposure to systemic corticosteroids, calcium and vitamin D. Our study sample was restricted to those aged 65 years and older with Medicare fee-for-service, in order to compare the incidence rate of fracture in a non-MS population. We recognize that persons with MS may enter the NH at a younger age, and our findings may not generalize to younger patients with MS. Finally, we did not have information on disease severity or clinical characteristic of MS that could be associated with fracture, such as MS disease course, duration or disability. However, we stratified our analyses based on self-transfer independence as a proxy of disability, as a previous study suggested that the EDSS had a great correlation with leg function.(37)
This retrospective cohort study found that the incidence rate of hip fracture was approximately 10 per 1,000 person-years in institutionalized residents with MS. Although hip fracture risk was lower than residents without MS, a key reason was that a significant proportion of residents with MS was functional dependent. These disabled patients may have complex healthcare needs and require specific health management. We also reported important risk factors for hip fracture in an aging population with MS. Fracture prevention efforts in older adults with MS should focus on those with low BMI, more independent on transfer, impaired cognitive function and those who are taking antidepressants and opioids. Fall preventive strategies need to be emphasized particularly for those independent residents. In dependent residents with MS, hip fracture prevention may be more related to the improvement of health status and NH facility quality of care, such as pneumonia prevention, reduce unnecessary antidepressants and opioid therapy.
Supplementary Material
Acknowledgments
Study Funding: This work was supported by the National Institute of Health (NIH), National Institute on Aging (NIA), #1R01AG045441 and #5P01AG027296-05. Dr. Zullo was funded by an Agency for Healthcare Research and Quality Award (5K12HS022998).
Footnotes
Disclosure: Drs. Zhang, McConeghy, Zullo and Daiello report no conflicts of interest. Ms. Lee and Liu report no conflicts of interest.
Dr. Shireman has received consulting fees from Pfizer, Inc., the University of Kansas Medical Center, and Temple University, on projects unrelated to the current project. Dr. Shireman receives grant funding from Insight Therapeutics and the National MS Society.
Dr. Mor holds stock of unknown value in PointRight, Inc. an information services company providing advice and consultation to various components of the long term care and post acute care industry, including suppliers and insurers. In addition, Dr. Mor chairs the Independent Quality Committee for HRC Manor Care, Inc., a nursing home chain, and serves as chair of a Scientific Advisory Committee for NaviHealth, a post-acute care service organization.
Dr. Kiel receives grant funding from Merck Sharp & Dohme and Policy Analysis, Inc and consulting fees from Merck Sharp & Dohme and Roivant unrelated to the current project.
Dr. Berry receives grant funding from Amgen.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Berry SD, Lee Y, Zullo AR, Kiel DP, Dosa D, Mor V. Incidence of Hip Fracture in U.S. Nursing Homes. J Gerontol A Biol Sci Med Sci. 2016;71(9):1230–4. doi: 10.1093/gerona/glw034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neuman MD, Silber JH, Magaziner JS, Passarella MA, Mehta S, Werner RM. Survival and functional outcomes after hip fracture among nursing home residents. JAMA Intern Med. 2014;174(8):1273–80. doi: 10.1001/jamainternmed.2014.2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tremlett H, Zhao Y, Rieckmann P, Hutchinson M. New perspectives in the natural history of multiple sclerosis. Neurology. 2010;74(24):2004–15. doi: 10.1212/WNL.0b013e3181e3973f. [DOI] [PubMed] [Google Scholar]
- 4.Tremlett H, Lucas R. The risks for falls and fractures in multiple sclerosis. Neurology. 2012;78(24):1902–3. doi: 10.1212/WNL.0b013e318259e2bf. [DOI] [PubMed] [Google Scholar]
- 5.Buchanan RJ, Wang S, Huang C, Graber D. Profiles of nursing home residents with multiple sclerosis using the minimum data set. Mult Scler. 2001;7(3):189–200. doi: 10.1177/135245850100700310. [DOI] [PubMed] [Google Scholar]
- 6.Dong G, Zhang N, Wu Z, Liu Y, Wang L. Multiple sclerosis increases fracture risk: a meta-analysis. Biomed Res Int. 2015;2015:650138. doi: 10.1155/2015/650138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Su S, Liu H. The association between multiple sclerosis and fracture risk. Int J Clin Exp Med. 2014;7(11):4327–31. [PMC free article] [PubMed] [Google Scholar]
- 8.Bazelier MT, de Vries F, Bentzen J, Vestergaard P, Leufkens HG, van Staa TP, et al. Incidence of fractures in patients with multiple sclerosis: the Danish National Health Registers. Mult Scler. 2012;18(5):622–7. doi: 10.1177/1352458511426739. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Medicare and Medicaid Services. MDS 2.0 for Nursing Homes. Centers for Medicare and Medicaid Services; 2012. Available from: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/NHQIMDS20.html. [Google Scholar]
- 10.Mor V, Angelelli J, Jones R, Roy J, Moore T, Morris J. Inter-rater reliability of nursing home quality indicators in the US. Bmc Health Serv Res. 2003;3(1):20. doi: 10.1186/1472-6963-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hawes C, Morris JN, Phillips CD, Fries BE, Murphy K, Mor V. Development of the nursing home Resident Assessment Instrument in the USA. Age and ageing. 1997;26(Suppl 2):19–25. doi: 10.1093/ageing/26.suppl_2.19. [DOI] [PubMed] [Google Scholar]
- 12.Mor V, Intrator O, Unruh MA, Cai S. Temporal and Geographic variation in the validity and internal consistency of the Nursing Home Resident Assessment Minimum Data Set 2.0. Bmc Health Serv Res. 2011;11(1):78. doi: 10.1186/1472-6963-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berry SD, Zullo AR, Lee Y, Mor V, McConeghy KW, Banerjee G, et al. Fracture Risk Assessment in Long-term Care (FRAiL): Development and Validation of a Prediction Model. J Gerontol A Biol Sci Med Sci. 2017 doi: 10.1093/gerona/glx147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lix LM, Yan L, Blackburn D, Hu N, Schneider-Lindner V, Teare GF. Validity of the RAI-MDS for ascertaining diabetes and comorbid conditions in long-term care facility residents. BMC Health Serv Res. 2014;14:17. doi: 10.1186/1472-6963-14-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buchanan RJ, Wang S, Ju H. Analyses of the minimum data set: comparisons of nursing home residents with multiple sclerosis to other nursing home residents. Multiple sclerosis. 2002;8(6):512–22. doi: 10.1191/1352458502ms823oa. [DOI] [PubMed] [Google Scholar]
- 16.Munson JC, Bynum JP, Bell JE, Cantu R, McDonough C, Wang Q, et al. Patterns of Prescription Drug Use Before and After Fragility Fracture. JAMA Intern Med. 2016;176(10):1531–8. doi: 10.1001/jamainternmed.2016.4814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ray WA, Griffin MR, Fought RL, Adams ML. Identification of fractures from computerized Medicare files. J Clin Epidemiol. 1992;45(7):703–14. doi: 10.1016/0895-4356(92)90047-q. [DOI] [PubMed] [Google Scholar]
- 18.Mansournia MA, Altman DG. Inverse probability weighting. BMJ. 2016;352:i189. doi: 10.1136/bmj.i189. [DOI] [PubMed] [Google Scholar]
- 19.Smee DJ, Anson JM, Waddington GS, Berry HL. Association between Physical Functionality and Falls Risk in Community-Living Older Adults. Curr Gerontol Geriatr Res. 2012;2012:864516. doi: 10.1155/2012/864516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fay MP, Feuer EJ. Confidence intervals for directly standardized rates: a method based on the gamma distribution. Stat Med. 1997;16(7):791–801. doi: 10.1002/(sici)1097-0258(19970415)16:7<791::aid-sim500>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 21.Minimum Data Set (MDS) - Version 2.0 For Nursing Home Resident Assessment and Care Screening. Basic Assessment Tracking Form. Available at: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/downloads/MDS20MDSAllForms.pdf+&cd=1&hl=en&ct=clnk&gl=us.
- 22.Becker DJ, Arora T, Kilgore ML, Curtis JR, Delzell E, Saag KG, et al. Trends in the utilization and outcomes of Medicare patients hospitalized for hip fracture, 2000–2008. J Aging Health. 2014;26(3):360–79. doi: 10.1177/0898264313516994. [DOI] [PubMed] [Google Scholar]
- 23.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. Journal of the American Statistical Association. 1999;94:496–509. [Google Scholar]
- 24.IBM Corp. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp; Released 2016. [Google Scholar]
- 25.Kiely DK, Kiel DP, Burrows AB, Lipsitz LA. Identifying nursing home residents at risk for falling. J Am Geriatr Soc. 1998;46(5):551–5. doi: 10.1111/j.1532-5415.1998.tb01069.x. [DOI] [PubMed] [Google Scholar]
- 26.Teng Z, Zhu Y, Wu F, Zhu Y, Zhang X, Zhang C, et al. Opioids contribute to fracture risk: a meta-analysis of 8 cohort studies. PLoS One. 2015;10(6):e0128232. doi: 10.1371/journal.pone.0128232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buchner DM, Larson EB. Falls and fractures in patients with Alzheimer-type dementia. Jama. 1987;257(11):1492–5. [PubMed] [Google Scholar]
- 28.Bazelier MT, van Staa TP, Uitdehaag BM, Cooper C, Leufkens HG, Vestergaard P, et al. Risk of fractures in patients with multiple sclerosis: a population-based cohort study. Neurology. 2012;78(24):1967–73. doi: 10.1212/WNL.0b013e318259e0ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bazelier MT, van Staa T, Uitdehaag BM, Cooper C, Leufkens HG, Vestergaard P, et al. The risk of fracture in patients with multiple sclerosis: the UK general practice research database. J Bone Miner Res. 2011;26(9):2271–9. doi: 10.1002/jbmr.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Darowski A, Chambers SA, Chambers DJ. Antidepressants and falls in the elderly. Drugs Aging. 2009;26(5):381–94. doi: 10.2165/00002512-200926050-00002. [DOI] [PubMed] [Google Scholar]
- 31.Leveille SG, Jones RN, Kiely DK, Hausdorff JM, Shmerling RH, Guralnik JM, et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009;302(20):2214–21. doi: 10.1001/jama.2009.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller M, Sturmer T, Azrael D, Levin R, Solomon DH. Opioid analgesics and the risk of fractures in older adults with arthritis. J Am Geriatr Soc. 2011;59(3):430–8. doi: 10.1111/j.1532-5415.2011.03318.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Daniell HW. Opioid osteoporosis. Arch Intern Med. 2004;164(3):338. doi: 10.1001/archinte.164.3.338-a. author reply. [DOI] [PubMed] [Google Scholar]
- 34.Unnanuntana A, Gladnick BP, Donnelly E, Lane JM. The assessment of fracture risk. J Bone Joint Surg Am. 2010;92(3):743–53. doi: 10.2106/JBJS.I.00919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Montoya A, Mody L. Common infections in nursing homes: a review of current issues and challenges. Aging health. 2011;7(6):889–99. doi: 10.2217/AHE.11.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Marrie RA, Elliott L, Marriott J, Cossoy M, Blanchard J, Tennakoon A, et al. Dramatically changing rates and reasons for hospitalization in multiple sclerosis. Neurology. 2014;83(10):929–37. doi: 10.1212/WNL.0000000000000753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoogervorst EL, Kalkers NF, Uitdehaag BM, Polman CH. A study validating changes in the multiple sclerosis functional composite. Arch Neurol. 2002;59(1):113–6. doi: 10.1001/archneur.59.1.113. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.