Abstract
Background
Hypotension is a common problem in general anesthesia. Maintaining the mean arterial pressure by choosing a vasopressor with minimal complications is still discussed in various surgeries.
Objectives
The aim of this study is comparison of ephedrine versus norepinephrine in treating anesthesia-induced hypotension in hypertensive patients in spinal surgery in a randomized double-blinded study.
Methods
This randomized, double-blinded study was approved by Iran University of Medical Sciences, operating room of medical center. Data collection was completed between Jan to Dec 2017. Inclusion criteria included age between 20 and 75 years, history of high blood pressure (a patient who has been treated for maximum 5 years with a anti hypertensive medication), and patients under general anesthesia in spinal surgery. The exclusion criteria were based on American Society of Anesthesiologists physical status of 3 or higher, history of arrhythmia, heart valve disease, cerebrovascular disease, kidney failure, beta-blocker use and diabetes, as well as intra operative massive blood loss. After initiation of anesthesia, when the pressure reaches less than 60, the patient entered the protocol and simultaneously administration of 5 mL/kg serum crystalloid and vasopressor. Patients were randomized to the ephedrine group (n = 28) who received 5 mg ephedrine intravenous (i.v.) or norepinephrine Group (n = 28) who received 10 µg (i.v.) bolus norepinephrine at anesthesia-induced hypotension. The administration of 5 mL/kg serum crystalloid and vasopressor was simultaneous. If the mean arterial pressure (MAP) had not reached 60 mmHg, the same dose should be repeated at a maximum of three or more times at five-minute intervals in the ephedrine group and at two minutes intervals in the norepinephrine group. All parameters were collected before and at the end of administration anesthesia drug and during episodes of hypotension. Hemodynamic variables, frequency of hypotension, and total number of vasopressors doses during anesthesia were recorded and analyzed.
Results
The mean number of hypotension times, the number of vasopressors doses in the first hypotension, the total number of doses consumed during the anesthesia, and heart rate at the end of anesthesia were lower in the norepinephrine group (P) respectively. MAP, 5 minutes after the first episode of hypotension and MAP at the end of anesthesia were higher in norepinephrine group.
Conclusions
Norepinephrine is more effective than ephedrine in maintenance of MAP in hypertensive patients undergoing spinal surgery under general anesthesia.
Keywords: Ephedrine, Norepinephrine, Hypotension, MAP, General Anesthesia
1. Background
Hypotension is a common problem in both general and spinal anesthesia (1-5). It has a prevalence between 5% to 99% and requires intervention in about two thirds of the cases (6). Intraoperative hypotension is usually defined as a mean arterial pressure less than 25% of the patient’s normal value. Intraoperative hypotension might lead to ischemia of vital organs (3). In severe cases, it is an emergency and requires rapid treatment, especially in pregnancy. Should it be left untreated, it can lead to nausea, vomiting, dizziness, decreased consciousness, stroke, myocardial infarction, acute tubular necrosis, and in obstetric surgeries, decreased uteroplacental blood flow, impaired fetal oxygenation with asphyxial stress, and fetal acidosis (1, 5, 7, 8). On the other hand, it leads to longer hospital stays, higher post operative morbidity and mortality (3). Hypertensive patients are at an increased risk of intraoperative hypotension. Some other conditions such as Addison’s disease, hypothyroidism, and carcinoid syndrome might increase the risk of intraoperative hypotension. Risk factors include chronic hypertension and advanced age (7). An effective way to treat intraoperative hypotension is intravascular administration of vasopressor (pressor agent) delivered by bolus or continuous infusion (2, 4). Vasopressors act by reversing sympathetic block in circulation. They also restore vascular tone and maintain venous return and cardiac filling (9). Vasopressors might cause adverse effects such as increased arterial stiffness, increased myocardial work, decreased stroke volume, and decreased arterial compliance (10). Ephedrine is considered a vasopressor of choice, especially in obstetric surgery (2, 11-13). However, ephedrine has some several adverse effects; it causes arrhythmia (10). Intraoperative hypotension is usually attributted to anesthetic agents causing reduction of cardiac output and systemic vascular resistance by a variety of mechanisms (2, 7). Spinal anesthesia induces hypotension by reduction of cardiac preload (6). Ephedrine has sympathomimetic effects on the heart. It improves preload, increases cardiac output, increases blood pressure and heart rate, and causes mild arteriolar constriction (11, 14, 15). However, ephedrine has several adverse effects; it causes arrhythmia (10). Recent studies suggest that norepinephrine may represent a valuable alternative to general anesthesia-induced hypotension, however, information in this area is not sufficient (2, 11). A few studies suggest a beneficial effect of norepinephrine compared to other vasoperssors in patients having cesarean delivery (9) and chronic pulmonary hypertension (16). In Vos and colleagues’ study, stable hemodynamic condition with maintaining tissue saturation has been created with bolus of norepinephrine at a dose of 10mg during anesthesia during eye surgery in patients with heart disease (17). Maintaining the mean arterial pressure by choosing a vasopressor with minimal complications is still discussed in various surgeries. The aim of this study is comparison of ephedrine vs. norepinephrine in treating anesthesia-induced hypotension in hypertensive patients in spinal surgery in a randomized double-blinded study.
2. Methods
2.1. Patients
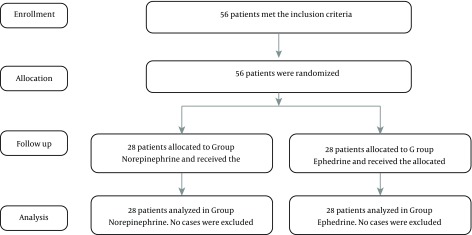
This randomized, double-blinded study was approved by Iran University of Medical Sciences (Tehran, Iran), Clinical Research Ethics Committee of Iran University of Medical Sciences, Iran (IR.IUMS.REC 1396.9311174021 ), and was registered in the Iran Clinical Trial Registry (registration No. IRCT20180110038296N1). All of the patients gave written informed consent to participate. The study was conducted in the operating rooms in the spinal surgery ward of Rasoul Akram teaching hospital. Data collection was completed between Jan to Dec 2017. In this study, sample selection was based on simple random sampling (available). Sample size was determined on 28 hypertensive patients and generally 56 patients in 2 groups were studied. Then eligible patients using table of random numbers were allocated to two groups, even numbers allocated to ephedrine intervention, and odd numbers allocated to norepinephrine intervention (Figure 1). Inclusion criteria individuals between the ages of 20 and 75 years, history of high blood pressure, and patients under general anesthesia in spinal surgery. The exclusion criteria were based on American Society of Anesthesiologists physical status of 3 or higher, history of arrhythmia, heart valve disease, cerebrovascular disease, kidney failure, beta-blocker use and diabetes, as well as intra operative massive blood loss.
Figure 1. Flowchart of the study.
2.1.1. Patient Hemodynamic Monitoring
In our center, spinal surgical patients are monitored thermodynamically, combining invasive arterial pressure via a radial artery catheter. A device, which allowed simultaneous recording of both arterial pressures, was used (Alborz B5, Saadat, Iran).
2.1.2. Collected and Calculated Parameters
Mean arterial pressure (MAP) from the invasive and noninvasive arterial blood pressure and heart rate (HR).
All these parameters were collected before and at the end of administration anesthesia drug and during episodes of hypotension.
2.2. Study Protocol
Patients in the operating room were monitored by pulse oximetry and electrocardiography and a peripheral venous catheter was inserted. All patients were pre-medicated with Midazolam (0.03 mg/kg), Fentanyl (2 µg/kg), and Ringer’s solution (5 mL/kg), and anesthesia was induced by Propofol (2 mg/kg) and then Cisatracurium (0.25 mg/kg) and after, intubation mechanical ventilation with continuous mandatory ventilation (CMV) mode was done. Anesthesia was maintained with Propofol (up to 100 µg/kg per minute) based on the patients age, weight, ASA physical status and blood pressure, and cisatracurium (2 mg per 40 minutes). Intra venous fluids and blood products were given as much as necessary. Urinary catheter, capnograph, and arterial line from radial artery were inserted. After initiation of anesthesia, when the pressure reaches less than 60, the patient entered the protocol and simultaneously administration of 5 mL/kg serum crystalloid and vasopressor.
2.2.1. Ephedrine Group
They received 1 mL intravenous ephedrine with density of 5 mg/mL and MAP was checked after 5 minutes. If it had not reached 60 mmHg, the same dose should be repeated at a maximum of three times at five-minute interval. The used ephedrine was a product of the Sterop Company in Belgium containing 50 mg of the agent in 1 mL vials.
2.2.2. Norepinephrine Group
They received 1 mL bolus intravenous norepinephrine with density of 10 µg/mL and MAP was checked after 2 minutes. If it had not reached 60 mmHg, the same dose should be repeated at a maximum of three times at two-minute interval. The used norepinephrine was a product of Normon S.A Company in Spain containing 10 mg of the agent in 10 mL vials.
In every MAP that fell below 60 mmHg during anesthesia, this protocol was repeated. In both groups, after 3 times injection, if MAP had not reached 60 mmHg it should be corrected with another method. Vasopressors were administrated via a peripheral venous catheter.
2.3. Blinding
Hypertensive patients are randomly assigned to test groups. To maintain blinding of both patients and examiner throughout the study, syringes for each patient were prepared by a doctor or nurse not involved in the subjects or recording data of the patients. No patient or examiner person is aware of which drug the patient receives.
2.3.1. Statistical Analysis
Sample size was determined based on the previous recommendation by Lecoq et al. (12), based on the results of Lecoq and colleagues’ study. Univariate data were assessed for normality using the Kolmogorov-Smirnov test and were compared between the patients who received norepinephrine and those who received ephedrine using student’s t-test or the Mann-Whitney U test, as appropriate. Final analyses were done using repeated measures ANOVA. A two-sided P value of 0.05 was considered significant. These analyses were performed using IBM SPSS statistics for Windows version 22 (IBM Corp., USA).
3. Results
A total of 56 hypertensive patients were enrolled in a randomized double-blinded study. They were randomly allocated into two equal groups (28 patients). All patients received the allocated interventions and were available for statistical analysis in both groups.
The ratio of men to women in the ephedrine group was 13/15 and in the epinephrine group 14/14. Gender differences in groups were not significantly different (P = 0.05). Mean age, weight, BMI, blood glucose before anesthesia, intraoperative bleeding, and duration of anesthesia did not differ significantly between two groups (Table 1). Characteristics of these patients are shown in Table 1.
Table 1. Demographic and Patient Characteristics in the Study Groupsa.
| Ephedrine Group (N = 28) | Norepinephrine Group (N = 28) | P Value | |
|---|---|---|---|
| Age | 57.85 ± 15.62 | 58.14 ± 10.9 | 0.937 |
| Weight | 76.78 ± 13.21 | 72.64 ± 10.06 | 0.193 |
| Body mass index | 27.44 ± 3.78 | 26.28 ± 3 | 0.209 |
| Blood glucose before anesthesia | 139.6 ± 35.82 | 148.6 ± 42.66 | 0.396 |
| Intraoperative hemorrhage | 919.64 ± 859.62 | 621.42 ± 375.01 | 0.774 |
| Anesthesia duration | 269.64 ± 100.2 | 280 ± 95.37 | 0.52 |
a Values are expressed as mean ± SD.
Table 2 shows the mean number of first hypotension, the number of doses at first hypotension after anesthesia in two groups, the results of this test indicate that the mean number of hypotension times, the number of doses in the first hypotension, and the total number of doses consumed. During the anesthesia, there was a significant difference between two groups (P = 0.005), (P < 0.001), and (P = 0.004), respectively.
Table 2. Comparison of Hypotension Variable in Response to Anesthesia in the First Time in Two Treatment Groupsa.
| Ephedrine Group (N = 28) | Norepinephrine Group (N = 28) | P Value | |
|---|---|---|---|
| Frequency of hypotension | 1.25 ± 0.44 | 1 ± 0 | 0.005 |
| Interval between the start of anesthesia and the first hypotension | 83.93 ± 64.7 | 85.35 ± 40.86 | 0.922 |
| Number of consumed dose at first episode | 1.92 ± 0.76 | 1.1 ± 0.31 | > 0.001 |
| Total number of doses during anesthesia | 2.39 ± 1.25 | 1.6 ± 1.1 | 0.004 |
| MAP at first dose | 48.82 ± 11.67 | 49.46 ± 5.9 | 0.79 |
| MAP 5 minutes after first dose | 59.1 ± 12.19 | 71.53 ± 8.94 | < 0.001 |
| MAP 5 minutes after second dose | 64.42 ± 19.96 | 72.33 ± 10.69 | 0.393 |
| MAP 5 minutes after third dose | 76.14 ± 11.56 | 62 ± 0 | 0.296 |
| HR at first dose | 72.1 ± 19.76 | 64.1 ± 10.88 | 0.066 |
| HR 5 minutes after first dose | 78.35 ± 14.54 | 78.07 ± 11.63 | 0.936 |
| HR 5 minutes after second dose | 81.1 ± 18.32 | 79.67 ± 16.8 | 0.9 |
| HR 5 minutes after third dose | 83.42 ± 19.85 | 83 ± 0 | 0.985 |
Abbreviations: HR, heart rate; MAP, mean arterial pressure.
a Values are expressed as mean ± SD.
Also, Table 2 shows the mean arterial pressure (MAP) and heart rate in the first episode of hypotension 5 minutes after the first, second, and third dose after administration drug. The result of this test showed that the mean MAP, 5 minutes after the first episode of hypotension, was significantly different in two groups (P < 0.001); other variables were not significantly different.
The results showed that MAP had a significant difference in the beginning (P = 0.020) and at the end of (P < 0.001) anesthesia and HR at the end of anesthesia (P = 0.012) in the two groups (Table 3)
Table 3. Comparison of Mean Arterial Pressure and Heart Rate in Two Treatment Groups in Start and End of Anesthesiaa.
| Ephedrine Group (N = 28) | Norepinephrine Group (N = 28) | P Value | |
|---|---|---|---|
| Beginning of anesthesia | |||
| MAP | 101.78 ± 16.64 | 101.28 ± 12.62 | 0. 020 |
| HR | 75.78 ± 10.11 | 71.35 ± 10.86 | 0.12 |
| At the end of anesthesia | |||
| MAP | 91.48 ± 10.93 | 98.85 ± 12.65 | < 0.001 |
| HR | 77.5 ± 9.22 | 70.5 ± 10.75 | 0.012 |
Abbreviations: HR, heart rate; MAP, mean arterial pressure.
a Values are expressed as mean ± SD.
There was no significant difference in response to treatment in study groups (P = 0.50)
4. Discussion
So far, many studies have been conducted on the comparison of drugs in low blood pressure. (18-21). However, our study (based on our knowledge) was the first study that compared the administration of intravenous boluses of norepinephrine and ephedrine to treat anesthesia-induced hypotension in hypertensive patients in the randomized double-blinded study.
During spinal surgery, we found that MAP was significantly lower in the norepinephrine group. Furthermore, the numbers of boluses of vasopressors used during anesthesia were lower in norepinephrine group compared with the use of ephedrine group. For preventing and treating hypotension of general anesthesia, vasopressors are effective. In the present study, ephedrine and norepinephrine were used as vasopressors. Ephedrine is a common vasopressor, it is safe, available, and comfortable to most anesthesiologists. Ephedrine has a sympathomimetic effect and causes positive inotropic and chronotropic effects on the heart. Its effect is both direct (α- and β-receptor agonist) and indirect (catecholamine, namely norepinephrine release). It improves preload, increases cardiac output, increases blood pressure and heart rate, and causes mild arteriolar constriction (11, 14, 15). Repeated administration of ephedrine diminishes its vasoconstrictive effect. It has a slow onset of action (11). Ephedrine can cause tachycardia, tachyphylaxis, and hypertension (2, 22). In the results of this study, ephedrine increased mean arterial pressure, however, compared to the effect of norepinephrine, it was weak. In addition, the number of episodes of hypotension was higher and the total number of doses consumed related to norepinephrine was more. Norepinephrine is considered as an ideal alternative to ephedrine without the adverse effects (11, 23, 24). It is more effective than ephedrine, however, it is more difficult to administrate (25). Norepinephrine is a weak β-adrenergic and potent α-adrenergic receptor agonist (11). It causes an arterial and venous vasoconstriction and improves venous return and cardiac preload.
Vallee et al. (2), showed that a dosage of 5 µg/mL of norepinephrine can be used as a vasopressor with no adverse effects. Our result was consistent with the results of Vallee et al.
Ali Elnabtity et al. (11), compared Intra venous boluses of norepinephrine and ephedrine to treat hypotensive effect of spinal anesthesia during cesarean delivery. They showed that norepinephrine maintained the maternal blood pressure and uterine artery blood flow better than ephedrine. Norepinephrine also caused less hypotension and hypertension episodes and less frequency of bradycardia and tachycardia; it also requireda less number of boluses. Although our doses were not exactly like this study, the results of this study were similar. In agreement with these results, in the present study, norepinephrine reduced the frequency of episode hypotension and increased the mean arterial pressure and mean number of boluses.
El Shafei et al. (26), showed that norepinephrine is effective in maintaining systolic blood pressure with reduction in heart rate, which is useful in coronary artery disease patients. In a recent investigation, we found similar results in relation to patients with spinal surgery.
Moran et al. (27), in treatment anesthesia induced hypotension, suggested that 5 - 10 mg boluses of ephedrine is comparable to 40 - 80 µg of phenylephrine. In comparison with this study, the treatment of hypertension in these observations was accompanied by fewer doses of vasopressors.
4.1. Conclusion
Use of solutions of norepinephrine (10 µg/mL) could reverse hypotension induced by general anesthesia, without complications. Considering the maintenance of MAP, norepinephrine is more effective than ephedrine, which is useful for hypertensive patients undergoing spinal surgery under general anesthesia.
Footnotes
Conflict of Interests:There are no conflicts of interest.
Contributor Information
Valiollah Hassani, Email: valiollah_hassani@yahoo.com.
Gholamreza Movaseghi, Email: gmovasaghi@yahoo.com.
Reza Safaeeyan, Email: rezasafa@yahoo.com.
Sahar Masghati, Email: saharmasghati@gmail.com.
Batool Ghorbani Yekta, Email: bahareh59gh@yahoo.com.
Reza Farahmand Rad, Email: dr.rezafarahmandrad@gmail.com.
References
- 1.Vallejo MC, Attaallah AF, Elzamzamy OM, Cifarelli DT, Phelps AL, Hobbs GR, et al. An open-label randomized controlled clinical trial for comparison of continuous phenylephrine versus norepinephrine infusion in prevention of spinal hypotension during cesarean delivery. Int J Obstet Anesth. 2017;29:18–25. doi: 10.1016/j.ijoa.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 2.Vallee F, Passouant O, Le Gall A, Joachim J, Mateo J, Mebazaa A, et al. Norepinephrine reduces arterial compliance less than phenylephrine when treating general anesthesia-induced arterial hypotension. Acta Anaesthesiol Scand. 2017;61(6):590–600. doi: 10.1111/aas.12905. [DOI] [PubMed] [Google Scholar]
- 3.Sudfeld S, Brechnitz S, Wagner JY, Reese PC, Pinnschmidt HO, Reuter DA, et al. Post-induction hypotension and early intraoperative hypotension associated with general anaesthesia. Br J Anaesth. 2017;119(1):57–64. doi: 10.1093/bja/aex127. [DOI] [PubMed] [Google Scholar]
- 4.Hess PE. What's new in clinical obstetric anesthesia in 2015? Int J Obstet Anesth. 2017;32:54–63. doi: 10.1016/j.ijoa.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 5.Nivatpumin P, Thamvittayakul V. Ephedrine versus ondansetron in the prevention of hypotension during cesarean delivery: a randomized, double-blind, placebo-controlled trial. Int J Obstet Anesth. 2016;27:25–31. doi: 10.1016/j.ijoa.2016.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Bauducel M, Piriou V, Dussart C, Aulagner G, Armoiry X. Current trends in vasopressor use to the operating room: A pharmacoepidemiologic study in French teaching and military hospitals. Ann Pharm Fr. 2017;75(4):276–84. doi: 10.1016/j.pharma.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 7.Bryant H, Bromhead H. Intraoperative hypotension anaesthesia . Tutorial of the week 148 24th August 2009. world federation of societies of anaesthesiologists; 2009. Available from: http://bristolsurgery.net/Documents/148%20Intraoperative%20hypotension.pdf. [Google Scholar]
- 8.Lee A, Ngan Kee WD, Gin T. A quantitative, systematic review of randomized controlled trials of ephedrine versus phenylephrine for the management of hypotension during spinal anesthesia for cesarean delivery. Anesth Analg. 2002;94(4):920–6. doi: 10.1097/00000539-200204000-00028. table of contents. [DOI] [PubMed] [Google Scholar]
- 9.Ngan Kee WD, Lee SW, Ng FF, Tan PE, Khaw KS. Randomized double-blinded comparison of norepinephrine and phenylephrine for maintenance of blood pressure during spinal anesthesia for cesarean delivery. Anesthesiology. 2015;122(4):736–45. doi: 10.1097/ALN.0000000000000601. [DOI] [PubMed] [Google Scholar]
- 10.Smith NT, Corbascio AN. The use and misuse of pressor agents. Anesthesiology. 1970;33(1):58–101. doi: 10.1097/00000542-197007000-00019. [DOI] [PubMed] [Google Scholar]
- 11.Ali Elnabtity AM, Selim MF. Norepinephrine versus Ephedrine to Maintain Arterial Blood Pressure during Spinal Anesthesia for Cesarean Delivery: A Prospective Double-blinded Trial. Anesth Essays Res. 2018;12(1):92–7. doi: 10.4103/aer.AER_204_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lecoq JP, Brichant JF, Lamy ML, Joris JL. Norepinephrine and ephedrine do not counteract the increase in cutaneous microcirculation induced by spinal anaesthesia. Br J Anaesth. 2010;105(2):214–9. doi: 10.1093/bja/aeq145. [DOI] [PubMed] [Google Scholar]
- 13.Ngan Kee WD, Khaw KS, Tan PE, Ng FF, Karmakar MK. Placental transfer and fetal metabolic effects of phenylephrine and ephedrine during spinal anesthesia for cesarean delivery. Anesthesiology. 2009;111(3):506–12. doi: 10.1097/ALN.0b013e3181b160a3. [DOI] [PubMed] [Google Scholar]
- 14.LaPorta RF, Arthur GR, Datta S. Phenylephrine in treating maternal hypotension due to spinal anaesthesia for caesarean delivery: effects on neonatal catecholamine concentrations, acid base status and Apgar scores. Acta Anaesthesiol Scand. 1995;39(7):901–5. doi: 10.1111/j.1399-6576.1995.tb04195.x. [DOI] [PubMed] [Google Scholar]
- 15.Kobayashi S, Endou M, Sakuraya F, Matsuda N, Zhang XH, Azuma M, et al. The sympathomimetic actions of l-ephedrine and d-pseudoephedrine: direct receptor activation or norepinephrine release? Anesth Analg. 2003;97(5):1239–45. doi: 10.1213/01.ANE.0000092917.96558.3C. [DOI] [PubMed] [Google Scholar]
- 16.Kwak YL, Lee CS, Park YH, Hong YW. The effect of phenylephrine and norepinephrine in patients with chronic pulmonary hypertension*. Anaesthesia. 2002;57(1):9–14. doi: 10.1046/j.1365-2044.2002.02324.x. [DOI] [PubMed] [Google Scholar]
- 17.Vos JJ, Poterman M, Hannivoort LN, Renardel De Lavalette VW, Struys MM, Scheeren TW, et al. Hemodynamics and tissue oxygenation during balanced anesthesia with a high antinociceptive contribution: an observational study. Perioper Med (Lond). 2014;3:9. doi: 10.1186/2047-0525-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pournajafian AR, Ghodraty MR, Faiz SH, Rahimzadeh P, Goodarzynejad H, Dogmehchi E. Comparing GlideScope Video Laryngoscope and Macintosh Laryngoscope Regarding Hemodynamic Responses During Orotracheal Intubation: A Randomized Controlled Trial. Iran Red Crescent Med J. 2014;16(4):e12334. doi: 10.5812/ircmj.12334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soltani Mohammadi S, Maziar A, Saliminia A. Comparing Clonidine and Lidocaine on Attenuation of Hemodynamic Responses to Laryngoscopy and Tracheal Intubation in Controlled Hypertensive Patients: A Randomized, Double-Blinded Clinical Trial. Anesth Pain Med. 2016;6(2):e34271. doi: 10.5812/aapm.34271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghodraty M, Khatibi A, Rokhtabnak F, Maleki M, Parsa F. Comparing Labetalol and Nitroglycerine on Inducing Controlled Hypotension and Intraoperative Blood Loss in Rhinoplasty: A Single-Blinded Clinical Trial. Anesth Pain Med. 2017;7(5):e13677. doi: 10.5812/aapm.13677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fathi M, Imani F, Joudi M, Goodarzi V. Comparison Between the Effects of Ringer`s Lactate and Hydroxyethyl Starch on Hemodynamic Parameters After Spinal Anesthesia: A Randomized Clinical Trial. Anesth Pain Med. 2013;2(3):127–33. doi: 10.5812/aapm.7850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee A, Ngan Kee WD, Gin T. A dose-response meta-analysis of prophylactic intravenous ephedrine for the prevention of hypotension during spinal anesthesia for elective cesarean delivery. Anesth Analg. 2004;98(2):483–90. doi: 10.1213/01.ANE.0000096183.49619.FC. [DOI] [PubMed] [Google Scholar]
- 23.Ngan Kee WD, Lee SWY, Ng FF, Khaw KS. Prophylactic Norepinephrine Infusion for Preventing Hypotension During Spinal Anesthesia for Cesarean Delivery. Anesth Analg. 2018;126(6):1989–94. doi: 10.1213/ANE.0000000000002243. [DOI] [PubMed] [Google Scholar]
- 24.Minzter BH, Johnson RF, Paschall RL, Ramasubramanian R, Ayers GD, Downing JW. The diverse effects of vasopressors on the fetoplacental circulation of the dual perfused human placenta. Anesth Analg. 2010;110(3):857–62. doi: 10.1213/ANE.0b013e3181c91ebc. [DOI] [PubMed] [Google Scholar]
- 25.Boccara G, Ouattara A, Godet G, Dufresne E, Bertrand M, Riou B, et al. Terlipressin versus norepinephrine to correct refractory arterial hypotension after general anesthesia in patients chronically treated with renin-angiotensin system inhibitors. Anesthesiology. 2003;98(6):1338–44. doi: 10.1097/00000542-200306000-00007. [DOI] [PubMed] [Google Scholar]
- 26.El Fawy DM, El Shafei MM, El Gendy HA. Norepinephrine versus ephedrine for the prevention of spinal anesthesia-induced hypotension in coronary artery disease patients undergoing knee arthroscopy. Ain Shams J Anaesthesiol. 2015;8(3):424. doi: 10.4103/1687-7934.161723. [DOI] [Google Scholar]
- 27.Moran DH, Perillo M, LaPorta RF, Bader AM, Datta S. Phenylephrine in the prevention of hypotension following spinal anesthesia for cesarean delivery. J Clin Anesth. 1991;3(4):301–5. doi: 10.1016/0952-8180(91)90224-B. [DOI] [PubMed] [Google Scholar]