Introduction
Postoperative pain after laparoscopic surgery is one of the major concerns of patients.1 Improper pain management can be associated with varied respiratory, cardiovascular, gastrointestinal, and psychological complications.1 Pain after laparoscopic surgery may be transient or persistent2 and opioids have traditionally been the mainstay treatment for postoperative pain.3 Increasing evidence exists to support a multimodal treatment approach for postoperative pain that reduces opioid side effects and decreases pain intensity (PI) scores.3 A proprietary nanocrystal intravenous (NIV) formulation of the non-steroidal anti-inflammatory meloxicam, a long-acting preferential cyclo-oxygenase-2 inhibitor, is being evaluated with the aim of providing rapid and sustained analgesia.
Material and methods
This was a phase II, randomized, double-blind, placebo and active controlled study in subjects undergoing laparoscopic abdominal surgery. Subjects were randomized 1:1:1:1:1 to intravenous (IV) doses of placebo, ketorolac every 6 hours (Q6H), meloxicamNIV 7.5 mg Q12H, meloxicamNIV15 mg Q12H, or meloxicamNIV30 mg once daily (QD) for up to 48 hours. Each subject was dosed Q6H (with placebo as applicable) to maintain blinding. Subjects were discharged from the study unit 48 hours after the initial dose of study drug and followed as outpatients through Day 28.
Efficacy was assessed by subject reports of PI on a 100 mm Visual Analog Scale anchored at 0 for no pain and 100 for worst possible pain. Rescue medication (parenteral morphine 2–6 mg) was available any time after the initial dose of study drug. Missing PI scores were imputed for the efficacy analysis using a 2-hour windowed last observation carried forward (W2LOCF) approach.
Safety was monitored through the reporting of adverse events, clinical laboratory testing, vital sign assessments, 12-lead electrocardiograms (ECGs), and wound site assessments.
The study was expected to enroll 200 subjects; however, the study was terminated for business reasons after 50 subjects enrolled. As a result, the original analyses were limited to disposition, demographics, and safety. Efficacy data were subsequently analyzed post hoc. No formal statistical analysis was performed.
The Aspire Institutional Review Board approved the protocol and the study was conducted according to Good Clinical Practices. All subjects provided written informed consent. Trial registration: ClinicalTrials.gov (Identifier: NCT01436032).
Results
Fifty subjects received at least one dose of study drug and 47 completed the study. The mean age overall was 41.8 years and most subjects were white and male.
Safety
Headache, dry mouth, dysuria, and nausea were the most common treatment emergent adverse events (TEAEs) reported across the meloxicam groups. Reported TEAE rates were similar to placebo (Table 1). Most TEAEs were mild in intensity and unrelated to treatment.
Table 1.
Disposition and TEAEs in the five study groups after laparoscopic abdominal surgerya
| Adverse events (preferred term), N (%) | Placebo IV N=11 | Ketorolac IV 30 mg Q6H N=8 | Meloxicam NIV 7.5 mg Q12H N=11 | Meloxicam NIV 15 mg Q12H N=10 | Meloxicam NIV 30 mg QD N=10 |
|---|---|---|---|---|---|
| Treated | 11 (100.0) | 8 (100.0) | 11 (100.0) | 10 (100.0) | 10 (100.0) |
| Any adverse event | 9 (81.8) | 8 (100.0) | 10 (90.9) | 7 (70.0) | 9 (90.0) |
| Serious adverse event | 0 | 1 (12.5) | 0 | 0 | 0 |
| Death | 0 | 0 | 0 | 0 | 0 |
| Withdrawals | |||||
| Adverse event | 0 | 0 | 1 (9.1) | 0 | 0 |
| Withdrawal of consent | 0 | 0 | 0 | 0 | 1 (10.0) |
| Missing | 0 | 0 | 0 | 1 (10.0) | 0 |
| TEAEs occurring in ≥2 subjectsb | |||||
| Headache | 6 (54.5) | 0 | 4 (36.4) | 2 (20.0) | 6 (60.0) |
| Dry mouth | 3 (27.3) | 2 (25.0) | 2 (18.2) | 4 (40.0) | 3 (30.0) |
| Dysuria | 3 (27.3) | 3 (37.5) | 4 (36.4) | 1 (10.0) | 3 (30.0) |
| Dizziness | 2 (18.2) | 0 | 0 | 1 (10.0) | 5 (50.0) |
| Nausea | 2 (18.2) | 0 | 2 (18.2) | 4 (40.0) | 2 (20.0) |
| Asthenia | 1 (9.1) | 0 | 2 (18.2) | 0 | 1 (10.0) |
| Constipation | 1 (9.1) | 1 (12.5) | 2 (18.2) | 0 | 2 (20.0) |
| Disturbance in attention | 1 (9.1) | 0 | 1 (9.1) | 2 (20.0) | 0 |
| Fatigue | 1 (9.1) | 2 (25.0) | 2 (18.2) | 1 (10.0) | 2 (20.0) |
| Musculoskeletal pain | 0 | 0 | 2 (18.2) | 1 (10.0) | 0 |
| Upper respiratory tract infection | 0 | 0 | 3 (27.3) | 0 | 1 (10.0) |
Notes:
Biliary tree surgery, common bile duct exploration/surgery, cholecystectomy, or inguinal hernia surgery.
The events listed are those reported by ≥2 subjects in any study group.
Abbreviations: NIV, nanocrystal intravenous formulation of meloxicam; TEAE, treatment emergent adverse event.
No deaths were reported. One ketorolac-treated subject who underwent hernia repair had a serious adverse event of post procedural hemorrhage. One meloxicamNIV 7.5 mg Q12H treated subject had a TEAE of mild truncal maculopapular rash that led to discontinuation. This subject had no signs of anaphylaxis.
The mean changes from baseline in laboratory parameters were small and similar across treatment groups. Leukocytosis in the meloxicamNIV 7.5 mg Q12H group and anemia secondary to post procedural hemorrhage in the ketorolac group were TEAEs. Mean changes from baseline in vital signs and ECG parameters were small and similar across treatment groups. Wound examinations showed normal healing in the meloxicamNIV and ketorolac groups.
Efficacy
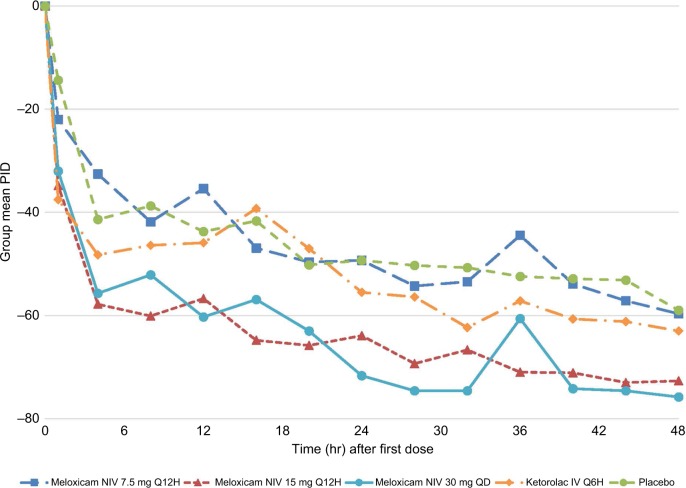
Mean PI differences over the 48-hour assessment period were similar between the meloxicamNIV15 mg Q12H and 30 mg QD groups and similar to ketorolac IV Q6H (Figure 1).
Figure 1.
Mean PIDs according to W2LOCF analysisa from baseline through 48 hours in the five study groups after laparoscopic abdominal surgeryb.
Notes: aIn the W2LOCF analysis, the pain intensity score collected immediately prior to rescue medication administration was carried forward to replace the scheduled pain intensity scores collected (or to be collected) within the 2-hour window following the use of rescue medication. bBiliary tree surgery, common bile duct exploration/surgery, cholecystectomy, or inguinal hernia surgery.
Abbreviations: NIV, nanocrystal intravenous formulation of meloxicam; PID, pain intensity difference; W2LOCF, 2-hour windowed last observation carried forward.
Conclusions
In this small study, meloxicam NIV was generally well tolerated with a safety profile similar to placebo. PI differences over time suggest meloxicamNIV15 mg Q12H, meloxicamNIV30 mg QD, and ketorolac IV Q6H may provide pain relief after laparoscopic abdominal surgery.
Acknowledgments
Funding for this research was provided by Recro Pharma, Inc., Malvern, PA 19355, USA.
Footnotes
Author contributions
NS contributed to the design of the study and its implementation. NS managed the subjects and contributed to acquisition of the data. WD provided statistical guidance for data analysis and interpretation. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
NS is an employee of Lotus Research, which conducted this trial. WD received consultancy fees from Recro Pharma, Inc., Malvern, PA, USA. RJM, SWM, AF, and SH are employees and security holders of Recro Pharma, Inc., Malvern, PA, USA. The authors report no other conflicts of interest in this work.
References
- 1.Golzari SE, Nader ND, Mahmoodpoor A. Underlying mechanisms of postoperative pain after laparoscopic surgery. JAMA Surg. 2016;151(3):295–296. doi: 10.1001/jamasurg.2015.3934. [DOI] [PubMed] [Google Scholar]
- 2.Alexander JI. Pain after laparoscopy. Br J Anaesth. 1997;79(3):369–378. doi: 10.1093/bja/79.3.369. [DOI] [PubMed] [Google Scholar]
- 3.Veerabhadram G, Cellini C. Postoperative pain control. Clinic Colon Rectal Surg. 2013;26(3):191–196. doi: 10.1055/s-0033-1351138. [DOI] [PMC free article] [PubMed] [Google Scholar]