Abstract
Background.
Cognitive therapy (CT) improves symptoms in adults with major depressive disorder (MDD) plus comorbid anxiety disorder, but the specific type of anxiety may influence outcomes. This study compared CT outcomes among adults with MDD plus social, other, or no comorbid anxiety disorders.
Methods.
Outpatients with recurrent MDD (N=523, including 87 with social and 110 with other comorbid anxiety disorders) received acute-phase CT. Higher risk responders (n=241 with partial or unstable response) were randomized to 8 months of continuation treatment (CT or clinical management plus fluoxetine or pill placebo), followed by 24 months of assessment. Lower risk responders (n=49) were assessed for 32 months without additional research treatment. Depression, anxiety symptoms, and social avoidance were measured repeatedly.
Results.
Other (non-social), but not social, anxiety disorders predicted elevated depression and anxiety symptoms throughout and after acute-phase CT. Social, but not other, anxiety disorder predicted greater reduction in depressive symptoms during acute-phase CT and elevated social avoidance during and after acute-phase CT.
Limitations.
Anxiety disorders were assessed only before acute-phase treatment. The anxiety symptom measure was brief. Generalization to other patient populations and treatments is unknown.
Conclusions.
Non-social comorbid anxiety disorders may reduce the efficacy of acute-phase CT for MDD by diminishing both short-and longer term outcomes relative to depressed patients without comorbid anxiety disorders. Comorbid social anxiety disorder may increase relative reductions in depressive symptoms during acute-phase CT for MDD, but patients with comorbid social anxiety disorder may require specialized focus on social avoidance during CT.
Keywords: depression, anxiety disorders, cognitive therapy, prognosis, comorbidity, major depressive disorder, social anxiety disorder, fluoxetine
Introduction
Anxiety disorders are often comorbid with major depressive disorder (MDD; Kessler et al., 2005; Kessler et al., 2015). Relations of comorbid anxiety disorders with MDD treatment outcomes are incompletely understood, although augmenting or sequencing medications or psychotherapies in varying combinations have been suggested for particular comorbid disorders (e.g., Coplan et al., 2015; Schoevers et al., 2008). The current study clarified short-and longer-term prognoses of outpatients who received cognitive therapy (CT) for recurrent MDD, comparing patients with social, other, or no comorbid anxiety disorders (Jarrett & Thase, 2010). These findings may expand the CT literature by differentiating social from other anxiety disorders and inform need for additional assessment and treatment.
Comorbid anxiety often predicts poorer outcomes during treatment of MDD, but prognoses may vary by types of treatment, as well as particular anxiety disorder diagnoses or symptoms (Schaffer et al., 2012). The literature is perhaps clearest for acute-phase pharmacotherapy, during which comorbid anxiety has often (but not always) predicted less response and remission and more relapse (e.g., Andreescu et al., 2007; Fava et al., 2008; Saveanu et al., 2015), and also greater psychosocial dysfunction despite increased medication prescription (Petersen et al., 2009). Anxiety has also predicted poorer outcomes in continuation pharmacotherapy or CT for depression employed in treatment augmentation or switch strategies (Farabaugh et al., 2012).
A smaller, inconsistent literature addresses comorbid anxiety during acute-phase CT (A-CT) for depression. A recent meta-analysis showed that psychotherapy for depression improved symptoms of both depression and anxiety compared to control conditions, with moderate-to-large effect sizes for both sets of symptoms (Weitz, et al., 2018). In addition, anxiety symptoms among patients with MDD have predicted more severe depression at intake and quicker reduction in depressive symptoms during CT (Forand et al., 2011; Forand et al., 2013; Smits et al., 2012). However, anxiety symptoms have also predicted lower rates of response and remission and more frequent relapse after response to A-CT (Forand et al., 2013; Smits et al., 2012). Similarly, anxiety symptoms have predicted delayed remission during interpersonal psychotherapy for MDD (Frank et al., 2011) and may become more closely tied to depression as time in treatment progresses (Wright et al., 2014). Finally, depressed patients with comorbid anxiety had better acute-phase outcomes when treated with CT compared to interpersonal psychotherapy; however the difference was not sustained afterward (van Bronswijk et al., 2018).
Rather than anxiety symptoms, other studies focused on anxiety disorder diagnoses. Among the anxiety disorders, social anxiety disorder has especially strong theoretico-empirical connections to depression. Many anxiety disorders (e.g., social anxiety disorder, generalized anxiety disorder, panic disorder, agoraphobia) share with depression elevations in non-specific negative emotionality. However, unlike other anxiety disorders, social anxiety disorder also shares with depression substantially reduced positive emotionality (Adams et al., 2016; Brown et al., 1998; Langer & Rodebaugh, 2014; Watson, Clark, & Carey, 1988; Watson, Gamez, & Simms, 2005). Cognitive therapy for depression targets both negative (e.g., via restructuring of negative automatic thoughts to reduce distress in response to internal and external stimuli) and positive (e.g., via behavioral activation to increase engagement with sources of reinforcement) emotionality (Beck et al., 1979). Because of stronger match of MDD with social versus other anxiety disorders in emotionality, and because CT for depression targets both positive and negative emotionality, MDD patients with comorbid social anxiety disorder may show better outcomes during CT for depression than do patients with other comorbid anxiety disorders.
Diagnosis of comorbid social anxiety disorder predicted more depressive symptoms after A-CT for MDD in one study, but with a small effect size and at a trend level of statistical significance (DeRubeis et al. 2005). Another study, however, found no evidence of less completion, response, remission, or rate of improvement in depressive symptoms among patients with comorbid social anxiety disorder receiving A-CT for MDD (Smits et al., 2009). Moreover, although comorbid anxiety disorders in general predict poorer long-term outcomes among individuals with MDD, many analyses, including those reported on by DeRubeis et al. and Smits et al., have not differentiated particular anxiety disorder diagnoses (Burcusa & Iacono, 2007).
In this context and to move the literature forward, the current study compared CT outcomes by type of anxiety disorder through secondary analyses of a clinical trial dataset (N = 523; Jarrett & Thase, 2010). The size and distribution of comorbid anxiety disorders in this dataset (see Table 1) supported differentiation of social from other (non-social) anxiety disorders. We tested the hypothesis that comorbid anxiety disorders, particularly other (non-social) compared to social anxiety disorders, predict poorer depression outcomes in A-CT for recurrent MDD (i.e., higher depressive symptoms and less frequent response) and for 32 months after A-CT response (i.e., higher depressive symptoms and more frequent relapse/recurrence). Parallel to this hypothesis about depression outcomes, we tested whether anxiety disorders predicted anxiety symptoms and social avoidance, which may be more specific consequences of these comorbid diagnoses, during and after response to A-CT for recurrent MDD. Thus, our analyses clarified how social versus other anxiety disorders predict several outcomes to inform efforts to increase CT’s efficacy.
Table 1. Anxiety Disorders at Intake to Acute Phase Cognitive Therapy for Depression.
| Diagnosis | n | % |
|---|---|---|
| Social anxiety disorder | 87 | 16.6% |
| Other anxiety disorders | 110 | 21.0% |
| Specific phobia | 38 | 7.3% |
| Panic disorder without agoraphobia | 33 | 6.3% |
| Generalized anxiety disorder | 30 | 5.7% |
| Panic disorder with agoraphobia | 12 | 2.3% |
| Anxiety disorder not otherwise specified | 8 | 1.5% |
| Agoraphobia without panic disorder | 6 | 1.1% |
| Separation anxiety disorder | 1 | 0.2% |
| Social anxiety disorder without other anxiety disorder | 58 | 11.1% |
| Other anxiety disorder without social anxiety disorder | 81 | 15.5% |
| Both social anxiety disorder and other anxiety disorder | 29 | 5.5% |
| Neither social anxiety disorder nor other anxiety disorder | 355 | 67.9% |
Note. N = 523. Anxiety disorders in the top portion of the table are not mutually exclusive.
Method
Data were drawn from a randomized clinical trial detailed by Jarrett and Thase (2010) and registered at ClinicalTrials.gov (NCT00118404, NCT00183664, and NCT00218764). We summarize below methods relevant to the current analyses.
Participants
Participants (N = 523) were outpatients who (a) provided written informed consent; (b) met DSM-IV criteria for recurrent MDD (American Psychiatric Association, 2000) assessed with the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 1996); (c) had remitted between prior depressive episodes, ≥ 1 depressive episode with complete inter-episode recovery, or antecedent dysthymic disorder; and (d) scored ≥ 14 on the 17-item Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960).1 Exclusion criteria were (a) severe or poorly controlled concurrent medical disorders that could cause depression, (b) psychotic or organic mental disorders, bipolar disorder, active substance dependence, or primary obsessive-compulsive or eating disorders, (c) could not complete questionnaires in English, (d) active suicide risk, (e) < 18 or > 70 years old, (f) previous failure to respond to ≥ 8 weeks of CT or 6 weeks of fluoxetine, or (g) pregnancy, current or planned during the first 11 months after intake.
The SCID was administered and scored by trained evaluators (nurses, psychologists, or research associates). In addition to MDD, other DSM-IV disorders were diagnosed using the SCID. In the current analyses, we focused on the subset of DSM-IV anxiety disorders that remained classified as anxiety disorders in DSM-5 (American Psychiatric Association, 2013). Diagnosed anxiety disorders are listed in Table 1, and other patient characteristics are summarized in Table 2. Supplement 1 depicts the flow of participants through the study phases described following.
Table 2. Sample Characteristics at Study Intake: Overall and by Anxiety Disorder Diagnoses.
| Patient Characteristics by Social, Other, or No Anxiety Disorder | ||||||
|---|---|---|---|---|---|---|
| All patients | Social | Other | No | |||
| Demographics | M or % | SD | M or % | M or % | M or % | Omnibus test |
| Female gender | 67.5% | 67.9% | 75.4% | 65.3% | F(2,520) = 1.99, p = .14 | |
| White ethnicity | 80.9% | 77.5%ab | 73.3%a | 83.6%b | F(2,520) = 3.40, p = .03 | |
| Age (years) | 42.37 | 12.11 | 39.31a | 41.65ab | 43.18b | F(2,520) = 3.88, p = .02 |
| Married or partnered | 41.9% | 33.7% | 39.0% | 44.2% | F(2,520) = 1.76, p = .17 | |
| Education (years) | 15.06 | 2.93 | 14.19a | 14.40a | 15.41b | F(2,520) = 9.48, p < .001 |
| Illness Characteristics | ||||||
| Age of MDD onset (years) | 21.16 | 10.76 | 18.36a | 20.42ab | 21.92b | F(2,520) = 4.21, p = .02 |
| Length of MDD (years) | 20.71 | 11.81 | 20.45 | 20.75 | 20.76 | F(2,520) = 0.02, p = .98 |
| Number of depressive episodes | 4.01 | 1.72 | 4.22 | 4.18 | 3.92 | F(2,520) = 1.27, p = .28 |
| Current episode length (months) | 24.97 | 45.13 | 28.31 | 24.22 | 24.50 | F(2,520) = 0.28, p = .75 |
| Total Axis I diagnoses | 1.61 | 0.83 | 2.32a | 2.48a | 1.21b | F(2,520) = 70.97, p < .001 |
| Depression symptom severity | 50.00 | 10.00 | 51.52a | 53.55a | 48.75b | F(2,520) = 11.29, p < .001 |
| Anxiety symptom severity | 0.46 | 0.16 | 0.48a | 0.54b | 0.43c | F(2,520) = 25.80, p < .001 |
| Social avoidance | 1.95 | 0.92 | 2.45a | 2.08b | 1.82c | F(2,507) = 18.14, p < .001 |
Note. N = 523, except social avoidance N = 510. Estimates of demographics and illness characteristics for patients with social, other, or no anxiety disorders derived from logistic (dichotomous variables: gender, ethnicity, married/partnered), Poisson (count variables: number of episodes, total Axis I diagnoses), or linear (remaining continuous variables) regression models. When the omnibus test for a row yielded p < .05, pairwise contrasts were computed and means or proportions without a common superscript varied at p < .05, two-tailed.
Acute-phase CT
Consenting patients (N = 523) withdrew from any psychotropic medications before CT. The cognitive therapists (12 doctoral, 4 masters-level; 12 women, 4 men) completed ≥ 1 year of supervised training in CT and demonstrated competence by maintaining Cognitive Therapy Scale (Young & Beck, 1980) mean scores ≥ 40. Therapists submitted videotaped sessions for review, participated in weekly group supervision, and received feedback. The acute-phase protocol lasted 12 weeks, with 2 additional weeks allowed for rescheduling. Patients received two CT sessions per week for 4 weeks. Then, patients with ≥ 40% reduction in HRSD scores received 8 additional weekly sessions (16 total sessions), whereas patients with < 40% reduction in HRSD scores received eight additional twice-weekly then four weekly sessions (20 total sessions).2 Patients with less early improvement received more sessions to increase their chances of response, defined as no MDD and HRSD ≤ 12 by independent evaluation at the end of A-CT. Responders were stratified by a priori criteria into lower risk (the last 7 acute-phase HRSD scores all ≤ 6) and higher risk (≥1 of the last 7 acute-phase HRSD scores ≥7) groups.
Continuation Phase
Higher risk A-CT responders (n = 241) were randomized to 8 months of continuation-phase CT (n = 86) or to clinical management with either fluoxetine (n = 86) or pill placebo (n = 69).3 A blinded evaluator assessed patients at the ends of months 4 and 8 (and during interims if relapse was suspected) for DSM-IV criteria for MDD using the SCID and the Longitudinal Interval Follow-up Evaluation (Keller et al., 1987). Lower risk A-CT responders (n = 49) were assessed on the same schedule but did not receive additional protocol treatment. Patients who relapsed were referred for non-research treatment.
The continuation CT protocol included 10 sessions (four biweekly then six monthly sessions) of approximately 60 minutes each (Jarrett et al., 1989; Jarrett, Vittengl, & Clark, 2008). Continuation CT patients applied compensatory skills to residual and emergent depressive symptoms; generalized CT skills across problems, time, and situation; and practiced preemptive coping to cognitive and behavioral risks identified previously. Patients’ acute and continuation CT therapists were the same, with few exceptions (e.g., due to a therapist’s maternity leave).
The fluoxetine and pill-placebo clinical-management protocol (Fawcett et al., 1987) was double blinded, provided by experienced pharmacotherapists, and included 10 sessions on the same schedule as continuation CT. The first session lasted up to 45 minutes and remaining sessions up to 30 minutes. Pharmacotherapists were prohibited from using any specific continuation CT methods. Research pharmacies dispensed active fluoxetine or identical placebo capsules. Patients first received 10 mg/day for 2 weeks, then 20 mg/day for 2 weeks, and 40 mg/day thereafter. Pharmacotherapists were allowed to decrease doses to lessen side effects. Patients who could not tolerate at least 10 mg/day were removed from medication and received only clinical management. Most patients (73%) achieved the target dose of 40 mg/day (Jarrett et al., 2013). All randomized patients are analyzed here.
Follow-up Phase
Patients completing the continuation phase entered a 24-month follow-up. Blinded evaluators assessed patients every 4 months. Patients experiencing depressive symptoms were encouraged to contact study personnel for interim evaluation. Patients were referred out for treatment in the event of relapse or recurrence.
Measures
Depression symptoms.
Patients completed the 21-item Beck Depression Inventory (BDI; Beck et al., 1961) and 30-item Inventory for Depressive Symptomatology self-report (IDS-SR; Rush et al., 1996), and clinicians completed the 17-item HRSD. Because these measures reflect the same construct during treatment of depression (Vittengl, Clark, Kraft, & Jarrett, 2005; Vittengl et al., 2013), we standardized (M = 50, SD = 10) the measures’ total scores based on their distributions at acute-phase intake and averaged them to form a robust composite, after excluding 4 items directly referencing anxiety symptoms (detailed subsequently). Higher scores indicated more severe depressive symptomatology. Treating the three scales as items, alpha reliability for the depression composite was high in the current sample (.96).4
Anxiety symptoms.
Two items each on the HRSD (“psychic anxiety,” “somatic anxiety”) and IDS-SR (“feeling tense or anxious,” “panic/phobic symptoms”) referenced anxiety directly. These item ratings were standardized as the percentage of maximum possible score (HRSD items were rated 0–4, whereas IDS-SR items were rated 0–3) and averaged to form an anxiety scale. Alpha reliability for the 4-item anxiety scale was moderate in the current dataset (.73; average inter-item r = .42, within the recommended range; Clark & Watson, 1995).
Social avoidance.
Patients completed the Inventory of Interpersonal Problems (Horowitz et al., 1988) to measure problematic behaviors, thoughts, and feelings in social relationships. We scored an eight-item subscale reflecting social avoidance (Horowitz et al., 2000) because social avoidance is central to social anxiety disorder. Higher scores reflect greater social avoidance. Alpha reliability for the social avoidance subscale (.89) was high in the current sample.
Completion and response.
Completion of A-CT was defined as missing no more than two CT sessions in the 16-or 20-session protocol described above. Acute-phase response was defined as no longer meeting criteria for MDD and having a final acute-phase HRSD score ≤ 12.
Relapse and recurrence.
Independent evaluators completed the Longitudinal Interval Follow-Up Evaluation (Keller et al., 1987) every 4 months after A-CT, at study exit, and when patients, therapists, or follow-up evaluators suspected major depressive relapse or recurrence. This semi-structured retrospective interview yielded weekly psychiatric status ratings of DSM-IV MDD. Ratings of 1 (no MDD symptoms) or 2 (one or two mild symptoms) for ≥ 35 continuous weeks defined recovery. Ratings of 5 (meets MDD criteria) or 6 (meets MDD criteria with severe impairment and/or psychosis) for ≥ 2 weeks defined relapse and recurrence before and after recovery, respectively (Jarrett & Thase, 2010). Patients who relapsed or recurred were censored at that point for survival analyses.
Related Previous Analyses
In previous analyses of the current dataset, anxiety symptoms (measured with HRSD items) predicted greater severity and faster improvement in depressive symptoms but less response and remission during A-CT (Smits et al., 2012). Beyond anxiety symptoms, the current analyses focused on formal anxiety-disorder diagnoses as predictors of outcomes, contrasting social with other anxiety disorders. In addition, the current analyses extended the time frame to consider outcomes in A-CT plus 32 subsequent months for responders.
During the first 8 months after A-CT, continuation CT or fluoxetine reduced relapse and residual depressive symptoms compared to pill placebo among higher risk acute-phase responders (Jarrett et al., 2013; Vittengl et al., 2014). In addition, lower versus higher risk patients were less likely to experience relapse during the continuation phase (Jarrett et al, 2016). Finally, gains in social-interpersonal functioning made during acute-phase CT were maintained for 32 months among higher-risk responders but not further improved by continuation treatment (Vittengl et al., 2016). In this context, we controlled but did not report differences among continuation-phase arms here.
Analyses Testing the Current Hypotheses and Research Questions
We predicted A-CT response and completion using logistic regression models, and we described effect sizes using the odds ratio. Among A-CT responders, we predicted time to relapse over the 8 month continuation phase, and relapse or recurrence over the 8 month continuation plus 24 month follow-up phases (32 total months), using Cox regression models with the hazard ratio as a measure of effect size. In the Cox regression models, patients were censored when they first exited the study, experienced relapse or recurrence, or completed the follow-up phase. During A-CT, and after A-CT among responders, we predicted depressive symptoms, anxiety symptoms, and social avoidance using repeated-measures multilevel linear models employing maximum likelihood estimation, autoregressive error structures, and the Satterthwaite approximation for degrees of freedom. In multilevel models, effect size d was estimated as the difference in least-squares estimated means divided by the outcome variable’s SD at acute-phase intake.
Statistical models used to test hypotheses controlled a number of variables to isolate the effects of social and other anxiety disorders. All models controlled patient age, gender, ethnicity, years of education, and age of MDD onset. In addition, all models controlled depressive symptom severity at intake, except models of acute-phase depressive symptom severity that already included this variable. Post-acute-phase models also controlled continuation-phase arm (dummy coded: lower risk—assessment only, higher risk—continuation CT, higher risk—continuation fluoxetine, or higher-risk—continuation pill placebo with clinical management). Finally, repeated-measures multilevel models included the effect of time (dummy coded, during A-CT: pre-, mid-, or post-CT; after A-CT: continuation phase, follow-up year 1 or 2).
For hypothesis tests, the fixed effects of interest were the main effects of anxiety disorder diagnoses (dummy coded: the presence or absence of any anxiety disorder; or the presence or absence of social anxiety disorder and other anxiety disorders). Because main effects of social and other anxiety disorders were entered simultaneously in the statistical models, results reflected the diagnostic variables’ unique relations with outcomes. In the multilevel models, we also tested interactions of anxiety disorders with time and trimmed non-significant interactions (p > .05) from final models to clarify main effects. We did not test interactions of social with other anxiety disorders, or anxiety disorders with continuation-phase arm, because we had no a priori hypotheses about these interactions and interaction tests would have relied on some small cell sizes (e.g., as few as 7 patients during continuation and 2 during follow-up phases).
Acute-phase response and completion data were complete in logistic regression models. A strength of Cox regression models is that they accurately handle patients with censored data, such as when patients exited the study before a relapse or recurrence event (e.g., Cohen et al., 2003). A strength of repeated-measures multilevel models with maximum likelihood estimation is that they support valid inferences when data are missing completely at random or missing for reasons predictable from variables included in the model (e.g., Schafer & Graham, 2002).
Preliminary Analyses
At intake to A-CT, correlations of depressive symptom severity with anxiety symptoms (.43) and social avoidance (.35), and between anxiety symptoms and social avoidance (.16), were statistically significant, ps < .001, but small-moderate in size. Similarly, acute-phase pre/post change correlations of depressive symptom severity with anxiety symptoms (.59) and social avoidance (.42), and between anxiety symptoms and social avoidance (.35), were statistically significant, ps < .001, and moderate in size. Thus, these three variables tapped related but partly distinct information about the current sample of patients with recurrent MDD.
To examine missing data patterns, we tallied the number of missing data points during the acute-phase, and after the acute phase for A-CT responders, among the depressive symptom, anxiety symptom, and social avoidance scales. Spearman correlations of any comorbid anxiety disorder, depressive symptom severity, anxiety symptoms, and social avoidance at intake with the number of missing data points were small (median rs = .10, range −.03 to .15). Statistically significant (p < .05) correlates of missing data included an anxiety disorder (.11), depressive symptoms (.14), and anxiety symptoms (.10) during the acute phase, and an anxiety disorder (.13) and depressive symptoms (.15) after the acute phase. However, the other statistically significant correlates of missing data became non-significant when depressive symptom severity at intake was partialled. Consequently, depressive symptom severity at intake appeared central to the pattern of missing data was included in all hypothesis-testing models.
Results
Patient Characteristics at Study Intake
Table 1 shows frequencies of anxiety disorders comorbid with recurrent MDD at intake to A-CT. The majority of patients (67.9%) had no comorbid anxiety disorder, but substantial subgroups had comorbid social anxiety disorder (16.6%) and/or other comorbid anxiety disorders (21.0%). The correlation between social and other anxiety disorder diagnoses was small but statistically significant (phi = .13, p = .004). A few patients (5.5%) had both social and other anxiety disorder diagnoses. All patients were included in the analyses.
Table 2 shows demographic and illness information. Gender, marital/partnered status, length of MDD, number of major depressive episodes, and length of the current depressive at intake did not relate significantly to anxiety disorder diagnoses. Patients with social or other anxiety disorders had about one more total Axis I diagnosis than did patients without comorbid anxiety disorders, as would be expected. Compared to patients without comorbid anxiety disorders, patients with social anxiety disorder were younger, had less formal education, an earlier age of MDD onset, and more severe depressive symptoms, anxiety symptoms, and social avoidance at intake. Similarly, compared to patients without comorbid anxiety disorders, patients with other anxiety disorders had less education plus more severe depressive symptoms, anxiety symptoms, and social avoidance at intake, and were less often of white ethnicity. However, anxiety symptoms were higher among patients with other versus social anxiety disorders, whereas social avoidance was higher among patients with social versus other anxiety disorders at intake.
Acute-phase CT
Our hypothesis tests first predicted outcomes from any anxiety disorder. We then differentiated social and other anxiety disorders. On average across the acute phase, patients with any versus no anxiety disorder had more depressive symptoms, anxiety symptoms, and social avoidance (see Table 3).
Table 3. Prediction of Anxiety and Depressive Symptoms and Social Avoidance during Acute-phase Cognitive Therapy for Depression.
| Model | Outcome | Predictors | Beta | SE | Effect size d [95% CI] |
|---|---|---|---|---|---|
| 1 | Anxiety Sx | Any anxiety disorder | 0.062*** | 0.012 | 0.38 [0.24,0.53] |
| 2 | Anxiety Sx | Social and other anxiety disorders: F(2,556) = 20.75, p < .001 | |||
| Social AD | −0.001 | 0.014 | 0.00 [−0.18,0.17] | ||
| Other AD | 0.085*** | 0.013 | 0.53 [0.37,0.69] | ||
| Contrast: Social – other | −0.086*** | 0.021 | −0.53 [−0.78,−0.28] | ||
| 3 | Depressive Sx | Any anxiety disorder | 3.237*** | 0.960 | 0.32 [0.14,0.51] |
| 4 | Depressive Sx | Social and other anxiety disorders: F(2,568) = 12.34, p <.001 | |||
| Social anxiety disorder | −0.712 | 1.221 | −0.07 [−0.31,0.17] | ||
| Other anxiety disorder | 5.543*** | 1.116 | 0.55 [0.34,0.77] | ||
| Contrast: Social – other | −6.255*** | 1.751 | −0.63 [−0.97,−0.28] | ||
| Time * anxiety disorders: F(4,898) = 2.74, p = .03 | |||||
| Pre-CT * social anxiety | 4.306* | 1.847 | |||
| Mid-CT * social anxiety | −1.662 | 1.718 | |||
| Pre-CT * other anxiety | 1.826 | 1.541 | |||
| Mid-CT * other anxiety | 1.583 | 1.446 | |||
| 5 | Social avoidance | Any anxiety disorder | 0.327*** | 0.074 | 0.36 [0.20,0.52] |
| 6 | Social avoidance | Social and other anxiety disorders: F(2,509) = 13.32, p < .001 | |||
| Social anxiety disorder | 0.458*** | 0.092 | 0.50 [0.30,0.70] | ||
| Other anxiety disorder | 0.069 | 0.085 | 0.08 [−0.11,0.26] | ||
| Contrast: Social – other | 0.388** | 0.131 | 0.42 [0.14,0.70] | ||
Note. N = 523. Anxiety disorders assessed at intake to acute-phase cognitive therapy. Symptom (Sx) and functioning outcome variables assessed at intake, the mid-point, and after acute-phase cognitive therapy (time period). Models controlled depressive symptom severity at study intake (except models 3–4), age, age of depression onset, education, ethnicity, gender, and time period. Data were analyzed with repeated-measures multilevel models. Anxiety disorders and time period were dummy coded (1 = present, 0 = absent) and centered. Non-significant (p > .05) interactions of anxiety disorders and time period were trimmed from the final models. CT = acute-phase cognitive therapy. CI = confidence interval.
p < .05
p < .01
p < .001.
However, results varied by type of anxiety disorder (Table 3). Compared to patients with no anxiety disorder, those with social anxiety disorder did not show significant elevations in depressive or anxiety symptoms, overall, but did have greater social avoidance. In contrast, compared to patients with no anxiety disorder, patients with other anxiety disorders showed significant elevations in anxiety and depression symptoms but not social avoidance. Finally, patients with social anxiety disorder had fewer anxiety and depression symptoms, but more social avoidance, than patients with other anxiety disorders.
The main effect of social/other/no anxiety disorder on depression severity was qualified by a significant interaction with time, as illustrated in Figure 1. From pre- to post-A-CT, patients with social anxiety disorder improved more than did patients with other (d = 0.49, CI95% 0.06 to 0.92) or no (d = 0.40, CI95% 0.04 to 0.75) anxiety disorders. Improvement did not differ significantly between patients with other versus no anxiety disorders (d = −0.09, CI95% −0.43 to 0.24). Post-A-CT, patients with other anxiety disorders had higher depression severity than patients with no (d = 0.51, CI95% 0.22 to 0.81) or social (d = 0.67, CI95% 0.29 to 1.05) anxiety disorder, but patients with social versus no anxiety disorder did not differ significantly (d= −0.16, CI95% −0.47 to 0.16).
Figure 1.
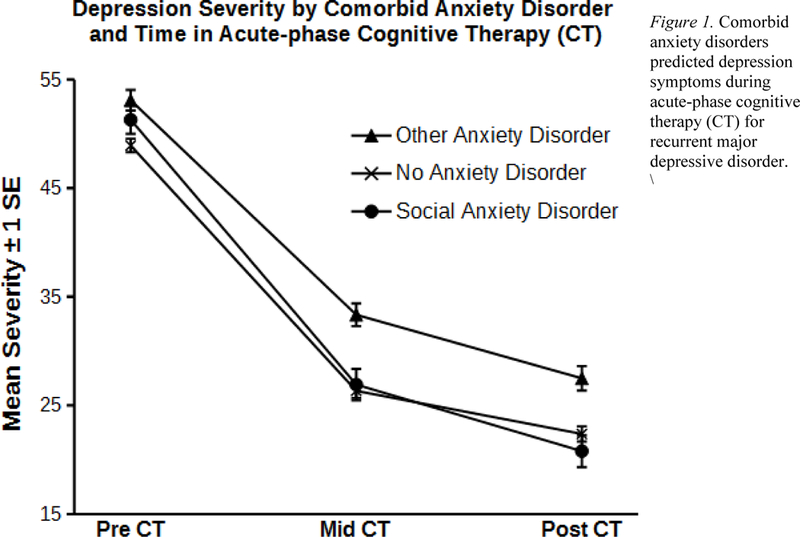
Comorbid anxiety disorders predicted depression symptoms during acute-phase cognitive therapy (CT) for recurrent major depressive disorder.
Finally, we tested whether anxiety disorders predicted A-CT completion and response (Table 4). Completion or response did not differ significantly by any/no or social/other/no anxiety disorder.
Table 4. Prediction of Acute-phase Cognitive Therapy Completion and Response, and Post-Acute Relapse and Recurrence.
| Model | Outcome | Predictors | Beta | SE | Effect size [95% CI] |
|---|---|---|---|---|---|
| 1 | A-CT completion | Any anxiety disorder | −0.019 | 0.245 | 0.98 [0.61,1.59] |
| 2 | A-CT completion | Social and other anxiety disorders: χ2(2) = 0.64, p = .72 | |||
| Social anxiety disorder | 0.198 | 0.308 | 1.22 [0.67,2.23] | ||
| Other anxiety disorder | −0.146 | 0.273 | 0.86 [0.51,1.48] | ||
| Contrast: Social – other | 0.344 | 0.429 | 1.41 [0.61,3.27] | ||
| 3 | A-CT response | Any anxiety disorder | −0.098 | 0.207 | 0.91 [0.60,1.36] |
| 4 | A-CT response | Social and other anxiety disorders: χ2(2) = 2.67, p = .26 | |||
| Social anxiety disorder | 0.280 | 0.264 | 1.32 [0.79,2.22] | ||
| Other anxiety disorder | −0.317 | 0.235 | 0.73 [0.46,1.16] | ||
| Contrast: Social – other | 0.597 | 0.372 | 1.82 [0.88,3.77] | ||
| 5 | Post-A-CT relapse | Any anxiety disorder | 0.107 | 0.335 | 1.11 [0.58,2.15] |
| 6 | Post-A-CT relapse | Social and other anxiety disorders: χ2(2) = 0.46, p = .80 | |||
| Social anxiety disorder | −0.221 | 0.431 | 0.80 [0.34,1.87] | ||
| Other anxiety disorder | 0.224 | 0.408 | 1.25 [0.56,2.78] | ||
| Contrast: Social – other | −0.445 | 0.659 | 0.64 [0.18,2.33] | ||
| 7 | Post-A-CT recurrence | Any anxiety disorder | 0.125 | 0.241 | 1.13 [0.71,1.82] |
| 8 | Post-A-CT recurrence | Social and other anxiety disorders: χ2(2) = 1.99, p = .37 | |||
| Social anxiety disorder | −0.187 | 0.302 | 0.83 [0.46,1.50] | ||
| Other anxiety disorder | 0.411 | 0.295 | 1.51 [0.85,2.69] | ||
| Contrast: Social – other | −0.598 | 0.480 | 0.55 [0.21,1.41] | ||
Note. Models 1–4 are logistic regression predicting outcomes of acute-phase cognitive therapy (A-CT) for recurrent major depressive disorder (N = 523). Models 5–8 are Cox regression survival analyses of A-CT responders’ (N = 290) relapse (over 8 months) or recurrence (over 32 months). Models controlled depressive symptom severity at study intake, age, age of depression onset, education, ethnicity, and gender; and models 5–8 also controlled continuation-phase arm (lower risk responders received no continuation treatment; higher risk responders were randomized to 8 months of cognitive therapy, or clinical management with fluoxetine or pill placebo). Effect sizes for models 1–4 and 5–8 are odds ratios and hazard ratios, respectively. CI = confidence interval.
Responders after Acute-phase CT
Pre-acute-phase anxiety disorders were tested as predictors of outcomes for 32 months after response to A-CT. On average for 32 months after response to acute-phase CT, patients with any versus no anxiety disorder had more anxiety symptoms and more social avoidance but did not differ in level of depressive symptoms (Table 5).
Table 5. Prediction of Anxiety and Depressive Symptoms and Social Avoidance after Acute-phase Cognitive Therapy for Depression.
| Model | Outcome | Predictors | Beta | SE | Effect size d [95% CI] |
|---|---|---|---|---|---|
| 1 | Anxiety Sx | Any anxiety disorder | 0.051*** | 0.012 | 0.32 [0.17,0.47] |
| 2 | Anxiety Sx | Social and other anxiety disorders: F(2,462) = 10.87, p < .001 | |||
| Social anxiety disorder | 0.001 | 0.015 | 0.01 [−0.17,0.18] | ||
| Other anxiety disorder | 0.070*** | 0.015 | 0.44 [0.25,0.62] | ||
| Contrast: Social – other | −0.070** | 0.023 | −0.43 [−0.71,−0.15] | ||
| 3 | Depressive Sx | Any anxiety disorder | 1.617 | 0.901 | 0.16 [−0.02,0.34] |
| 4 | Depressive Sx | Social and other anxiety disorders: F(2,464) = 3.77, p =.02 | |||
| Social anxiety disorder | −0.748 | 1.061 | −0.07 [−0.28,0.13] | ||
| Other anxiety disorder | 3.080** | 1.123 | 0.31 [0.09,0.53] | ||
| Contrast: Social – other | −3.829 | 1.694 | −0.38 [−0.72,−0.05] | ||
| 5 | Social avoidance | Any anxiety disorder | 0.229** | 0.086 | 0.25 [0.06,0.43] |
| 6 | Social avoidance | Social and other anxiety disorders: F(2,311) = 4.04, p = .02 | |||
| Social anxiety disorder | 0.254* | 0.102 | 0.28 [0.06,0.50] | ||
| Other anxiety disorder | 0.099 | 0.108 | 0.11 [−0.12,0.34] | ||
| Contrast: Social – other | 0.156 | 0.161 | 0.17 [−0.18,0.52] | ||
Note. N = 290 responders to acute-phase cognitive therapy for depression, including 241 higher risk and 49 lower risk responders. Anxiety disorders assessed at intake to acute-phase cognitive therapy. Symptom (Sx) and functioning outcome variables assessed every 4 months during the 8-month continuation phase, follow-up year 1, and follow-up year 2 (time period). Models controlled depressive symptom severity at study intake, age, age of depression onset, education, ethnicity, gender, time period, and continuation-phase arm (lower risk responders received no continuation treatment; higher risk responders were andomized to 8 months of cognitive therapy, or clinical management with fluoxetine or pill placebo). Anxiety disorders and time period were dummy coded (1 = present, 0 = absent) and centered. Non-significant (p > .05) interactions of anxiety disorders and time period were trimmed from the final models. CI = confidence interval.
p < .05
p < .01
p < .001.
Similar to the acute phase, results varied by type of anxiety disorder. Responders with social anxiety disorder had greater social avoidance, but did not have significantly more depression or anxiety symptoms, compared to responders with no anxiety disorder. Responders with other versus no anxiety disorders had greater depression and anxiety symptoms but not more social avoidance. Finally, responders with other versus social anxiety disorder had more anxiety and depression symptoms, but not social avoidance (Table 5).
Finally, we predicted time to MDD relapse during the continuation phase (8 months) and relapse/recurrence during the continuation plus follow-up phases (32 total months). Any/noor social/other/no anxiety disorders did not predict relapse or recurrence among A-CT responders (Table 4).
Discussion
The current analyses clarified the potential impact of comorbid social and other (i.e., non-social) anxiety disorders on treatment of MDD with A-CT. Other anxiety disorders predicted more depressive and anxiety symptoms throughout A-CT and for 32 months after A-CT response, on average. In contrast, social anxiety disorder did not predict increased depression or anxiety symptoms during A-CT or for the 32 months following acute-phase response. Instead, social anxiety disorder predicted larger decreases in depression symptoms during A-CT. Even so, social anxiety disorder predicted higher social avoidance throughout A-CT that persisted for 32 months among A-CT responders. Anxiety disorders did not predict categorical A-CT completion, response, or subsequent relapse/recurrence.
Other comorbid anxiety disorders in the current sample (primarily specific phobias, panic disorder, and generalized anxiety disorder) presented a serious challenge during CT for depression. Patients with other anxiety disorders had elevated depressive symptoms both pre-and post-CT, compared to patients without comorbid anxiety disorders. This result matches past studies showing that comorbid anxiety reduced efficacy of antidepressants (e.g., Fava et al., 2008; Saveanu et al. 2015) and interpersonal psychotherapy (van Bronswijk et al., 2018). Our finding that comorbid anxiety disorders did not predict completion of CT for depression also replicated past research (Smits et al., 2009; Forand et al., 2011) and suggested that cognitive therapists engaged these patients successfully.
Engagement in CT may provide a platform to improve treatment of depression with comorbid anxiety. For example, clinicians who provide CT for depression may need to focus more on homework or action plans involving exposure for anxious patients. Additionally, transdiagnostic psychotherapies focusing on core processes underlying anxiety and depression hold potential for improved outcomes by flexibly addressing individual patients’ strengths and weaknesses (Barlow et al., 2017; Titov et al., 2015). These core processes may include both positive (extraversion) and negative (neuroticism or low emotional stability) emotionality that are improved moderately in several types of psychotherapy (Roberts et al., 2017). Although current substance dependence was an exclusionary criterion in the current clinical trial, “self-medication” with alcohol or other substances may also need to be addressed in some patients with depression and comorbid anxiety (Howland et al., 2009; Windle et al., 2012). Finally, functional analysis that was central to “first and second wave” behavioral and cognitive-behavioral therapists’ practice (Ferster, 1973) provided an empirical platform for tailoring treatment to individual patients’ behaviors (e.g., marked by comorbid diagnoses), but may have been deemphasized during the field’s more recent dissemination of disorder-specific protocols. Perhaps new technologies can be developed to assist cognitive behavioral therapists with incorporating functional analyses more fully into their daily practice.
Although comorbid social anxiety disorder did not hinder depression outcomes in CT, the current findings suggest that patients with MDD plus comorbid social anxiety disorder receiving CT for depression may need additional treatment for social avoidance. Focusing on anxiety during CT for depression is one option, but a process study suggested that doing may hamper reduction of both depression and anxiety (Gibbons & DeRubeis, 2008). Instead, increased therapeutic focus on avoidance behavior (e.g., through activity scheduling in CT, including pleasant social activities) might help comorbid patients resolve a “behavioral trap” in which coping with actual or perceived threats of social exclusion by withdrawing is negatively reinforcing in the short-term but in the long-run amplifies negative emotion and dampens positive emotion (Langer & Rodebaugh, 2014 ). Thus, whether CT for depression can be augmented in focus, length, or other parameters to address comorbid social avoidance more fully and effectively, or whether parallel or sequential treatment is needed for social avoidance, are questions requiring empirical clarification.
Patients with comorbid social anxiety disorder had higher depressive symptoms initially but greater reductions in depressive symptoms during A-CT, replicating past research on comorbid anxiety symptoms (Forand et al. 2011; Forand et al., 2013) but not social anxiety disorder (Smits et al., 2009). Whether the difference between the current study and Smits et al. (2009) regarding greater change in depressive symptoms with social anxiety disorder is due to sampling error or some unknown systematic factor (e.g., subtypes of social anxiety or depression) would be an important topic for future research. It is worth noting, for example, that Smits et al (2009) simply compared those with comorbid versus those without comorbid social anxiety disorder without considering or controlling for different anxiety disorder diagnoses. Assuming patients with comorbid social anxiety disorder do experience greater/faster reduction in depressive symptoms during CT for depression, possible explanations might be profitably tested in future research. For example, anxious physiological arousal possibly increases activity level and engagement during CT (Forand et al., 2011), and/or CT might be a better therapeutic “fit” for patients with more strongly decreased positive and increased negative emotionality common to social anxiety and depression (Watson et al., 2005).
Limitations
The current analyses have important limitations. First, assessment of anxiety disorders occurred only before A-CT and not again after response. Consequently, how many patients remitted from anxiety disorders during A-CT and before post-acute data were collected is unknown. Further, inter-rater reliability for anxiety disorder diagnoses was not evaluated in the current clinical trial focused on recurrent MDD. Second, the measure of anxiety symptoms was brief, derived from depression scales, and not designed for the current analytic purposes. Future research using psychometrically stronger, more nuanced measures of depression and anxiety chosen a priori may yield greater insights into treatment issues identified here (e.g., Kessler et al., 2017; Watson et al., 2007). Third, future research with larger samples might allow finer differentiation of other (non-social) anxiety disorders (e.g., generalized anxiety disorder, panic disorder, agoraphobia), their impact on A-CT outcomes, and interactions of anxiety disorders with continuation treatments for A-CT responders. Finally, generalization of the current findings beyond outpatient adults with recurrent MDD who displayed a specific pattern of comorbidity and were treated by expert cognitive therapists is unknown. For example, the study recruited patients who sought CT as first-line treatment for depression, but this group may or may not vary in important ways from patients seeking pharmacotherapy.
Conclusions
Studying comorbidity that influences CT’s efficacy may inform efforts to improve treatment outcomes. Our findings suggest that the influence of comorbid anxiety disorders on the efficacy of CT for patients presenting with recurrent depression may vary depending on the specific anxiety disorder. Anxiety symptoms improved notably during CT for depression in the current dataset, consistent with past research (Weitz et al., 2018). Nonetheless, further improving anxiety and depression outcomes through personalized or precision medicine (Simon & Perlis, 2010) may require modifying, augmenting, tailoring a focus to comorbid symptoms or underlying processes (i.e., core perceived threats, maladaptive safety/avoidance behaviors), or sequencing CT for depression with comorbid social or other anxiety disorders. The current findings present some initial guidance in these efforts by addressing patient outcomes in A-CT and 32 months after response.
Supplementary Material
Highlights.
Cognitive therapy (CT) for major depressive disorder (MDD) is often helpful.
We predicted outcomes for CT patients with MDD plus anxiety disorders.
Social anxiety disorder did not limit depression outcomes during or after CT.
Other anxiety disorders predicted more depression symptoms during and after CT.
Modified treatment may improve outcomes for MDD with other anxiety disorders.
Acknowledgments
We appreciate the careful review by members of the trial’s Data Safety and Monitoring Board. We are indebted to our research teams and our colleagues at The University of Texas Southwestern Medical Center, the University of Pittsburgh (where Dr. Thase was located during patient accrual), and the University of Pennsylvania (Dr. Thase’s current affiliation).We appreciate the participation of colleagues, previously named, and study participants without whom such research could not have been completed.
Funding
This report was supported by Grants Number K24 MH001571, R01 MH58397, R01 MH69619 (to Robin B. Jarrett, Ph.D.) and R01 MH58356 and R01 MH69618 (to Michael E. Thase, M.D.) from the National Institute of Mental Health (NIMH). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Notes
Two patients entered CT erroneously with HRSD = 13 at one of two diagnostic visits. During CT, one of these patients responded and one dropped out. As recommended by the Data Safety and Monitoring Board (DSMB), the patients are analyzed here as they were treated during data collection.
Four patients were incorrectly assigned to 16 or 20 session protocols. As recommended by the DSMB, they are analyzed here as they were treated during data collection.
Three non-responders were randomized in error. As recommended by the DSMB, they are analyzed here as they were treated during data collection. Also, during the final years of randomization, allocation to placebo was reduced to increase the proportions of patients randomly assigned to the two depression-specific treatments.
We computed alpha internal consistency reliability estimates after pooling data across time points because measures had restricted ranges at some points in the clinical trial (e.g., pre-treatment when all patients had MDD).
Contributor Information
Jeffrey R. Vittengl, Department of Psychology, Truman State University.
Lee Anna Clark, Department of Psychology, University of Notre Dame.
Jasper A. J. Smits, Department of Psychology, University of Texas at Austin
Michael E. Thase, Department of Psychiatry, Perelman School of Medicine, University of Pennsylvania
Robin B. Jarrett, Department of Psychiatry, The University of Texas Southwestern Medical Center.
References
- Adams GC, Balbuena L, Meng X, & Asmundson GG, 2016. When social anxiety and depression go together: A population study of comorbidity and associated consequences. J. Affect. Disord 206, 48–54. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, 2000. Diagnostic and Statistical Manual of Mental Disorders, fourth ed., text rev. American Psychiatric Association, Washington, DC. [Google Scholar]
- American Psychiatric Association, 2013. Diagnostic and Statistical Manual of Mental Disorders, fifth ed., American Psychiatric Association, Washington, DC. [Google Scholar]
- Andreescu C, Lenze EJ, Dew MA, Begley AE, Mulsant BH, Dombrovski AY, & Reynolds CF, 2007. Effect of comorbid anxiety on treatment response and relapse risk in late-life depression: Controlled study. Br. J. Psychiatry 190, 344–349. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Bullis JR, Gallagher MW, Murray-Latin H, Sauer-Zavala S….Cassiello-Robbins C, 2017. The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders compared with diagnosis-specific protocols for anxiety disorders: A randomized clinical trial. JAMA Psychiatry 74, 875–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, & Erbaugh J, 1961. An inventory for measuring depression. Arch. Gen. Psychiatry 4, 561–571. [DOI] [PubMed] [Google Scholar]
- van Bronswijk SC, Lemmens LHJM, Huibers MJH, Arntz A, Peeters FPML, 2018. The influence of comorbid anxiety on the effectiveness of cognitive therapy and interpersonal psychotherapy for major depressive disorder. J. Affect. Disord 10.1016/j.jad.2018.02.003 [DOI] [PubMed]
- Brown TA, Chorpita BF, & Barlow DH, 1998. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. J. Abnorm. Psychol 107, 179–192. [DOI] [PubMed] [Google Scholar]
- Burcusa SL, & Iacono WG, 2007. Risk for recurrence in depression. Clin. Psychol. Rev 27, 959–985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, & Watson D, 1995. Constructing validity: Basic issues in objective scale development. Psychol. Assess 7, 309–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS, 2003. Applied Multiple Regression/correlation Analysis for the Behavioral Sciences, third ed. Lawrence Erlbaum Associates Publishers; Mahwah, NJ. [Google Scholar]
- Coplan JD, Aaronson CJ, Panthangi V, Kim Y, 2015. Treating comorbid anxiety and depression: Psychosocial and pharmacological approaches. World J. Psychiatry 5, 366–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, Gallop R, 2005. Cognitive therapy vs medications in the treatment of moderate to severe depression. Arch. Gen. Psychiatry 62, 409–416. [DOI] [PubMed] [Google Scholar]
- Dunn TW, Vittengl JR, Clark LA, Carmody T, Thase ME, & Jarrett RB, 2012. Change in psychosocial functioning and depressive symptoms during acute-phase cognitive therapy for depression. Psychol. Med 42, 317–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farabaugh A, Alpert J, Wisniewski SR, Otto MW, Fava M, Baer L, ... Thase ME, 2012. Cognitive therapy for anxious depression in STAR(*) D: what have we learned?. J. Affect. Disord 142, 213–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fava M, Rush AJ, Alpert JE, Balasubramani GK, Wisniewski SR, Carmin CN, & ... Trivedi MH, 2008. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am. J. Psychiatry 165, 342–351. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Epstein P, Fiester S, Elkin I, & Autry J, 1987. Clinical management--imipramine/placebo administration manual. NIMH Treatment of Depression Collaborative Research Program. Psychopharmacol. Bull 23, 309–324. [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB, 1996. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID-I/P, Version 2.0) New York State Psychiatric Institute, Biometrics Research Department, New York. [Google Scholar]
- Ferster CB, 1973. A functional analysis of depression. Am. Psychol 28, 857–870. [DOI] [PubMed] [Google Scholar]
- Forand NR, Gunthert KC, Cohen LH, Butler AC, & Beck JS, 2011. Preliminary evidence that anxiety is associated with accelerated response in cognitive therapy for depression. Cognit. Ther. Res 35, 151–160. [Google Scholar]
- Forand NR, & DeRubeis RJ, 2013. Pretreatment anxiety predicts patterns of change in cognitive behavioral therapy and medications for depression. J. Consult. Clin. Psychol 81, 774–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank E, Cassano GB, Rucci P, Thompson WK, Kraemer HC, Fagiolini A, & ... Forgione RN, 2011. Predictors and moderators of time to remission of major depression with interpersonal psychotherapy and SSRI pharmacotherapy. Psychol. Med 41, 151–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M, 1960. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz LM, Alden LE, Wiggins JS, & Pincus AL, 2000. Inventory of Interpersonal Problems Manual Psychological Corporation, Odessa, Florida. [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureño G, Villaseñor VS, 1988. Inventory of interpersonal problems: psychometric properties and clinical applications. J. Consult. Clin. Psychol 56, 885–892. [DOI] [PubMed] [Google Scholar]
- Howland RH, Rush AJ, Wisniewski SR, Trivedi MH, Warden D, Fava M, ... Berman SR, 2009. Concurrent anxiety and substance use disorders among outpatients with major depression: clinical features and effect on treatment outcome. Drug Alcohol Depend 99, 248–260. [DOI] [PubMed] [Google Scholar]
- Jarrett RB, Thase ME, 2010. Comparative efficacy and durability of continuation phase cognitive therapy for preventing recurrent depression: design of a double-blinded, fluoxetine-and pill placebo-controlled, randomized trial with 2-year follow-up. Contemp. Clin. Trials 31, 355–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrett RB, Minhajuddin A, Gershenfeld H, Friedman ES, Thase ME, 2013. Preventing depressive relapse and recurrence in higher risk cognitive therapy responders: A randomized trial of continuation phase cognitive therapy, fluoxetine, or matched pill placebo. JAMA Psychiatry 70, 1152–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrett RB, Minhajuddin A, Vittengl JR, Clark LA, Thase ME, 2016. Quantifying and qualifying the preventive effects of acute-phase cognitive therapy: Pathways to personalizing care. J. Consult. Clin. Psychol 84, 365–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrett RB, Vittengl JR, Clark LA, 2008. Preventing recurrent depression, Whisman MA (Ed.), Adapting Cognitive Therapy for Depression: Managing Complexity and Comorbidity Guilford Press, New York, pp. 132–156. [Google Scholar]
- Jarrett RB, 1989. Cognitive therapy for recurrent unipolar major depressive disorder: The continuation/maintenance phase. Unpublished treatment manual.
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC, 1987. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Arch. Gen. Psychiatry 44, 540–548. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE, 2005. Prevalence, severity, and comorbidity of 12-Month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62, 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, van Loo HM, Wardenaar KJ, Bossarte RM, Brenner LA, Ebert DD, & Zaslavsky AM, 2017. Using patient self-reports to study heterogeneity of treatment effects in major depressive disorder. Epidemiol. Psychiatr. Sci 26, 22–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langer JK, & Rodebaugh TL, 2014. Comorbidity of social anxiety disorder and depression, Richards CS, & O’Hara MW (Eds.), The Oxford Handbook of Depression and Comorbidity Oxford University Press, New York, pp. 111–128. [Google Scholar]
- Petersen T, Andreotti CF, Chelminski I, Young D, & Zimmerman M, 2009. Do comorbid anxiety disorders impact treatment planning for outpatients with major depressive disorder? Psychiatry Res 169, 7–11. [DOI] [PubMed] [Google Scholar]
- Renner F, Jarrett RB, Vittengl JR, Clark LA, Thase ME, 2012. Interpersonal problems as predictors of therapeutic alliance and symptom improvement in cognitive therapy for depression. J. Affect. Disord 138, 458–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Luo J, Briley DA, Chow PI, Su R, Hill PL, 2017. A systematic review of personality trait change through intervention. Psychol. Bull 143, 117–141. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH, 1996. The Inventory of Depressive Symptomatology (IDS): Psychometric properties. Psychol. Med 26, 477–486. [DOI] [PubMed] [Google Scholar]
- Saveanu R, Etkin A, Duchemin A, Goldstein-Piekarski A, Gyurak A, Debattista C, & ... Williams LM, 2015. The International Study to Predict Optimized Treatment in Depression (iSPOT-D): Outcomes from the acute phase of antidepressant treatment. J Psychiatr. Res 61, 1–12. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW, 2002. Missing data: our view of the state of the art. Psychol. Methods 7, 147–177. [PubMed] [Google Scholar]
- Schaffer A, Mcintosh D, Goldstein BI, Rector NA, McIntyre RS, Beaulieu S, & ... Yatham LN, 2012. The Canadian Network for Mood and Anxiety Treatments (CANMAT) task force recommendations for the management of patients with mood disorders and comorbid anxiety disorders. Ann. Clin. Psychiatry 24, 6–22. [PubMed] [Google Scholar]
- Schoevers RA, Van HL, Koppelmans V, Kool S, Dekker JJ, 2008. Managing the patient with co-morbid depression and an anxiety disorder. Drugs 68, 1621–1634. [DOI] [PubMed] [Google Scholar]
- Simon GE, & Perlis RH, 2010. Personalized medicine for depression: Can we match patients with treatments? Am. J. Psychiatry 167, 1445–1455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JAJ, Minhajuddin A, Jarrett RB, 2009. Cognitive therapy for depressed adults with comorbid social phobia. J. Affect. Disord 114, 271–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smits JAJ, Minhajuddin A, Thase ME, & Jarrett RB, 2012. Outcomes of acute phase cognitive therapy in outpatients with anxious versus nonanxious depression. Psychother. Psychosom 81, 153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Titov N, Dear BF, Staples LG, Terides MD, Karin E, Sheehan J, & ... McEvoy PM, 2015. Disorder-specific versus transdiagnostic and clinician-guided versus self-guided treatment for major depressive disorder and comorbid anxiety disorders: A randomized controlled trial. J. Anxiety Disord 35, 88–102. [DOI] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Kraft D, Jarrett RB, 2005. Multiple measures, methods, and moments: A factor-analytic investigation of change in depressive symptoms during acute phase cognitive therapy. Psychol. Med 35, 693–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Thase ME, Jarrett RB, 2013. Nomothetic and idiographic symptom change trajectories in acute-phase cognitive therapy for recurrent depression. J. Consult. Clin. Psychol 81, 615–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Thase ME, Jarrett RB, 2014. Stable remission and recovery after acute-phase cognitive therapy for recurrent major depressive disorder. J. Consult. Clin. Psychol 82, 1049–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Thase ME, Jarrett RB, 2016. Longitudinal social-interpersonal functioning among higher-risk responders to acute-phase cognitive therapy for recurrent major depressive disorder. J. Affect. Disord 199, 148–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Carey G, 1988. Positive and negative affectivity and their relation to anxiety and depressive disorders. J. Abnorm. Psychol 97, 346–353 [DOI] [PubMed] [Google Scholar]
- Watson D, Gamez W, & Simms LJ, 2005. Basic dimensions of temperament and their relation to anxiety and depression: A symptom-based perspective. J. Res. Pers 39, 46–66. [Google Scholar]
- Watson D, O’Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA, & ... Stuart S, 2007. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS). Psychol. Assess 19, 253–268. [DOI] [PubMed] [Google Scholar]
- Weitz E, Kleiboer A, van Straten A, & Cuijpers P, 2018. The effects of psychotherapy for depression on anxiety symptoms: a meta-analysis. Psychol. Med 10.1017/S0033291717003622 [DOI] [PubMed]
- Windle M, & Windle RC (2012). Testing the specificity between social anxiety disorder and drinking motives. Addict. Behav 37, 1003–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AC, Hallquist MN, Swartz HA, Frank E, & Cyranowski JM, 2014. Treating co-occurring depression and anxiety: Modeling the dynamics of psychopathology and psychotherapy using the time-varying effect model. J. Consult. Clin. Psychol 82, 839–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young J, Beck AT, 1980. Cognitive Therapy Scale: Rating Manual Center for Cognitive Therapy, Philadelphia, PA. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


