Abstract
A key predictor of whether or not an individual who hears voices (auditory verbal hallucinations; AVH) meets criteria for a psychiatric diagnosis is the level of negative content of the voices (e.g., threats, criticism, abuse). Yet the factors that contribute to negative voice-content are still not well understood. This study aimed to test the hypotheses that levels of childhood adversity would predict levels of negative voice-content, and that negative voice-content would partially mediate a relation between childhood adversity and voice-related distress. These hypotheses were tested in a clinical sample of 61 patients with formally diagnosed psychotic disorders (48 schizophrenia, 13 bipolar). We found evidence consistent with negative voice-content fully (not partially) mediating the relation between childhood adversity and voice-related distress. Although bivariate analyses found depression to be associated with both negative voice-content and voice-related distress, we found no evidence of an indirect effect of childhood adversity on either negative voice-content or voice-related distress via depression. Alternative study designs are now needed to test if our findings are replicable and causal. Should they be, it will be necessary for psychological therapies to devise ways to reduce negative voice-content itself, rather than just changing beliefs about voices. A number of techniques are discussed (Avatar Therapy, Compassion Focused Therapy, voice-dialogue) that already show promise for this.
Keywords: cognitive model, trauma, voice-hearing
Introduction
Auditory verbal hallucinations (AVH), also described as ‘hearing voices’ or ‘voice-hearing’, refer to the experience of hearing a voice in the absence of an external stimulus. Approximately two-thirds of people with a schizophrenia-spectrum diagnosis will have experienced AVH (Thomas et al., 2007; McCarthy-Jones et al., 2017b) and around a quarter of those with longstanding such diagnoses will have experienced them in the past month (McCarthy-Jones et al., 2017b). There is no necessary link between AVH and distress or dysfunction (Johns et al., 2014; Krakvik et al., 2015; Daalman et al., 2011; Honig et al., 1998; Romme & Escher, 1993) and these experiences may or may not be problematic (Laroi, 2012). This raises the important clinical question as to why some AVH lead to distress or dysfunction and others do not.
Cognitive models of AVH have stressed the role of hearers’ beliefs about their voices in determining ensuing levels of distress (Chadwick & Birchwood, 1994). In particular, beliefs about voice omnipotence (perceived power) and voice intent (perceived malevolence) have been found to predict levels of voice-related distress (Peters et al., 2012; Cole et al., 2017). While addressing the link between appraisal processes and distress is an important clinical task, the focus on hearers’ beliefs about their voices has drawn attention away from the role voice-content itself may play in causing distress and the need to develop new methods to attempt to address this (although, of course, even in clinical populations, not all voice-hearing causes distress) (McCarthy-Jones, 2014a). Peters et al (2012), claim that “it’s not what you hear, it’s the way you think about it” could be taken to suggest the independence of beliefs about voices from voice-content. This does not seem plausible. Indeed, even Chadwick & Birchwood’s (1994) seminal paper, which launched cognitive models of AVH, stressed the importance of voice-content, noting that “voice content was frequently put forward [by voice-hearers] as evidence for a particular belief” (p. 192). The importance of this, clinically, is that it suggests that attempting to reduce distress exclusively by changing beliefs about voices is likely to be ineffective unless interventions also alter voice content.
One property of voice-content that would appear to have a prima facie relationship with voice-distress is negative valence. The majority of people with a diagnosis of schizophrenia with AVH will hear voices with negative content, i.e., ones which threaten, criticize, abuse, or shame them (Connor & Birchwood, 2013; McCarthy-Jones et al., 2014b; Nayani & David, 1996). The important clinical implications of negative voice-content have been demonstrated by a study by Daalman et al (2011) that found that negative voice-content could accurately predict patient status in 88% of people hearing voices. This work foregrounds the importance of understanding the causes and drivers of negative content.
It has previously been suggested that the content of AVH is related to “the stresses that precipitate” them (Bentall, 1990). One key such stressor appears likely to be childhood adversity, which has repeatedly been found to be associated with AVH (Bentall et al., 2012; Read & Argyle, 1999; Read et al., 2003; Morrison & Petersen, 2003; Offen et al., 2003; Shevlin et al., 2007). A number of studies have provided evidence of links between AVH content and earlier adverse experiences. For example, Reiff et al (2012) found that 76% of participants diagnosed with schizophrenia-spectrum disorders, who had experienced physical/sexual abuse as children, made links between the abuse they experienced and the content of their hallucinations. Corstens & Longden (2013) found that 94% of voice-hearers (the majority of whom had been diagnosed with schizophrenia) had voices whose content could be related to earlier emotionally overwhelming events. A number of other studies have also reported associations between the nature of stressors/traumas preceding AVH and the content of the ensuing AVH (Hardy et al., 2005; Thompson & Waltz, 2010; Raune et al., 2006; Rosen et al., 2017).
Surprisingly though, Daalman et al (2011), failed to find an association, in a mixed sample of clinical and non-clinical participants with AVH, between sexual or emotional abuse and what they termed the ‘emotional valence of content’; a composite measure made up of three PSYRATS-AH (Haddock et al., 1999) items (amount of negative content, degree of negative content, and amount of distress). However, it is possible that the limited number of abuse experiences they examined, and the use of dichotomized measures of abuse experiences, may have limited the sensitivity of their analyses, leading to Type II error.
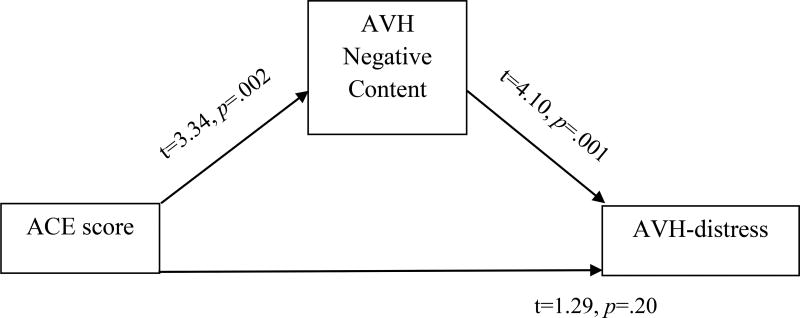
Based on the research discussed above, we hypothesized that levels of childhood adversity in people who heard voices would be positively associated with negative voice-content. We also hypothesized that levels of negative voice-content would be positively associated with levels of voice-related distress. These two hypotheses are combined in the mediation model depicted in Figure 1, in which negative voice-content mediates the relationship between childhood adversity and voice-distress. Given the potential for a range of other factors to influence voice-distress, we hypothesized that negative voice-content would only partially, rather than fully, mediate the relationship between childhood adversity and voice-related distress. The model was tested in a clinical population of people with formally diagnosed psychotic disorders.
Figure 1.
Results of primary mediation analysis
Note. Total effect of ACE score on AVH-distress is significant, b=0.26, SE=0.09, 95% CI=0.08 – 0.44, p=.006. Indirect effect of ACE score on AVH-distress via AVH negative-content is significant, b=.14, SE = 0.05, 95% CI = 0.05 – 0.30, p<.05.
Method
Study Design
The clinical sample was selected from a large urban university medical center that included referrals from community treatment facilities. The study was approved by the University of Illinois at Chicago Internal Review Board (IRB2012-0113) and was conducted in accordance with the latest version of the Declaration of Helsinki (General Assembly of the World Medical Association, 2014). All participants gave signed written consent. Inclusion criteria for the clinical sample were that they should be between the ages of 21 – 60 years and meet diagnostic criteria for schizophrenia or bipolar disorder/psychosis with current state psychosis. Exclusion criteria included current substance dependence, seizure disorders, current pregnancy, and neurological conditions.
Participants
Sixty-one participants (33 female) who had experienced AVH in the past week and had a consensus diagnosis, determined by the clinical and research team using the Structured Clinical Diagnostic Interview, SCID-IV (First et al., 2002), of either schizophrenia (n=48) or bipolar with psychosis (n=13) took part in the study. There was a mean age of 47.98 years (SD=11.09; range 20–65) with 77% identifying as African American, 15% Caucasian, and 8% Hispanic. At the time of the study evaluation many of the participants were taking atypical antipsychotic medications (n=33 schizophrenia, n=10 bipolar), with a smaller subsample taking typical antipsychotics (n=5 schizophrenia, n=0 bipolar). Antipsychotic use for participants with schizophrenia was converted to chlorpromazine equivalents (CPZE) (Danivas & Venkatasubramanian 2013; Gardner et al., 2010). Additionally, there were some participants currently taking antidepressant medications (n =22 schizophrenia, n=5 bipolar).
Measures
Childhood adversity (CA)
CA was assessed using the Adverse Childhood Experiences (ACE) questionnaire (Reavis 2013). This is a ten-item questionnaire that assesses the presence of experiences related to abuse (emotional, physical, and sexual), neglect (emotional and physical), and household dysfunction (battered mother, parental abandonment, substance-abusing, mentally ill, or incarcerated household member in the household) occurring before a person’s 18th birthday. Total scores can range from 0 to 10, with higher scores indicating a greater number of types of adverse childhood experiences.
Auditory verbal hallucinations
AVH were assessed using the auditory hallucination subscale of the Psychotic Symptom Rating Scale (PSYRATS-AH; Haddock et al., 1999). This multidimensional tool assesses eleven dimensions of AVH over the past week: frequency, duration, location, loudness, loudness, beliefs re-origin, negative content (two items: amount and intensity), distress (two items: amount and intensity), disruption, and controllability. Each item is scored on a five-point Likert scale (0–4). For the purpose of this study, the two PSYRATS-AH negative content items were summed into a new ‘negative voice-content’ variable, and the two distress items were summed into a new ‘voice-related distress’ variable in order to increase the sensitivity of our analyses. Summed total scores on each of these items could therefore range from 0–8. Both variables had satisfactory internal reliability (Cronbach’s alpha = .85 and .88, respectively).
Depression
This was assessed using scores on the Depression factor of the Positive and Negative Syndrome Scale (PANSS; Kay et al., 1989). This factor comprises items assessing somatic concern, anxiety, guilt feelings, depression, and preoccupation. Each item is scored on a seven-point Likert scale, which ranges from 1 (asymptomatic) to 7 (extreme symptom severity) and the items are summed to give an overall score for the factor (Lindenmayer et al., 1994; Lehoux et al., 2009). The internal reliability score for the PANSS Depression factor score (Cronbach’s alpha = .79) was satisfactory.
Statistical Analyses
Total, direct and indirect (via negative voice-content) associations between ACE scores and voice-relate distress were first tested using the PROCESS computational tool (model 4; Hayes, 2017) in SPSS v.22, which provides a regression-based approach for testing for mediation. Bias corrected, bootstrapped 95% confidence intervals were used to test for an indirect relationship between these variables via negative voice-content scores. Age, gender, CPZ, and antidepressant usage were to be entered as covariates if they demonstrated relations with the study variables. Covariates were to be used in models of both the mediator and the dependent variable.
At the suggestion of an anonymous reviewer, we also examined the association between the study variables and depression, and tested a revised serial mediation model in which relations between childhood adversity and negative voice-content were mediated by depression, and relations between depression and voice-related distress were mediated by negative voice-content.
Results
ACE and AVH
Mean scores for the study measures were ACE=4.28 (SD=2.66, range 0–10, Cronbach’s α=.75), voice related-distress=4.26 (SD=1.99, range 0–8, α=.88) and negative voice-content=4.98 (SD=2.24, range 0–8, α=.85). Only 6 people (10% of sample) had a zero ACE score. Full PSYRATS-AH data is presented in Table 1.
Table 1.
Bivariate correlations between ACE and PSYRATS-AH total and item scores
| Item | Mean (SD) | Range |
|---|---|---|
| 1. Frequency | 2.57 (1.28) | 0 – 4 |
| 2. Duration | 2.64 (1.18) | 0 – 4 |
| 3. Location | 2.20 (1.09) | 0 – 4 |
| 4. Loudness | 1.90 (0.81) | 0 – 4 |
| 5. Beliefs re-origin | 2.72 (1.13) | 1 – 4 |
| 6. Amount of negative content | 2.34 (1.14) | 0 – 4 |
| 7. Degree of negative content | 2.64 (1.27) | 0 – 4 |
| 8. Amount of distress | 2.20 (1.08) | 0 – 4 |
| 9. Intensity of distress | 2.07 (1.03) | 0 – 4 |
| 10. Disruption | 1.39 (0.86) | 0 – 3 |
| 11. Control | 2.82 (1.16) | 0 – 4 |
| Total Scale Score | 25.49 (7.14) | 4 – 38 |
Sex was not associated with ACE score, t(59)=0.95, p=.35, voice-related distress, t(59)=0.82, p=.42, or negative voice-content, t(59)=0.74, p=.46. It was hence not included as a covariate in our mediation analyses. Age was associated with voice-related distress, r(59)=0.26, p=.04, and negative voice-content, r(59)=0.47, p<.001, but not ACE score, r(59)=0.18, p=.16. It was hence included as a covariate in our mediation analyses.
There was no evidence that medications patients were taking were associated with their levels of either negative voice-content or voice-related distress. Current antipsychotic dosage (CPZ equivalent) did not correlate with either negative voice-content, r(45)=.22, p=.14, or voice-related distress, r(45)=.13, p=.38, in the subsample of patients for whom this data was available. Patients currently on antidepressants (n=27) did not differ in levels of negative voice-content, t(59)=0.18, p=.86, or voice-related distress, t(59)=-0.50, p=.62. Medication use was hence not included as a covariate in our mediation analyses.
Correlations between ACE scores and PSYRATS-AH total and item-scores are presented in Table 2. There was a significant correlation between voice-related distress and negative voice-content, r(59)=.59, p<.001.
Table 2.
Bivariate correlations between ACE and PSYRATS-AH total and item scores
| PSYRATS-AH | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Item #1 | Item #2 | Item #3 | Item #4 | Item #5 | Σitems #6–7 | Σitems #8–9 | Item #10 | Item #11 | |
| score | Frequency | Duration | Location | Loudness | Beliefs reorigin |
Negative content |
Distress | Disruption | Controllability | |
| Pearson’s r | .43 | .28 | .24 | .07 | .07 | .13 | .44 | .38 | .16 | .26 |
| 95% CI* | .25 to .62 | .03 to .52 | −.03 to .48 | −.17 to .34 | −.16 to .32 | −.15 to .42 | .22 to .62 | .14 to .58 | −.07 to .42 | .02 to .48 |
| p | <.001 | .026 | .064 | .578 | .608 | .311 | <.001 | .003 | .211 | .044 |
1,000 bootstrapped samples.
Mediation analysis was first undertaken to test for the pattern of relations shown in Figure 1. This analysis include age as a covariate. A significant total effect of ACE scores on voice-related distress was found, b=0.26, SE=0.09, 95% CI=0.08 – 0.44, p=.006. There was no direct effect of ACE scores on voice-related distress, b=0.11, SE=0.09, 95% CI= −0.06 – 0.29, p=.20. However, there was an indirect effect of ACE scores on voice-related distress via negative voice-content, b=0.14, SE=0.05, 99% CI = 0.05 – 0.30. This is represented graphically in Figure 1. The pattern of significance of these results did not change when age was not controlled for.
At the suggestion of an anonymous reviewer, we examined if depression potentially played a significant role in voice-related distress and negative voice-content. There was a significant positive bivariate correlation between depression and both negative voice-content, r(59)= .42, p=.001, and voice-related distress, r(59)=.42, p=.001. Given the well-documented association between childhood adversity and depression (Anda et al., 2002; Lindert et al., 2014) we hypothesized that childhood adversity would lead to increased levels of depression, which would drive negative voice-content which would in turn increase levels of voice-related distress.
This led us to first test the hypothesis that there would be an indirect effect of childhood adversity on negative voice-content via depression. Using the PROCESS macro (model 4), and controlling for age, we found no evidence of such an indirect effect, b=0.05, SE = 0.03, 95% CI = −0.01 – 0.13, p >.05. We next tested the serial mediation model presented in Figure 2 (using PROCESS model 6). Necessarily, the total and direct effects of ACE score on voice-related distress were identical to our previous analyses. However, three new indirect effects of ACE scores on voice-related distress were tested for; 1) ACE→ depression → voice-related distress; 2) ACE → depression → negative voice-content → voice-related distress; 3) ACE → negative voice-content → voice-related distress). To reduce the probability of Type I error, significance was set at p=.01 (employing 99% confidence intervals). There only significant indirect effect of ACE scores on voice-related distress was via negative voice-content (ACE → negative voice-content → voice-related distress), b=.10, SE = 0.04, 99% CI 0.02 – 0.23, p <.01.
Figure 2.
Results of secondary mediation analysis
Note. Controlling for age. The only significant indirect effect of ACE score on AVH-distress was via AVH negative content (i.e., ACE→AVH negative-content→ AVH-distress), b=.10, SE = 0.04, 99% CI = 0.02 – 0.23, p<.01.
Discussion
The results of this study not only provided evidence of a positive association between levels of childhood adversity and voice-related distress, but also found evidence consistent with this relation being fully mediated by negative voice-content. If this association between childhood adversity and negative voice-content proves to be replicable, future research would then need to assess whether this relationship is causal—i.e. whether childhood adversity engenders negative voice-content, in turn engendering voice-related distress. There are strong theoretical reasons for suspecting that this would be the case. While there are multiple models of AVH (Jones, 2010), there are good reasons to suspect that at least some AVH are forms of trauma memory (Hardy, 2017) meaning that voice-content is likely to reflect these negative past experiences. It has also been argued that some AVH result from hypervigilance for threat after stressful life event, which leads to negative voice-content (Dodgson & Gordon, 2009). Such models provide a theoretical basis for expecting a causal association between adverse experiences and negative voice-content.
Although bivariate analyses found a positive association between depression and both negative voice content and voice-related distress, we failed to find evidence that the relation between ACE scores and negative voice-content was mediated by depression. This was in part due to a failure to find a relation between ACE scores and depression in the current sample. Given the well-documented association between childhood adversity and later life depression (Anda et al., 2002; Lindert et al., 2014), a failure to find such a relation in our data was surprising. Better powered study and dedicated measures of depression should be utilized by future research to further study this potential relation.
In terms of the potential clinical implications of our study, our results suggest the hypothesis that reducing negative voice-content should lead to a reduction in voice-related distress. If the association we found between childhood adversity and negative voice-content were to be causal, then this suggests that negative voice-content could be reduced through trauma-focused interventions. However, at present there is very little research that speaks to how trauma-focused interventions can impact voice-hearing in people with a history of childhood trauma. Whilst a recent meta-analysis found only a small, non-significant effect of such interventions on hallucinations (Brand et al., 2017) three of the four studies included employed EMDR and all employed the outcome measure of the Psychotic Symptom Ratings Scale (Haddock et al., 1999). The use of such a global measure of AVH-severity has previously been criticized for being employed in studies which appear to only hypothesize changes to specific aspects of AVH, hence limiting their power to detect effects (McCarthy-Jones, 2014a). More empirical research is needed into this question. If negative voice-content can be changed, it appears there are two classes of way in which this could be done; ‘objectively’ and ‘subjectivity’. A subjective reduction in negative voice-content would involve a change in the hearer’s beliefs about what the voice is saying, without any change in the voice itself. This is what is traditionally attempted by cognitive behavioral therapy for voice-hearing (Peters et al., 2012). A similar process can be seen in the Hearing Voices Movement approach. Here the message of the voice can be treated as being metaphorical. For example, a voice advising the person to kill themselves could be interpreted as a potentially helpful alert that one needs to make significant changes in part of one’s life (McCarthy-Jones, 2017a).
In contrast, an alternative approach would be to attempt an ‘objective’ reduction in negative voice-content. This would involve the negative utterances of the voice itself changing, for example, by no longer issuing threats, abuse or criticism. Ways to do this are much more underdeveloped, in part due to the dominant focus on appraisals in the cognitive model of AVH (McCarthy-Jones, 2014a). One therapeutic approach which has attempted to engender such ‘objective’ reductions in negative voice-content is AVATAR therapy (Leff et al., 2013; Craig et al., 2018).
AVATAR therapy uses a virtual reality paradigm to allowed controlled interactions between a patient and a mock-up of their dominant voice, which is role-played by the therapist (Leff et al., 2014). It attempts to facilitate a dialogue between the patient and their dominant voice in which “the patient is enabled to gain control and the persecutor mellows” (Leff et al., 2013, p. 428). Thus an explicit aim of this therapy is to alter voice-content objectively. It proposes to do this through the therapist changing the character of the avatar, from initially being critical and abusive to eventually becoming helpful and supportive. The assumption here is that this will encourage similar changes in the patient’s own persecutory voice (Leff et al., 2013). This process involves encouraging patients to tell the avatar that they will only listen when it says pleasant things, the patient going through a list of their positive qualities with the avatar, and the physical expression of the avatar changing from being menacing or neutral to smiling (Leff et al., 2014). The theoretical underpinnings of this approach are that the negative content of voices are a reflection of the patients’ own self-critical thoughts (Leff et al., 2014). Narrative descriptions have been given of reductions in negative voice-content as a result of this process (Leff et al., 2014). However, a recent large randomised controlled trial of this approach (Craig et al., 2018) while reporting specifically on changes in frequency and distress relating to voice-hearing, did not report on changes in negative content. Given that the study employed the Psychotic Rating Symptom Scale (Haddock et al., 1999), data on both the amount and degree of negative voice-content was collected by the trial, and would be interesting to examine.
Similar to the approach advocated by AVATAR therapy, another way to alter ‘objectively’ negative voice-content could be through specifically increasing self-compassion in patients. A small case study of Compassion Focused Therapy (N=3) has reported that helping patients to develop self-compassion and self-soothing abilities “had a major effect on voice-hearers’ hostile voices, changing them into more reassuring, less persecutory and less malevolent voices” (Mayhew & Gilbert, 2008). Similarly, enhancing self-esteem could also potentially reduce ‘objectively’ negative voice-content. One way to do this would be to increase the accessibility of positive self-schema. Ways to do this have been designed by both Group Person-Based Cognitive Therapy (Chadwick, 2006) an approach which integrates cognitive therapy and mindfulness, as well as the technique of Competitive Memory Training (van der Gaag et al., 2012) which involves patients being asked to recall previous experiences of being successful or competent (see Fielding-Smith et al., 2015 for a useful review) . Other possibilities are to develop new positive self-schema, potentially through assertiveness training (Hayward et al., 2009). Finally, within the Hearing Voices Movement the technique of voice-dialogue has some anecdotal ability to reduce negative voice-content through engaging in reasoning, conversation and understanding with the voice (Corstens & Longden, 2013). Aspects of all such approaches could be used by therapists, with there being some suggestion that this could help both objective and subjective voice-content (Kennedy & Ellerby, 2016). However, formal trials of such approaches’ ability to specifically alter negative voice-content, and the impact of this on levels of distress, are required.
This study had a number of limitations. First, experiencing childhood adversity is also associated with a number of other forms of adversity experienced later in life including poverty, substance use, ongoing victimization, and incarceration, which could have acted as a confound. Alternatively though, these factors could be mediators of the relation between childhood adversity and negative voice-content, not confounds. A more comprehensive study is needed that assesses historical and contemporary experiences of adversity, relational challenges and psychological dynamics (e.g., attachment, schema, self-esteem, ability to trust others) to develop and test a more comprehensive model of the potential relations between childhood adversity and negative voice-content. It is also possible that negative voice-content may be less “the problem” in of itself than a reflection of more generalized underlying depression, distrust, or social anxiety that fuels or exacerbates distress in many forms. Second, our measure of childhood adversity did not allow us to meaningfully assess whether specific adverse experiences, e.g., sexual abuse, physical abuse, may have differential associations with negative voice-content. This is worthy of further investigation, using tools such as the Childhood Trauma Questionnaire (Bernstein & Fink, 1998). Third, a more nuanced measure of negative voice-content could be employed, which assess specific aspects of negativity such as shaming content, insulting content, and physical threats. A bespoke measure would be needed to assess this. Finally, despite our documentation of a relation between childhood adversity and negative voice-content, clearly not all negative voice-content in people who hear voices will be related to earlier histories of abuse or adversity (which, indeed, is not always present). There is hence the need to better understand the various pathways that can lead to negative voice-content, including more neurologically-based routes such as activation of right Broca’s area (Sommer & Diederen, 2009), and to establish the relative frequency of these potential routes to negative content. Lastly, there were some potential challenges to the external validity of our findings, as clinicodemographics of this sample consisted predominantly of persons with a mean age of 48 years old and identified as African American. It hence remains to be seen if these findings can be generalized to persons experiencing their first episode of psychosis or persons of differing race and cultural experiences.
Conclusion
In conclusion, our study suggests that childhood adversity is a predictor of the level of negative voice-content and voice-distress, and presented findings consistent with the relation between childhood adversity and voice-distress being fully mediated by negative voice-content. There is now the need to attempt replication of this, with future studies also needing to address some of the limitations of our study. A better understanding of both the causes, nature, and consequences of negative voice-content would seem to be an important direction for future study.
Acknowledgments
The authors would like to thank all the individuals who participated in this study for their contributions to the advancement of this scientific knowledge.
Funding: This work was supported in part by PHS grant (NIH) R01MH094358 (R.P.S.) and NARSAD Young Investigator Grant (KAC).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authors Rajiv Sharma and Cherise Rosen designed the study and wrote the protocol. Authors Cherise Rosen and Simon McCarthy-Jones managed the literature searches and analyses. Authors Cherise Rosen and Simon McCarthy-Jones undertook the statistical analysis, and all authors contributed to the first draft and all authors contributed to and have approved the final manuscript. Authors Cherise Rosen and Simon McCarthy-Jones share first authorship and author Cherise Rosen is the corresponding author.
References
- Anda RF, Whitfield CL, Felitti VJ, Chapman D, Edwards VJ, Dube SR, Williamson DF. Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatric services. 2002;53(8):1001–1009. doi: 10.1176/appi.ps.53.8.1001. [DOI] [PubMed] [Google Scholar]
- Bentall RP. The illusion of reality: a review and integration of psychological research on hallucinations. Psychological bulletin. 1990;107(1):82. doi: 10.1037/0033-2909.107.1.82. [DOI] [PubMed] [Google Scholar]
- Bentall RP, Wickham S, Shevlin M, Varese F. Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 the Adult Psychiatric Morbidity Survey. Schizophrenia bulletin. 2012;38(4):734–740. doi: 10.1093/schbul/sbs049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood trauma questionnaire: A retrospective self-report: Manual. Psychological Corporation; 1998. [Google Scholar]
- Brand RM, McEnery C, Rossell S, Bendall S, Thomas N. Do trauma-focussed psychological interventions have an effect on psychotic symptoms? A systematic review and meta-analysis. Schizophrenia research. 2017 doi: 10.1016/j.schres.2017.08.037. S0920-9964(17)30513-3 [pii] [DOI] [PubMed] [Google Scholar]
- Chadwick P, Birchwood M. The omnipotence of voices: A cognitive approach to auditory hallucinations. The British Journal of Psychiatry. 1994;164(2):190–201. doi: 10.1192/bjp.164.2.190. [DOI] [PubMed] [Google Scholar]
- Chadwick P. Person-based cognitive therapy for distressing psychosis. John Wiley & Sons; 2006. [Google Scholar]
- Cole ER, Strauss C, Fife-Schaw C, McCarthy-Jones S. Echoes of others: A path analytic examination of an interpersonal-cognitive model of voice-related distress. Psychology and Psychotherapy: Theory, Research and Practice. 2017;90(4):617–632. doi: 10.1111/papt.12129. [DOI] [PubMed] [Google Scholar]
- Connor C, Birchwood M. Through the looking glass: self-reassuring meta-cognitive capacity and its relationship with the thematic content of voices. Frontiers in human neuroscience. 2013;7:213. doi: 10.3389/fnhum.2013.00213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corstens D, Longden E. The origins of voices: links between life history and voice hearing in a survey of 100 cases. Psychosis. 2013;5(3):270–285. [Google Scholar]
- Craig TK, Rus-Calafell M, Ward T, Leff JP, Huckvale M, Howarth E, Emsley R, Garety PA. AVATAR therapy for auditory verbal hallucinations in people with psychosis: a single-blind, randomised controlled trial. The Lancet Psychiatry. 2018;5(1):31–40. doi: 10.1016/S2215-0366(17)30427-3. S2215-0366(17)30427-3 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daalman K, Boks MP, Diederen KM, de Weijer AD, Blom JD, Kahn RS, Sommer IE. The same or different? A phenomenological comparison of auditory verbal hallucinations in healthy and psychotic individuals. J clin Psychiatry. 2011;72(3):320–325. doi: 10.4088/JCP.09m05797yel. [DOI] [PubMed] [Google Scholar]
- Danivas V, Venkatasubramanian G. Current perspectives on chlorpromazine equivalents: comparing apples and oranges! Indian journal of psychiatry. 2013;55(2):207. doi: 10.4103/0019-5545.111475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodgson G, Gordon S. Avoiding false negatives: are some auditory hallucinations an evolved design flaw? Behavioural and cognitive psychotherapy. 2009;37(3):325–334. doi: 10.1017/S1352465809005244. [DOI] [PubMed] [Google Scholar]
- Fielding-Smith SF, Hayward M, Strauss C, Fowler D, Paulik G, Thomas N. Bringing the “self” into focus: conceptualising the role of self-experience for understanding and working with distressing voices. Frontiers in psychology. 2015;6:1129. doi: 10.3389/fpsyg.2015.01129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-patient Edition Biometrics Research. New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- Gardner DM, Murphy AL, O’Donnell H, Centorrino F, Baldessarini RJ. International consensus study of antipsychotic dosing. FOCUS. 2014;12(2):235–243. doi: 10.1176/appi.ajp.2009.09060802. [DOI] [PubMed] [Google Scholar]
- General Assembly of the World Medical Association. World medical association declaration of helsinki: Ethical principles for medical research involving human subjects. J Am Coll Dent. 2014;81(3):14–18. [PubMed] [Google Scholar]
- Haddock G, McCarron J, Tarrier N, Faragher EB. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS) Psychological medicine. 1999;29(4):879–889. doi: 10.1017/s0033291799008661. [DOI] [PubMed] [Google Scholar]
- Hardy A, Fowler D, Freeman D, Smith B, Steel C, Evans J, Garety P, Kuipers E, Bebbington P, Dunn G. Trauma and hallucinatory experience in psychosis. The Journal of nervous and mental disease. 2005;193(8):501–507. doi: 10.1097/01.nmd.0000172480.56308.21. 00005053-200508000-00001 [pii] [DOI] [PubMed] [Google Scholar]
- Hardy A. Pathways from trauma to psychotic experiences: a theoretically informed model of posttraumatic stress in psychosis. Frontiers in psychology. 2017;8:697. doi: 10.3389/fpsyg.2017.00697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Publications; 2017. [Google Scholar]
- Hayward M, Overton J, Dorey T, Denney J. Relating therapy for people who hear voices: a case series. Clinical Psychology & Psychotherapy. 2009;16(3):216–227. doi: 10.1002/cpp.615. [DOI] [PubMed] [Google Scholar]
- Honig A, Romme MA, Ensink BJ, Escher SD, Pennings MH, Devries MW. Auditory hallucinations: a comparison between patients and nonpatients. The Journal of nervous and mental disease. 1998;186(10):646–651. doi: 10.1097/00005053-199810000-00009. [DOI] [PubMed] [Google Scholar]
- Johns LC, Kompus K, Connell M, Humpston C, Lincoln TM, Longden E, Preti A, Alderson-Day B, Badcock JC, Cella M, Fernyhough C. Auditory verbal hallucinations in persons with and without a need for care. Schizophrenia bulletin. 2014;40(Suppl_4):S255–S264. doi: 10.1093/schbul/sbu005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones SR. Do we need multiple models of auditory verbal hallucinations? Examining the phenomenological fit of cognitive and neurological models. Schizophrenia bulletin. 2008;36(3):566–575. doi: 10.1093/schbul/sbn129. 10.1093/schbul/sbn129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay SR, Opler LA, Lindenmayer JP. The Positive and Negative Syndrome Scale (PANSS): rationale and standardisation. The British Journal of Psychiatry; 1989. [PubMed] [Google Scholar]
- Kennedy A, Ellerby M. A Compassion-Focused Approach to Working With Someone Diagnosed With Schizophrenia. Journal of clinical psychology. 2016;72(2):123–131. doi: 10.1002/jclp.22251. [DOI] [PubMed] [Google Scholar]
- Kråkvik B, Larøi F, Kalhovde AM, Hugdahl K, Kompus K, Salvesen Ø, Stiles TC, Vedul-Kjelsås E. Prevalence of auditory verbal hallucinations in a general population: A group comparison study. Scandinavian journal of psychology. 2015;56(5):508–515. doi: 10.1111/sjop.12236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larøi F. How do auditory verbal hallucinations in patients differ from those in non-patients? Frontiers in human neuroscience. 2012;6:25. doi: 10.3389/fnhum.2012.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leff J, Williams G, Huckvale MA, Arbuthnot M, Leff AP. Computer-assisted therapy for medication-resistant auditory hallucinations: proof-of-concept study. The British Journal of Psychiatry. 2013;202(6):428–433. doi: 10.1192/bjp.bp.112.124883. [DOI] [PubMed] [Google Scholar]
- Leff J, Williams G, Huckvale M, Arbuthnot M, Leff AP. Avatar therapy for persecutory auditory hallucinations: what is it and how does it work? Psychosis. 2014;6(2):166–176. doi: 10.1080/17522439.2013.773457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehoux C, Gobeil MH, Lefèbvre AA, Maziade M, Roy MA. The five-factor structure of the PANSS: a critical review of its consistency across studies. Clinical Schizophrenia & Related Psychoses. 2009;3(2):103–110. [Google Scholar]
- Lindenmayer JP, Bernstein-Hyman R, Grochowski S. Journal of Nervous and Mental Disease. 1994. Five-factor model of schizophrenia: initial validation. [DOI] [PubMed] [Google Scholar]
- Lindert J, von Ehrenstein OS, Grashow R, Gal G, Braehler E, Weisskopf MG. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. International Journal of Public Health. 2014;59(2):359–372. doi: 10.1007/s00038-013-0519-5. [DOI] [PubMed] [Google Scholar]
- Mayhew SL, Gilbert P. Compassionate mind training with people who hear malevolent voices: A case series report. Clinical Psychology & Psychotherapy. 2008;15(2):113–138. doi: 10.1002/cpp.566. [DOI] [PubMed] [Google Scholar]
- McCarthy-Jones S. What have we learnt about the phenomenology of voice-hearing. Psychological Approaches to Understanding and Treating Auditory Hallucinations: From Theory to Therapy. 2014a;1:5–26. [Google Scholar]
- McCarthy-Jones S, Thomas N, Strauss C, Dodgson G, Jones N, Woods A, Brewin CR, Hayward M, Stephane M, Barton J, Kingdon D. Better than mermaids and stray dogs? Subtyping auditory verbal hallucinations and its implications for research and practice. Schizophrenia bulletin. 2014b;40(Suppl_4):S275–S284. doi: 10.1093/schbul/sbu018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy-Jones S. Can’t You Hear Them?: The Science and Significance of Hearing Voices. Jessica Kingsley Publishers; 2017a. [Google Scholar]
- McCarthy-Jones S, Smailes D, Corvin A, Gill M, Morris DW, Dinan TG, Murphy KC, Waddington JL, Donohoe G, Dudley R. Occurrence and cooccurrence of hallucinations by modality in schizophrenia-spectrum disorders. Psychiatry research. 2017b;252:154–160. doi: 10.1016/j.psychres.2017.01.102. S0165-1781(16)31064-2 [pii] [DOI] [PubMed] [Google Scholar]
- Morrison AP, Petersen T. Trauma, metacognition and predisposition to hallucinations in non-patients. Behavioural and Cognitive Psychotherapy. 2003;31(3):235–246. [Google Scholar]
- Nayani TH, David A. The neuropsychology and neurophenomenology of auditory hallucinations. Schizophrenia: A neuropsychological perspective; 1996. [Google Scholar]
- Offen L, Thomas G, Waller G. Dissociation as a mediator of the relationship between recalled parenting and the clinical correlates of auditory hallucinations. British Journal of Clinical Psychology. 2003;42(3):231–241. doi: 10.1348/01446650360703357. [DOI] [PubMed] [Google Scholar]
- Peters ER, Williams SL, Cooke MA, Kuipers E. It’s not what you hear, it’s the way you think about it: appraisals as determinants of affect and behaviour in voice hearers. Psychological Medicine. 2012;42(7):1507–1514. doi: 10.1017/S0033291711002650. [DOI] [PubMed] [Google Scholar]
- Raune D, Bebbington P, Dunn G, Kuipers E. Event attributes and the content of psychotic experiences in first-episode psychosis. Psychological Medicine. 2006;36(2):221–230. doi: 10.1017/S003329170500615X. S003329170500615X [pii] [DOI] [PubMed] [Google Scholar]
- Read J, Argyle N. Hallucinations, delusions, and thought disorder among adult psychiatric inpatients with a history of child abuse. Psychiatric Services. 1999;50(11):1467–1472. doi: 10.1176/ps.50.11.1467. [DOI] [PubMed] [Google Scholar]
- Read J, Agar K, Argyle N, Aderhold V. Sexual and physical abuse during childhood and adulthood as predictors of hallucinations, delusions and thought disorder. Psychology and Psychotherapy: Theory, research and practice. 2003;76(1):122. doi: 10.1348/14760830260569210. [DOI] [PubMed] [Google Scholar]
- Reiff M, Castille DM, Muenzenmaier K, Link B. Childhood abuse and the content of adult psychotic symptoms. Psychological Trauma: Theory, Research, Practice, and Policy. 2012;4(4):356. [Google Scholar]
- Reavis JA, Looman J, Franco KA, Rojas B. Adverse childhood experiences and adult criminality: how long must we live before we possess our own lives? The Permanente Journal. 2013;17(2):44. doi: 10.7812/TPP/12-072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romme M, Escher S. Accepting voices. London: MIND publications; 1993. [Google Scholar]
- Rosen C, Jones N, Longden E, Chase KA, Shattell M, Melbourne JK, Keedy SK, Sharma RP. exploring the intersections of Trauma, structural adversity, and Psychosis among a Primarily african-american sample: a Mixed-Methods analysis. Frontiers in psychiatry. 2017;8:57. doi: 10.3389/fpsyt.2017.00057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shevlin M, Dorahy MJ, Adamson G. Trauma and psychosis: an analysis of the National Comorbidity Survey. American Journal of Psychiatry. 2007;164(1):166–169. doi: 10.1176/ajp.2007.164.1.166. 164/1/166 [pii] [DOI] [PubMed] [Google Scholar]
- Sommer IE, Diederen KM. Language production in the non-dominant hemisphere as a potential source of auditory verbal hallucinations. Brain. 2009;132(10):e124–e124. [Google Scholar]
- Thomas P, Mathur P, Gottesman II, Nagpal R, Nimgaonkar VL, Deshpande SN. Correlates of hallucinations in schizophrenia: a cross-cultural evaluation. Schizophrenia research. 2007;92(1):41–49. doi: 10.1016/j.schres.2007.01.017. S0920-9964(07)00077-1 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson BL, Waltz J. Mindfulness and experiential avoidance as predictors of posttraumatic stress disorder avoidance symptom severity. Journal of anxiety disorders. 2010;24(4):409–415. doi: 10.1016/j.janxdis.2010.02.005. [DOI] [PubMed] [Google Scholar]
- van der Gaag M, Van Oosterhout B, Daalman K, Sommer IE, Korrelboom K. Initial evaluation of the effects of competitive memory training (COMET) on depression in schizophrenia-spectrum patients with persistent auditory verbal hallucinations: A randomized controlled trial. British Journal of Clinical Psychology. 2012;51(2):158–171. doi: 10.1111/j.2044-8260.2011.02025.x. [DOI] [PubMed] [Google Scholar]