Abstract
Blastomycosis is a fungal infection caused by Blastomyces species. This infection is endemic to North America particularly states bordering the Mississippi, Ohio and St Lawrence Rivers, and the Great Lakes but also occurs worldwide. While the most common site of infection is the lung, it can also manifest in the bones, skin and central nervous system. Blastomycosis is a great masquerader and it can present in a manner difficult to distinguish from bacterial pneumonia, tuberculosis (TB), histoplasmosis or carcinoma. Here, we describe a 36-year-old male with disseminated blactomycosis infection who presented with right arm weakness. Initial diagnostic evaluation was cofounded by a previous concern for TB; however, broncho-alveolar lavage confirmed Blastomyces spp. Pulmonary and brain lesions markedly improved after Amphotericin and Itraconazole.
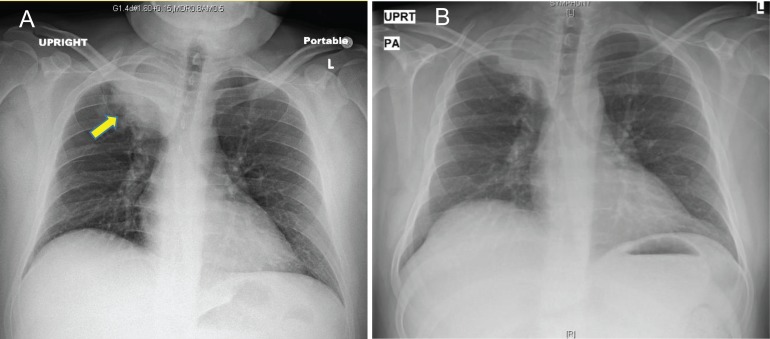
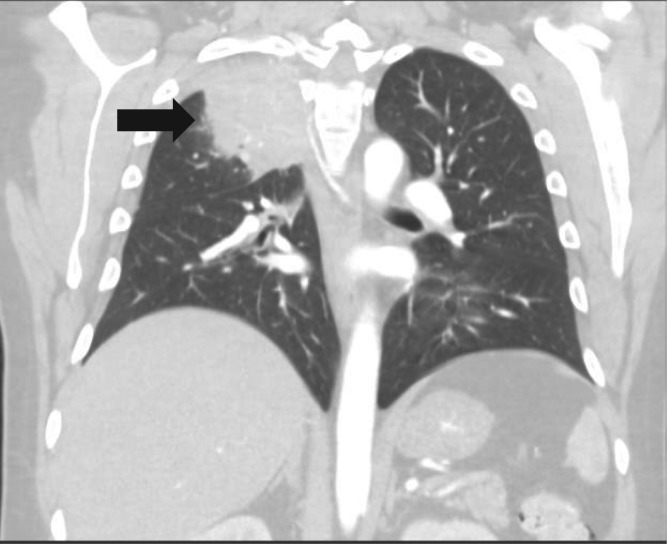
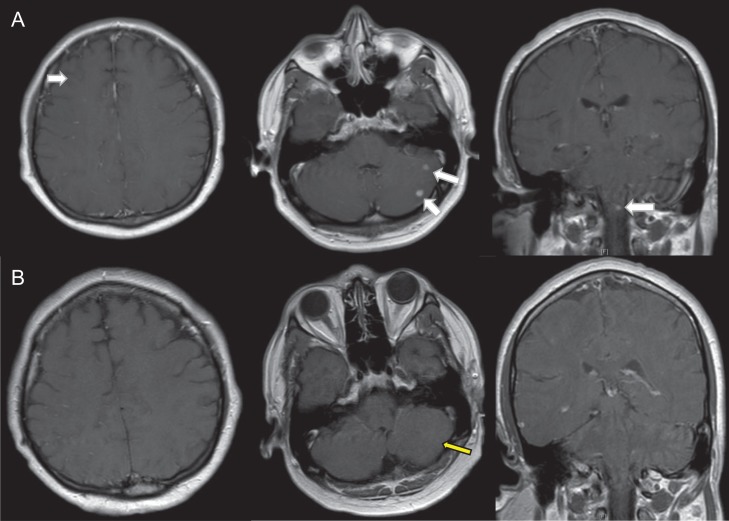
A 36-year-old healthy Hispanic patient presents with 5-day history of right arm weakness and tingling. He also reported persistent cough with blood-streaked sputum, fever and unintentional 8-lbs weight loss for the past 8 weeks. As pertinent medical history, 2 months before this visit, he was diagnosed with pulmonary tuberculosis (TB) after he presented to an outside hospital for hemoptysis and night sweats. He denied any previous TB exposure, no recent travel, sick contacts or direct exposure to soil. He worked as a building supervisor. At that time, he refused broncho-alveolar lavage (BAL) and decision was made to treat him as an active TB with rifampin, isoniazid, pyrazinamide and ethambutol (RIPE) therapy. On admission, his vital signs were stable, physical exam remarkable for decrease breath sounds at the right apex, his cranial nerves were intact and there were no sensory or motor deficits. Laboratory workup including HIV test was negative. Chest X-ray revealed a dense consolidation in the right upper lung (Fig. 1); moreover, computed tomography (CT) of the chest confirmed a 9.2 cm focal consolidation in the right upper lobe and right apex (Fig. 2). Magnetic resonance imaging (MRI) of the brain (Fig. 3) was consistent with small enhancing lesions in the right frontal cortex, left cerebellar hemisphere and upper cervical cord-lower brainstem; sputum sent for stain and culture was negative for bacteria, fungal and mycobacterium, further BAL yielded Blastomyces spp. We discontinued his treatment for TB and started the patient on IV liposomal Amphotericin B for 6 weeks followed by oral Itraconazole for 12 months. After 2 months, the patient was asymptomatic and follow-up MRI and X-rays showed nearly complete resolution of previous lesions (Figs 1 and 3). He continues to be free of symptoms after almost 1 year.
Figure 1:
(A) Initial antero-posterior chest X-ray showing dense consolidation present in the right upper lung (yellow arrow). (B) Postero-anterior chest X-ray shows moderate resolution of the consolidation 1 month after treatment with IV Amphotericin B.
Figure 2:
Initial coronal computed tomography section of the chest showing a 9.2 cm focal consolidation in the involving the right upper lobe (black arrow).
Figure 3:
(A) Small homogeneously enhancing lesions in the right frontal cortex, left cerebellar hemisphere and upper cervical cord-lower brainstem (white arrows). (B) After 8 weeks of IV Amphotericin B, there is marked improvement with near complete resolution of the intracranial enhancing lesions. Single, submillimeter enhancing focus in the left cerebellar hemisphere in the region of previously noted 7 mm enhancing lesion (yellow arrow). No enhancement in the rest of the previously described bilateral cerebellar and frontal lobe lesion and brainstem lesions.
CONCLUSION
Blastomycosis is not a common infection. In North America, the annual incidence of blastomycosis ranges from 0.2 to 1.94 cases per 100 000 persons [1]. Blastomyces dermatitidis and Blastomyces gilchristii are recognized as etiologic agents of blastomycosis, currently only PCR followed by sequence analysis is the only method of differentiating these species [2]. This infection can disseminate to any organ in the body. When it compromises both lungs and central nervous system (CNS), it can mimic other entities such as nocardiosis, cryptococcosis and tuberculosis [3]. In order to make a definitive diagnosis, Blastomyces spp. must be isolated in culture, or observed in a smear or histologic specimen. Specimens obtained for culture by bronchoscopy yield a positive diagnosis in 92% of patients [1]. Treatment of choice for CNS blastomycosis is liposomal amphotericin 5 mg/kg/day for 4–6 weeks followed by oral triazole (voriconazole, fluconazole or itraconazole) for at least 6–12 months [1]. It is not clear which azole is optimal for step-down therapy. However, limited data favor voriconazole in light of good CNS penetration [4]. Nonetheless, clinical trials have not been performed comparing oral azole regimes for step-down therapy of CNS blastomycosis.
Blastomycosis should be considered in the differential diagnosis of patients with neurological and respiratory symptoms in endemic areas in order to avoid errors in treatment or progression of untreated infection.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
INFORMED CONSENT
Informed consent was obtained from the patient for publication of this study.
REFERENCES
- 1. McBride JA, Gauthier GM, Klein BS. Clinical manifestations and treatment of blastomycosis. Clin Chest Med 2017;38:435–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dalcin D, Rothstein A, Spinato J, Escott N, Kus JV. Fungal infections of the nervous system: current perspective and controversies in management. Emerg Infect Dis 2016;22:306–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sharma R. Fungal infections of the nervous system: current perspective and controversies in management. Int J Surg 2010;8:591–601. [DOI] [PubMed] [Google Scholar]
- 4. Bariola JR, Perry P, Pappas PG, Proia L, Shealey W, Wright PW, et al. . Blastomycosis of the central nervous system: a multicenter review of diagnosis and treatment in the modern era. Clin Infect Dis 2010;50:797–804. [DOI] [PubMed] [Google Scholar]