Abstract
Introduction:
The aims of this study were to evaluate, using 3-dimensional superimposition techniques, the skeletal changes in Class II subjects with different vertical facial patterns treated with the Herbst appliance and to compare these skeletal changes to those of Class II controls treated with elastics.
Methods:
Sixteen Herbst patients who met the inclusion criteria were divided into 2 equal groups based on vertical facial pattern as determined by the Frankfort mandibular plane angle (brachyfacial, ≤22°; mesofacial, 23°−29°) and had cone-beam computed tomographs taken before treatment, 8 weeks after Herbst appliance removal, and after subsequent fixed appliance treatment. Eleven Class II control patients treated with fixed appliances and elastics had cone-beam computed tomographs taken before and after treatment. Three-dimensional models were generated from the cone-beam computed tomography images, registered on the anterior cranial bases, and analyzed using color maps and point-to-point measurements.
Results:
There were minimal differences in treatment response between the 2 Herbst groups across all skeletal parameters measured. The Herbst subjects showed a greater inferior displacement of anterior nasal spine compared with the Class II controls (Herbst brachyfacial, −1.44 mm; Herbst mesofacial,−1.95 mm) with other maxillary changes being clinically insignifi-cant. The Herbst subjects showed greater inferior displacement of B-point compared with the Class II controls (Herbst brachyfacial, −2.59 mm; Herbst mesofacial, −2.75 mm). There were no statistically significant differences in mean linear mandibular measurements. All groups showed a trend toward posterior displacement of the condyles and glenoid fossae from the start to the end of treatment, with no significant differences across the 3 groups. There were minimal differences in the changes in gonial angle and Frankfort mandibular plane angle across all groups.
Conclusion:
Approximately 2 years after Herbst treatment, the Herbst subjects with different vertical facial patterns showed similar patterns of skeletal change compared with the Class II controls treated with elastics. (Am J Orthod Dentofacial Orthop 2018;154:238–48)
Management of Class II malocclusion in a growing person is a routine clinical challenge to orthodontists.1 Mandibular retrognathism is the predominant etiologic factor in the majority of these malocclusions.2,3
Functional appliances have been used to correct Class II malocclusions through a combination of skeletal and dental changes,4 and the Herbst appliance is one of the most popular fixed functional appliances because it reduces the level of compliance required.5 However, despite the widespread use of the Herbst appliance, the exact mechanism of action, and its skeletal and dental effects, are unclear. There are claims of restriction of maxillary growth, forward positioning of the glenoid fossa, mandibular gonial angle changes, and stimulation of condylar growth,6 with variations of the skeletal component of Class II correction ranging from 13% to 85%.7,8
There should be some certainty for any widely used appliance about the effects on the dentition and skeleton. The inconsistencies in reported treatment outcomes with the Herbst appliance may be because of differences in timing of treatment relative to peak growth, anatomic differences of the study subjects,9,10 and use of 2-dimensional cephalometric imaging that is subject to various errors, including the superimposition process, magnification differences, geometric distortion, patient positioning, and obstruction of anatomic structures.11–13 There can be bias in the superimposition process if the examiners are not blinded. Two-dimensional angular and linear cephalometric measurements do not adequately describe the complex 3-dimensional (3D) process of bone remodeling and skeletal change with growth and treatment.10 Now that 3D imaging is widely accessible and able to give a more detailed and accurate picture of the skeleton and dentition, it is incumbent on the orthodontic specialty to use the available tools to determine the real effects of treatment. There has been only 1 published pilot study examining 3D outcomes with the Herbst appliance,10 and few studies have examined the effects of the first phase of Herbst therapy followed by a further phase of fixed orthodontic appliances.14 A more detailed study with a larger sample is necessary to enable the specialty to learn more about the effects of the appliance in 3 dimensions. Our group gained access to 3D data of a number of Herbst patients, as well as similar data from patients treated with Class II elastics who could be used as matched controls.
Therefore, the aims of this study were to use 3D imaging and superimposition techniques to assess skeletal changes associated with Class II correction in growing children with different vertical facial patterns treated with the Herbst appliance followed by a subsequent phase of fixed appliances. The changes were compared with a matched group of Class II control patients. Maxillary positional changes, differences in mandibular growth, and condylar and glenoid fossa positional changes were evaluated.
MATERIAL AND METHODS
Ethics approval for this retrospective study was obtained from the University of Melbourne Human Research Ethics Committee (ID: 1443363). All Herbst subjects were sourced from the office of a specialist orthodontist. The subjects were selected by searching the database for an item code denoting Herbst appliance insertion.
This retrospective cohort study used a convenience sample. The Herbst sample consisted of 16 patients and was divided on the basis of vertical facial pattern, as determined by the Frankfort mandibular plane angle (FMPA). The sample included 8 mesofacial (FMPA, 23°−29°) subjects (7 girls, 1 boy). The brachyfacial group (FMPA, <22°) also consisted of 8 subjects (4 girls, 4 boys). The sample size was limited by the number of available suitable records.
A control group of 11 deidentified, matched Class II control subjects (Table I) treated with Class II elastics was obtained from the University of North Carolina at Chapel Hill and the University of Michigan at Ann Arbor.
Table I.
Demographics and statistical comparisons of Herbst and Class II control subjects
| Measurement | Herbst brachyfacial mean | SD | Herbst mesofacial mean | SD | Control mean | SD | P value |
|---|---|---|---|---|---|---|---|
| Age (y) | 13.36 | 0.58 | 12.74 | 0.85 | 13.73 | 0.82 | 0.03* |
| Sex | 4 female, 4 male | - | 7 female, 1 male | 6 female, 5 male | - | - | |
| Phase 1 duration (mo) | 7.21 | 1.41 | 7.93 | 2.23 | - | - | 0.46 |
| Phase 2 duration (mo) | 20.38 | 3.92 | 19.25 | 4.40 | - | - | 0.60 |
| Total treatment time (mo) | 27.59 | 4.31 | 27.18 | 5.78 | 22.81 | 8.69 | 0.25 |
| ANB (°) | 6.0 | 0.9 | 5.4 | 1.4 | 3.9 | 2.2 | 0.03† |
| Pog-N perp (mm) | −2.4 | 4.4 | −3.8 | 6.1 | −3.8 | 3.6 | 0.83 |
| Gonial angle (Co-Go-Me) (°) | 118.1 | 3.9 | 127.1 | 5.6 | 122.8 | 4.9 | 0.003‡ |
| FMPA (°) | 18.3 | 4.1 | 27.9 | 1.4 | 24.5 | 5.0 | 0.0002‡ |
| Class II molar relationship (mm) | 6.6 | 1.5 | 6.3 | 1.5 | 4.6 | 1.4 | 0.01§ |
Significant difference at P<0.05 for Herbst mesofacial vs control group only;
Significant difference at P<0.05 for Herbst brachyfacial vs control group only;
Significant difference at P<0.05 for Herbst brachyfacial group vs Herbst mesofacial and control group;
Significant difference at P<0.05 for Herbst brachyfacial group and Herbst mesofacial vs control group.
The Herbst appliance design consisted of stainless steel crowns fitted to the maxillary and mandibular permanent first molars. A cantilevered arm extended forward from the mandibular first molar to the level of the mandibular first premolar. A well-adapted 0.040-in stainless steel lingual arch connected the left and right mandibular molars, also incorporating an occlusal rest on the mandibular first premolar or second primary molar. A hyrax expansion screw was incorporated in all cases to expand the maxillary arch to accommodate the advanced position of the mandibular arch. The mandible was initially advanced by 5 mm and then progressively advanced in 2-mm increments to bring the incisors into an overcorrected edge-to-edge position. The mean Herbst treatment time in both groups was 7.6 months, which matched the Herbst protocols of other authors.15,16 When the incisor relationship did not allow the required advancement, as in Class II Division 2 subjects, limited maxillary fixed appliances were placed to procline the maxillary incisors before placement of the Herbst appliance.
No patient was treated with extractions, and extraoral traction was not used in the control sample.
A power calculation was undertaken using the SPSS statistical software package (version 22.0; IBM, Armonk, NY). This showed that 8 subjects in each group would provide 80% statistical power in detecting a 2-mm difference for mandibular length between the control and treatment groups, assuming a standard deviation of 1.99 mm and significance of P <0.05.10 This 2-mm difference was considered the threshold for clinical relevance. A pilot study found a 0.71 mm difference between comparable treatment and control groups; however, this difference was not clinically relevant.
Cone-beam computed tomography (CBCT) scans were taken before treatment (T1) for both the Herbst and the Class II control patients, and 8 weeks after completion of the Herbst phase (T2). The Herbst patients all had a subsequent period of fixed appliance treatment. A final CBCT scan was taken once the fixed appliances were removed (T3) for both the Herbst and control subjects. The Herbst and Class II control subjects’ scans were taken using an i-Cat machine (Imaging Sciences International, Hatfield, Pa) with a 16 × 22-cm field of view. All patients were instructed to bite in maximum intercuspation during the scan. Scans at all time points were evaluated to ensure that the condyles were seated in the center of the fossa, and subjects were excluded if the condyles were postured.
The original scans were taken at 0.3 to 0.4 mm3 voxel size, and then the DICOM files were deidentified and downsized to a 0.5-mm3 voxel size using 3D Slicer (www.slicer.org) to decrease the computational power and time for cranial base registration. A study evaluating CBCT accuracy showed no statistically significant difference in error measurements when the voxel size of the scan was changed from 0.2 to 0.3 to 0.4 mm3.17 ITK-SNAP (www.itksnap.org) was used to construct virtual 3D surface models.17 Scans at T1, T2, and T3 were registered on the anterior cranial base using a fully automated voxel-wise ridged registration technique.18–20
The limits of the anterior cranial base registration were defined anteriorly by the inner cortical layer of the frontal bone, posteriorly by the anterior wall of sella, laterally including the lesser wings of the sphenoid bone, and superiorly including the frontal bone. This area included the cribriform plate and the superior aspect of the ethmoid bone. These structures cease growth by the age of 7 years and are therefore considered stable landmarks.21,22 Standardized head orientation of the registered 3D models was used to obtain a common coordinate system, allowing proper assessment of anteroposterior and vertical changes. This method has been shown to be accurate and reproducible.23
Qualitative and quantitative assessments of treatment response and growth were calculated using 3D color maps and semitransparencies and point-to-point landmark identification.
Landmarks selected for this study are shown in the Supplementary Figure. Additional landmarks included the geometric center of the condyle, a point in the head of the condyle created by plotting the midpoint of a line joining the medial and lateral poles. Cephalo-metric landmark placement on 3D structures has been shown to be reproducible and accurate.24,25
The point-to-point measurements are reported as either a 3D distance or a distance split into lateral (x), anteroposterior (y), and vertical (z) coordinates. In contrast to a previous pilot study by LeCornu et al,10 we chose to decompose some of the 3D landmark point-to-point changes into the 3 axes, because the clinical questions of this study required more precise information regarding the location and amount of changes in each direction. For the y-axis, positive values indicated anterior displacement, and negative values indicated posterior displacement. For the z-axis, positive values indicated superior displacement, and negative values indicated inferior displacement. The lateral (x) axis measurements are not reported due to the lack of clinical significance in this study.
The 2 Herbst groups differing in vertical facial pattern were compared 8 weeks after the appliance was removed (T1-T2) and after the next phase of fixed appliances (T2-T3). After fixed appliance therapy, the 2 Herbst groups were also compared with the Class II control group treated in a single phase with Class II elastics (T1-T3).
Qualitative assessments of maxillary, mandibular, and glenoid fossa skeletal changes at T1-T2, T2-T3, and T1-T3 were performed using color maps and semi-transparent overlays of the superimpositions.
Subjects were restricted to adolescents treated near the peak of pubertal growth, as determined by cervical vertebral maturation assessment (stages 3 and 4).26 All subjects had Class II skeletal (ANB, >4°) and dental relationships (bilateral Class II molar relationships, each side >4 mm).
Subjects were excluded if they had early orthodontic treatment, craniofacial syndromes, or incomplete pre-treatment and posttreatment records.
Statistical analysis
Parametric testing was used since the data were normally distributed. Data analysis was undertaken using the Minitab statistical software package (version 17; Minitab, State College, Pa). Means, standard deviations, and ranges were calculated for all subjects. Statistical differences were assessed using 1-way analysis of variance. The Fisher exact test was used to assess differences in skeletal changes between the Herbst and Class II control subjects. Repeated measurements of 10 subjects were made 8 weeks after the initial measurements by an examiner (A.A.), and Bland-Altman plots of the 95% limits of agreement were used to evaluate the reliability of the repeated measures (Table II).27
Table II.
Error of 3D landmark location and measurement: Bland-Altman means, standard deviations, and 95% limits of agreement for y and z coordinates and 3D distances
| Variable | Mean | SD | P | Limits of agreement | |
|---|---|---|---|---|---|
| Low | High | ||||
| A-point anteroposterior axis (mm) | 0.00 | 0.12 | 0.98 | −0.24 | 0.24 |
| A-point superoinferior axis (mm) | −0.01 | 0.29 | 0.92 | −0.58 | 0.56 |
| ANS anteroposteror axis (mm) | 0.07 | 0.30 | 0.48 | −0.52 | 0.66 |
| ANS superoinferior axis (mm) | 0.11 | 0.66 | 0.62 | −1.18 | 1.39 |
| ANS-PNS (°) | 0.57 | 0.69 | 0.03 | −0.78 | 1.91 |
| Pogonion anteroposterior axis (mm) | 0.00 | 0.13 | 0.96 | −0.26 | 0.26 |
| Pogonion superoinferior axis (mm) | −0.22 | 1.12 | 0.55 | −2.41 | 1.97 |
| B-point anteroposterior axis (mm) | 0.04 | 0.14 | 0.43 | −0.24 | 0.31 |
| B-point superoinferior axis (mm) | −0.16 | 1.07 | 0.64 | −2.23 | 1.94 |
| Right mandibular length (mm) | 0.62 | 0.82 | 0.04 | −0.99 | 2.22 |
| Left mandibular length (mm) | −0.17 | 0.78 | 0.50 | −1.70 | 1.35 |
| Right ramus height (mm) | 0.03 | 0.81 | 0.91 | −1.55 | 1.62 |
| Left ramus height (mm) | −0.89 | 0.88 | 0.01 | −2.62 | 0.84 |
| Right corpus length (mm) | −0.43 | 1.48 | 0.39 | −3.32 | 2.47 |
| Left corpus length (mm) | −0.15 | 0.87 | 0.60 | −1.85 | 1.56 |
| Right gonial angle (o) | −0.01 | 2.27 | 0.99 | −4.46 | 4.43 |
| Left gonial angle (o) | −0.50 | 0.93 | 0.13 | −2.33 | 1.33 |
| Right FMPA (o) | 0.52 | 0.73 | 0.05 | −0.92 | 1.96 |
| Left FMPA (o) | 0.61 | 0.58 | 0.01 | −0.53 | 1.75 |
| Right condylion anteroposterior axis (mm) | −0.23 | 0.81 | 0.39 | −1.82 | 1.36 |
| Right condylion superoinferior axis (mm) | −0.08 | 0.28 | 0.41 | −0.63 | 0.47 |
| Left condylion anteroposterior axis (mm) | −0.77 | 0.91 | 0.03 | −2.56 | 1.02 |
| Left condylion superoinferior axis (mm) | 0.02 | 0.45 | 0.91 | −0.86 | 0.89 |
| Geometric center of right condyle anteroposterior axis (mm) | −0.14 | 0.34 | 0.24 | −0.81 | 0.54 |
| Geometric center of right condyle superoinferior axis (mm) | −0.04 | 0.66 | 0.86 | −1.32 | 1.25 |
| Geometric center of left condyle anteroposterior axis (mm) | −0.02 | 0.44 | 0.89 | −0.87 | 0.84 |
| Geometric center of left condyle superoinferior axis (mm) | 0.05 | 0.95 | 0.88 | −1.81 | 1.90 |
| Right anterior fossa anteroposterior axis (mm) | 0.14 | 0.32 | 0.21 | −0.49 | 0.77 |
| Right anterior fossa superoinferior axis (mm) | −0.15 | 0.28 | 0.13 | −0.69 | 0.40 |
| Left anterior fossa anteroposterior axis (mm) | 0.19 | 0.35 | 0.11 | −0.49 | 0.88 |
| Left anterior fossa superoinferior axis (mm) | −0.33 | 0.46 | 0.05 | −1.23 | 0.58 |
| Right posterior fossa anteroposterior axis (mm) | −0.01 | 0.35 | 0.90 | −0.70 | 0.67 |
| Right posterior fossa superoinferior axis (mm) | −0.10 | 0.64 | 0.65 | −1.35 | 1.16 |
| Left posterior fossa anteroposterior axis (mm) | 0.02 | 0.16 | 0.71 | −0.29 | 0.33 |
| Left posterior fossa superoinferior axis (mm) | 0.00 | 0.24 | 0.99 | −0.48 | 0.48 |
RESULTS
The descriptive statistics comparing both Herbst groups (brachyfacial and mesofacial) and the Class II control group are summarized in Table I.
The Herbst groups were well matched with regard to age (brachyfacial, 13.36 years; mesofacial, 12.74 years), duration of Herbst treatment (brachyfacial, 7.21 months; mesofacial, 7.93 months), and duration of fixed appliance therapy that followed (brachyfacial, 20.38 months; mesofacial, 19.25 months). There were significant differences (P = 0.0002) in the FMPA (brachyfacial, 18.3°; mesofacial, 27.9°) and the gonial angle (P = 0.003) between the 2 Herbst groups (brachyfacial, 118.1°; meso-facial, 127.1°).
The Herbst groups and the Class II control group were well matched in regard to total treatment time (Herbst brachyfacial, 27.59 months; Herbst mesofacial, 27.18 months; control, 22.81 months) and Pog-N perpendicular (Herbst brachyfacial, −2.4 mm; Herbst mesofacial, −3.8 mm; control, −3.8 mm). There was a significant difference (P = 0.03) in age between the Herbst mesofacial group and the Class II control group (Herbst mesofacial, 12.74 years; control, 13.73 years). There were also statistically significant differences in the severity of the Class II malocclusion as shown by the average molar occlusion (P = 0.01) between the groups (Herbst brachyfacial, 6.6 mm; Herbst mesofacial, 6.3 mm; control, 4.6 mm) and the ANB angle (P = 0.03) between the Herbst brachyfacial and Class II control group (Herbst brachyfacial, 6.0°; control 3.9°).
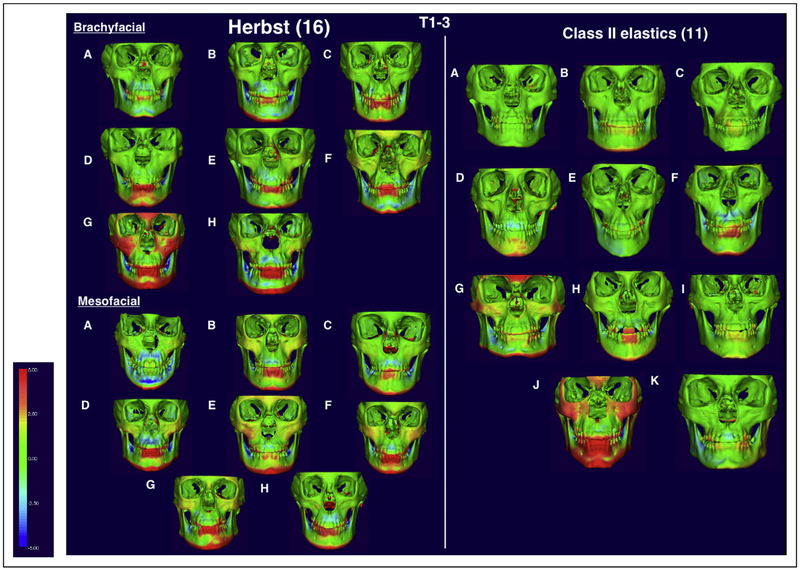
Qualitative evaluations of the maxillary and mandibular skeletal changes at all times were undertaken using semitransparent overlays and color maps of the cranial base superimpositions (Figs 1 and 2).
Fig 1.
Color maps showing skeletal displacements calculated from the 3D volume renderings for both Herbst groups and the Class II controls at T1 to T3 when registered and superimposed at the anterior cranial base. The color map scale is set from −5 to +5 mm. Red represents regions of anterior displacement of T3 in relation to T1; blue represents regions of posterior displacement.
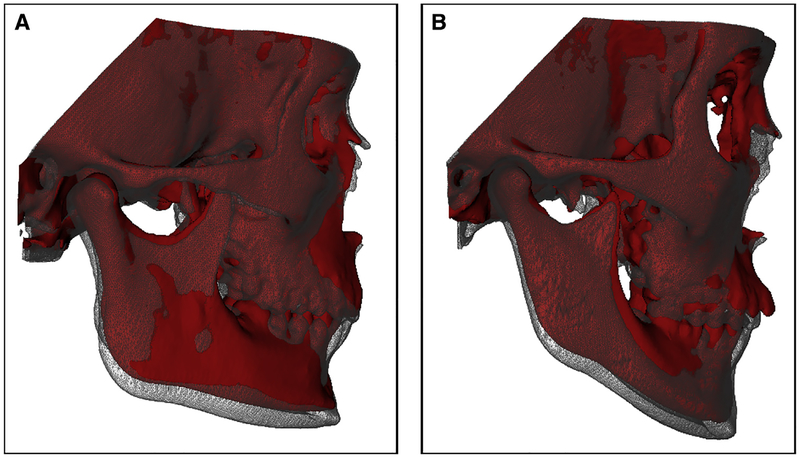
Fig 2.
Semitransparencies of superimposed 3D renderings registered at the anterior cranial base: A, Herbst brachyfacial and B, Herbst mesofacial subjects from T1 (red) to T3 (white).
Quantitative assessments of maxillary changes at the initial (T1) and final (T3) timepoints are reported in Table III. There were no significant differences in the vertical and anteroposterior positions of A-point or ANS between the 2 Herbst groups according to the y- and z-coordinates. There was a significant difference (P = 0.01) in the change in vertical position of ANS in the Herbst brachyfacial (−1.44 mm) and Herbst mesofacial (P = 0.001) (−1.95 mm) groups compared with the Class II control group from T1 to T3. There were no significant differences in palatal plane angulation (ANS-PNS) across all 3 groups from T1 to T3.
Table III.
Differences between the T1 and T3 skeletal changes for the Herbst brachyfacial group, Herbst mesofacial group and Class II elastics controls
| Measurement | Herbst brachyfacial (HB) mean | SD | Herbst mesofacial (HM) mean | SD | Control (C) mean | SD | Difference of means (HM vs HB) (95% CI) | P value | Difference of means (C vs HB) (95% CI) | P value | Difference of means (C vs HM) (95% CI) | P value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Maxillary skeletal | ||||||||||||
| A point AP (mm) | 0.43 | 0.69 | 0.02 | 1.06 | 0.59 | 1.21 | −0.41 (−1.48, 0.66) | 0.43 | 0.16 (−0.83, 1.16) | 0.74 | 0.57 (−0.42, 1.57) | 0.24 |
| A point SI (mm) | −2.03 | 1.77 | −1.85 | 2.07 | −0.98 | 2.08 | 0.18 (−1.88, 2.23) | 0.98 | 1.04 (−1.27, 3.36) | 0.51 | 0.87 (−1.44, 3.18) | 0.62 |
| ANS AP (mm) | 0.61 | 1.45 | 0.88 | 0.97 | 0.65 | 1.61 | 0.27 (−1.18, 1.71) | 0.71 | 0.03 (−1.31, 1.37) | 0.96 | −0.23 (−1.58, 1.1 1) | 0.72 |
| ANS SI (mm) | −2.28 | 1.05 | −2.80 | 0.43 | −0.85 | 1.49 | −0.52 (−1.69, 0.66) | 0.38 | 1.44 (0.34, 2.53) | 0.01* | 1.95 (0.85, 3.04) | 0.001* |
| Palatal plane (ANS-PNS) (°) | −1.18 | 0.94 | −0.85 | 1.96 | −0.59 | 1.62 | 0.33 (−1.30, 1.95) | 0.68 | 0.59 (−0.93, 2.09) | 0.43 | 0.26 (−1.25, 1.77) | 0.72 |
| Mandibular skeletal | ||||||||||||
| Pogonion AP (mm) | 1.25 | 1.81 | 1.35 | 2.73 | 0.73 | 1.12 | 0.10 (−2.29, 2.49) | 0.99 | −0.52 (−2.74, 1.70) | 0.83 | −0.62 (−2.84, 1.60) | 0.77 |
| Pogonion SI (mm) | −4.88 | 2.70 | −5.09 | 2.63 | −3.72 | 2.86 | −0.22 (−3.65, 3.21) | 0.99 | 1.16 (−2.03, 4.35) | 0.64 | 1.37 (−1.82, 4.56) | 0.54 |
| B Point AP (mm) | 0.70 | 1.28 | 1.01 | 2.23 | 0.56 | 1.17 | 0.31 (−1.32, 1.94) | 0.70 | −0.14 (−1.66, 1.37) | 0.84 | −0.45 (−1.97, 1.06) | 0.54 |
| B point SI (mm) | −5.82 | 2.68 | −5.98 | 2.02 | −3.23 | 2.47 | −0.16 (−2.65, 2.33) | 0.89 | 2.59 (0.28, 4.91) | 0.03* | 2.75 (0.44, 5.07) | 0.02* |
| Right mandibular length (Co-Gn) (mm) | 5.65 | 2.81 | 5.68 | 2.57 | 3.35 | 2.36 | 0.03 (−2.61, 2.67) | 0.98 | −2.30 (−4.75, 0.16) | 0.07 | −2.32 (−4.78, −0.13) | 0.06 |
| Left mandibular length (Co-Gn) (mm) | 4.93 | 2.26 | 5.14 | 1.33 | 3.24 | 2.54 | 0.21 (−2.03, 2.44) | 0.85 | −1.70 (−3.77, 0.38) | 0.10 | −1.90 (−3.98, 0.17) | 0.07 |
| Right ramus height (Co-Go’) (mm) | 4.19 | 2.14 | 3.44 | 1.66 | 2.87 | 2.46 | −0.75 (−2.98, 1.48) | 0.49 | −1.31 (−3.38, 0.76) | 0.20 | −0.56 (−2.63, 1.51) | 0.58 |
| Left ramus height (Co-Go’) (mm) | 3.75 | 1.71 | 3.81 | 1.56 | 3.07 | 2.60 | 0.05 (−2.11, 2.21) | 0.96 | −0.69 (−2.70, 1.32) | 0.49 | −0.74 (−2.75, 1.27) | 0.45 |
| Right corpus length (Go-Gn) (mm) | 3.18 | 1.77 | 3.74 | 1.54 | 2.28 | 2.56 | 0.56 (−1.60, 2.70) | 0.60 | −0.90 (−2.90, 1.10) | 0.36 | −1.45 (−3.45, 0.54) | 0.15 |
| Left corpus length (Go-Gn) (mm) | 3.15 | 1.61 | 3.26 | 1.39 | 1.86 | 1.70 | 0.1 1 (−1.53, 1.75) | 0.89 | −1.29 (−2.82, 0.23) | 0.09 | −1.40 (−2.93, 0.12) | 0.07 |
| Right gonial angle (Co-Go-Me) (_) | −0.78 | 1.41 | 0.46 | 1.28 | −1.13 | 1.52 | 1.24 (−0.23, 2.70) | 0.10 | −0.35 (_1.72, 1.00) | 0.60 | −1.59 (−2.95, −0.22) | 0.02* |
| Left gonial angle (Co-Go-Me) (°) | −0.42 | 0.77 | −0.05 | 1.65 | −0.40 | 0.92 | 0.37 (−0.81, 1.56) | 0.52 | 0.02 (−1.08, 1.12) | 0.97 | −0.35 (−1.45, 0.75) | 0.52 |
| Right FMPA (°) | 0.16 | 1.82 | −0.38 | 2.48 | −0.35 | 1.51 | −0.54 (−2.53, 1.45) | 0.58 | −0.52 (−2.36, 1.33) | 0.57 | 0.02 (−1.83, 1.87) | 0.98 |
| Left FMPA (°) | 0.50 | 1.41 | 0.17 | 1.60 | 0.26 | 1.07 | −0.33 (−1.72, 1.06) | 0.63 | −0.24 (−1.53, 1.05) | 0.70 | 0.09 (−1.20, 1.38) | 0.89 |
| Condyle/glenoid fossa skeletal | ||||||||||||
| Right anterior fossa AP (mm) | −1.55 | 1.50 | −0.75 | 0.90 | −0.30 | 0.46 | 0.79 (−0.23, 1.82) | 0.12 | 1.25 (0.30, 2.20) | 0.01* | 0.46 (−0.49, 1.41) | 0.33 |
| Right anterior fossa SI (mm) | −0.54 | 0.73 | −0.80 | 0.47 | −0.16 | 0.56 | −0.26 (−0.87, 0.35) | 0.39 | 0.38 (−0.19, 0.94) | 0.18 | 0.64(0.07, 1.20) | 0.03* |
| Left anterior fossa AP (mm) | −0.93 | 1.74 | −0.58 | 0.49 | −0.26 | 0.39 | 0.35 (−0.69, 1.39) | 0.50 | 0.67 (−0.30, 1.63) | 0.17 | 0.32 (−0.64, 1.29) | 0.50 |
| Left anterior fossa SI (mm) | −0.55 | 0.44 | −0.61 | 0.41 | −0.25 | 0.68 | −0.07 (−0.63, 0.50) | 0.81 | 0.30 (−0.22, 0.82) | 0.25 | 0.37 (−0.16, 0.89) | 0.16 |
| Right posterior fossa AP (mm) | −0.57 | 0.77 | −0.31 | 0.62 | −0.52 | 0.85 | 0.27 (−0.52, 1.05) | 0.50 | 0.05 (−0.68, 0.79) | 0.88 | −0.21 (−0.94, 0.52) | 0.56 |
| Right posterior fossa SI (mm) | 0.62 | 1.19 | 0.69 | 0.54 | 0.05 | 0.36 | 0.06 (−0.71, 0.83) | 0.87 | −0.57 (−1.29, 0.14) | 0.11 | −0.63 (−1.35, 0.08) | 0.08 |
| Left posterior fossa AP (mm) | −0.80 | 0.81 | −0.42 | 0.53 | −0.43 | 0.73 | 0.38 (−0.35, 1.11) | 0.29 | 0.38 (−0.30, 1.05) | 0.26 | 0.00 (−0.68, 0.67) | 0.99 |
| Left posterior fossa SI (mm) | 0.82 | 0.98 | −0.15 | 0.12 | 0.01 | 0.43 | −0.97 (−1.71, −0.24) | 0.01* | −0.81 (−1.49, −0.13 | 0.02* | 0.16 (−0.52, 0.84) | 0.63 |
| Right condylion AP (mm) | −0.61 | 0.87 | −0.32 | 1.64 | −0.22 | 0.58 | 0.30 (−0.81, 1.40) | 0.58 | 0.39 (−0.64, 1.42) | 0.44 | 0.09 (−0.93, 1.12) | 0.85 |
| Right condylion SI (mm) | −0.58 | 0.73 | −0.64 | 1.03 | 0.03 | 0.56 | −0.06 (−0.86, 0.74) | 0.88 | 0.61 (−0.13, 1.35) | 0.10 | 0.67 (−0.07, 1.41) | 0.08 |
| Left condylion AP (mm) | −0.60 | 1.31 | −0.07 | 0.65 | 0.12 | 0.65 | 0.53 (−0.40, 1.45) | 0.25 | 0.71 (−0.14, 1.57) | 0.10 | 0.19 (−0.67, 1.05) | 0.65 |
| Left condylion SI (mm) | −0.53 | 0.81 | −0.49 | 0.65 | 0.28 | 0.81 | 0.04 (−0.75, 0.83) | 0.92 | 0.81 (0.07, 1.54) | 0.03* | 0.77 (0.03, 1.50) | 0.04* |
| Right geometric center of condyle AP (mm) | −1.00 | 0.88 | −0.32 | 1.09 | −0.26 | 0.81 | 0.67 (−0.28, 1.62) | 0.16 | 0.73 (−0.15, 1.62) | 0.10 | 0.06 (−0.82, 0.94) | 0.89 |
| Right geometric center of condyle SI (mm) | −0.34 | 0.65 | −0.41 | 1.02 | −0.49 | 0.64 | −0.08 (−0.87, 0.72) | 0.84 | −0.16 (−0.90, 0.58) | 0.67 | −0.08 (−0.82, 0.66) | 0.83 |
| Left geometric center of condyle AP (mm) | −0.60 | 1.81 | −0.68 | 0.71 | −0.22 | 0.57 | −0.08 (−1.22, 1.07) | 0.89 | 0.39 (−0.68, 1.45) | 0.46 | 0.46 (−0.60, 1.53) | 0.38 |
| Left geometric center of condyle SI (mm) | −0.26 | 0.99 | −0.42 | 1.19 | 0.15 | 0.99 | −0.15 (−1.24, 0.93) | 0.77 | 0.41 (−0.59, 1.42) | 0.41 | 0.57 (−0.44, 1.57) | 0.26 |
AP, Antero-posterior (negative=posterior displacement, positive=anterior displacement); SI, Supero-inferior (negative=inferior displacement, positive=superior displacement).
Statistically significant at P<0.05 based on Fisher exact test.
Quantitative assessments of mandibular changes at the initial (T1) and final (T3) timepoints are reported in Table III. There were no significant differences in the vertical and anteroposterior positions of B-point between the 2 Herbst groups. There was a significant difference (P = 0.03) in the vertical position of B-point in the Herbst brachyfacial (−2.59 mm) and Herbst mesofacial (−2.75 mm) groups (P = 0.02) compared with the Class II control group at T1 to T3. However, there were considerable individual variations in this parameter, with significant overlaps in the range of vertical changes in B-point across all 3 groups.
There were no significant differences in the changes in the vertical or anteroposterior position of pogonion between the 2 Herbst groups from T1 to T3. Greater vertical displacements of pogonion at T1 to T3 were noted in the Herbst groups compared with the Class II controls, but the values were not statistically signifi-cant. There were no significant differences in the ante-roposterior position of pogonion across all 3 groups from T1 to T3.
Both Herbst groups showed similar increases in right and left mandibular lengths during phase 1, with no significant differences between the groups. There were no statistically significant differences in linear mandibular changes across both Herbst groups and the Class II control subjects at T3. Also, angular measurements evaluating changes in the FMPA showed no differences in changes across all 3 groups at all 3 times. There was a statistically significant (P = 0.02) closure of the right gonial angle in the Herbst mesofacial group (−1.59°) compared with the control group at T3.
Mean condylar and glenoid fossa displacements are shown in Table III. There were no significant differences in condylar and glenoid fossa changes in both Herbst groups from T1 to T3. There were no significant differences in the 3D positions of the geometric center of the condyle across all 3 groups at T3, with the overall trend being a slight posterior displacement. Point-to-point linear changes were evaluated for condylion, and showed a mean slight posterior displacement of right (−0.61 mm) and left (−0.60 mm) condylions in the Herbst brachyfacial group at T1 to T3. Similar results were reported for the Herbst mesofacial group (right condylion,−0.32 mm; left condylion,−0.07 mm).
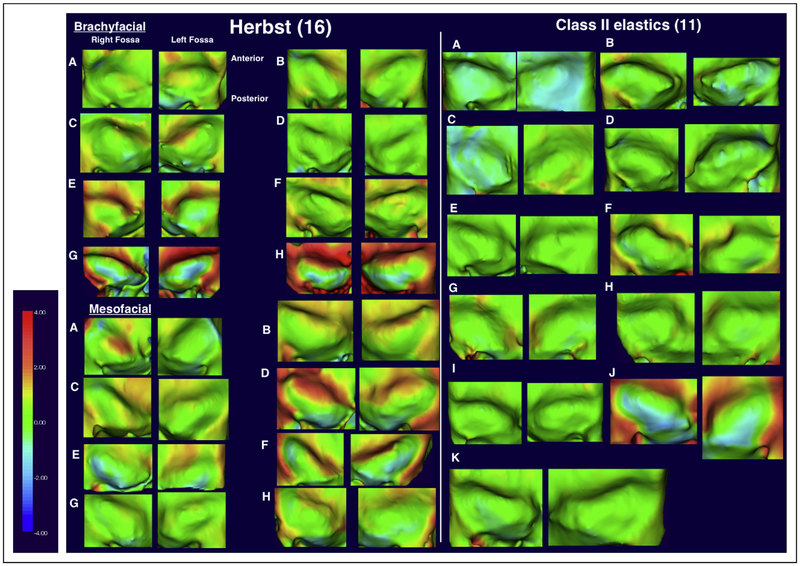
There were minimal differences in the direction and amount of fossa displacement in all 3 groups, with a trend toward posterior displacement of the right and left fossae from T1 to T3. This correlates with the direction of condylar displacement in the groups. There was a statistically significant (P = 0.01) increase in the mean posterior displacement in the right anterior fossa in the Herbst brachyfacial vs the Class II control group (−1.25 mm). The composite of individual fossa color maps, indicating a similar trend of either minimal change or slight posterior displacement of the fossae across all subjects, is illustrated in Figure 3.
Fig 3.
Color maps showing glenoid fossa skeletal changes calculated from the 3D volume renderings for both Herbst groups and the Class II controls at T1 to T3 when registered and superimposed at the anterior cranial base. The color map scale is set from −4 to +4 mm. Red represents regions of bony deposition; blue represents regions of bony resorption.
DISCUSSION
Previous studies evaluating the effects of functional appliances often use untreated Class II samples from the Bolton-Brush or the Michigan growth study as control subjects.28–30 A comparable untreated Class II sample with 3D radiographic data does not exist. Class II elastics have been shown to exert primarily dentoalveolar changes and therefore can be considered a suitable comparison group when evaluating skeletal and orthopedic changes with the Herbst appliance.8,10
The role of maxillary change in correcting Class II occlusion with the Herbst appliance has been unclear. Several cephalometric studies have reported a “headgear” effect with the Herbst appliance due to the posterior and upward force vector imparted to the maxilla.30,31 However, other studies have suggested that this “headgear” effect is negligible.8,15,32 The disagreement in the literature arises from the differences in methodology used to assess maxillary positional changes cephalometrically, primarily through changes in A-point. A-point can be affected by dentoalveolar changes because of movement of the maxillary incisors, and the use of SNA to assess maxillary anteroposterior changes has limitations, since vertical movement of A-point can account for the decrease in the SNA angle.33,34
The unreliability of 2-dimensional studies measuring changes with the appliance stimulated our aim in this study: to use 3D imaging and accurate superimpositions on the cranial base to measure accurately the effect on the maxilla.
Our study showed the expected forward and downward growth pattern of the maxilla in both the Herbst patients and the Class II controls, with no significant differences in the vertical and anteroposterior changes in A-point at the end of treatment across all 3 groups. The greater mean inferior movement of ANS observed here for the Herbst groups compared with the Class II controls could be due to the slightly shorter observation time for the control subjects. There were minimal differences in palatal plane angulation changes between the Herbst groups and the Class II control subjects.
Changes in the horizontal projection of the mandible can be related to (1) changes in mandibular growth direction, (2) changes in the amount of mandibular growth, or (3) changes in condylar or fossa position.
There are inconsistencies in the literature, with some evidence showing an increase in mandibular length and improved chin projection with Herbst treatment,9 and other studies showing no change in these parameters.32,35 Two-dimensional mandibular length measurements can be affected by deviations in patient positioning and superimposition of the left and right sides of the mandible and the difficulty in observing the condyle.10 We were able to reduce these sources of error using 3D imaging and found a slight increase in mandibular length in the Herbst groups compared with the Class II controls at T3, but this was not statistically significant.
There was also no statistically significant difference in pogonion position in the anteroposterior dimension across all 3 groups from T1 to T3, although there was slightly more individual variation in the Herbst brachyfacial group. There was an increase in inferior displacement of pogonion, but this was not statistically significant. There was a greater inferior displacement of B-point in the Herbst sample compared with the Class II controls; this can be attributed to an increase in vertical growth in the Herbst subjects.
Previous animal36,37 and human studies15,38 have shown changes in the gonial angle with functional appliance treatment. This directional change in growth can affect the horizontal projection of the chin. Our study showed, at T3, a statistically significant opening of the gonial angle (1.59°) in the Herbst mesofacial group compared with the Class II controls, but the clinical significance of such a small change is limited.
Previous research indicated that Herbst appliance treatment largely does not change the FMPA, although there is some evidence of a counterclockwise rotation of the mandible.39 We found a minimal change in the FMPA across the Herbst and Class II control groups at all 3 time points with some individual variations in all groups. This correlates well with previous cephalometric studies examining changes in the FMPA with Herbst treatment.40,41
The anterior displacement of the glenoid fossa is one purported skeletal change induced by the Herbst appliance that is thought to contribute to an increase in the horizontal projection of the mandible. This has been shown in several animal studies,42,43 but most human studies have been limited by the use of 2-dimensional imaging modalities. A previous magnetic resonance imaging study showed signs of glenoid fossa remodelling in most Herbst patients and suggested that the normal posteriorly directed fossa displacement was reverted in an anterior direction.44,45 Long-term cephalometric findings showed that this effect on the anterior displacement of the glenoid fossa was only temporary, and the amount and direction of the fossa changes were independent of the patients’ vertical facial pattern.46 These findings can be criticized, since for validity they rely on an unchanged condyle-fossa relationship according to the method described by Buschang and Santos-Pinto.47
The previous pilot CBCT study by LeCornu et al10 found resorption of the anterior wall of the glenoid fossa with deposition at the posterior wall in the Herbst sample. This was in contrast to the Class II control sample that had a posteriorly directed displacement of the fossa, which has been observed in other studies as part of the expected growth pattern in Class II subjects.47,48
In contrast to the findings of LeCornu et al,10 our study with a larger sample and longer follow-up period showed a similar posteriorly directed repositioning of the fossa in both Herbst groups and the Class II control subjects. There was a statistically significant mean difference of −1.25 mm in the position of the anterior wall of the right glenoid fossa in the Herbst brachyfacial group compared with the Class II controls; this has minimal clinical significance and is likely to be a reflection of the continued fossa growth pattern in Class II subjects. There were no clinically significant differences in the amount of glenoid fossa posterior displacement during the Herbst phase (T1-T2) and the subsequent fixed appliance phase (T2-T3). The differences in our findings could be due to a difference in the duration of Herbst treatment in our study (mean, 7.6 months) compared with the study of LeCornu et al (mean, 11.42 months), with a longer period of posturing the mandible forward possibly required to induce anterior displacement of the fossa or to alter the normal posteriorly directed growth pattern. Nevertheless, the outcomes reported by Le-Cornu et al were short term, and it is plausible that the glenoid fossa changes could have reverted if followed up over a longer observation time in their study.
A comparison of condylar and fossa positions indicated that they were both displaced posteriorly together. This is consistent with previous studies, which showed that the condyle-glenoid fossa relationship is largely unchanged with Herbst treatment.7,43,45 A future study with 3D regional mandibular superimpositions would be useful in determining differences in condylar remodelling and in the direction of condylar growth between the Herbst and Class II control patients.
The major limitation of this study was the small sample size. A larger study could distinguish changes that may be due to natural growth or differences that are too small to detect with our methodology. The use of CBCT could address this shortcoming in future studies. Additional weaknesses of the sample include differences in the observation times between the Herbst patients and the Class II control patients and the relative severity of the Class II skeletal malocclusions, particularly in the Herbst brachyfacial group compared with the Class II control group. Because of the retrospective nature of the study and the limited availability of Class II control subjects with 3D data, it was not possible to match the groups as well as in a prospective study design. It was also difficult to standardize the time of follow-up, with a large standard deviation (8.69 months) in treatment duration for the Class II control subjects. A prospective CBCT study with a larger sample size is recommended.
CONCLUSIONS
Three-dimensional imaging and superimposition techniques showed the following.
No significant differences in Herbst treatment response were seen in brachyfacial vs mesofacial subjects.
Herbst treatment in subjects with different vertical facial patterns showed the same posterior pattern of glenoid fossa and condylar displacement as did the Class II controls.
Herbst treatment in subjects with different vertical facial patterns did not show clinically significant maxillary growth restraint compared with Class II controls.
There were no clinically significant differences in changes in the mandibular plane and gonial angles in the Herbst subjects vs the Class II controls.
There were considerable individual variations in mandibular length changes in both Herbst groups, but this did not necessarily translate to an increase in the anteroposterior projection of pogonion. Larger samples are needed to verify these findings.
Supplementary Material
ACKNOWLEDGMENTS
We thank Paul Buchholz for providing all clinical Herbst records for this study and Ian Gordon, Department of Mathematics and Statistics at the University of Melbourne, for his help with assessment of the data.
REFERENCES
- 1.Proffit WR, Fields HW, Moray LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthod Orthognath Surg 1998;13:97–106. [PubMed] [Google Scholar]
- 2.Buschang PH, Martins J. Childhood and adolescent changes of skeletal relationships. Angle Orthod 1998;68:199–206. [DOI] [PubMed] [Google Scholar]
- 3.McNamara JA. Components of Class II malocclusion in children 8–10 years of age. Angle Orthod 1981;51:177–202. [DOI] [PubMed] [Google Scholar]
- 4.Pancherz H The Herbst appliance–its biologic effects and clinical use. Am J Orthod 1985;87:1–20. [DOI] [PubMed] [Google Scholar]
- 5.Keim RG, Gottlieb EL, Nelson AH, Vogels DI 3rd. 2008 JCO study of orthodontic diagnosis and treatment procedures. Part 1: results and trends. J Clin Orthod 2008;42:625–40. [PubMed] [Google Scholar]
- 6.Darendeliler MA. Validity of randomized clinical trials in evaluating the outcome of Class II treatment. Semin Orthod 2006; 12:67–79. [DOI] [PubMed] [Google Scholar]
- 7.Hansen K, Pancherz H, Hägg U. Long-term effects of the Herbst appliance in relation to the treatment growth period: a cephalo-metric study. Eur J Orthod 1991;13:471–81. [DOI] [PubMed] [Google Scholar]
- 8.Nelson B, Hansen K, Hägg U. Class II correction in patients treated with Class II elastics and with fixed functional appliances: a comparative study. Am J Orthod Dentofacial Orthop 2000;118:142–9. [DOI] [PubMed] [Google Scholar]
- 9.Cozza P, Baccetti T, Franchi L, De Toffol L, McNamara JA Jr. Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am J Orthod Dentofacial Orthop 2006;129:599.e1–12. [DOI] [PubMed] [Google Scholar]
- 10.LeCornu M, Cevidanes LH, Zhu H, Wu CD, Larson B, Nguyen T. Three-dimensional treatment outcomes in Class II patients treated with the Herbst appliance: a pilot study. Am J Orthod Dentofacial Orthop 2013;144:818–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baumrind S, Miller D, Molthen R. The reliability of head film measurements. Am J Orthod 1976;70:617–44. [DOI] [PubMed] [Google Scholar]
- 12.Houston W, Lee R. Accuracy of different methods of radiographic superimposition on cranial base structures. Eur J Orthod 1985;7:127–35. [DOI] [PubMed] [Google Scholar]
- 13.Pittayapat P, Bornstein MM, Imada TS, Coucke W, Lambrichts I, Jacobs R. Accuracy of linear measurements using three imaging modalities: two lateral cephalograms and one 3D model from CBCT data. Eur J Orthod 2014;37:202–8. [DOI] [PubMed] [Google Scholar]
- 14.Schaefer AT, McNamara JA, Franchi L, Baccetti T. A cephalometric comparison of treatment with the Twin-block and stainless steel crown Herbst appliances followed by fixed appliance therapy. Am J Orthod Dentofacial Orthop 2004;126:7–15. [DOI] [PubMed] [Google Scholar]
- 15.Pancherz H The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. Am J Orthod 1982; 82:104–13. [DOI] [PubMed] [Google Scholar]
- 16.Franchi L, Baccetti T, McNamara JA Jr. Treatment and posttreatment effects of acrylic splint Herbst appliance therapy. Am J Orthod Dentofacial Orthop 1999;115:429–38. [DOI] [PubMed] [Google Scholar]
- 17.Waltrick KB, de Abreu Junior MJ, Corrêa M, Zastrow MD, D’Avila Dutra V. Accuracy of linear measurements and visibility of the mandibular canal of cone-beam computed tomography images with different voxel sizes: an in vitro study. J Periodontol 2013; 84:68–77. [DOI] [PubMed] [Google Scholar]
- 18.Cevidanes LH, Heymann G, Cornelis MA, DeClerck HJ, Tulloch JF. Superimposition of 3-dimensional cone-beam computed tomography models of growing patients. Am J Orthod Dentofacial Orthop 2009;136:94–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cevidanes LH, Styner MA, Proffit WR. Image analysis and superim-position of 3-dimensional cone-beam computed tomography models. Am J Orthod Dentofacial Orthop 2006;129:611–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cevidanes LH, Oliveira AE, Grauer D, Styner M, Proffit WR. Clinical application of 3D imaging for assessment of treatment outcomes. Semin Orthod 2011;17:72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Björk A, Skieller V. Normal and abnormal growth of the mandible. A synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod 1983;5:1–46. [DOI] [PubMed] [Google Scholar]
- 22.Melsen B The cranial base: the postnatal development of the cranial base studied histologically on human autopsy material. Acta Odontol Scand 1974;32(Suppl 62). [Google Scholar]
- 23.de Oliveira Ruellas AC, Tonello C, Gomes LR, Yatabe MS, Macron L, Lopinto J, et al. Common 3-dimensional coordinate system for assessment of directional changes. Am J Orthod Dentofacial Orthop 2016;149:645–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park SH, Yu HS, Kim KD, Lee KJ, Baik HS. A proposal for a new analysis of craniofacial morphology by 3-dimensional computed tomography. Am J Orthod Dentofacial Orthop 2006;129:600.e23–34. [DOI] [PubMed] [Google Scholar]
- 25.Periago DR, Scarfe WC, Moshiri M, Scheetz JP, Silveira AM, Farman AG. Linear accuracy and reliability of cone beam CT derived 3-dimensional images constructed using an orthodontic volumetric rendering program. Angle Orthod 2008; 78:387–95. [DOI] [PubMed] [Google Scholar]
- 26.Baccetti T, Franchi L, McNamara JA. The cervical vertebral maturation (CVM) method for the assessment of optimal treatment timing in dentofacial orthopedics. Semin Orthod 2005;11:119–29. [Google Scholar]
- 27.Bland JM, Altman D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 327:307–10. [PubMed] [Google Scholar]
- 28.Serbesis-Tsarudis C, Pancherz H. “Effective” TMJ and chin position changes in Class II treatment. Angle Orthod 2008;78:813–8. [DOI] [PubMed] [Google Scholar]
- 29.VanLaecken R, Martin CA, Dischinger T, Razmus T, Ngan P. Treatment effects of the edgewise Herbst appliance: a cephalometric and tomographic investigation. Am J Orthod Dentofacial Orthop 2006;130:582–93. [DOI] [PubMed] [Google Scholar]
- 30.Wigal TG, Dischinger T, Martin C, Razmus T, Gunel E, Ngan P. Stability of Class II treatment with an edgewise crowned Herbst appliance in the early mixed dentition: skeletal and dental changes. Am J Orthod Dentofacial Orthop 2011;140:210–23. [DOI] [PubMed] [Google Scholar]
- 31.Pancherz H, Anehus-Pancherz M. The headgear effect of the Herbst appliance: a cephalometric long-term study. Am J Orthod Dentofacial Orthop 1993;103:510–20. [DOI] [PubMed] [Google Scholar]
- 32.Barnett GA, Higgins DW, Major PW, Flores-Mir C. Immediate skeletal and dentoalveolar effects of the crown or banded type Herbst appliance on Class II division 1 malocclusion. Angle Orthod 2008; 78:361–9. [DOI] [PubMed] [Google Scholar]
- 33.Ghafari J, Baumrind S, Efstratiadis S. Misinterpreting growth and treatment outcome from serial cephalographs. Clin Orthod Res 1998;1:102–6. [DOI] [PubMed] [Google Scholar]
- 34.Ricketts RM. Cephalometric synthesis: an exercise in stating objectives and planning treatment with tracings of the head roentgeno-gram. Am J Orthod 1960;46:647–73. [Google Scholar]
- 35.Pancherz H, Littmann C. Morphology and position of mandible in Herbst treatment. Cephalometric analysis of changes to end of growth period. Inf Orthod Kieferorthop 1988;21:493–513. [PubMed] [Google Scholar]
- 36.Voudouris JC, Woodside DG, Altuna G, Angelopoulos G, Bourque PJ, Lacouture CY. Condyle-fossa modifications and muscle interactions during Herbst treatment, part 2. Results and conclusions. Am J Orthod Dentofacial Orthop 2003;124:13–29. [DOI] [PubMed] [Google Scholar]
- 37.Voudouris JC, Woodside DG, Altuna G, Kuftinec MM, Angelopoulos G, Bourque PJ. Condyle-fossa modifications and muscle interactions during herbst treatment, part 1. New technological methods. Am J Orthod Dentofacial Orthop 2003;123: 604–13. [DOI] [PubMed] [Google Scholar]
- 38.Pancherz H The effects, limitations, and long-term dentofacial adaptations to treatment with the Herbst appliance. Semin Orthod 1997;3:232–43. [DOI] [PubMed] [Google Scholar]
- 39.Hägg U Change in mandibular growth direction by means of a Herbst appliance? A case report. Am J Orthod Dentofacial Orthop 1992;102:456–63. [DOI] [PubMed] [Google Scholar]
- 40.Pancherz H Vertical dentofacial changes during Herbst appliance treatment. A cephalometric investigation. Swed Dent J Suppl 1982;15:189–96. [PubMed] [Google Scholar]
- 41.Ruf S, Pancherz H. The effect of Herbst appliance treatment on the mandibular plane angle: a cephalometric roentgenographic study. Am J Orthod Dentofacial Orthop 1996;110:225–9. [DOI] [PubMed] [Google Scholar]
- 42.Rabie AB, Zhao Z, Shen G, Hägg EU, Robinson W. Osteogenesis in the glenoid fossa in response to mandibular advancement. Am J Orthod Dentofacial Orthop 2001;119:390–400. [DOI] [PubMed] [Google Scholar]
- 43.Woodside D, Metaxas A, Altuna G. The influence of functional appliance therapy on glenoid fossa remodeling. Am J Orthod Dentofacial Orthop 1987;92:181–98. [DOI] [PubMed] [Google Scholar]
- 44.Pancherz H, Fischer S. Amount and direction of temporomandibular joint growth changes in Herbst treatment: a cephalo-metric long-term investigation. Angle Orthod 2003;73: 493–501. [DOI] [PubMed] [Google Scholar]
- 45.Ruf S, Pancherz H. Temporomandibular joint growth adaptation in Herbst treatment: a prospective magnetic resonance imaging and cephalometric roentgenographic study. Eur J Orthod 1998;20: 375–88. [DOI] [PubMed] [Google Scholar]
- 46.Pancherz H, Michailidou C. Temporomandibular joint growth changes in hyperdivergent and hypodivergent Herbst subjects. A long-term roentgenographic cephalometric study. Am J Orthod Dentofacial Orthop 2004;126:153–61. [DOI] [PubMed] [Google Scholar]
- 47.Buschang PH, Santos-Pinto A. Condylar growth and glenoid fossa displacement during childhood and adolescence. Am J Orthod Dentofacial Orthop 1998;113:437–42. [DOI] [PubMed] [Google Scholar]
- 48.Agronin KJ, Kokich VG. Displacement of the glenoid fossa: a cephalometric evaluation of growth during treatment. Am J Orthod Dentofacial Orthop 1987;91:42–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.