Abstract
A new triterpene glycoside ilexdunnoside A (1) and a new sulfated triterpene derivative ilexdunnoside B (2), together with five known analogues 3–7 were isolated from the roots of Ilex dunniana Levl. The structures were established by NMR spectroscopic analysis and acid hydrolysis. Results of an in vivo study of the biological activity showed that 75% ethanol and n-butanol extracts of the plant displayed anti-inflammatory activities against ear edema in mice, with inhibition rates of 23.5% and 37.5%, respectively, at a dose of 50 mg/kg. Furthermore, Compounds 1, 2 and 3 exhibited moderate indirect inhibitory effects on lipopolysaccharide-induced NO production in BV2 microglial cells in vitro, with IC50 values of 11.60, 12.30 and 9.70 μM, respectively.
Keywords: triterpene glycosides, Ilex dunniana Levl, anti-inflammatory
1. Introduction
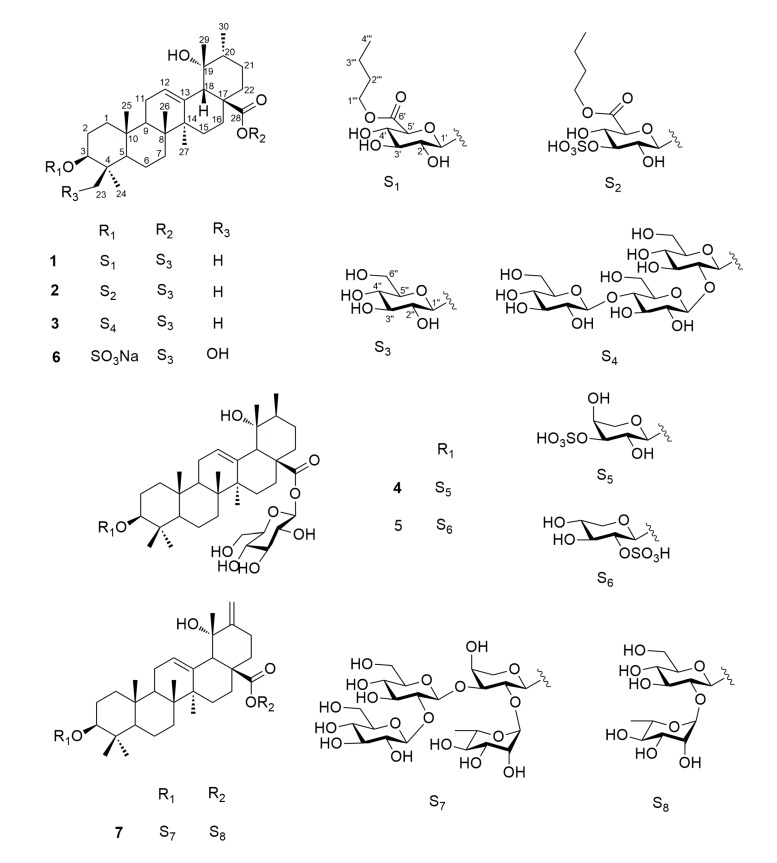
Inflammation is an important pathophysiological factor of many diseases, such as pneumonia, intestinal catarrh, rheumatoid arthritis, infectious diseases and so on. Plants from the genus Ilex (Aquifoliaceae) have been used in the clinic for clearing away inflammation, relieving cough, eliminating phlegm, and so on [1]. In order to search for anti-inflammatory active ingredients, we have performed systematical chemical and pharmacological investigations of Ilex dunniana Levl, an evergreen shrub or dungarunga widely distributed to the south of the Qinling mountains and Yangtze Valley in China. Herein we report the isolation and structural elucidation of two new triterpene glycosides, ilexdunnoside A (1) and ilexdunnoside B (2) (Figure 1), together with five known analogues 3–7 from the roots of Ilex dunniana Levl, as well as the anti-inflammatory activity of all the isolated compounds.
Figure 1.
Structures of compounds 1–7.
2. Results and Discussion
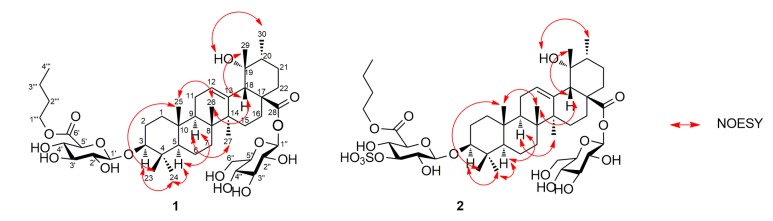
Ilexdunnoside A (1) was isolated as a white, amorphous powder. Its molecular formula was established as C46H74O15 by HRESIMS (m/z 865.4943 [M − H]−, calcd for 865.4955) and NMR data, implying 10 degrees of unsaturation. The 1H-NMR spectrum (see Table 1 and Figure S1) showed six tertiary methyl groups at δH 0.86, 0.96, 1.15, 1.33, 1.39, and 1.69 (each 3H, s), a secondary methyl at δH 1.06 (3H, d, J = 8.0 Hz), an oxymethine proton at δH 3.32 (1H, dd, J = 11.7, 4.5 Hz), and an olefinic proton at δH 5.53 (1H, br s). The 13C-NMR spectrum (see Table 1 and Figure S2) exhibited 46 carbon resonances, of which 30 were attributed to the aglycone. Signals at δC 89.2 (C-3), 72.5 (C-19), 128.3 (C-12), 139.2 (C-13), and 176.9 (C-28) were assigned to an oxygenated sp3 methine, an oxygenated sp3 quaternary, a pair of typical olefinic carbons and a carboxy carbon, respectively. The aforementioned data suggested that 1 was a pentacyclic triterpenoid derivative, similar to 3β,19α-dihydroxy-urs-12-en-28-oic acid [2], with the primary difference being the presence of a d-glucuronic acid (GlcA), a d-glucose (Glc), and a n-butyl in 1. The relative configuration of the aglycone of 1 was elucidated based on the spectrum (Figure 2). The correlations of H-3/Me-24, H-5/Me-24, H-5/H-9, H-9/Me-27, OH-19/Me-30 confirmed that these groups were cofacial and α-oriented. Likewise, correlations of Me-23/Me-25, Me-25/Me-26, H-18/Me-26, H-18/Me-29 showed the β-orientation of these groups. The absolute configuration of the aglycone of 1 was presumed to be 3S, 5R, 8R, 9R, 10R, 14S, 17S, 18S, 19R, and 20R, by the hypothetical biogenetic pathway.
Table 1.
1H- (400 MHz) and 13C-NMR (100 MHz) spectral data of 1 and 2 in C5D5N (δ in ppm).
| Position | Compound 1 | Compound 2 | ||
|---|---|---|---|---|
| δC | δH a (J in Hz) | δC | δH a (J in Hz) | |
| 1 | 38.7 | 0.84, 1.46 | 38.2 | 0.76, 1.37 |
| 2 | 26.9 | 1.85, 2.12 | 26.4 | 1.88, 1.74 |
| 3 | 89.2 | 3.32 dd (11.7, 4.5) | 88.9 | 3.23 dd (12.0, 4.5) |
| 4 | 39.4 | 39.0 | ||
| 5 | 55.7 | 0.80 | 55.2 | 0.71 |
| 6 | 18.6 | 1.44, 1.28 | 18.1 | 1.37, 1.21 |
| 7 | 33.4 | 1.41, 1.56 | 32.9 | 1.49, 1.31 |
| 8 | 40.4 | 40.0 | ||
| 9 | 47.6 | 1.74 | 47.1 | 1.65 |
| 10 | 36.8 | 36.4 | ||
| 11 | 23.9 | 2.00 | 23.4 | 1.89 |
| 12 | 128.3 | 5.53 br s | 127.8 | 5.41 br s |
| 13 | 139.2 | 138.7 | ||
| 14 | 42.0 | 41.5 | ||
| 15 | 29.1 | 2.44 m, 1.22 | 28.7 | 2.31 m, 1.13 |
| 16 | 26.0 | 3.09 m, 1.99 | 25.5 | 2.95 m, 1.97 |
| 17 | 48.6 | 48.1 | ||
| 18 | 54.3 | 2.90 s | 53.9 | 2.78 s |
| 19 | 72.5 | 72.0 | ||
| 20 | 42.0 | 1.33 | 41.6 | 1.25 |
| 21 | 26.6 | 2.00, 1.84 | 26.0 | 1.86, 1.99 |
| 22 | 37.6 | 2.03, 1.82 | 37.2 | 1.70, 1.89 |
| 23 | 28.0 | 1.33 s | 27.5 | 1.17 s |
| 24 | 16.8 | 0.96 s | 16.3 | 0.88 s |
| 25 | 15.5 | 0.86 s | 15.0 | 0.72 s |
| 26 | 17.3 | 1.15 s | 16.8 | 1.02 s |
| 27 | 24.5 | 1.69 s | 24.0 | 1.58 s |
| 28 | 176.9 | 176.5 | ||
| 29 | 26.9 | 1.39 s | 26.1 | 1.29 s |
| 30 | 16.6 | 1.06 d (8.0) | 16.1 | 0.98 d (6.4) |
| 1′ | 107.3 | 4.95 d (7.7) | 106.2 | 4.89 d (7.6) |
| 2′ | 75.3 | 4.06 | 73.4 | 4.02 |
| 3′ | 77.9 | 4.26 | 83.6 | 5.16 |
| 4′ | 73.0 | 4.48 | 72.0 | 4.40 t (9.1) |
| 5′ | 77.2 | 4.57 | 76.1 | 4.48 d (9.5) |
| 6′ | 170.3 | 169.3 | ||
| 1′′ | 95.7 | 6.26 d (8.0) | 95.3 | 6.13 d (8.0) |
| 2′′ | 73.9 | 4.20 | 71.2 | 4.10 |
| 3′′ | 78.8 | 4.28 | 78.2 | 4.19 |
| 4′′ | 71.1 | 4.31 | 70.6 | 4.20 |
| 5′′ | 79.1 | 4.02 | 78.7 | 3.91 m |
| 6′′ | 62.2 | 4.44, 4.38 | 61.6 | 4.32, 4.27 |
| 1′′′ | 64.9 | 4.26 | 64.6 | 4.19 |
| 2′′′ | 30.8 | 1.56 | 30.3 | 1.48 |
| 3′′′ | 19.2 | 1.30 | 18.7 | 1.22 |
| 4′′′ | 13.7 | 0.75 t (7.3) | 13.2 | 0.68 t (7.1) |
a Multiplicity is not clear for some signals due to overlapping.
Figure 2.
Key NOESY correlations of 1 and 2.
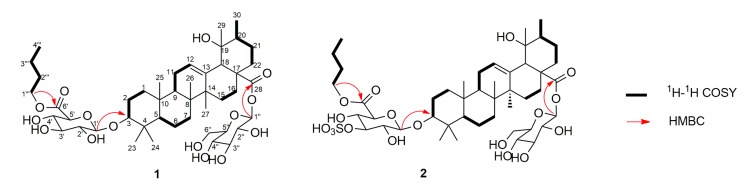
In the 1H-NMR spectrum, the sugar portion showed two anomeric proton signals at δH 4.95 (1H, d, J = 7.7 Hz) and δH 6.26 (1H, d, J = 8.0 Hz), with corresponding anomeric carbons at δC 107.3 and 95.7, respectively. The sugar units were confirmed to be d-glucuronic acid (GlcA) and d-glucose (Glc) by GC analysis of their chiral derivatives after the hydrolysis of 1 with 2 N CF3COOH. The 1H-1H COSY and HSQC spectra revealed the presence of an n-butyl in 1, while HMBC correlations from H2-1‴ to C-6′ (170.3) (Figure 3), indicated the attachment of the n-butyl to C-6′ Relative large coupling constants of 3JH1’–H2’ (7.7 Hz) and 3JH1″–H2″ (8.0 Hz) of (6′-BuO) GlcA and Glc in their pyranose form indicated the β-anomeric orientation of them. HMBC correlations from H-1′ to C-3 (δC 89.2), and from H-1″ to C-28 (δC 176.9) indicated that the anomeric carbons of (6′-BuO) GlcA and Glc were connected to C-3 and C-28 of the aglycone, respectively. Thus, compound 1 was identified as 3β-(6-O-n-butyl-d-glucuronopyranosyl)-19α-hydroxy-urs-12-en-28-oic acid 28-O-β-d-glucopyranoside, and named ilexdunnoside A.
Figure 3.
Key 1H-1H COSY and HMBC correlations of 1 and 2.
Ilexdunnoside B (2) was obtained as a white, amorphous powder. It had the molecular formula of C46H74O18S according to the deprotonated molecule at m/z 945.4538 [M − H]− (calcd for 945.4523) in the HRESIMS, suggesting that there was a sulfate group in the molecule. The 1H- and 13C-NMR spectra showed the characteristic resonances of a 3β,19α-dihydroxy-urs-12-en-28-oic acid skeleton, similar to those of 1, the only difference being in the sugar portion of 2. The NMR data showed the presence of an unusual d-(3-O-sulphonyl-6-O-n-butyl)-glucuronopyranosyl unit in 2 instead of the d-(6-O-n-butyl)-glucuronopyranosyl moiety in 1, as supported by the downfield shifts of the H-3′ (δH 5.16) and C-3′ (δC 83.6) of 2 compared with H-3′ (δH 4.26) and C-3′ (δC 77.9) of 1. Acid hydrolysis of 2, followed by treatment with BaCl2, obtained a white precipitate, also demonstrating the presence of a sulfate group. On the basis of the NOESY spectrum, the relative configuration of 2 was identical to that of 1. Using the hypothetical biogenetic pathway permitted the assignment of the absolute configuration of 2 as 3S, 5R, 8R, 9R, 10R, 14S, 17S, 18S, 19R and 20R. Therefore, the structure of compound 2 was elucidated as 3β-(3-O-sulphonyl-6-O-n-butyl-d-glucuronopyranosyl)-19α-hydroxy-urs-12-en-28-oic acid 28-O-β-d-glucopyranoside, and named ilexdunnoside B.
The five known compounds were identified as hylonoside II (3), ilexpublesnin H (4), ilexpublesnin I (5), ilexoside XXXV (6), ilekudinoside F (7), based on the analysis and comparison of their experimental physical and spectroscopic data with literature values [3,4,5,6]. Compounds 1–7 are triterpene glycosides, of which compounds 4 and 5 belong to the sulfated triterpene glycoside class of compounds.
Microglial cells, which are regarded as the most important immune cells in the central nervous system (CNS), are activated by brain injuries. Following activation by bacterial toxins, microglial cells secrete a wide range of inflammatory mediators, such as nitric oxide (NO), tumor necrosis factor-α (TNF-α), interleukin (IL)-1β, and prostanoids [7]. Nitric oxide (NO) plays an important role in the inflammatory process, and an inhibitor of NO production may be considered as a potential anti-inflammatory agent [8]. NO is a physiological messenger that triggers a variety of actions in several systems [9]. It can modulate the release of various inflammatory mediators from a wide range of cells participating in inflammatory responses. Because of its anti-inflammatory properties and cytoprotective effects, adjunctive NO has been considered a plausible means for improving the anti-inflammatory activity. In recent years, NO-releasing drugs have been developed, usually as derivatives of other drugs, which exhibit very powerful anti-inflammatory effects [10,11,12,13].
In order to identify the biological activity, an in vivo anti-inflammatory model were used, the results showed that the 75% ethanol and n-butanol extracts of the plant exhibited anti-inflammatory activities against ear edema in vivo, with inhibition rates of 23.5% and 37.5%, respectively, at a dose of 50 mg/kg (as shown in Table 2). Furthermore, as shown in Table 3, in vitro results showed that compounds 1–7 obtained from the n-butanol extract were tested for their inhibitory effects on lipopolysaccharide-induced NO production in mouse microglial cells. Compounds 1–3 displayed moderate indirect anti-inflammatory activity, in which, compound 3 showed cytotoxic activity against microglial cell in vitro (Table 4), so the indirect anti-inflammatory activity of 3 partly may be caused by the cytotoxic activity. The other compounds exhibited weak activities for the inhibition of NO production, and did not show cytotoxic activity.
Table 2.
Effects of the plant extracts on ear edema induced by croton oil in mice.
| Extracts | Dose (mg/kg) | Edema Degree (mg) | Inhibitation Rate (%) |
|---|---|---|---|
| 75% Ethanol extract | 50.0 | 15.31 ± 2.01 * | 23.5 |
| n-Butanol extract | 50.0 | 12.50 ± 1.50 ** | 37.5 |
| Dexamethasone a | 1.0 | 5.80 ± 0.90 ** | 71.0 |
| Control group | - | 20.01 ± 2.31 | - |
a Positive control; * p < 0.05 vs. control group; ** p < 0.01 vs. control group.
Table 3.
Inhibitory effects of compounds against LPS-induced NO production in mouse BV2 microglial cells (n = 3).
| Compounds | IC50 (μM) | Compounds | IC50 (μM) |
|---|---|---|---|
| 1 | 11.60 ± 0.89 | 5 | 50.7 ± 3.25 |
| 2 | 12.30 ± 1.21 | 6 | 22.3 ± 2.23 |
| 3 | 9.70 ± 0.86 | 7 | 55.2 ± 3.26 |
| 4 | 33.5 ± 2.11 | dexamethasone a | 0.03 |
a Positive control.
Table 4.
The cytotoxic activity of compounds on BV2 microglial cells (n = 3).
| Compounds | Cell Viability | ||||
|---|---|---|---|---|---|
| 5.0 μM | 10.0 μM | 20.0 μM | 40.0 μM | 80.0 μM | |
| 1 | 99.74 ± 1.21 | 99.28 ± 1.32 | 99.35 ± 1.26 | 99.62 ± 1.89 | 99.70 ± 1.36 |
| 2 | 98.32 ± 2.05 | 98.25 ± 1.87 | 98.16 ± 1.25 | 98.56 ± 1.37 | 98.26 ± 1.88 |
| 3 | 91.74 ± 1.11 * | 90.28 ± 1.82 * | 89.35 ± 1.35 * | 88.62 ± 1.21 * | 88.50 ± 1.32 * |
| 4 | 99.36 ± 1.31 | 99.37 ± 1.21 | 99.67 ± 1.32 | 99.57 ± 1.53 | 99.33 ± 1.30 |
| 5 | 98.21 ± 1.93 | 99.33 ± 1.54 | 99.32 ± 1.32 | 99.21 ± 1.66 | 99.13 ± 1.28 |
| 6 | 102.21 ± 1.03 | 102.28 ± 1.56 | 103.35 ± 1.58 | 103.26 ± 1.28 | 103.22 ± 1.89 |
| 7 | 101.55 ± 1.42 | 101.68 ± 1.36 | 101.76 ± 1.47 | 101.38 ± 1.58 | 101.68 ± 1.38 |
| Control group | 100.00 ± 1.51 | 100.00 ± 1.26 | 100.00 ± 1.56 | 100.00 ± 1.78 | 100.00 ± 1.55 |
| Dexamethasone a | 101.02 ± 1.01 | 99.98 ± 1.32 | 100.25 ± 1.67 | 101.37 ± 1.83 | 99.78 ± 1.63 |
a Positive control; * p < 0.05 vs. control group.
3. Experimental Section
3.1. General Information
Optical rotations were obtained on a P2000 automatic digital polarimeter (JASCO, Tokyo, Japan). NMR spectra were measured on a Mercury-400 spectrometer (Varian, Palo Alto, CA, USA). HRESIMS spectra were acquired with an Agilent Technologies 6250 Accurate-Mass Q-TOF LC/MS spectrometer (Agilent, Santa Clara, CA, USA). The MPLC system (Biotage, Uppsala, Sweden) was equipped with an YMC-Pack ODS-A column (500 mm × 50 mm, 50 μm, YMC, Tokyo, Japan). Column chromatography was conducted with MCI GEL CHP20P resin (75–150 μm, Mitsubishi, Tokyo, Japan) and Sephadex LH-20 (Pharmacia Biotech AB, Uppsala, Sweden). TLC was carried out with glass precoated with silica gel GF254. BV2 microglial cells were obtained from the Cell Bank of the Chinese Academy of Sciences (Shanghai, China). A microplate reader (Thermo Fisher Scientific, Waltham, MA, USA) was used for the cytotoxicity assays.
3.2. Plant Material
The roots of Ilex dunniana Levl were collected in Mount Emei, Sichun Province, People’s Republic of China, in August 2015, and were identified by Associate Prof. Xiao-Zhong Chen from Heilongjiang University of Chinese Medicine. A voucher specimen (ID-g-20150828) was deposited at the herbarium of the Jiamusi College, Heilongjiang University of Chinese Medicine.
3.3. Extraction and Isolation
The air-dried, powdered root of Ilex dunniana Levl (5 kg) were extracted with 75% EtOH (10 L × 1 h × 3). A dried extract (800 g), obtained after concentration in vacuo, was suspended in H2O, and partitioned with petroleum ether (60–90 °C), EtOAc, and n-BuOH, successively. After the solvent was removed, the n-BuOH extracts (60 g) was subjected to MCI GEL CHP20P resin (75–150 μm) eluting with H2O, 50% EtOH, and 95% EtOH. The 50% EtOH eluate (20 g) was separated by MPLC (5–100% MeOH-H2O, 80 mL/min, 6 h) to obtain 30 fractions (Fr. 1–Fr. 30). Fraction 5 (1.0 g) was chromatographed over Sephadex LH-20 using MeOH, to give compound 7 (12.0 mg). Fraction 6 (2.0 g) was subjected to Sephadex LH-20 eluting with MeOH, to obtain compound 3 (8.0 mg). The separation of fraction 9 (1.0 g) was achieved by Sephadex LH-20 using MeOH as the eluent, to afford 4 (5.0 mg) and 5 (6.3 mg). Fractions 10 (3.5 g) and 15 (1.3 g) were also purified by Sephadex LH-20 eluting with MeOH, to give compounds 1 (7.5 mg), 2 (9.5 mg), and 6 (5.0 mg), respectively.
3.4. Product Characterization
Ilexdunnoside A (1): white, amorphous power; [α] + 38.1 (c 0.1, CH3OH); 1H-NMR (C5D5N, 400 MHz) and 13C-NMR (C5D5N, 100 MHz) see Table 1; HRESIMS m/z 865.4943 [M − H]− (calcd. for 865.4955, C46H73O15).
Ilexdunnoside B (2): white, amorphous power; [α] + 56.1 (c 0.2, CH3OH); 1H-NMR (C5D5N, 400 MHz) and 13C-NMR (C5D5N, 100 MHz) see Table 1; HRESIMS m/z 945.4538 [M − H]− (calcd. for 945.4523, C46H73O18S).
3.5. Acid Hydrolysis of Saponins
Each saponin (1.0 mg) was refluxed with 2 N aqueous CF3COOH (10 mL) at 100 °C for 2 h. The reaction mixture was partitioned between H2O (10 mL) and CH2Cl2 (3 × 4 mL). The CH2Cl2 layer were washed with H2O and evaporated to obtain the aglycone. After evaporation in vacuo and removing the acid by adding MeOH, the aqueous extracts were analyzed by GC. Thus, the absolute configuration of the crude sugar was demonstrated as described in the previous papers [14,15].
3.6. Detection of the Sulfate Group
Each compound (2–3 mg) was refluxed with 10% HCl (4 mL) for 4 h. After that the reaction mixture was extracted with Et2O. Then, an aliquot of the aqueous layer of each sample was treated with 70% BaCl2 to yield a white precipitate (BaSO4) [16].
3.7. In Vitro Anti-Inflammatory Activity Assays
BV2 microglial cells were maintained in RPMI1640 medium at 37 °C in 5% CO2. The cells were placed in 48-well plates and preincubated for 24 h, treated with tested triterpene glycosides dissolved in DMSO at various final concentrations (5.0, 10.0, 20.0, 40.0, 80.0 μM) in triplicate for 1 h, and continuously incubated with LPS (1 μg/mL) for 24 h. Dexamethasone (10−6 M) was used as the positive control. From each well, the supernatants (100 μL) were mixed with an equal amount of Griess reagent at room temperature for 20 min. The concentration of NO2− was measured for the amount of NO by a microplate reader at 570 nm, using sodium nitrite as the standard to calculate the concentration of the nitrite [17,18].
3.8. Cytotoxicity Assays
Cell viabilities were measured using the MTT assay. Briefly, BV2 microglial cells were seeded in 96-well plates at concentrations of 1 × 105 cells per well. After incubation for 2 h, the cells were incubated with compounds for 24 h and then washed with PBS three times. Following the washing step, 200 μL of RPMI 1640 medium containing 0.5 mg/mL MTT were added to each well, the cells were then incubated at 37 °C for another 4 h. Finally, the culture medium was removed, and the formazan crystal was dissolved by adding 150 μL of DMSO. Absorbances at 570 nm were measured using a microplate reader.
3.9. In Vivo Anti-Inflammatory Assays
On the basis of the inhibition of croton oil-induced ear edema in mice, the topical anti-inflammatory activity of the test compounds was evaluated. Animal experiments were performed in accordance to the Institutional Guidelines for Animal Care and Use of the Chinese Academy of Medical Sciences and Peking Union Medical College. The protocol was approved by the Committee on the Ethics of Animal Experiments of the Chinese Academy of Medical Sciences and Peking Union Medical College (permit pumber: 002973).The croton oil (Croton tiglium L., seed oil) was purchased from Sigma-Aldrich (St. Louis, MO, USA). In ICR male mice (18–20 g, n = 10 per group), croton oil (0.4 mg) was mixed with acetone (1 mL) to be applied to the left ear (10 μL each side) topically to induce ear edema. The animals were administered with candidate extracts (50 mg/kg) for 1 h, followed by treatment with croton oil for 4 h. After the application of croton oil, the mice were euthanized using sodium pentobarbital, and ear tissues (8 mm diameter punches) were collected for the measurement of the weight of ear patches (left and right). Based on the weight difference between two plugs (8 mm diameter) of the treated (left) and untreated (right) ears, the edematous response was measured. The percentage reduction in edema in treated mice compared with control mice is calculated for the expression of anti-inflammatory activity. Dexamethasone was used as the positive control [18,19].
4. Conclusions
The results of croton-oil ear inflammation in mice showed that 75% ethanol and n-butanol extracts of powdered root of Ilex dunniana Levl exerted anti-inflammatory activity in vivo against ear edema. Bioactivity-guided isolation of the n-butanol extract yielded two new triterpene glycoside 1 and 2 together with five known ones 3–7. Compounds 1–7 belong to the triterpene glycosides, of which compounds 4 and 5 belong to sulfated triterpene glycosides. Futhermore, in vitro anti-inflammatory activity showed that compounds 1, 2 and 3 obtained from the n-butanol extract exhibited moderate indirect anti-inflammatory activity on LPS-induced proinflammatory factors production in BV2 microglial cells.
Acknowledgments
Thanks to the support from the Natural Science Foundation of Liaoning Province of China (No. 20170540201), the Open Research Fund of State Key Laboratory of Bioactive Substance and Function of Natural Medicines, Dr. Start-up Fund of Dalian Nationalities University, the Science Research Fund Project of Heilongjiang University of Chinese Medicine (No. 201736), National Natural Science Foundation of China (No. 81673667), CAMS Innovation Fund for Medical Science (CIFMS) (No. 2016-I2M-3-015) and Middle-aged Academic Leaders and Reserved Talent Foundation of Yunnan (No. 2013HB099).
Supplementary Materials
The following are available online at http://www.mdpi.com/1420-3049/22/7/1206/s1.
Author Contributions
Xi Chen organized the study. Yu-Sheng Shi and Yan Zhang carried out the extraction and isolation. Wen-Zhong Hu, Xin Fu, Xia Lv, Li-Hong Zhang, Ning Zhang, and Guang Li interpreted the results and helped write the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Sample Availability: Samples of the compounds 1–7 are available from the authors.
References
- 1.Zhang Y., Li L., Zhang P., Pi H.F., Ruan H.L., Wu J.Z. Anti-inflammatory and free radical scavenging activities of ethanol extracts of two plants of Ilex. Acta Med. Univ. Sci. Technol. Huazhong. 2011;40:71–74. [Google Scholar]
- 2.Song J.L., Yang Y.J., Qi H.Y., Li Q. Chemical Constituents from Flowers of Gardenia jasminoides. J. Chin. Med. Mater. 2013;36:752–755. [PubMed] [Google Scholar]
- 3.Ouyang M.A. Glycosides from the leaves of Ilex hylonoma. Nat. Prod. Res. 2003;17:183–188. doi: 10.1080/1057563021000040781. [DOI] [PubMed] [Google Scholar]
- 4.Zhou Y., Chai X.Y., Zeng K.W., Zhang J.Y., Li N., Jiang Y., Tu P.F. Ilexpublesnins C-M, eleven new triterpene saponins from the roots of Ilex pubescens. Planta Med. 2013;79:70–77. doi: 10.1055/s-0032-1327927. [DOI] [PubMed] [Google Scholar]
- 5.Amimoto K., Yoshikawa K., Arihara S. Triterpenes and triterpene glycosides from the leaves of Ilex rotunda. Phytochemistry. 1993;33:1475–1480. doi: 10.1016/0031-9422(93)85114-7. [DOI] [Google Scholar]
- 6.Nishimura K., Miyase T., Noguchi H. Triterpenoid saponins from Ilex kudincha. J. Nat. Prod. 1999;62:1128–1133. doi: 10.1021/np990128y. [DOI] [PubMed] [Google Scholar]
- 7.Moon D.O., Choi Y.H., Kim N.D., Park Y.M., Kim G.Y. Anti-Inflammatory effects of beta-lapachone in lipopolysaccharide-stimulated BV2 microglia. Int. Immunopharmacol. 2007;7:506–514. doi: 10.1016/j.intimp.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Liu Y., Ma J.H., Zhao Q., Liao C.R., Ding L.Q., Chen L.X., Zhao F., Qiu F. Guaiane-type sesquiterpenes from Curcuma phaeocaulis and their inhibitory effects on nitric oxide production. J. Nat. Prod. 2013;76:1150–1156. doi: 10.1021/np400202f. [DOI] [PubMed] [Google Scholar]
- 9.Kerwin J.F., Heller M. The arginine-nitric oxide pathway: A target for new drugs. Med. Res. Rev. 1994;14:23–74. doi: 10.1002/med.2610140103. [DOI] [PubMed] [Google Scholar]
- 10.Konturek S., Konturek P.C. Role of nitric oxide in the digestive system. Digestion. 1995;56:1–13. doi: 10.1159/000201214. [DOI] [PubMed] [Google Scholar]
- 11.Katsuyama K., Shichiri M., Marumo F., Hirata Y. NO inhibits cytokine-induced iNOS expression and NF-κB activation by interfering with phosphorylation and degradation of IκB-α. Arterioscler. Thromb. Vasc. Biol. 1998;18:1796–1802. doi: 10.1161/01.ATV.18.11.1796. [DOI] [PubMed] [Google Scholar]
- 12.Ignarro L. Nitric oxide as a unique signaling molecule in vascular system: A historical overview. J. Physiol. Pharmacol. 2002;53:503–514. [PubMed] [Google Scholar]
- 13.Wallace J.L. Nitric oxide as a regulator of inflammatory processes. Mem. Inst. Oswaldo Cruz. 2005;100:5–9. doi: 10.1590/S0074-02762005000900002. [DOI] [PubMed] [Google Scholar]
- 14.Chaturvedula V.S.P., Schilling J.K., Miller J.S., Andriantsiferana R., Rasamison V.E., Kingston D.G.I. New cytotoxic oleanane saponins from the infructescences of Polyscias amplifolia from the Madagascar rainforest. Planta Med. 2003;69:440–444. doi: 10.1055/s-2003-39711. [DOI] [PubMed] [Google Scholar]
- 15.Elbandy M., Miyamoto T., Delaude C., Lacaille-Dubois M.A. Acylated preatroxigenin glycosides from Atroxima congolana. J. Nat. Prod. 2003;66:1154–1158. doi: 10.1021/np030057+. [DOI] [PubMed] [Google Scholar]
- 16.Akai E., Takeda T., Kobayashi Y., Ogihara Y. Minor triterpenoid saponins from the leaves of Bupleurum rotundifolium L. Chem. Pharm. Bull. 1985;33:3715–3723. doi: 10.1248/cpb.33.3715. [DOI] [Google Scholar]
- 17.Sacco R.E., Waters W.R., Rudolph K.M., Drew M.L. Comparative nitric oxide production by LPS-stimulated monocyte-derived macrophages from Ovis canadensis and Ovis aries. Comp. Immunol. Microbiol. Infect. Dis. 2006;29:1–11. doi: 10.1016/j.cimid.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 18.García-Argáez A.N., Ramírez Apan T.O., Delgado H.P., Velázquez G., Martínez-Vázquez M. Anti-inflammatory activity of coumarins from Decatropis bicolor on TPA ear mice model. Planta Med. 2000;66:279–281. doi: 10.1055/s-2000-14894. [DOI] [PubMed] [Google Scholar]
- 19.Mencherini T., Cau A., Bianco G., Loggia R.D., Aquino R.P., Autore G. An extract of Apium graveolens var. dulce leaves: Structure of the major constituent, apiin, and its anti-inflammatory properties. J. Pharm. Pharmacol. 2007;59:891–897. doi: 10.1211/jpp.59.6.0016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.