Abstract
The authors report the first case of traumatic late dissociation of the polyethylene insert with patellar tendon rupture after total knee arthroplasty using a high-flex posterior-stabilized Genesis II prosthesis in a 60-year-old Parkinson's disease patient. Insert dislodgement has been described most commonly with mobile-bearing and cruciate-retaining TKAs. Only four cases of insert dissociation in a high-flex fixed-bearing prosthesis have been described to date. This case report paves the way to understanding the potential reasons for insert dissociation and its management strategy.
Keywords: Arthroplasty, Replacement, Knee, Knee prosthesis, Knee joint, Prosthesis design, Female
Resumo
Os autores relatam o primeiro caso de dissociação tardia traumática do inserto de polietileno com ruptura do tendão patelar após artroplastia total do joelho, utilizando uma prótese Genesis II de alta flexibilidade e estabilização posterior, em paciente com 60 anos de idade com doença de Parkinson. A luxação do inserto plástico tem sido mais comumente descrita em ATJs com suporte de carga móvel e que pouparam o ligamento cruzado. Até o presente, foram descritos apenas quatro casos de dissociação dos insertos de polietileno em próteses de suporte fixo e alta flexibilidade. Este relato de caso abre caminho para a compreensão das potenciais causas de dissociação inserto de polietileno e sua conduta.
Palavras-chave: Artroplastia, Substituição, Joelho, Prótese de joelho, Articulação do joelho, Desenho da prótese, Sexo feminino
Introduction
Dissociation of the polyethylene insert from the tibial base plate is a rare entity and is usually been reported with mobile bearing total knee arthroplasty (TKA).1, 2 The occurrence of such an event is extremely rare with a fixed bearing prosthesis and has always been reported with cruciate retaining TKA.3, 4, 5 Till date dissociation of the polyethylene insert after high-flex posterior stabilized (PS) Genesis II TKA (Smith & Nephew, Memphis, Tennessee, USA) has been described in four reports.6, 7, 8, 9 Causes of dissociation described in these reports are thought to be due to trauma or failure of the locking mechanism.
Present case report describes polyethylene insert dissociation with patellar mechanism disruption in a fixed bearing High-flex PS Genesis II TKA. Unlike other cases, this case had a history of fall, late presentation (>2 years after primary surgery) and patellar tendon rupture. To our knowledge, this is the first case reported with patellar tendon disruption following a traumatic dissociation of polyethylene insert in a fixed bearing TKA.
Case report
A 60 year old female with Parkinson's disease underwent bilateral total knee replacement without patellar resurfacing for osteoarthritis, using fixed bearing high flex posterior stabilized (PS) Genesis II (Smith & Nephew, Memphis, Tennessee, USA) prosthesis in July 2014. Midvastus approach was used. Adequate ligamentous balancing with equal and symmetrical flexion-extension gaps were achieved intra-operatively. Cobalt chromium based metal components were used and fixed with cement. A 9 mm high flex PS polyethylene insert was slid into the baseplate until it engaged the locking mechanism. Proper seating of the insert was checked circumferentially, with medial and lateral aspects checked for complete locking of the posterior dovetails. The postoperative course was uneventful and a pain-free range of motion of 0–135° was achieved one month after the surgery. Walker assisted full-weight bearing ambulation was started on 1st post-operative day and continued for a month followed by unassisted ambulation. Radiographs showed well-fixed implants in five degrees of valgus. She came for routine follow-ups which were unremarkable with no pain or limitations in her daily activities.
At 28 months after the primary surgery, the patient complained of sudden onset knee pain with restricted motion after a fall at home. On examination, a swollen knee with an audible crepitus was appreciated. She was not able to actively extend her knee but a passive movement of 30°–70° was possible. Radiograph of the right knee revealed anterior dissociation of the insert from the tibial base plate without loosening of the femoral or tibial component (Fig. 1). A medial parapatellar arthrotomy was undertaken using the previous skin incision. A mid-substance patellar tendon rupture with complete dissociation of the polyethylene insert from the tibial base plate with anterior displacement was found (Fig. 2). Retrieved insert showed compression damage more on the posteromedial than on the posterolateral side of the non-articulating surface of the insert (Fig. 3). There was no damage/deformation seen on the articulating/superior surface or the post of the insert (Fig. 4). The intraoperative evaluation showed well-fixed components with no rotational malalignment. No osseous or soft tissue impingement was evident and flexion-extension gap balancing was also adequate. Since the tibial base plate demonstrated no loosening with an intact locking mechanism, a new conventional posterior stabilized 9 mm polyethylene insert was slid into the tibial base plate regaining a range of motion of 0–125. Medial and lateral sides were checked for proper engagement of dovetails.
Fig. 1.

Lateral radiograph showing anterior displacement of dissociated polyethylene insert from tibial base plate.
Fig. 2.
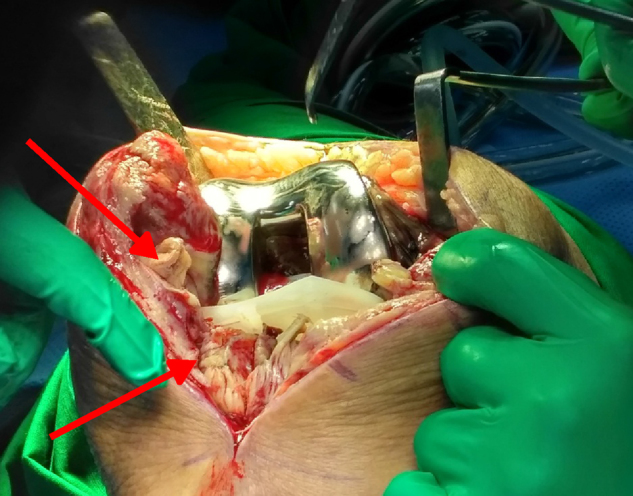
Intraoperative image showing mid-substance patellar tendon rupture (arrows pointing at both the ends) with anterior displacement of insert.
Fig. 3.

Images of the inferior surface of the retrieved insert showing damage of both the medial (red arrow) and lateral (yellow) dovetails. Damage was more on the postero-medial surface (red arrow).
Fig. 4.

Image of the superior surface showing lack of any deformation on the articulating side, including the post.
A direct repair of the mid-substance patellar tendon rupture was done which was further augmented with a harvested hamstring tendon graft. Same incision was used to harvest semitendinosus tendon. Intra-operative sample sent for culture were negative. Walker assisted full weight bearing ambulation with knee brace was started on 1st post-operative day. The range of flexion was increased to 60° at 2 weeks and to 90° at four weeks. At six weeks, knee brace was discontinued and an active extension was started.
Discussion
Polyethylene insert is primarily loaded in compression and there is a lack of tensile forces between insert and base plate.3 Therefore, insert dissociation from its base plate is very rare especially in a fixed bearing prosthesis. Its reported incidence in mobile bearing prosthesis varies from 0.4% to 9.3%.10 There are few reports of insert dissociation after fixed bearing prosthesis, and they had cruciate retaining prosthesis.3, 4, 5 Such an event is very rarely seen with fixed bearing high flex posterior stabilized TKA and there are only four cases reported till now.6, 7, 8, 9 All the cases used Genesis II (Smith & Nephew, Memphis, Tennessee, USA), similar to our case.
In this case report, patient had Parkinson's disease which in itself is a known predictor of poor functional outcome following TKA.11, 12, 13 Reports evaluating the outcomes of TKA in patients with Parkinson's disease are sparse. Although studies have concluded good pain relief but significant improvement in function is limited, owing to the disease itself.11, 14 Studies have reported an increased complication of fixed flexion contracture,11, 12, 13 extensor mechanism disruption,11, 12, 13 and posterior dislocation of the tibia11, 15 following TKA in these group of patients. But there are no published studies till now reporting insert dissociation following TKA in Parkinson's disease.
Rutten and Janssen6 reported a case of spontaneous dissociation of the insert at 14 months after an uneventful TKA. Retrieved insert showed no signs of damage on the articulating side but slight damage on the posterior side of the non-articulating surface was reported. The authors have stated that the dissociation was due to posterior lift-off of the insert as a result of the impingement of an osteophyte at the posterior femoral condyle. In et al. reported a case of recurring spontaneous dissociation of the insert after mini-vastus approach.7 Primary dissociation was seen within one month of TKA, followed by second dissociation occurring within one month of insert change. They believed that limited exposure leads to the incomplete seating of the insert resulting in early failure. Further, they have also believed that strong lift-off forces during high flexion could have damaged the tibial post and might have contributed to dissociation.
Lee et al.8 published a case of spontaneous dissociation that occurred at two and half years after TKA. Authors have attributed incomplete seating of the insert as a cause of late dissociation. Further, authors have stated that design of the high flex PS Genesis II might also have contributed to the cause. They believe that anterior tab snap-fit locking mechanism is too shallow, thus initiating an anterior insert lift-off the tray. This shallowness would facilitate a transition from lift-off to complete dissociation. They have also stated that repeated micro motion leads to progressive wear of the thin posterior dovetails resulting into subsequent dissociation. Astoul Bonorino et al.9 reported a case of traumatic dislodgement of the insert at 32 weeks after TKA. They have associated failure of the posterior locking mechanism to be the reason for dissociation.
Our case has some differences from the other cases reported. We have reported an occurrence of mid-substance patellar tendon rupture as a result of insert cutting through the extensor mechanism during complete dislodgement. Unlike In et al.,7 no tibial post damage was identified and in contrast to Rutten and Janssen,6 dissociation was not initiated as a result of impingement. We have reported a late presentation similar to Lee et al.8 which is in contrast to other studies presenting within two years of TKA.6, 7, 9 All the studies have reported damage to the posterior lips (medial and/or lateral) of the non-articulating surface of the polyethylene insert and anterior dislocation. These findings suggest damage of the thin posterior dovetails of the insert along with the failure of posterior locking mechanism leading to dissociation.
Astoul Bonorino et al.9 established three potential risk factors for liner dissociation which includes: error in surgical technique, prosthesis design, and patient-related factors. Various factors like flexion-extension gap balancing, ligamentous instability and inadequate capture of the insert on the base plate locking mechanism might play a role. Inserts with shallow anterior tab and thin posterior dovetails promote insert dissociation during deep flexion. Patient-related factors include young active patients, an involvement of high demanding activities like jumping and increased BMI. Based on the review of the literature, we conclude that implant related factor play the most important role in the occurrence of such an event and insert dislodgement can occur even when the soft tissue balancing is acceptable. Thin posterior dovetails with shallow anterior tab fit locking mechanism seen with Genesis II implant is the main reason behind insert dissociation. Association with Parkinson's disease can also be a risk factor which might have played a role.
Most of the authors suggest only changing the polyethylene insert, while others have recommended revision of the tibial base plate as well. They opine that such dissociations, not only damages the insert but also incapacitates the locking mechanism of the base plate necessitating revision.3, 16 Rutten and Janssen6 also show the association of posterior osteophytes impingement causing dissociation, which was corrected with insert change and removal of osteophyte. In our case, no structural damage to the locking mechanism of the base plate was seen, thus a polyethylene insert change to a conventional posterior stabilized was done without revision of the base plate.
Common to cases reported earlier in literature, this is insert dissociation following damage of the posterior dovetails, suggesting that the design of Genesis II is an issue particularly when greater stress is transmitted on the insert in condition like Parkinson's disease. Severity of dissociation can slice through the extensor mechanism which has not been reported in literature earlier. We wish to caution our colleagues to be aware of and look for this possibility at the time of revision of such a case.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at the P.D. Hinduja National Hospital, Department of Orthopaedics, Mumbai, India.
References
- 1.Fisher D.A., Bernasek T.L., Puri R.D., Burgess M.L. Rotating platform spinouts with cruciate-retaining mobile-bearing knees. J Arthroplasty. 2011;26(6):877–882. doi: 10.1016/j.arth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 2.Kobayashi H., Akamatsu Y., Taki N., Ota H., Mitsugi N., Saito T. Spontaneous dislocation of a mobile-bearing polyethylene insert after posterior-stabilized rotating platform total knee arthroplasty: a case report. Knee. 2011;18(6):496–498. doi: 10.1016/j.knee.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Anderson J.A., MacDessi S.J., Della Valle A.G. Spontaneous, recurrent dislodgment of the polyethylene tibial insert after total knee arthroplasty. A case report. J Bone Joint Surg Am. 2007;89(2):404–407. doi: 10.2106/JBJS.F.00750. [DOI] [PubMed] [Google Scholar]
- 4.Hedlundh U., Andersson M., Enskog L., Gedin P. Traumatic late dissociation of the polyethylene articulating surface in a total knee arthroplasty – a case report. Acta Orthop Scand. 2000;71(5):532–533. doi: 10.1080/000164700317381298. [DOI] [PubMed] [Google Scholar]
- 5.Davis P.F., Bocell J.R., Jr., Tullos H.S. Dissociation of the tibial component in total knee replacements. Clin Orthop Relat Res. 1991;(272):199–204. [PubMed] [Google Scholar]
- 6.Rutten S.G., Janssen R.P. Spontaneous late dislocation of the high flexion tibial insert after Genesis II total knee arthroplasty. A case report. Knee. 2009;16(5):409–411. doi: 10.1016/j.knee.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 7.In Y., Sur Y.J., Won H.Y., Moon Y.S. Recurrent dissociation of the tibial insert after mini-subvastus posterior-stabilized total knee arthroplasty: a case report. Knee. 2011;18(6):461–463. doi: 10.1016/j.knee.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 8.Lee D.H., Lee T.G., Park S.J., Han S.B. Spontaneous late dissociation of the tibial insert after high-flex posterior-stabilized Genesis II total knee arthroplasty. J Arthroplasty. 2013;28(2) doi: 10.1016/j.arth.2012.03.056. 374.e13-e16. [DOI] [PubMed] [Google Scholar]
- 9.Astoul Bonorino J.F., Slullitel P.A., Kido G.R., Bongiovanni S., Vestri R., Carbó L. Traumatic dislodgement of tibial polyethylene insert after a high-flex posterior-stabilized total knee replacement. Case Rep Orthop. 2015;2015:810716. doi: 10.1155/2015/810716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thompson N.W., Wilson D.S., Cran G.W., Beverland D.E., Stiehl J.B. Dislocation of the rotating platform after low contact stress total knee arthroplasty. Clin Orthop Relat Res. 2004;(425):207–211. doi: 10.1097/00003086-200408000-00029. [DOI] [PubMed] [Google Scholar]
- 11.Duffy G.P., Trousdale R.T. Total knee arthroplasty in patients with Parkinson's disease. J Arthroplasty. 1996;11(8):899–904. doi: 10.1016/s0883-5403(96)80130-6. [DOI] [PubMed] [Google Scholar]
- 12.Oni O.O., Mackenney R.P. Total knee replacement in patients with Parkinson's disease. J Bone Joint Surg Br. 1985;67(3):424–425. doi: 10.1302/0301-620X.67B3.3997953. [DOI] [PubMed] [Google Scholar]
- 13.Shah S.N., Hornyak J., Urquhart A.G. Flexion contracture after total knee arthroplasty in a patient with Parkinson's disease: successful treatment with botulinum toxin type A. J Arthroplasty. 2005;20(8):1078–1080. doi: 10.1016/j.arth.2004.11.008. [DOI] [PubMed] [Google Scholar]
- 14.Tinning C.G., Cochrane L.A., Singer B.R. Primary total knee arthroplasty in patients with Parkinson's disease: analysis of outcomes. Acta Orthop Belg. 2013;79(3):301–306. [PubMed] [Google Scholar]
- 15.Erceg M., Maricević A. Recurrent posterior dislocation following primary posterior-stabilized total knee arthroplasty. Croat Med J. 2000;41(2):207–209. [PubMed] [Google Scholar]
- 16.Tradonsky S., Postak P.D., Froimson A.I., Greenwald A.S. A comparison of the disassociation strength of modular acetabular components. Clin Orthop Relat Res. 1993;(296):154–160. [PubMed] [Google Scholar]


