A 40-year-old man presented to emergency department with an acute 2-day history of severe epigastric pain, coffee-ground emesis, and fatigue. Patient denied any history of trauma, acid/alkali ingestion, recent infections, smoking, alcohol consumption, non-steroidal anti-inflammatory drug use, varices, esophagitis, gastritis, peptic ulcer disease, or liver disease. Past medical and surgical history were notable for pancreatic vasoactive intestinal peptide-producing tumor; the post-resection status 18 months ago was without complications. Physical examination was unremarkable. Laboratory studies were remarkable for a hemoglobin level of 8.2 g/dL.
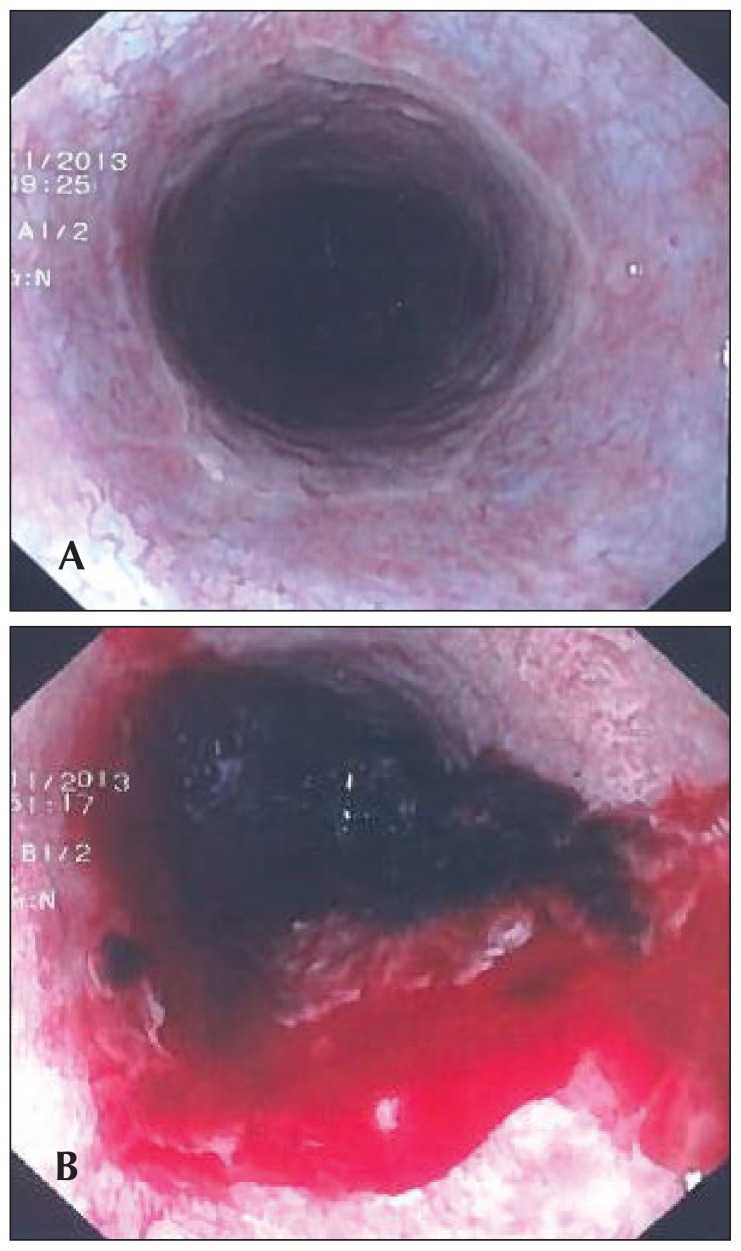
Esophagogastroduodenoscopy was done and showed circumferential black pigmentation, fragile esophageal necrotic mucosa, and multiple superficial ulcerations in the middle and lower thirds of esophagus (Figure 1A). The lower one-third of esophagus was covered with dark exudates, oozing fresh red-colored blood with minimal touch (Figure 1B). Stomach and duodenum (bulb, D1 and D2) were normal. Multiple biopsies from the lower esophagus and gastroesophageal junction were taken.
Figure 1.
Upper gastrointestinal endoscopy: (A) circumferential black pigmentation, fragile necrotic mucosa, and multiple superficial ulcerations in the middle and lower thirds of esophagus and (B) the lower one-third of the esophagus was covered with dark coffee-ground exudates, oozing fresh red-colored blood with minimal touch.
Histopathological examination was negative for malignancy and revealed small fragments of gastroesophageal mucosa with a focal area of ulceration (Figure 2A). The ulcerated area was replaced by local inflammatory changes comprising necrotic debris, neutrophil exudates, hemorrhage, and background fibrinous material deposition (Figure 2B). A diagnosis of acute esophageal necrosis was established.
Figure 2.
Microscopic examination of lower esophageal biopsy: (A) small fragments of gastroesophageal mucosa with focal area of ulceration (hematoxylin and eosin stain; magnification power: 10×) and (B) the ulcerated area was replaced by local inflammatory changes comprising necrotic debris, neutrophil exudates, hemorrhage, and background fibrinous material deposition (hematoxylin and eosin stain; magnification power: 40×).
Patient was admitted and kept nil-per-oral (NPO) and started on intravenous fluids, analgesia, total parenteral nutrition, high-dose omeprazole, and ranitidine. Patient received 2 units of packed red blood cells to restore hemoglobin levels. Three days later, the patient’s condition improved, and he was discharged home in a stable condition. At a 2-week follow-up, the patient was asymptomatic tolerating oral medications.
Acute esophageal necrosis (AEN) is also known as black esophagus, acute necrotizing esophagitis, acute esophageal infarction, and Gurvits syndrome.1,2 The exact pathogenesis of AEN is still unknown and likely to be multifactorial.3 Hematemesis, coffee-ground emesis, and melena are the most frequent presenting symptoms in roughly 90% of patients.3 Upper gastrointestinal endoscopy is the imaging modality of choice to establish the definitive diagnosis of AEN.4 Esophageal biopsy is supportive but not required for the diagnosis.4
Probable complications of untreated AEN may include the occurrence of esophageal stenosis, stricture, perforation, microbial superimposed infection, mediastinitis, mediastinal abscess, or death.3 The prognosis of AEN is generally very unfortunate with an approximated mortality rate of around 33% depending primarily on the underlying critical illness, comorbid conditions, and general health status of the patient.3,4 However, mortality rate specific to AEN itself is roughly about 6%.3
The management of AEN is geared toward treating the underlying illness and comorbid conditions. The contemporary recommendations include: NPO setting, intravenous hydration, analgesia, total parenteral nutrition, antacids (proton pump inhibitors and histamine receptor-2 inhibitors), and packed red blood cell units (as needed). The role of prophylactic antibiotics is debatable. Surgical intervention is largely reserved for patients with complicated AEN such as perforated esophagus with consequential mediastinitis, mediastinal abscess development, or massive esophageal hemorrhage.4
REFERENCES
- 1.Grudell AB, Mueller PS, Viggiano TR. Black esophagus: report of six cases and review of the literature, 1963–2003. Dis Esophagus. 2006;19:105–10. doi: 10.1111/j.1442-2050.2006.00549.x. [DOI] [PubMed] [Google Scholar]
- 2.Ben Soussan E, Savoye G, Hochain P, Hervé S, Antonietti M, Lemoine F, et al. Acute esophageal necrosis: a 1-year prospective study. Gastrointest Endosc. 2002;56:213–7. doi: 10.1016/s0016-5107(02)70180-6. [DOI] [PubMed] [Google Scholar]
- 3.Gurvits GE, Shapsis A, Lau N, Gualtieri N, Robilotti JG. Acute esophageal necrosis: a rare syndrome. J Gastroenterol. 2007;42:29–38. doi: 10.1007/s00535-006-1974-z. [DOI] [PubMed] [Google Scholar]
- 4.Gurvits GE. Black esophagus: acute esophageal necrosis syndrome. World J Gastroenterol. 2010;16:3219–25. doi: 10.3748/wjg.v16.i26.3219. [DOI] [PMC free article] [PubMed] [Google Scholar]