Abstract
BACKGROUND
Despite the extensive reporting of pediatric ulcerative colitis (UC) from industrialized developed countries, reports from developing countries are limited to small-case series from single centers. The objective of our large multicenter study was to determine the clinical, laboratory, endoscopic characteristics of UC in children from a developing country, Saudi Arabia.
DESIGN AND SETTINGS
A retrospective study of children diagnosed with UC under the age of 18 years during the period from 2003 to 2012.
METHODS
Patients enrolled from 15 medical centers from different regions in Saudi Arabia. A unified database collection form specifically designed for this study was completed by all participating centers.
RESULTS
A total of 188 children were diagnosed with UC during the study period (97 males [51.6%] and 91 females [48.4%]). The mean age at diagnosis was 9.1 years, and the mean duration of symptoms before diagnosis was 8.7 months. Consanguinity was present in 57 cases (32.6%), and the family history of inflammatory bowel disease (IBD) was noted in 16 cases (9%). The most common clinical presentation was blood in stool (90%), followed by diarrhea (86%) and abdominal pain (62%). Laboratory investigations revealed elevated erythrocyte sedimentation rate (82%), anemia (75%), thrombocytosis (72%), and hypoalbuminemia (33%). The extent of the disease was pan colonic in 46.1%, and confined to left side of colon and rectum in 23% and 9.6% of the cases, respectively.
CONCLUSION
This demographically pediatric IBD retrospective study revealed age-related variation in the distribution of IBD. Clinical presentation, with a high prevalence of positive consanguinity and positive family history, was noted in young patients with UC. The data from this study indicate that UC is increasingly recognized in Saudi Arabia and show many similarities to data from North America and Europe.
Inflammatory bowel disease (IBD) is a global health care problem with a sustained increasing incidence. It has been extensively reported in Caucasians of the Western world and is most prevalent in developed countries, including the USA and European countries.1–4 Epidemiological and family studies demonstrate that genetic factors play a role in the susceptibility to IBD. There is an increased prevalence of IBD in first- and second-degree relatives and a higher relative risk among siblings.5,6 Current etiologic theories focus not only on environmental and genetic factors, but also on immunoregulatory defects7 and microbial exposure.8 Ulcerative colitis (UC) is a chronic relapsing disease of the colon that is characterized by inflammation and ulceration of the colonic mucosa. The symptoms of UC and possible complications vary depending on the extent of inflammation in the rectum and the colon.
Despite extensive reporting of pediatric UC from industrialized developed countries, reports from developing countries are limited to small case series from single centers.9–16 Therefore, characteristics of pediatric UC have yet to be well documented in developing countries, and it remains to be determined whether the low number of reports and small case series from developing countries reflect true low incidence of pediatric UC or just under-recognition of the disease entity in this part of the world.
This large multicenter retrospective study on pediatric UC was undertaken to clarify the demographic characteristics, clinical spectrum, and endoscopic findings. This report also discusses similarities between pediatric UC in Saudi Arabia and Western countries.
METHODS
This retrospective study of children diagnosed with UC under the age of 18 years during the period from January 1, 2003, to December 31, 2012, at 15 medical centers from different regions in Saudi Arabia. Children with UC were identified by either computerized hospital system using the International Classification of Disease codes of the hospital admissions database, endoscopy, or through personal physician records. A unified database collection form specifically designed for this study was completed by all participating centers and reviewed by gastroenterologists. Demographic data, clinical symptoms, results of laboratory tests (including hemoglobin, erythrocyte sedimentation rate [ESR], and liver function tests), and endoscopic findings were collected from medical records and endoscopic reports at the time of diagnosis and were reviewed carefully to ensure that the final diagnosis was consistent with the published diagnostic criteria4,9 and in accordance with ESPGHAN Porto Criteria.17 In Saudi Arabia, pediatric patients of suspected IBD are referred to gastroenterology centers that are distributed in major cities. These centers are staffed with certified gastroenterologists and equipped with adequate facilities for the investigation and management of IBD. All suspected pediatric IBD cases presenting to any of the centers undergo extensive workup to exclude infectious causes of enteritis or colitis by stool cultures (for Salmonella, Shigella, Yersinia, and Campylobacter) and stool tests for Clostridium difficile, Giardia lamblia, and Entamoeba histolytica (parasites, cysts, and ova).
This report is part of a multicenter collaborative research project entitled “characteristics of IBD in Saudi children,” which has been approved by the Institutional Review Board of the college of medicine (No: 10/2647/IRB) at King Saud University in Riyadh and the local Institutional Review Board in participating centers.
RESULTS
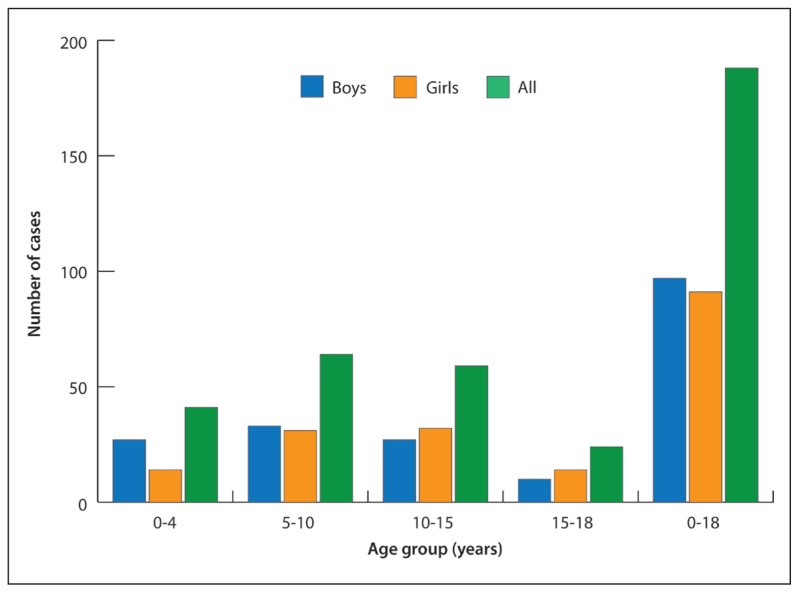
A total of 188 children were diagnosed with UC during the study period. The demographic characteristics of pediatric UC cases are presented in Table 1. Males and females were almost equally affected across all pediatric age groups. However, males were affected twice as females in children below 4 years of age (27 boys vs 14 girls). Out of 188 patients, 167 (89 %) were Saudi; the rest (11%) were from other nationalities.
Table 1.
Demographics of ulcerative colitis.
| Variables | Ulcerative colitis |
|---|---|
|
| |
| Gender: males (%) | 97/188 (51.6%) |
| Age at diagnosis (mo): mean (Min, Max, SD) | 109.4 (4, 215, 55.2) |
| Duration of symptoms (mo): mean (Min, Max, SD) | 8.7 (0.0, 104, 12.3) |
| Positive family history | 16/180 (9%) |
| Positive consanguinity | 57/175 (32.6%) |
Min: Minimum; Max: maximum; SD: standard deviation.
Figure 1 shows the Frequency of UC by age and sex. The patients of this study presented with a combination of gastrointestinal and extra-intestinal symptoms and signs of UC (Table 2). Blood in stools was the most common presenting symptom (90%) followed by diarrhea (86%) and abdominal pain (62%). Only third of the patient had weight loss and anorexia (37% and 32%, respectively). Extra-intestinal manifestation, i.e., arthritis and skin rash were seen only in 2%.
Figure 1.
Frequency of cases by age and sex.
Table 2.
Clinical presentation of 188 children diagnosed with ulcerative colitis.
| Clinical features | Frequency (%) |
|---|---|
|
| |
| Abdominal pain | 117 (62) |
| Diarrhea | 161 (86) |
| Blood in stools | 170 (90) |
| Weight loss | 70 (37) |
| Anorexia | 60 (32) |
| Vomiting | 28 (15) |
| Pallor | 26 (14) |
| Fever | 22 (12) |
| Bloating/flatulence | 9 (5) |
| Nausea | 6 (3) |
| Arthritis | 3 (2) |
| Skin rash | 3 (2) |
The most common laboratory abnormalities (Table 3) were high ESR, followed by anemia, and thrombocytosis in 82%, 75%, and 72%, respectively. Hypoalbuminemia was seen in 33%, and only 28% had leukocytosis. High alanine transferase was noticed in only 6% patients.
Table 3.
Laboratory presenting features of children with UC.
| Test | Number/Total (%) |
|---|---|
|
| |
| Hemoglobin (low ) | 104/139 (75) |
| Hematocrit (low) | 52/71 (73) |
| White blood cells (high) | 27/96 (28) |
| Neutrophils (high) | 11/41 (27) |
| Platelets (high) | 96/133 (72) |
| ESR (high) | 97/118 (82) |
| CRP (high) | 48/76 (63) |
| Serum albumin (low) | 35/106 (33) |
| Alanine transferase (high) | 6/101 (6) |
| Alkaline phosphatase (high) | 7/99 (7) |
UC:Ulcerative colitis; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein.
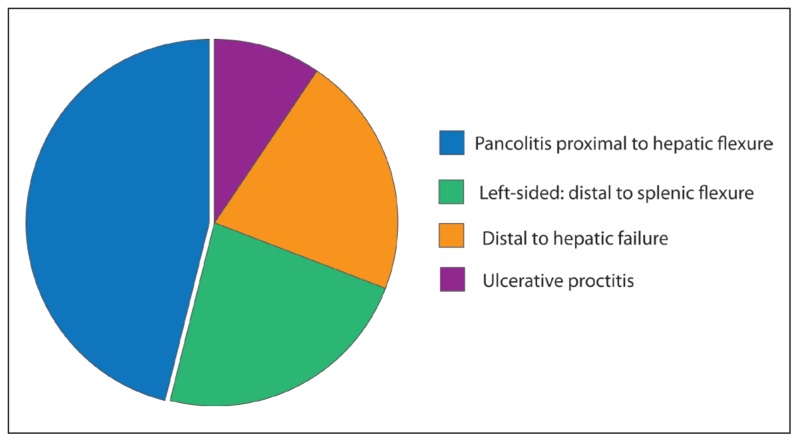
Data on colonic extent were available in 178 (95%) of 188 cases. Figure 2 shows the extent of colonic involvement in 178 patients at diagnosis; almost half of the patients had pancolitis (46.1%) at presentation and 9.6% had ulcerative proctitis.
Figure 2.
Extent of colonic involvement in 178 patients at diagnosis.
DISCUSSION
There are few published reports describing UC in children in the Middle East. Rising incidence of pediatric IBD (both Crohn disease and UC) were noticed in many countries worldwide2,4,18 including Saudi Arabia.19 This study highlights the characteristic features of pediatric UC in Saudi Arabia. The present paper probably reports the largest series describing the characteristics of UC in children from the Middle East.
The pattern of gender distribution with slight male predominance in UC is similar to the reports from other Western countries including the USA.20 However, a significant male predominance was observed in children below 4 years of age as indicated by a 2:1 male-to-female ratio.
A considerable progress has been made in the last decade in the genetics studies of IBDs;5 Familial association of IBD is recognized by many authors, especially in younger patients, with a great variability in the percentage of affected family members.21 Despite the high percentage of consanguineous marriage, 32.6% prevalence found in this study is still lower than the 56% prevalence in the general Saudi population.22 Only 9% positive family history of IBD was reported in this study, which is higher than 6.6% reported by Roma et al23 but lower than the 11% reported from Wisconsin, USA;24 15.3% reported in the central region of Saudi Arabia15 and 31% reported in Kuwait.11 This relatively low prevalence of positive family history in Saudi Arab children with IBD, a population with high prevalence of consanguinity,22 is surprising and provides more support to the current etiologic theories are multifactorial and not only focus on genetic factors but also on environmental triggers,1 immunoregulatory defects,7 and microbial exposure.8 However, this observation requires further investigations.
This report documents the presenting features of pediatric UC in Saudi Arabia, usually diarrhea, which may be associated with blood. The presenting clinical and laboratory features indicate that UC in Saudi children may present at any age as early as 4 months old, and certain clinical and laboratory features are more common than others. These findings are consistent with classical descriptions of pediatric UC in other population,25,26 which may suggest similar disease etiology and pattern. It is worth mentioning that the variation in the numbers of cases for each laboratory test is due to the fact that these patients presented were investigated in many hospitals, and some laboratory tests at presentation were not available.
The implications of this descriptive study are very important, as these help increase the index of suspicion among physicians caring for children in all regions of Saudi Arabia, leading to early diagnosis and treatment of patient with UC.
In conclusion, the presenting features of pediatric UC in Saudi Arabia are similar to descriptions from other populations, suggesting similar disease etiology and pattern. A prospective research is needed to study the role of lifestyle, microbiome, and genetics of UC in this population.
Acknowledgments
The authors extend their appreciation to the Deanship of Scientific Research at King Saud University for funding this work through Research Group No. RG-1436-007.
REFERENCES
- 1.Zhang Yi-Zhen, Li Yong-Yu. Inflammatory bowel disease: Pathogenesis. World J Gastroenterol. 2014 Jan 7;20(1):91–99. doi: 10.3748/wjg.v20.i1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Henderson P, Hansen R, Cameron FL, et al. Rising incidence of pediatric inflammatory bowel disease in Scotland. Inflamm Bowel Dis. 2012;18:999– 1005. doi: 10.1002/ibd.21797. [DOI] [PubMed] [Google Scholar]
- 3.Martín-de-Carpi J, Rodríguez A, Ramos E. Increasing incidence of pediatric inflammatory bowel disease in Spain (1996–2009): the SPIRIT Registry. Inflamm Bowel Dis. 2013 Jan;19(1):73–80. doi: 10.1002/ibd.22980. [DOI] [PubMed] [Google Scholar]
- 4.Malmborg P, Grahnquist L, Lindholm J, et al. Increasing incidence of paediatric inflammatory bowel disease in northern Stockholm County, 2002–2007. J Pediatr Gastroenterol Nutr. 2013 Jul;57(1):29–34. doi: 10.1097/MPG.0b013e31828f21b4. [DOI] [PubMed] [Google Scholar]
- 5.Satsangi J, Morecroft J, Shah NB, et al. Genetics of inflammatory bowel disease: scientific and clinical implications. Best Pract Res Clin Gastroenterol. 2003 Feb;17(1):3–18. doi: 10.1053/bega.2002.0349. [DOI] [PubMed] [Google Scholar]
- 6.Binder V. Genetic epidemiology of inflammatory bowel disease. Dig Dis. 1998 Nov-Dec;16(6):351–5. doi: 10.1159/000016891. [DOI] [PubMed] [Google Scholar]
- 7.Neish AS, Gewirtz AT, Zeng H, et al. Prokaryotic regulation of epithelial responses by inhibition of IkappaB-alpha ubiquitination. Science. 2000 Sep 1;289(5484):1560–3. doi: 10.1126/science.289.5484.1560. [DOI] [PubMed] [Google Scholar]
- 8.Abreu MT. The pathogenesis of inflammatory bowel disease: translational implications for clinicians. Curr Gastroenterol Rep. 2002 Dec;4(6):481–9. doi: 10.1007/s11894-002-0024-0. [DOI] [PubMed] [Google Scholar]
- 9.Treepongkaruna S, Pienvichit P, Sornmayura P, Pornkul R, Wisdopas N, Phuapradit P. Inflammatory bowel disease in Thai children: presentations and outcome of treatment. Asian Pac J Allergy Immunol. 2006;24:73–9. [PubMed] [Google Scholar]
- 10.Ahmaida AI, Al-Shaikhi SA. Childhood Inflammatory Bowel Disease in Libya: Epidemiological and Clinical features. Libyan J Med. 2009 Jun 1;4(2):70–4. doi: 10.4176/081210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Qabandi WA, Buhamrah EK, et al. Inflammatory bowel disease in children, an evolving problem in Kuwait. Saudi J Gastroenterol. 2011 Sep-Oct;17(5):323–7. doi: 10.4103/1319-3767.84487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fallahi GH, Moazzami K, Tabatabaeiyan M, Zamani MM, Asgar-Shirazi M, Najafi M, et al. Clinical characteristics of Iranian pediatric patients with inflammatory bowel disease. Acta Gastroenterologica Belg. 2009;72:230–4. [PubMed] [Google Scholar]
- 13.Shen YM, Wu JF, Chen HL, Hsu HY, Chang MH, Hsieh TK, et al. Characteristics and incidences of pediatric Crohn disease in the decades before and after 2000. Pediatr Neonatol. 2011;52:317–20. doi: 10.1016/j.pedneo.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Avinash B, Dutta AK, Chacko A. Pediatric Inflammatory Bowel Disease in South India (Research letter) Indian Pediatrics. 2009;46:639–40. [PubMed] [Google Scholar]
- 15.El Mouzan MI, Al Mofarreh MA, Assiri AM, et al. Presenting features of childhood-onset inflammatory bowel disease in the central region of Saudi Arabia. Saudi Med J. 2012 Apr;33(4):423–8. [PubMed] [Google Scholar]
- 16.Saadah O. Ulcerative colitis in children and adolescents from the Western region of Saudi Arabia. Saudi Med J. 2011;32:943–7. [PubMed] [Google Scholar]
- 17.Inflammatory bowel disease in children and adolescents: recommendations for diagnosis--the Porto criteria. J Pediatr Gastroenterol Nutr. 2005 Jul;41(1):1–7. doi: 10.1097/01.mpg.0000163736.30261.82. [DOI] [PubMed] [Google Scholar]
- 18.Martín-de-Carpi J, Rodríguez A, Ramos E. Increasing incidence of pediatric inflammatory bowel disease in Spain (1996–2009): the SPIRIT Registry. Inflamm Bowel Dis. 2013 Jan;19(1):73–80. doi: 10.1002/ibd.22980. [DOI] [PubMed] [Google Scholar]
- 19.El Mouzan M, Saadah O, Al-Saleem K, et al. Incidence of pediatric inflammatory bowel disease in Saudi Arabia: a multicenter national study. Inflamm Bowel Dis. 2014 Jun;20(6):1085–90. doi: 10.1097/MIB.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 20.Loftus EV, Jr, Silverstein MD, Sandborn WJ, et al. Ulcerative colitis in Olmsted County, Minnesota, 1940–1993: incidence, prevalence, and survival. Gut. 2000 Mar;46(3):336–43. doi: 10.1136/gut.46.3.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weinstein TA, Levine M, Pettei MJ, Gold DM, Kessler BH, Levine JJ. Age and family history at presentation of pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2003 Nov;37(5):609–13. doi: 10.1097/00005176-200311000-00020. [DOI] [PubMed] [Google Scholar]
- 22.El Mouzan MI, Al Salloum AA, Al Herbish AS, Qurachi MM, Al Omar AA. Regional variation in the prevalence of consanguinity in Saudi Arabia. Saudi Med J. 2007 Dec;28(12):1881–4. [PubMed] [Google Scholar]
- 23.Roma ES, Panayiotou J, Pachoula J, Constantinidou C, Polyzos A, Zellos A, Lagona E, Mantzaris GJ, Syriopoulou VP. Inflammatory bowel disease in children: the role of a positive family history. Eur J Gastroenterol Hepatol. 2010 doi: 10.1097/MEG.0b013e32832e2bd8. [DOI] [PubMed] [Google Scholar]
- 24.Kugathasan S, Judd RH, Hoffmann RG, Heikenen J, Telega G, Khan F, et al. Epidemiologic and clinical characteristics of children with newly diagnosed inflammatory bowel disease in Wisconsin: A statewide population-based study. J Pediatr. 2003 Oct;143(4):525–31. doi: 10.1067/s0022-3476(03)00444-x. [DOI] [PubMed] [Google Scholar]
- 25.Leichtner AM, Higuchi L. Ulcerative colitis. In: Walker WA, Kleinman RE, Sherman PM, Shneider BL, Sanderson IR, editors. Pediatric Gastrointestinal disease. 4th ed. Hamilton (CN): BC Decker Inc; 2004. pp. 825–849. [Google Scholar]
- 26.Sawczenko A, Sandhu B. Presenting features of inflammatory bowel disease in Great Britain and Ireland. Arch Dis Child. 2003 Nov;88(11):995–1000. doi: 10.1136/adc.88.11.995. [DOI] [PMC free article] [PubMed] [Google Scholar]