Abstract
BACKGROUND AND OBJECTIVES
Tissue hypoxia due to repeated apneas among patients of obstructive sleep apnea syndrome (OSAS) leads to cumulative oxidative stress. It is established that an increased plasma level of hypoxanthine/xanthine may serve as a criterion of tissue hypoxia. We presumed that plasma levels of hypoxanthine/xanthine might be high among patients of OSAS due to oxidative stress. Nobody studied this relationship earlier. The aim of this study was to estimate their plasma levels as markers of hypoxia.
DESIGN AND SETTINGS
This case-control study was performed for a period of 1-year including patients referred to a tertiary care hospital, New Delhi, India.
MATERIALS AND METHODS
It was a case-control study. A total of 43 patients of OSAS, diagnosed by overnight polysomnography (PSG), were included in the study. Age- and sex-matched 43 subjects in whom the presence of OSAS was not confirmed by overnight PSG were enrolled as healthy controls. The severity of disease was classified on the basis of apnea-hypopnea index (AHI). Out of 43 patients, 9 were moderate and 14 were severe. None was with mild OSAS. The venous blood sample was collected in the morning after PSG. Hematological and biochemical assays were also performed. Plasma levels of hypoxanthine/xanthine were measured by fluorometric analysis (normal laboratory reference <2.00 mmol/L). Data collected was analyzed statistically by SPSS version 14.0, student unpaired t test, chi-square test, Mann-Whitney U test, and Pearson correlation coefficient.
RESULTS
The mean plasma level of hypoxanthine/xanthine in patients of OSAS was found to be 5.4 (5.1) mmol/L, and in controls it was 1.2 (0.4) mmol/L. A statistically significant (P=.000) difference was found between both groups. Among patients, a positive correlation between hypoxanthine/xanthine levels with age, AHI, and serum triglyceride levels was observed. The joint explanatory power of these significant factors was found to be 59.6% (P<.001).
CONCLUSION
Plasma levels of xanthine/hypoxanthine were significantly elevated in patients of OSAS, and these were positively correlated with age, serum triglyceride levels, AHI, and severity of the disease.
Obstructive sleep apnea syndrome (OSAS) is related to upper airway obstruction that develops during sleep with manifestations including snoring, apneas, and hypopneas. The oxidative stress markers increase in the blood of OSAS patients to a variable degree depending on the severity of the syndrome.1 There is a need of an appropriate biochemical marker to assess this hypoxic-oxidative stress and a reliable way to assess the antioxidant status of the body.
Hypoxanthine and xanthine are products in the pathway of purine degradation. Purine is catabolized through a few intermediates to hypoxanthine that is converted to xanthine, giving rise to uric acid, a final product of purine metabolism in human beings.
Both uric acid and lactate are positively correlated with the degree of hypoxia in OSAS.2 It was observed that an increased blood plasma level of hypoxanthine/xanthine may serve as an additional criterion of tissue hypoxia.3 These extracellular markers of ischemia have been studied in many clinical conditions of oxidative stress, including acute coronary syndromes,4 perinatal asphyxia, acute respiratory distress syndrome, cerebral ischemia, and preeclampsia.5 It is evident that plasma levels of xanthine and hypoxanthine in patients of OSAS will be high. However, this relationship is not probed earlier.
MATERIALS AND METHODS
The institutional academic board and ethical committee approved the study protocol. An informed and written consent was taken from each participant. A detailed history was taken with special emphasis on loud snoring and excessive daytime sleepiness. They were asked to rate the degree of daytime sleepiness according to Epworth Sleepiness scale (ESS) 6 in various situations in day-to-day life. Subjects with psychiatric, neurological, other otorhinolaryngeal, or respiratory disorders were excluded from the study.
Over a year, 88 patients were referred to our tertiary care hospital with the suspicion of OSAS. The diagnosis of OSAS was confirmed by overnight polysomnography (PSG) in 43 patients. Another 43 healthy volunteers in whom the presence of OSAS was ruled out were also included as controls. These subjects were age, sex, and body mass index (BMI) matched with those of patients. Height, weight, waist, and neck circumference and waist/hip ratio (WHR) of all OSAS and control subjects were measured.
Polysomnography
For all subjects, a nocturnal polysomnographic monitoring was performed during sleep for 6 to 8 hours. Sleep monitoring was performed using VIASYS Healthcare Sleep Apnea Screen cardiopolysomnography equipment (VIASYS Healthcare, Germany) in sleep laboratory. PSG recorded central electroencephalogram (C3/A2 and C4/A1), electrooculogram, submental electromyogram, anterior tibialis electromyogram, electrocardiogram (modified lead V2) for cardiac monitoring, continuous pulse oximetry using a finger probe, thoracic and abdominal movements, and oronasal thermistor to measure airflow at the nose and mouth.
Sleep apnea syndrome was defined as more than 5 apneas per hour or 30 apneas per 8 hours of sleep. Apnea was defined as a decrease of inspiratory flow to <20% of waking levels for at least 10 seconds. Hypopnea was defined as a decrease in inspiratory flow to <50% of waking levels. The apnea-hypopnea index (AHI) is derived from the total number of apneas and hypopneas divided by the total sleep time. A normal cutoff for AHI has never been defined. Most sleep centers use a cutoff of 5 to 10 episodes per hour. The severity of OSA is arbitrarily defined and differs widely between centers. Recommendations for cutoff levels on AHI include 5 to 15 episodes per hour for mild, 15 to 30 episodes per hour for moderate, and more than 30 episodes per hour for severe.
Blood sample
The morning after night PSG, 10 mL of fasting peripheral venous blood of all subjects was collected and divided in a plain vial, a fluoride vial, and an EDTA vial. The serum sample and fluoride sample were used for routine biochemical investigations, viz., serum cholesterol, serum triglyceride, and serum fasting blood sugar. The EDTA sample was immediately transported to the genetic laboratory. The sample was centrifuged, and the separated plasma was labeled and stored at −80°C.
Estimation of plasma levels of hypoxanthine/xanthine
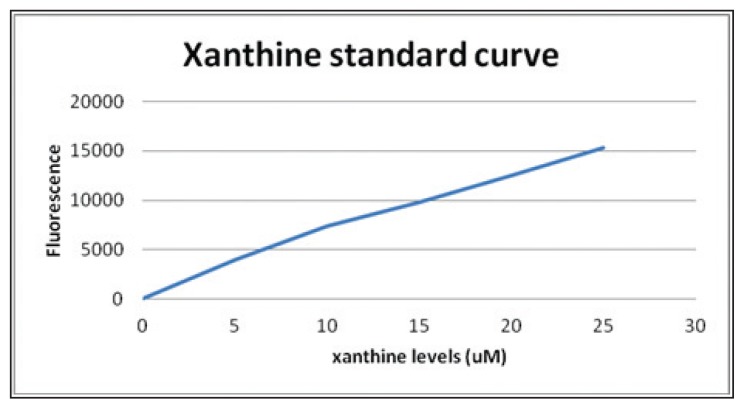
Plasma levels of xanthine and hypoxanthine were measured by fluorometric analysis using a commercially available plate-based assay kit (Invitrogen, United Kingdom) according to the manufacturer’s instructions. Xanthine oxidase catalyzes the oxidation of hypoxanthine or xanthine to O2•−, which spontaneously degrades to H2O2. In the presence of horseradish peroxidase, H2O2 reacts with Amplex Red to generate the red oxidation product, resorufin, which was assayed fluorometrically. A standard curve was plotted by diluting the xanthine provided in the kit in 1X Reaction Buffer to produce concentrations of 0 to 40 μM (Figure 1). The 1X Reaction Buffer without hypoxanthine or xanthine was used as a negative control. The reaction was incubated for 30 minutes or longer at 37°C protected from light. The fluorescence was measured in a microplate reader using excitation in the range of 530–560 nm and emission detection at ~590 nm or absorbance at ~560 nm. Correction for the background fluorescence or absorbance was done by subtracting the value derived from the negative control. The measured value in this assay was a combination of both hypoxanthine and xanthine.
Figure 1.
Xanthine standard curve.
Statistical analysis
The data was analyzed statistically by SPSS version 20. Variables between the OSAS and the control group were compared using student unpaired t test. The P value <.05 was considered to be statistically significant. The correlation between various quantitative variables with hypoxanthine/xanthine levels was assessed using Pearson correlation coefficient. The stepwise regression method was used to find out the significant factors influencing hypoxanthine/xanthine levels. The dependent variable in the regression was hypoxanthine/xanthine level. The independent variables tried in the regression equation were age, ESS, BMI, WHR, neck circumference, mean arterial pressure, serum cholesterol, serum triglyceride, fasting blood glucose, and AHI.
RESULTS
Age and other parameters of patients of OSAS and healthy controls are presented in Table 1. There was statistically no difference between the age and BMI of OSAS and control groups. However, the OSAS group had greater waist circumference, neck circumference, and WHR than the control group. Thus, obesity variables showed that the OSAS group, though matched for BMI, had a greater central fat distribution compared to the control group. The mean arterial blood pressure of the OSAS group was significantly higher than that of the control group (P<.05). There was a statistically significant elevation of serum cholesterol, serum triglyceride, and fasting blood sugar levels in patients of the OSAS group than in the control group. On the basis of AHI, OSAS was moderate in 9 patients and severe in 34 patients. There were no patients of the mild OSAS.
Table 1.
Descriptive statistics and P value of different variables in case (patients) of OSAS and control groups.
| Parameters | Group | Mean | SD | Minimum | Maximum | P value |
|---|---|---|---|---|---|---|
|
| ||||||
| Age (y) | Case | 45.23 | 10.63 | 19 | 70 | .50000 |
| Control | 45.23 | 10.03 | 22 | 66 | ||
| Height (cm) | Case | 157.24 | 8.34 | 142.5 | 173 | .05051 |
| Control | 154.53 | 6.73 | 140 | 170 | ||
| Weight (kg) | Case | 86.90 | 18.26 | 63 | 150 | .08720 |
| Control | 82.02 | 14.51 | 57 | 120 | ||
| BMI (kg/m2) | Case | 35.21 | 7.15 | 26.61 | 57.07 | .33838 |
| Control | 34.55 | 7.30 | 25.39 | 57.07 | ||
| Waist (cm) | Case | 105.19 | 16.04 | 86 | 156 | .00000 |
| Control | 87.63 | 4.34 | 82 | 102 | ||
| Hip (cm) | Case | 103.74 | 14.81 | 80 | 146 | .00000 |
| Control | 88.67 | 3.94 | 83 | 100 | ||
| Waist-hip ratio | Case | 1.01 | 0.06 | 0.90 | 1.19 | .00373 |
| Control | 0.99 | 0.03 | 0.94 | 1.05 | ||
| Neck circumference (cm) | Case | 43.30 | 4.70 | 35 | 58 | .00000 |
| Control | 39.16 | 3.27 | 32 | 45 | ||
| BP - systolic (mm Hg) | Case | 129.98 | 16.02 | 98 | 170 | .00925 |
| Control | 122.07 | 14.47 | 96 | 154 | ||
| BP diastolic (mm Hg) | Case | 83.86 | 10.15 | 66 | 110 | .01098 |
| Control | 79.44 | 7.14 | 60 | 92 | ||
| Mean arterial pressure (mm Hg) | Case | 99.23 | 11.27 | 78 | 130 | .00603 |
| Control | 93.65 | 8.75 | 72 | 110.67 | ||
| Serum cholesterol | Case | 205.81 | 44.70 | 122 | 340 | .00033 |
| Control | 178.05 | 25.47 | 127 | 231.00 | ||
| Serum triglyceride | Case | 171.63 | 45.65 | 88 | 310 | .00144 |
| Control | 146.35 | 28.85 | 93 | 219.00 | ||
| Fasting blood sugar | Case | 112.56 | 28.14 | 79 | 210 | .00415 |
| Control | 99.79 | 12.93 | 72 | 134.00 | ||
| Hypoxanthine/Xanthine levels | Case | 5.38 | 5.11 | 0.4 | 28 | .00000 |
| Control | 1.23 | 0.42 | 0.4 | 1.80 | ||
BP: Blood pressure; BMI: body mass index; OSAS: obstructive sleep apnea syndrome; SD: standard deviation.
The mean plasma level of hypoxanthine/xanthine in patients of the OSAS group was found to be 5.38 (5.11) μM (range from 0.4–28 μM) and that in patients of the control group was found to be 1.23 (0.42) μM (range from 0.4–1.8 μM). The difference between the mean plasma levels of OSAS and control groups was found to be statistically significant (P value .0000).
Among the patients, the correlation analysis of plasma levels of hypoxanthine/xanthine was done with respect to qualitative factors, viz. gender, hypertension, diabetes mellitus, and severity of OSAS. Plasma levels of hypoxanthine/xanthine showed a positive correlation with the severity of OSAS (P<.05). No correlation could be found between hypoxanthine/xanthine levels and gender, or presence of hypertension and diabetes mellitus.
The correlation analysis of hypoxanthine/xanthine levels was done with respect to various quantitative parameters, viz., age, ESS, BMI, WHR, neck circumference, mean arterial blood pressure, serum cholesterol, serum triglyceride, fasting blood sugar, and AHI (Table 2). A statistically significant positive correlation was found between hypoxanthine/xanthine levels and 3 quantitative parameters, viz. age, serum triglyceride, and AHI.
Table 2.
Correlation of plasma levels of hypoxanthine/xanthine in OSAS patients with different quantitative parameters.
| Xanthine and hypoxanthine levels | Coefficient | P value |
|---|---|---|
|
| ||
| Age | 0.320 | .03654 |
| ESS | 0.268 | .08208 |
| BMI | −0.048 | .75980 |
| WHR | 0.257 | .09653 |
| Neck circumference | 0.041 | .79401 |
| MAP | 0.008 | .96057 |
| Serum cholesterol | 0.163 | .29558 |
| Serum triglyceride | 0.414 | .00575 |
| FBS | 0.054 | .73075 |
| AHI | 0.653 | .00000 |
AHI: Apnea-hypopnea index; BMI: body mass index; ESS: Epworth Sleepiness scale; FBS: fasting blood sugar; MAP: mean arterial pressure; OSAS: obstructive sleep apnea syndrome; WHR: waist/hip ratio.
A further regression analysis confirmed the results obtained through the correlation analysis. The joint explanatory power of these significant factors, viz., age, serum triglyceride, and AHI was 59.6%. The coefficients obtained through the regression analysis was interpreted as follows (Table 3): for every 1 year increase in age, plasma levels of hypoxanthine/xanthine increased by 0.115 μM; for every 1 unit rise in serum triglyceride level, the value of hypoxanthine/xanthine levels increased by 0.030 μM, and for every 1 unit increase in AHI, the value of plasma levels of hypoxanthine/xanthine increased by 0.102 μM.
Table 3.
Multivariate regression analysis to determine the factors influencing plasma levels of hypoxanthine/xanthine in patients with OSAS.
| Variable (s) | Unstandardized coefficients | Standard error | Standardized coefficients | t | P value |
|---|---|---|---|---|---|
|
| |||||
| Constant | −1.038 | 1.306 | 0.653 | −0.795 | .431 |
| AHI | 0.107 | 0.019 | 5.525 | .000 | |
| Constant | −7.267 | 2.273 | −3.197 | .003 | |
| AHI | 0.100 | 0.018 | 0.614 | 5.714 | .000 |
| Serum triglyceride | 0.039 | 0.012 | 0.344 | 3.205 | .003 |
| Constant | −11.159 | 2.776 | −4.020 | .000 | |
| AHI | 0.102 | 0.017 | 0.623 | 6.076 | .000 |
| Serum triglyceride | 0.030 | 0.012 | 0.272 | 2.529 | .016 |
| Age | 0.115 | 0.051 | 0.239 | 2.243 | .031 |
AHI: Apnea-hypopnea index; OSAS: obstructive sleep apnea syndrome.
DISCUSSION
There are reasons to investigate the role of hypoxanthine/xanthine oxidase as a marker of tissue hypoxia in OSAS. First, the xanthine oxidase activity increased by hypoxia and by various cytokines such as tumor necrosis factor-α (TNF-α).7 Since patients with OSAS experience frequent hypoxic episodes during sleep, TNF-α concentrations elevated in patients with OSAS;8 xanthine oxidase activity may also be increased in patients with OSAS. It was demonstrated that two weeks of xanthine oxidase inhibition improved flow-mediated dilation in the brachial arteries of patients with OSAS, suggesting that xanthine oxidase plays a role in vascular impairments caused by OSAS.9
Obesity, dyslipidemia, and sedentary lifestyle are common risk factors for both OSAS and cardiovascular diseases. Moreover, in OSAS, hypoxemia and retention of CO2 (both of which activate the chemoreflexes) as well as abrupt changes in intrathoracic pressure and arousal from sleep occur. This results in acute hemodynamic consequences of obstructive apnea that include sympathetic-mediated vasoconstriction and consequent increase in blood pressure. In this study also, the mean blood pressures (systolic, diastolic, and mean arterial pressure) in the control group were found to be significantly higher than in patients of OSAS that corroborates previous studies.10 The interrelationship between OSAS and dyslipidemia has been observed.11 In this study also fasting levels of serum cholesterol and serum triglycerides significantly elevated in patients of OSAS (P<.05).
Studies have provided evidence supporting an in crease of oxidative stress in OSAS.1,12,13 It has been postulated that one potential source of OSAS-induced oxidative stress in vascular endothelium is the cytosolic and membrane-bound enzyme xanthine oxidase. Superoxide anions generated by this enzyme could limit nitric oxide bioavailability, thereby impairing endothelium-dependent vasodilatation and contribute to vascular remodeling. It has been demonstrated that an increased blood plasma level of hypoxanthine/xanthine might serve as an important criterion of tissue hypoxia.3
Hypoxanthine/xanthine is catabolized by xanthine oxidase to uric acid. In this study, fluorometric principle was used to measure the plasma level of hypoxanthine/xanthine. The fluorometer assayed the enzyme activity that reflected the level of both hypoxanthine and xanthine. The hypoxanthine could not be separated from xanthine, as both are catabolized by xanthine oxidase to uric acid. The measured value in this assay is a combination of both. The inability to separate them is less critical when one is evaluating tissue injury caused by oxygen radical formation because both metabolites are involved in hypoxic injury.
Previous studies14 have shown a positive correlation of xanthine oxidase activity with age, sex, and obesity. To avoid the effect of these confounding factors, a control group was selected, which was age, sex, and obesity matched. In this study, the mean level of serum hypoxanthine/xanthine was found to be higher in the OSAS patients than in the control group (P=.00). This suggested that these metabolites (hypoxanthine/xanthine) in the plasma of OSAS patients denote tissue hypoxia.
Further analysis was done to determine the effect of various quantitative factors on plasma levels of hypoxanthine/xanthine in the OSAS group. Only the patients of the OSAS group were analyzed. A significant positive correlation between plasma levels of hypoxanthine/xanthine with age, serum triglyceride levels, and AHI levels was found. The previous studies did reveal a positive correlation between xanthine and hypoxanthine levels with age and dyslipidemia.15,16 Present studies showed a positive correlation between hypoxanthine/xanthine with AHI; this observation signified the fact that the hypoxanthine/xanthine level increased with the severity of the disease. The results of stepwise regression analysis revealed that AHI was the most important factor influencing hypoxanthine/xanthine plasma levels. The other significant factors influencing hypoxanthine/xanthine levels were serum triglyceride and age.
It was concluded that plasma levels of hypoxanthine/xanthine significantly elevated in patients of OSAS; and they were positively correlated with the severity of OSAS. The oxidative stress markers increase in the blood of OSAS patients to a variable degree, depending on the severity of the syndrome and, therefore, may be suitable for a clinical follow-up of such patients. A positive correlation between hypoxanthine/xanthine levels with age and serum triglyceride levels did exist.
REFERENCES
- 1.Cofta S, Wysocka E, Piorunek T, Rzymkowska M, Gabrye BH, Torlinski L. Oxidative stress markers in the blood of persons with different stages of obstructive sleep apnea syndrome. Journal of Physiology and Pharmacology. 2008;59:183–90. [PubMed] [Google Scholar]
- 2.Hira HS, Shukla A, Kaur A, Kapoor S. Serum uric acid and lactate levels among patients with obstructive sleep apnea syndrome: which is a better marker of hypoxemia? Annals of Saudi Medicine. 2011;32:37–42. doi: 10.5144/0256-4947.2012.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Riabov GA, Ladygin SS, Azizov IuM. The concentration of end products of purine metabolism as possible signs of tissue hypoxia in critically ill surgical patients. Anesteziol Reanimatol. 1993;4:41–3. [PubMed] [Google Scholar]
- 4.Turgan N, Boydak B, Habif S, Gutter C, Senol B, Mutaf I, Ozmen D, Bayindir O. Urinary hypoxanthine and xanthine levels in acute coronary syndromes. Int J Clin Lab Res. 1999;29:162–5. doi: 10.1007/s005990050084. [DOI] [PubMed] [Google Scholar]
- 5.Quinlan GJ, Lamb NJ, Tilley R, Evans TW, Gutteridge JM. Plasma hypoxanthine levels in ARDS: implications for oxidative stress, morbidity mortality. Am J Respir Crit Care Med. 1997;155:479–84. doi: 10.1164/ajrccm.155.2.9032182. [DOI] [PubMed] [Google Scholar]
- 6.Johns MW. Daytime sleepiness, snoring and obstructive sleep apnea: The Epworth Sleepiness Scale. Chest. 1993;103:30–6. doi: 10.1378/chest.103.1.30. [DOI] [PubMed] [Google Scholar]
- 7.Hassoun PM, Feng-Sheng Y, Cote CG, Zulueta JJ, Sawhney R, Skinner KA, Skinner HB, Parks DA, Lanzillo JJ, Skinner HB, Parks DA, Lanzillo JJ. Upregulation of xanthine oxidase by lipo-polysaccharide, interleukin-1 and hypoxia. Role in acute lung injury. Am J Respir Crit Care Med. 1998;1998;158:299–305. doi: 10.1164/ajrccm.158.1.9709116. [DOI] [PubMed] [Google Scholar]
- 8.Vgontzas AN, Papanicolaou DA, Bixler EO, Hopper K, Lotsikas A, Lin HM, Kales A, Chrousos GP. Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance and hypercytokinemia. J Clin Endocrinol Metab. 2000;85:1151–8. doi: 10.1210/jcem.85.3.6484. [DOI] [PubMed] [Google Scholar]
- 9.Johns MW. Daytime sleepiness, snoring and obstructive sleep apnea: The Epworth Sleepiness Scale. Chest. 1993;103:30–6. doi: 10.1378/chest.103.1.30. [DOI] [PubMed] [Google Scholar]
- 10.El Sohl AA, Saliba R, Bosinki T, Grant BJ, Berbary E, Miller N. Allopurinol improves endothelial function in sleep apnea: a randomized controlled study. Eur Respir J. 2007;29:216–7. doi: 10.1183/09031936.06.00101005. [DOI] [PubMed] [Google Scholar]
- 11.Shamsuzzaman ASM, Gersh BJ, Somers VK. Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA. 2003;290:1906–14. doi: 10.1001/jama.290.14.1906. [DOI] [PubMed] [Google Scholar]
- 12.Strobel RJ, Rosen RC. Obesity and weight loss in obstructive sleep apnea: a critical review. Sleep. 1996;19:104–15. doi: 10.1093/sleep/19.2.104. [DOI] [PubMed] [Google Scholar]
- 13.Barcelo AF, Barbe M, de la Pena M. Antioxidant status in patients with sleep apnea and impact of continuous positive airway pressure treatment. Eur Respir J. 2006;27:756–60. doi: 10.1183/09031936.06.00067605. [DOI] [PubMed] [Google Scholar]
- 14.Jabs CM, Neglen P, Eldof B, Thomas EJ. Adenosine, inosine and hypoxanthine/xanthine measured in tissue and plasma by a luminescence method. Clin Chem. 1990;36:81–7. [PubMed] [Google Scholar]
- 15.Aranda R, Doménech E, Rus AD, Real JT, Sastre J, Viña J. Age-related increase in xanthine oxidase activity in human plasma and rat tissues. Free Radic Res. 2007;41:1195–200. doi: 10.1080/10715760701481461. [DOI] [PubMed] [Google Scholar]
- 16.Chiney MS, Schwarzenberg SJ, Johnson LA. Altered xanthine oxidase and N-acetyltransferase activity in obese children. Br J Clin Pharmacol. 2011;72:109–15. doi: 10.1111/j.1365-2125.2011.03959.x. [DOI] [PMC free article] [PubMed] [Google Scholar]