Abstract
Postoperative patient handovers are fraught with technical and communication errors and may negatively impact patient safety. We systematically reviewed the literature on handover of care from the operating room to postanesthesia or intensive care units and summarized process and communication recommendations based on these findings. From >500 papers, we identified 31 dealing with postoperative handovers. Twenty-four included recommendations for structuring the handover process or information transfer. Several recommendations were broadly supported, including (1) standardize processes (e.g., through the use of checklists and protocols); (2) complete urgent clinical tasks before the information transfer; (3) allow only patient-specific discussions during verbal handovers; (4) require that all relevant team members be present; and (5) provide training in team skills and communication. Only 4 of the studies developed an intervention and formally assessed its impact on different process measures. All 4 interventions improved metrics of effectiveness, efficiency, and perceived teamwork. Most of the papers were cross-sectional studies that identified barriers to safe, effective postoperative handovers including the incomplete transfer of information and other communication issues, inconsistent or incomplete teams, absent or inefficient execution of clinical tasks, and poor standardization. An association between poor-quality handovers and adverse events was also demonstrated. More innovative research is needed to define optimal patient handovers and to determine the effect of handover quality on patient outcomes.
Patient handovers, defined as “the transfer of information and professional responsibility and accountability between individuals and teams,”1 are high-risk, error-prone patient care episodes.2,3 Handover failures are common and can lead to diagnostic and therapeutic delays and precipitate adverse events.4–8 The transfer of care after surgery to the postanesthesia care unit (PACU) or intensive care unit (ICU) presents special challenges to providers on both the delivering and receiving teams. The operating room (OR) anesthesia and surgical team is charged with transporting the patient, along with clinical and monitoring equipment, from the OR to the receiving unit, while simultaneously monitoring and performing additional therapeutic tasks such as manual ventilation. Upon arrival at the receiving unit, the technology and support are transferred to local systems while knowledge of the patient gained by the OR team during the procedure is transmitted, in an environment that is often chaotic and busy, to a team largely unfamiliar with the patient. This knowledge transfer involves cross-disciplinary staff with varied experience; the delivering team members with their diverse yet important perspectives of the course of surgery; and the receiving team concurrently stabilizing, assessing, and making care plans for the patient.
It is not surprising, under these circumstances, that postoperative handovers are rife with technical and communication errors.7,9,10 Several studies also point to a relationship between handovers and patient outcomes.11–13 As recognition of the risks inherent to patient handovers has grown, increasing attention has focused on this process of care. In light of this interest, it is important to characterize current practices in postoperative handovers and to identify evidence-based methods to improve them. The goal of this study was to present a review of the literature on this topic and to summarize process and communication recommendations based on its findings.
METHODS
A search was conducted using the PubMed and ProQuest databases with the terms handover, handoff, and patient transfer and combinations of each term with the terms postoperative, anesthesia, postanesthesia, surgery, operating room, ICU, critical care, intensive care, surgical intensive care, admission, communication, and team. Other information sources included the Agency for Healthcare Research and Quality Collection on Discontinuities, Gaps, and Hand-Off Problemsa and handover-related literature reviews.14–18 More than 500 papers were identified. All titles were reviewed for possible inclusion and, for those that were deemed relevant, the abstracts were examined to ensure relevance. Reference sections of papers that met inclusion criteria were scrutinized for additional sources. All papers that addressed patient transfers from the OR to the PACU or ICU were included in the literature review. Papers on other handover types, e.g., work shift changes, and those discussing transfers not originating in the OR were excluded.
Papers included in this review were classified into 1 of 4 categories as proposed by Wong et al.16:
Category 1: Comprehensive intervention-based study— Clear articulation of entire approach to improve clinical handover covering data collection, intervention design, implementation and evaluation, and insights into lessons learned. High level of potential transferability.
Category 2: Intervention-based study—Approach to clinical handover improvement intervention that is not comprehensive or is limited in depth/clarity. Medium to low level of potential transferability.
Category 3: Preintervention study—Studies variously engaging in data collection, analysis, and evaluation to investigate different aspects of clinical handover. Focused on enhancing understanding, identifying gaps and challenges, or the utility of particular research approaches. Some studies provide recommendations for change management, handover improvement interventions, or system reform. High to low level of potential transferability.
Category 4: Published opinions or reviews—Publications not involving any primary research and often not peer reviewed. Can provide potentially useful perspectives on different aspects of clinical handover including high-risk scenarios, evidence gaps, and factors imposing limitations on sustainability or transferability of handover initiatives.
RESULTS
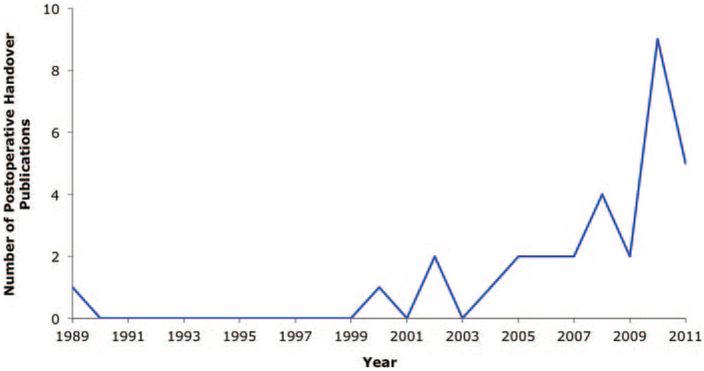
Thirty-one articles met the inclusion criteria. Twenty-four included recommendations for structuring the handover process or information transfer. Of these, 14 supported the proposed solutions with some level of evidence. Only 4 papers described comprehensive intervention-based studies (category 1). Five additional studies described handover training initiatives and the creation of printed or electronic postoperative reports, with limited evaluation of their efforts (category 2). There are 18 cross-sectional studies characterizing current postsurgery handover practices (category 3). All papers were published in 2000 or later with the exception of a 1989 paper listing information needed by the PACU nurse receiving new patients.19 Fourteen were published in 2010 or later (Fig. 1). The papers are presented in Table 1
Figure 1.
Number of journal articles dealing with postoperative handovers by year.
Table 1.
Postoperative Handover Papers Included in the Review.
| Authors | Categorya | Methods | Results | Information content recommendationsb |
Process recommendationsb |
|---|---|---|---|---|---|
| Amato-Vealey et al. (2008)54 | 4 | Recommendations for operationalizing SBAR in the perioperative environment, including information that should be communicated to the PACU nurse | — | P | P |
| Anwari (2002)23 | 3 | After 276 handovers, PACU nurses were surveyed regarding the quality of verbal information, patient condition on admission, the professional behavior of the anesthetist, and the nurse’s satisfaction with the handover | Nurses reported many missing pieces of information. 24% of handovers were rated as “bad” | P | P |
| Beckmann et al. (2004)13 | 3 | Cross-sectional analysis of incident reports relating to the intrahospital transfer of critically ill patients | The majority of incidents (36%) involved OR-to-ICU or ICU-to-OR transportation | R | |
| Botti et al. (2009)55 | 4 | A framework of methods to measure and promote clinical governance, clinician engagement, ecological validity, safety culture and team climate, and sustainability in the context of handovers to the PACU | — | ||
| Catchpole et al. (2007)10 | 1 | Redesign of handovers of pediatric cardiac patients from OR to ICU. A handover protocol and information transfer checklist were developed based on discussions with Formula 1 racing team and aviation training captains | The intervention reduced the number of technical errors and information omissions | R | R |
| Catchpole et al. (2010)56 | 3 | Interviews with Formula 1 racing teams and clinicians involved in postoperative handovers to compare work practices | Deficiencies in proactive prevention, active handover management, and learning from error analysis were identified in health care practice | P | |
| Chen et al. (2010)57 | 2 | Description of 2 simulation scenarios for handing over pediatric cardiac patients from OR to ICU | Positive comments from simulation participants | P | |
| Chen et al. (2011)30 | 3 | Three years after implementation of a protocol to standardize postoperative handovers to a pediatric cardiac ICU, observed practice was compared with protocol guidelines | Attendance of required providers was high. Only 53% of required content items were reported, but other relevant information was often reported. A mean of 2.3 distractions per minute of communication was noted, more than half of which were not essential to patient care. | P | P |
| Clancy (2008)3 | 3 | Description of a study to improve handovers to the PACU using simulation-based training | — | ||
| Currey et al. (2006)52 | 3 | Interviews with ICU nurses regarding perceptions of assuming responsibility for patient care, after observation of their admission of cardiac surgical patients | Nurses who perceived receiving patients to be a positive challenge used handovers to identify decision points. Nurses who were daunted by this process used them to gather information about patient hemodynamic status, likely trajectories, and management priorities | R | |
| de Leval et al. (2000)4 | 3 | Cross-sectional study of major and minor events associated with arterial switch operations | Examples of events that occurred during transfer to the ICU include incorrect interpretation of serious patient deterioration, communication problems during handover, lack of seniority in OR or ICU teams, and prolonged absence of monitoring | ||
| Entin et al. (2006)28 | 4 | A research agenda for investigating the impact of team training on perioperative patient safety. Includes a brief discussion of postoperative handovers | In handover observations, lack of consistency and organization was noted during information transfer. Important information was sometimes omitted, undetected | ||
| Greenberg et al. (2007)12 | 3 | An analysis of surgical malpractice claims that involved communication failures | At least 43% of claims were associated with handovers and 39% were associated with patient transfers | R | |
| Joy et al. (2011)21 | 1 | Development of a protocol and anesthesia information transfer template to standardize postsurgical patient transfer to the pediatric cardiac ICU, based on FMEA and root cause analyses | The intervention led to a reduction in technical errors, information omissions, time to transfer central venous pressure monitoring, and time to definitively secure the endotracheal tube. Perceptions of teamwork and received information improved | R | R |
| Kim et al. (2012)33 | 2 | Development of a protocol and electronic checklist to reduce communication errors during transfer of care of postoperative pediatric airway patients | Of 33 patients, 2 experienced adverse events preintervention. Postintervention, of 93 patients, none experienced adverse events. Anecdotal evidence of increased efficiency | P | P |
| Kluger and Bullock (2002)11 | 3 | An analysis of incident reports relating to the PACU | Poor communication was the second most common contributing factor, associated with 14% of incidents | ||
| Manser et al. (2010)32 | 3 | Development and validation of a handover rating tool assessing technical and nontechnical skills. Validation included ratings of OR to PACU handovers | Three concepts were found to be of importance during handovers: information transfer, shared understanding, and working atmosphere | R | R |
| Mazzocco et al. (2009)6 | 3 | The teamwork of surgical teams was scored for the induction, intraoperative, and handover phases; patients’ 30-day outcomes were documented | Patients whose teams exhibited less briefing and information sharing during the handover were at higher risk for complications or death | R | R |
| McQueen-Shadfar and Taekman (2010)58 | 2 | Description of a simulation scenario for handing over a pediatric patient from OR to PACU using the I PASS the BATON mnemonic | — | P | |
| Meyer-Bender45 | 2 | Generation of printed reports from an anesthesia information management system for postoperative handovers, among other uses | Anecdotal evidence of good acceptance by users | P | |
| Mistry et al. (2005)7 | 3 | Assessed the prevalence of missing or inaccurate information during handover of patients to the pediatric ICU postsurgery | Miscommunication occurred in 100% of handovers. In 94% of cases, there was >1 error | ||
| Mistry et al. (2008)22 | 1 | A Six Sigma methodology was used to improve handover of cardiac patients to the pediatric ICU. The intervention included a handover protocol and team training | The intervention reduced handover and lab draw times and increased the percentage of chest radiographs completed and patients placed on monitors within 3 min | R | |
| Nagpal et al. (2010a)25 | 3 | Development of a checklist of information to be communicated during handover to the recovery room using interviews and the Delphi consensus building method | Handovers were characterized by fragmented information transferred by an incomplete team. Handover effectiveness was highly variable. A 21-item checklist was developed | R | R |
| Nagpal et al. (2010b)26 | 3 | An examination of perioperative communication using HFMEA | One of the critical failures identified deals with incomplete or inaccurate handovers to recovery. Authors recommend a debrief in the OR in the presence of the recovery nurse and use of an information transfer checklist | R | |
| Nagpal et al. (2010c)27 | 3 | HFMEA and interviews were used to develop ITCAS, an observational tool for assessing perioperative communication | Only 56% of essential information was transferred to the recovery suite. Two incidents were observed related to information omission | R | R |
| Nagpal et al. (2011)9 | 3 | Development and assessment of the validity, reliability, and feasibility of PoHAT, an observational tool for evaluating postoperative handovers | There were 9.1 information omissions and 2.9 task errors per handover. Distractions occurred in 35% of handovers and correlated with information omissions | R | R |
| Nestel et al. (2005)59 | 2 | Handover training was developed for “perioperative specialist practitioners” who deliver care before and after surgery and transmit patient information to surgeons and anesthetists | Trainees gave positive feedback related to the training intervention | P | |
| Smith et al. (2008)24 | 3 | A qualitative description of handovers to the recovery room based on observations and interviews | Handovers showed inherent professional and organizational tensions. Standardization efforts should recognize these factors | ||
| Smith and Mishra (2010)31 | 3 | A qualitative description of postoperative handovers based on observations and interviews | Handovers showed inherent professional and organizational tensions. Authors make recommendations for standardizing the process | P | R |
| Welter and Reiff (1989)19 | 4 | A checklist of information to be provided to the PACU nurse at handover | — | P | P |
| Zavalkoff et al. (2011)20 | 1 | Development of an information checklist to standardize postsurgical patient transfers to the pediatric cardiac ICU, based on interviews with stakeholders | The medical, surgical, and total handover scores improved after implementation of the handover tool. No change in the current status and preoperative scores, handover duration, and high-risk events | R |
SBAR = Situation, Background, Assessment, Recommendation. A mnemonic for conveying patient information; PACU = postanesthesia care unit; OR = operating room; ICU = intensive care unit; FMEA = Failure Modes and Effects Analysis; I PASS the BATON = Introduction, Patient, Assessment, Situation, Safety concerns, Background, Actions, Timing, Ownership, Next. A mnemonic for conveying patient information; HFMEA = Healthcare Failure Modes and Effects Analysis; ITCAS = Information Transfer and Communication Assessment Tool for Surgery; PoHAT = Postoperative Handover Assessment Tool.
Categories represent the type of journal article16:
• Category 1: Comprehensive intervention-based study
• Category 2: Intervention-based study
• Category 3: Preintervention study
• Category 4: Published opinions or reviews
P = recommendations provided without any supporting empirical data; R = recommendations provided and supported by at least some empirical data.
As stated earlier, 4 of the studies developed an intervention and formally assessed its impact on process measures during handovers.10,20–22 The interventions involved various combinations of a handover protocol to structure tasks and processes, an information transfer checklist to standardize communication, and team training. Different methods were used to develop them. A Six Sigma approach was adopted in 1 study in which 3 barriers to safe handovers were identified: (1) inconsistent participation of clinicians from the delivering team in information exchange; (2) poor standardization of content and processes; and (3) the presence of interruptions and distractions. A protocol was developed to address these and other issues that were found to lead to frequent communication errors.22 In another study, a protocol for handover of surgical patients was developed based on analogs drawn between postoperative patient handovers and other multiprofessional safety-critical processes, namely, racing team pit stops and aviation training. A checklist was created for the surgeon, anesthesiologist, and receiving ICU team to ensure that important patient information was communicated.10 Two additional studies relied on outcomes of a Failure Modes and Effects Analysis and small-scale root cause analyses21 and on interviews with expert care providers20 to develop handover protocols and checklists. Interestingly, all 4 comprehensive intervention-based papers analyzed the same study population, pediatric cardiac patients. They all improved metrics of effectiveness (decreased technical errors and information omissions), efficiency (reduced handover duration or time to complete specific tasks), and perceived teamwork. However, the interventions did not significantly reduce high-risk events20 or realized errors.21 Their effects on patient outcomes were not evaluated.
Most of the papers provided quantitative or qualitative descriptions of current postsurgical care transfers. These cross-sectional studies present evidence of the many errors and deficiencies associated with handovers, their impact on patient safety, and the effect of handover practices on the work of care providers. Although most papers examined only 1 or 2 care settings, it is striking to note that many of their findings are consistently observed across multiple sites. Common barriers to safe, effective postoperative handovers include the incomplete transfer of information,7,9,10,20,22–30 other communication issues (e.g., inaccurate information, lack of consistency and organization, information overload),4,6,7,11,22,25,28 distractions (including performing clinical activities during the transfer of information),9,22,24–26,30,31 inconsistent or incomplete teams,22,25 absent or inefficient execution of clinical tasks,4,9,10,21 and poor standardization.22,25,26
These barriers, and poor communication in particular, may affect patient outcomes. A study of surgical malpractice claims involving communication failures that resulted in patient harm found the transfer of care to be particularly vulnerable to breakdowns. At least 43% of communication breakdowns were associated with handovers, and 39% were associated with physical patient transfers.12 In an analysis of incidents related to the intrahospital transfer of ICU patients, 36% of events involved the OR as the origin or destination of transport.13 In PACUs, the second most common factor contributing to reported incidents was poor communication, associated with 14% of incidents.11 Finally, postoperative patients were found to be at higher risk for complications or death when their surgical teams exhibited less briefing and information sharing during handover.6 Although these findings do not establish a cause-and-effect relationship between poor handovers and decreased patient safety, they imply an association that warrants a more in-depth examination of postoperative transfer of care.
A number of authors developed tools to measure handover quality, e.g., for the purpose of evaluating the effectiveness of interventions. These tools are largely focused on information transfer,9,10,20,21,23,27,32 but some also assess clinical task performance,9,10,21,23 nontechnical skills,6,9,32 and nursing satisfaction with handover quality.23 Most tools are observational and involve assessing whether certain pieces of information have been transferred or tasks have been executed. The extent to which their validity and reliability have been evaluated is variable.
Many of the papers included in this literature review recommend strategies for facilitating the different phases of postsurgical handovers and for quality improvement. A complete list is shown in Appendix 1. Some of these strategies are supported by quantitative and/or qualitative data and are repeatedly identified as important by several authors. They are presented in Table 2. Similarly, suggestions for patient information to be included in verbal or written handovers are outlined in Appendix 2 and those that are supported most extensively are summarized in Table 3.
Table 2.
Strategies for Safe and Effective Postoperative Handovers Consistently Identified in the Literature
| •Prepare monitor, alarms, equipment, and fluids before patient arrival •Complete urgent care tasks before the verbal handover •Set aside time for handover communication. Avoid performing other tasks during this time and, conversely, limit conversations while performing tasks •Use the “sterile cockpit”—only patient-specific conversation or urgent clinical interruptions can occur during the handover •All relevant members of the operating room and postoperative receiving teams should be present during the handover •Only 1 care provider should speak at a time, with minimal distractions and interruptions •Provide an opportunity to ask questions and voice concerns •Document the handover •Use supporting documentation, e.g., lab test results, anesthesia chart •Use structured checklists to guide communication and ensure completeness of information. Use forms or reference cards as reminders •Use protocols to standardize processes •Provide formal team or handover training |
Table 3.
Postoperative Information Transfer Recommendations consistently Identified in the Literature
| Patient information |
|---|
| •Name •Age •Weight •Allergies •Diagnosis •Procedure performed •Condition •Medical history Anesthesia information •Type of anesthesia and anesthetic course •Anesthesia complications •Intraoperative medications, including dose and time •IV fluids administered •Blood products (type and amount) •Estimated blood loss •Transesophageal echocardiography/echocardiogram report Surgical information •Surgical course •Surgical site information, including dressings, tubes, drains, and packing •Surgical complications and interventions •Cardiopulmonary bypass (CPB)/circulatory arrest/cross-clamp/other procedure durations •Problems weaning from CPB Current status •Assessment of hemodynamic stability Care plan •Anticipated recovery and problems •Clear postoperative management plan •Postoperative orders and investigations •Monitoring plan and range for physiological variables •Analgesia plan •Plan for IV fluids, antibiotics, medications, deep venous thrombosis prophylaxis •Plan for nasogastric tube and feeding |
DISCUSSION
Our review of the literature on patient and knowledge transfers after surgery reveals that research in this area is still in its infancy. Although many studies examine current handover practices from various perspectives, few have tested approaches for improving them. These intervention-based studies suffer from small sample sizes (between 31 and 171 handovers, pre- and postintervention combined) and insufficient details about the solutions or methods used to evaluate them. Furthermore, they all focus on 1 study population, pediatric patients undergoing cardiac surgery. The perioperative and recovery teams caring for this patient population are typically small, consistent, and highly specialized, while the patients are often characterized by high complexity regarding invasive monitoring, IV vasoactive infusions, assisted ventilation, etc. Thus, the generaliz-ability of the approach described in these studies is limited. In addition, no rigorous experimental designs (e.g., with randomized group assignments) have been performed to isolate the effects of interventions from extraneous factors. Perhaps more importantly, we identified only 1 study that attempted to assess the impact of an intervention (handover protocol and checklist) on patient outcomes,33 and this study was not sufficiently powered or adequately designed and analyzed to conclusively document an improvement in outcomes. However, checklists and team training, tools that have been shown to improve handover quality, have face validity, and their effectiveness in reducing patient morbidity and mortality has been demonstrated in other health care activities.34–37 Rigorous study designs, adequate sample sizes, diverse study sites, and assessments of patient outcomes are needed to effectively evaluate approaches to improving postoperative handovers.
Other interesting questions arise regarding patient outcomes. For example, do patients with poor handovers do worse or, conversely, do unstable patients get poor handovers? This question is difficult to answer, and we found no studies that attempted to do so. Those most closely related include an observational study that showed that patients whose surgical teams exhibited less briefing and information sharing were at a higher risk for poor outcomes, even after adjusting for patients’ risk category.6 However, although it is possible that poor information exchange led to complications, the reverse is also possible (e.g., that providers concentrated on emergent patient care needs, rather than communication, during handovers). In another study, Catchpole et al.10 found a positive relationship between patients’ operative risk and information omissions. It is possible that when patients are medically compromised, less information is shared about them. But other factors may also be responsible for omitting important information when handing over high-risk patients (e.g., if a particularly laconic surgeon performs specific procedures in complex patients). One reason why it is important to consider the patient safety implications of deficient handovers is the notion of opportunity cost, or the cost of the handover to providers (time expended), measured in terms of the value of other activities that are foregone to complete it. If we cannot demonstrate that inadequate handovers contribute to poor patient outcomes (or proxy measures of outcomes, such as medication errors), care providers may not recognize the benefit of such resource-intensive recommendations as ensuring the presence of all relevant team members, foregoing other activities during handover communication, and using checklists to guide discussions (Table 2).
Additional research questions regarding the characteristics of a good handover are worthy of attention. For example, what role does provider experience have in communicating important information? It may be that providers who are more experienced (or more familiar with each other’s work practices) are able to communicate more succinctly than, for example, junior trainees, even though the same information is conveyed. Conversely, it is possible that experienced providers, who handover or receive patients on a daily basis, may incorrectly assume certain information (“this anesthesiologist always reverses neuromuscular blocking drugs, even if the reversal drug is not documented in the anesthesia record”) or forget to share or request information. It would be interesting to test the utility of information transfer checklists for providers with different experience levels, with a special focus on the implications of assumptions and unspoken understandings.
In addition, it would be valuable to compare different information delivery methods, e.g., face-to-face, telephone, recorded, written, or electronic. Although verbal, face-to-face postoperative handovers are the norm in the studies we reviewed, simulation-based studies of shift-change handovers have shown that information retention was worst during verbal handovers compared with verbal with note taking and handovers using a printed handout.38,39 It is also possible that multiple interactions, e.g., a review of the electronic record followed by a documented conversation with the delivering team, would provide the receiving team with a more comprehensive picture of the recovering patient. However, the impact on workflow entailed by such double-task handovers would need to be considered.
Related to these issues, research on electronic tools to support postoperative handovers is also needed. Such tools can facilitate handovers by extracting information from databases, thereby ensuring data accuracy, completeness, and timeliness.40,41 Standardizing knowledge transfers using electronic health record–based systems can decrease the incidence of information errors and omissions and reduce adverse events.41–44 However, our literature review identified only 2 studies that used information technology to facilitate handovers from the OR. In 1 study, the authors created various printed reports generated from the Anesthesia Information Management System records and distributed them to different patient destinations (ICU, general ward, etc.). This report was not formally evaluated.45 In another study, a document was created as part of the patient’s electronic health record using provider-entered data, but its evaluation was similarly limited.33 Another idea for future research is to assess the utility of providing PACU and ICU clinicians with access to intraoperative information (e.g., labs, anesthesia chart) via the electronic health record in real time. Such functionality would allow the clinicians to prepare for the patient’s arrival and could increase handover efficiency, but the impact of such changes on work-flow must also be considered.
Finally, further research is needed on the topic of sustainability. This topic has not been examined in the context of other types of patient handovers.16 Only 1 of the papers we reviewed studied the feasibility and long-term effects of changes in postoperative handover practice.30 This study found only partial compliance with a handover protocol initiated 3 years prior. Although attendance of team members was high, distractions were common and information delivery did not adhere to the protocol. Indeed, some elements of the protocol were inconsistently reported whereas other elements, also of clinical importance, but not included in the original protocol, were frequently discussed during the handover. (This positive change was labeled by the manuscript’s authors as user-centered innovation.) In other quality improvement research, some studies have shown that compliance rates decrease after the initial period of implementation, whereas others have demonstrated successful change management.46–48 Sustainable change is critical to high-quality patient care. It is important to understand how sustainability can be achieved, including overcoming economic, structural, and cultural barriers to success.
Many of the research questions discussed herein cannot be ethically or practically answered using randomized controlled trials, the “gold standard” of clinical investigation. Other, more feasible experimental designs may be required, such as the pragmatic trial. These trials compare 2 or more interventions in terms of their effectiveness in real-world practice, using broad eligibility criteria without blinding to treatment assignment. Thus, they sacrifice internal validity but gain generalizability.49 A pragmatic trial might be possible by randomizing patients to different handover methods by hospital or surgical service. With a pilot study to estimate effect size, feasibility, and cost implications, such a trial could assess the impact of different interventions on patient outcomes and process measures. Simulation-based studies can be used to determine the characteristics of a good handover. Simulated patients can range from high-fidelity mannequins to written descriptions and have been used to compare information transfer methods, train in teamwork and communication, and study information loss in handovers.38,39,50,51 Finally, both quantitative and qualitative observational studies can be valuable in describing current practice and many have been published on the topic of postoperative handovers.6,23,27,52
There are several limitations associated with our review of the literature. First, we elected to include all research on postoperative handovers, regardless of the patient population or destination unit. Thus, patients and settings ran the gamut from adults admitted to the PACU to infants admitted to the pediatric cardiac ICU. The level of complexity associated with the different types of handovers varied considerably, as did the members of the delivering and receiving teams. However, all postsurgical handovers have some common characteristics, which, we believe, warranted their shared analysis: (1) they all involve the physical transfer of a patient in a vulnerable state, along with monitoring and clinical equipment; (2) upon arrival, the transfer of knowledge and care responsibility occurs between multiprofessional clinicians with different levels of experience, which contributes to a communication gap53; and (3) many of the information items to be transferred and tasks to be completed are common to all surgical patients.
Second, based on the body of literature, we compiled a list of recommendations for improving the physical and communication aspects of postoperative handovers. However, not all recommendations are supported empirically; and for those that are, the levels of evidence vary. This is attributable to the paucity of relevant studies and to limited efforts to validate findings, and points again to the need for more research to support recommendations and identify best practices in postoperative patient handovers.
Associated with this limitation is the challenge of adapting the recommendations to clinical practice. With respect to the knowledge transfer, for example, there are 74 elements listed in Appendix 2. Clearly, it is impractical to convey so much information in a brief handover, and some elements may be irrelevant for certain settings, operations, or patient populations. In addition, excessive information can act as a distracter and keep providers from other work, while providing little value to the receiving team. However, Table 3, which lists the best substantiated and most frequently recommended information requirements, is clearly not a blanket solution. For instance, some of the information requirements included in papers authored by nurses19,54 were not included in most other papers, such as the patient’s English comprehension, preoperative level of consciousness, or contact information for members of the OR team in case of problems. Thus, they were not added to Table 3. However, to the extent that this information allows nurses to better prepare and care for their patients, it should be included in postoperative handovers. Thus, each clinical practice must identify a minimal dataset that is essential for safe, effective patient care, and a methodology that promotes flexible standardization of the information content.
Finally, our search strategy may have led us to omit articles, for example, by not including all relevant terms in our list of keywords. We improved our search by using complementary strategies, including scanning literature reviews and bibliographies of pertinent articles. Although this approach minimized the likelihood of missing suitable articles, it did not eliminate the possibility. Related to this, a publication bias may have affected our findings. Because of the tendency to favor studies with positive results, studies with negative results may not have been published.
CONCLUSIONS
More than 40 million patients undergo surgery in the United States annuallyb and are subsequently transferred to a PACU or ICU for recovery. According to our review of the literature, these transfers are characterized by poor teamwork and communication, patients arriving in a compromised state, unclear procedures, technical errors, unstructured processes, interruptions and distractions, lack of central information repositories, and nurse inattention because of multitasking. An association between poor-quality handovers and adverse events is also demonstrated, although causality cannot be proven.
Although the quality of research on postoperative handovers is variable and strong evidence is lacking, several recommendations are broadly supported. First, standardizing this process can improve patient care by ensuring information completeness and accuracy and increasing the efficiency of the patient transfer process. Handover standardization also addresses a Joint Commission national patient safety goal.c As part of this recommendation, the use of checklists to guide communication and protocols to structure clinical activities is advocated. To ensure the attention of all team members, many authors advise completing urgent tasks before the information transfer, limiting conversations while performing tasks, and adopting the “sterile cockpit” approach, i.e., allowing only patient-specific discussions during the verbal handover. All relevant team members should be present during the handover, and each should have an opportunity to speak or ask questions. Finally, training in team skills and communication is also promoted in some publications. These recommendations have the potential to improve the quality of postoperative handovers and the safety of patients during this critical period.
ACKNOWLEDGMENTS
We thank Kathy Gage for her critical review of the manuscript.
Supported by the VA National Center for Patient Safety.
Appendix
Appendix 1. Recommendations for Facilitating Postoperative Handovers.
| Process recommendation | Support for recommendation |
|---|---|
| Before patient transport | |
| Conduct a debrief in the OR in the presence of PACU/SICU nurses | Nagpal et al. (2010b)26 |
| Preparation for transport should include patient and equipment checks (including oxygen in cylinders and battery life) and liaison with staff at the destination | Beckmann et al. (2004)13 |
| Unconscious patients should be brought to the PACU breathing high-concentration inspired oxygen in the lateral position | Anwari (2002),23 Nagpal et al. (2011)9 |
| Patients should arrive hemodynamically stable, in no (or in mild) pain, and decently covered | Anwari (2002),23 Nagpal et al. (2011)9 |
| Put ventilator on test lung before patient arrival | Catchpole et al. (2007)10 |
| Prepare monitor, alarms, equipment, and fluids before patient arrival | Catchpole et al. (2007),10 Joy et al. (2011),21 Nagpal et al. (2011)9 |
| During patient transport | |
| A dedicated team should be available for patient transport. Team members should be familiar with the transportation of critically ill patients, skilled in airway management and resuscitation, patient monitoring and moving, and familiar with all equipment | Beckmann et al. (2004)13 |
| Adequate monitoring of the critically ill patient during transport should include ECG, blood pressure, oxygen saturation, and, if ventilated, end-tidal carbon dioxide | Beckmann et al. (2004)13 |
| Patient observations should be documented during transport | Beckmann et al. (2004)13 |
| Clinical care | |
| Complete urgent care tasks before the verbal handover | Mistry et al. (2008),22 Smith and Mishra (2010),31 Welter and Reiff (1989)19 |
| Identify a person in charge who will be responsible for coordinating the handover | Catchpole et al. (2007)10 |
| Identify a person responsible for situation awareness at handover and for safety checks | Catchpole et al. (2007)10 |
| Allocate tasks to people in specific roles | Catchpole et al. (2007)10 |
| Allocate experienced nurses to assist nurses receiving complex patients to the SICU. Assistants can establish ventilation and chest drainage, complete documentation, and provide decision support | Currey et al. (2006)52 |
| Minimize time patient is off ventilator or unmonitored | Catchpole et al. (2007)10 |
| Check pumps, lines, equipment, drains, urine bag | Catchpole et al. (2007),10 Nagpal et al. (2011)9 |
| Place drains on suction | Catchpole et al. (2007),10 Nagpal et al. (2011)9 |
| Keep lines untangled | Catchpole et al. (2007)10 |
| For orthopedic procedures, locate and mark a pulse distal to the surgical site for assessing the patient | Welter and Reiff (1989)19 |
| Anesthesia providers should check initial vital signs and patient stability before leaving | Anwari (2002),23 Smith and Mishra (2010)31 |
| Anesthesia providers should return to the PACU to review their patients | Anwari (2002)23 |
| Information transfer | |
| Establish a positive working atmosphere | Manser et al. (2010)32 |
| Take the awake patient’s experience into consideration | Manser et al. (2010)32 |
| Hand over information at the patient’s bedside to assist in recall of information and to prompt questions | Currey et al. (2006)52 |
| Provide sufficient time for handovers | Manser et al. (2010)32 |
| Set aside time for handover communication. Avoid performing other tasks during this time and limit conversations while performing tasks | Amato-Vealey et al. (2008),54 Catchpole et al. (2007),10 Chen et al.(2010),57 Currey et al. (2006),52 Nagpal et al. (2010c),27 Smith and Mishra (2010)31 |
| Recognize the importance of halting communication to address patient care | Chen et al. (2010)57 |
| Use the “sterile cockpit”—only patient-specific conversation or urgent clinical interruptions can occur during the handover | Chen et al. (2011),30 Joy et al. (2011),21 Mistry et al. (2008)22 |
| All relevant members of the surgical and receiving teams should be present during the handover and each specialty should take turns speaking | Chen et al. (2011),30 Kim et al. (2012),33 Mistry et al. (2008),22 Nagpal et al. (2010a),25 Nagpal et al. (2010c)27 |
| Only 1 care provider should speak at a time, with minimal distractions and interruptions | Catchpole et al. (2007),10 Chen et al. (2010),57 Joy et al. (2011),21 Welter and Reiff (1989)19 |
| Encourage cross-disciplinary discussions | Catchpole et al. (2007)10 |
| Cultivate mutual respect | Mazzocco et al. (2009)6 |
| Use verbal skills to convey information: speak clearly, structure information, emphasize key points, summarize, and separate fact from judgment | Manser et al. (2010),32 Nestel et al. (2005)59 |
| Provide an opportunity to ask questions and voice concerns | Amato-Vealey et al. (2008),54 Chen et al. (2010),57 Manser et al. (2010),32 Mazzocco et al. (2009),6 Mistry et al. (2008),22 Smith and Mishra (2010)31 |
| To verify that information was received, apply closed-loop communication, e.g., read back | Chen et al. (2010),57 Greenberg et al. (2007)12 |
| Important information should be communicated verbally | Anwari (2002),23 Nagpal et al. (2010c)27 |
| Document the handover | Kim et al. (20 12),33 Manser et al. (20 10),32 Nagpal et al. (2010b),26 Nagpal et al. (2010c)27 |
| Use supporting documentation, e.g., lab test results, anesthesia chart | Joy et al. (2011),21 Manser et al. (2010),32 Nestel et al. (2005)59 |
| Confirm handover completion and readiness of the receiving team to accept responsibility for the patient | Catchpole et al. (2007),10 Manser et al. (2010)32 |
| Quality improvement | |
| Use structured checklists to guide communication and ensure completeness of information. Use forms or reference cards as reminders | Amato-Vealey et al. (2008),54 Catchpole et al. (2007),10 Catchpole et al. (2010),56 Kim et al. (20 12),33 McQueen-Shadfar and Taekman (2010),58 Nagpal et al. (2010a),25 Nagpal et al. (2010b),26 Nagpal et al. (2010c),27 Smith and Mishra (2010)31 |
| Use protocols to standardize processes (such as preparation for transport and sequences of tasks) | Beckmann et al. (2004),13 Catchpole et al. (2007),10 Catchpole et al. (2010),56 Greenberg et al. (2007),12 Mistry et al. (2008),22 Nagpal et al. (2010a)25 |
| Computerize the handover by combining provider-entered notes with data extracted from electronic patient records | Kim et al. (20 12),33 Nagpal et al. (2010c)27 |
| Provide formal team or handover training | Catchpole et al. (2007),10 Catchpole et al. (2010),56 Chen et al. (2010),57 Mistry et al. (2008),22 Smith and Mishra (2010)31 |
OR = operating room; PACU = postanesthesia care unit; SICU = surgical intensive care unit; ECG = electrocardiogram.
Appendix 2. Recommendations for Information Content During Postoperative Handovers.
| Handover information recommendation | Support for recommendation |
|---|---|
| Team information | |
| Names of participating providers | Amato-Vealey et al. (2008),54 McQueen-Shadfar and Taekman (2010)58 |
| Surgery and anesthesia contact information in case of problems | Kim et al. (2012),33 Nagpal et al. (2010a),25 Welter and Reiff (1989)19 |
| Patient information | |
| Name | Amato-Vealey et al. (2008),54 Catchpole et al. (2007),10 Joy et al. (2011),21 Mazzocco et al. (2009),6 Meyer-Bender et al. (2010),45 Nagpal et al. (2011),9 Welter and Reiff (1989)19 |
| Identifiers | McQueen-Shadfar and Taekman (2010)58 |
| Date of birth | Amato-Vealey et al. (2008),54 Meyer-Bender et al. (2010)45 |
| Age | Catchpole et al. (2007),10 Joy et al. (2011),21 Nagpal et al. (2011),9 Welter and Reiff (1989),19 Zavalkoff et al. (2011)20 |
| Weight | Catchpole et al. (2007),10 Joy et al. (2011),21 Zavalkoff et al. (2011)20 |
| Allergies | Nagpal et al. (2010a),25 Nagpal et al. (2011),9 Welter and Reiff (1989),19 Zavalkoff et al. (2011)20 |
| No code/do not resuscitate status | Welter and Reiff (1989)19 |
| Diagnosis | Catchpole et al. (2007),10 Joy et al. (2011),21 Kim et al. (2012),33 Mazzocco et al. (2009),6 Meyer-Bender et al. (2010),45 Nagpal et al. (2010c),27 Nagpal et al. (2011),9 Zavalkoff et al. (2011)20 |
| Procedure performed | Amato-Vealey et al. (2008),54 Anwari (2002),23 Catchpole et al. (2007),10 Chen et al. (2011),30 Joy et al. (2011),21 Kim et al. (2012),33 Mazzocco et al. (2009),6 McQueen-Shadfar and Taekman (2010),58 Meyer-Bender et al. (2010),45 Mistry et al. (2008),22 Nagpal et al. (2010a),25 Nagpal et al. (2011),9 Welter and Reiff (1989)19 |
| Condition | Catchpole et al. (2007),10 Mazzocco et al. (2009),6 Zavalkoff et al. (2011)20 |
| Medical history | Amato-Vealey et al. (2008),54 Chen et al. (2011),30 Mazzocco et al. (2009),6 McQueen-Shadfar and Taekman (2010),58 Mistry et al. (2008),22 Nagpal et al. (2010a),25 Nagpal et al. (2010c),27 Nagpal et al. (2011),9 Welter and Reiff (1989),19 Zavalkoff et al. (2011)20 |
| Social history | Welter and Reiff (1989)19 |
| Patient use of eyeglasses or a hearing aid | Welter and Reiff (1989)19 |
| Patient’s English comprehension | Welter and Reiff (1989)19 |
| Previous operations | Chen et al. (2011),30 Welter and Reiff (1989)19 |
| Preoperative information | |
| Preoperative assessment | Anwari (2002),23 McQueen-Shadfar and Taekman (2010),58 Welter and Reiff (1989)19 |
| Premedication | Anwari (2002),23 Welter and Reiff (1989),19Zavalkoff et al. (2011)20 |
| Preoperative ECG | Welter and Reiff (1989)19 |
| Preoperative level of consciousness | Welter and Reiff (1989)19 |
| Anesthesia information | |
| Type of anesthesia and anesthetic course | Amato-Vealey et al. (2008),54 Catchpole et al. (2007),10 Meyer-Bender et al. (2010),45 Mistry et al. (2008),22 Nagpal et al. (2010a),25 Nagpal et al. (2011),9 Smith and Mishra (2010),31 Welter and Reiff (1989)19 |
| Anesthesia complications | Joy et al. (2011),21 Nagpal et al. (2010a),25 Nagpal et al. (2011)9 |
| Intraoperative medications, including dose and time | Amato-Vealey et al. (2008),54 McQueen-Shadfar and Taekman (2010),58 Meyer-Bender et al.(2010),45 Nagpal et al. (2011),9 Smith and Mishra (2010),31 Welter and Reiff (1989),19 Zavalkoff et al. (2011)20 |
| Antibiotics | Catchpole et al. (2007),10 Meyer-Bender et al. (2010)45 |
| IV fluids administered | Amato-Vealey et al. (2008),54 Catchpole et al. (2007),10 Chen et al. (2011),30 Joy et al. (2011),21 Meyer-Bender et al. (2010),45 Smith and Mishra (2010),31 Welter and Reiff (1989),19 Zavalkoff et al. (2011)20 |
| Blood products (type and amount) | Catchpole et al. (2007),10 Chen et al. (2011),30 Joy et al. (2011),21 Meyer-Bender et al. (2010),45 Nagpal et al. (2010c),27 Nagpal et al. (2011),9 Zavalkoff et al. (2011)20 |
| Estimated blood loss | Amato-Vealey et al. (2008),54 Catchpole et al. (2007),10 Chen et al. (2011),30 Meyer-Bender et al. (2010),45 Nagpal et al. (2010a),25 Nagpal et al. (2010c),27 Nagpal et al. (2011),9 Smith and Mishra (2010),31 Zavalkoff et al. (2011)20 |
| Bleeding problems | Joy et al. (2011)21 |
| Pain management method | Amato-Vealey et al. (2008),54 Anwari (2002),23 Smith and Mishra (2010)31 |
| Tubes/lines/wires | McQueen-Shadfar and Taekman (2010),58 Meyer-Bender et al. (2010),45 Welter and Reiff (1989),19 Zavalkoff et al. (2011)20 |
| Endotracheal tube size | Joy et al. (2011),21 Zavalkoff et al. (2011)20 |
| Laryngoscopy grade | Zavalkoff et al. (2011)20 |
| Intubation conditions | Meyer-Bender et al. (2010)45 |
| Ventilation | Catchpole et al. (2007),10 Chen et al. (2011),30 Zavalkoff et al. (2011)20 |
| Ventilation problems | Zavalkoff et al. (2011)20 |
| Hemodynamics | Chen et al. (2011),30 Joy et al. (2011)21 |
| Hemodynamic problems | Zavalkoff et al. (2011)20 |
| Electrolyte problems | Zavalkoff et al. (2011)20 |
| Glucose problems | Zavalkoff et al. (2011)20 |
| TEE/echocardiogram | Catchpole et al. (2007),10 Joy et al. (2011),21 Zavalkoff et al. (2011)20 |
| Intraoperative ECG changes | Chen et al. (2011),30 Welter and Reiff (1989),19 Zavalkoff et al. (2011)20 |
| Intraoperative positioning | Welter and Reiff (1989)19 |
| Last lab values | Chen et al. (2011),30 Meyer-Bender et al. (2010)45 |
| Last clinical findings | Meyer-Bender et al. (2010)45 |
| Surgical information | |
| Surgical course | Anwari (2002),23 Chen et al. (2011),30 McQueen-Shadfar and Taekman (2010),58 Nagpal et al. (2010a),25 Nagpal et al. (2011)9 |
| Surgical site information, including dressings, tubes, drains, and packing | Amato-Vealey et al. (2008),54 Kim et al. (20 12),33 Mazzocco et al. (2009),6 Nagpal et al.(2011),9 Smith and Mishra (2010),31 Welter and Reiff (1989)19 |
| Significant intraoperative events | Amato-Vealey et al. (2008)54 |
| Surgical complications and interventions | Amato-Vealey et al. (2008),54 Anwari (2002),23 Catchpole et al. (2007),10 Nagpal et al. (2010a),25 Nagpal et al. (2011),9 Welter and Reiff (1989)19 |
| New diagnosis, if different than original | Zavalkoff et al. (2011)20 |
| CPB/circulatory arrest/cross-clamp/other procedure durations | Catchpole et al. (2007),10 Chen et al. (2011),30 Joy et al. (2011),21 Meyer-Bender et al.(2010),45 Zavalkoff et al. (2011)20 |
| Problems weaning from CPB | Catchpole et al. (2007),10 Joy et al. (2011),21 Zavalkoff et al. (2011)20 |
| Current status | |
| Current IV fluids and rate of administration | Welter and Reiff (1989),19 Zavalkoff et al. (2011)20 |
| Inotropes | Chen et al. (2011),30 Joy et al. (2011)21 |
| Airway and oxygenation status | Amato-Vealey et al. (2008),54 Zavalkoff et al. (2011)20 |
| Assessment of hemodynamic stability | Amato-Vealey et al. (2008),54 Catchpole et al. (2007),10 Nagpal et al. (2011),9 Welter and Reiff (1989),19 Zavalkoff et al. (2011)20 |
| Pacing | Chen et al. (2011),30 Zavalkoff et al. (2011)20 |
| Thermal status | Amato-Vealey et al. (2008),54 Welter and Reiff (1989)19 |
| Urine output | Amato-Vealey et al. (2008),54 Joy et al. (2011)21 |
| Level of pain | Amato-Vealey et al. (2008)54 |
| Care plan | |
| Anticipated recovery and problems | Catchpole et al. (2007),10 Manser et al. (2010),32 McQueen-Shadfar and Taekman (2010),58 Nagpal et al. (2010a),25 Smith and Mishra (2010),31 Zavalkoff et al. (2011)20 |
| Clear postoperative management plan | Anwari (2002),23 Joy et al. (2011),21 Manser et al. (20 10),32 Mazzocco et al. (2009),6 McQueen-Shadfar and Taekman (2010),58 Meyer-Bender et al. (2010),45 Nagpal et al. (2010b),26 Smith and Mishra (2010)31 |
| Postoperative orders and investigations | Amato-Vealey et al. (2008),54 Nagpal et al. (2010a),25 Nagpal et al. (2010c),27 Nagpal et al. (2011)9 |
| Monitoring plan and range for physiological variables | Nagpal et al. (2010a),25 Nagpal et al. (2010c),27 Nagpal et al. (2011),9 Smith and Mishra (2010),31 Zavalkoff et al. (2011)20 |
| Analgesia plan | Kim et al. (2012),33 Nagpal et al. (2010a),25 Nagpal et al. (2010c),27 Nagpal et al. (2011)9 |
| Plan for IV fluids, antibiotics, medications, deep venous thrombosis prophylaxis | Kim et al. (2012),33 Nagpal et al. (2010a),25 Nagpal et al. (2010c),27 Nagpal et al. (2011),9Smith and Mishra (2010),31 Welter and Reiff (1989)19 |
| Needed blood | Nagpal et al. (2011)9 |
| Plan for tubes and drains | Nagpal et al. (2010a),25 Nagpal et al. (2011)9 |
| Plan for nasogastric tube and feeding | Kim et al. (2012),33 Nagpal et al. (2010a),25 Nagpal et al. (2010c),27 Nagpal et al. (2011)9 |
| Positioning plan | Smith and Mishra (2010)31 |
| Conditions for informing providers of a departure from normal patient status | Smith and Mishra (2010)31 |
| Plan for contacting social services, speech and physical therapists | Kim et al. (2012)33 |
| Plan for patient/caregiver education | Kim et al. (2012)33 |
| Plan for emergency care | Kim et al. (2012)33 |
ECG = electrocardiogram; TEE = transesophageal echocardiogram; CPB = cardiopulmonary bypass.
Footnotes
The Durham VA Patient Safety Center of Inquiry is a multidisciplinary team focused on optimizing the safety of patient care through research, high-fidelity point-of-care simulation training, and the diverse perspectives of clinicians, human factors engineers, and organizational behavior experts. Its members are B. Atkins, A. Barbeito, A. Bonifacio, R. Burton, J. Emery, G. Hobbs, M. Holtschneider, O. Jennings, S. Kellum, J. Mark, S. Perfect, D. Rogers, R. Schroeder, T. Schwartz, N. Segall, S. Sitkin, J. Taekman, D. Thornlow, and M. Wright.
DISCLOSURES
Name: Noa Segall, PhD.
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript.
Attestation: Noa Segall approved the final manuscript.
Name: Alberto S. Bonifacio, BSN.
Contribution: This author helped design the study, conduct the study, and analyze the data.
Attestation: Alberto S. Bonifacio approved the final manuscript.
Name: Rebecca A. Schroeder, MD.
Contribution: This author helped design the study and analyze the data.
Attestation: Rebecca A. Schroeder approved the final manuscript.
Name: Atilio Barbeito, MD.
Contribution: This author helped analyze the data and write the manuscript.
Attestation: Atilio Barbeito approved the final manuscript.
Name: Dawn Rogers, BSN.
Contribution: This author helped analyze the data.
Attestation: Dawn Rogers approved the final manuscript.
Name: Deirdre K. Thornlow, RN, PhD.
Contribution: This author helped analyze the data and write the manuscript.
Attestation: Deirdre K. Thornlow approved the final manuscript.
Name: James Emery, PhD.
Contribution: This author helped analyze the data.
Attestation: James Emery approved the final manuscript.
Name: Sally Kellum, RN-BC, MSN.
Contribution: This author helped analyze the data.
Attestation: Sally Kellum approved the final manuscript.
Name: Melanie C. Wright, PhD.
Contribution: This author helped design the study and write the manuscript.
Attestation: Melanie C. Wright approved the final manuscript.
Name: Jonathan B. Mark, MD.
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript.
Attestation: Jonathan B. Mark approved the final manuscript.
This manuscript was handled by: Sorin J. Brull, MD, FCARCSI (Hon).
The authors declare no conflicts of interest.
Agency for Healthcare Research and Quality: Discontinuities, Gaps, and Hand-Off Problems. Available at:http://www.psnet.ahrq.gov/collectionBrowse.aspx?taxonomyID=412. Accessed November 21, 2011.
Anesthesia in the United States 2009. Available at: aqihq.org/Anesthesia%20in%20the%20US%202_19_10.pdf. Accessed January 19, 2012.
The Joint Commission Accreditation Program: Hospital—National Patient Safety Goals. Available athttp://www.healthlawyers.org/SiteCollectionDocuments/Content/ContentGroups/Publications2/Health_Lawyers_Weekly2/Volume_3/Issue_25/JCAHO_guidance.pdf. (p. 6; although this is not the original document). Accessed August 24, 2009.
Reprints will not be available from the authors.
REFERENCES
- 1.Jeffcott SA, Evans SM, Cameron PA, Chin GSM, Ibrahim JE. Improving measurement in clinical handover. Qual Saf Health Care 2009;18:272–6 [DOI] [PubMed] [Google Scholar]
- 2.Borowitz SM, Waggoner-Fountain LA, Bass EJ, Sledd RM. Adequacy of information transferred at resident sign-out (inhospital handover of care): a prospective survey. Qual Saf Health Care 2008;17:6–10 [DOI] [PubMed] [Google Scholar]
- 3.Clancy CM. The importance of simulation: preventing hand-off mistakes. AORN J 2008;88:625–7 [DOI] [PubMed] [Google Scholar]
- 4.de Leval MR, Carthey JC, Wright DJ, Farewell VT, Reason JT. Human factors and cardiac surgery: a multicenter study. J Thorac Cardiovasc Surg 2000;119:661–72 [DOI] [PubMed] [Google Scholar]
- 5.Arora V, Johnson J, Lovinger D, Humphrey H, Meltzer D. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care 2005;14:401–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mazzocco K, Petitti DB, Fong KT, Bonacum D, Brookey J, Graham S, Lasky RE, Sexton JB, Thomas EJ. Surgical team behaviors and patient outcomes. Am J Surg 2009;197:678–85 [DOI] [PubMed] [Google Scholar]
- 7.Mistry K, Landrigan C, Goldmann D, Bates DW. Communication error during post-operative patient hand off in the pediatric intensive care unit. Crit Care Med 2005;33:A12 [Google Scholar]
- 8.Kitch B, Cooper J, Zapol W, Marder J, Karson A, Hutter M, Campbell E. Handoffs causing patient harm: a survey of medical and surgical house staff. Jt Comm J Qual Patient Saf 2008;34:563–70 [DOI] [PubMed] [Google Scholar]
- 9.Nagpal K, Abboudi M, Fischler L, Schmidt T, Vats A, Manchanda C, Sevdalis N, Scheidegger D, Vincent C, Moorthy K. Evaluation of postoperative handover using a tool to assess information transfer and teamwork. Ann Surg 2011;253:831–7 [DOI] [PubMed] [Google Scholar]
- 10.Catchpole KR, de Leval MR, McEwan A, Pigott N, Elliott MJ, McQuillan A, MacDonald C, Goldman AJ. Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. Paediatr Anaesth 2007;17:470–8 [DOI] [PubMed] [Google Scholar]
- 11.Kluger MT, Bullock MFM. Recovery room incidents: a review of 419 reports from the Anaesthetic Incident Monitoring Study (AIMS). Anaesthesia 2002;57:1060–6 [DOI] [PubMed] [Google Scholar]
- 12.Greenberg C, Regenbogen S, Studdert D, Lipsitz S, Rogers S, Zinner M, Gawande A. Patterns of communication breakdowns resulting in injury to surgical patients. J Am Coll Surg 2007;204:533–40 [DOI] [PubMed] [Google Scholar]
- 13.Beckmann U, Gillies DM, Berenholtz SM, Wu AW, Pronovost P. Incidents relating to the intra-hospital transfer of critically ill patients: an analysis of the reports submitted to the Australian Incident Monitoring Study in Intensive Care. Intensive Care Med 2004;30:1579–85 [DOI] [PubMed] [Google Scholar]
- 14.Australian Council for Safety and Quality in Health Care. Clinical Handover and Patient Safety: Literature Review Report, 2005 [Google Scholar]
- 15.Cohen MD, Hilligoss PB. Handoffs in Hospitals: a Review of the Literature on Information Exchange While Transferring Patient Responsibility or Control. Ann Arbor, MI: University of Michigan, 2009 [Google Scholar]
- 16.Wong MC, Yee KC, Turner PA Structured Evidence-Based Literature Review Regarding the Effectiveness of Improvement Interventions in Clinical Handover eHealth Services Research Group, ed. University of Tasmania, Australia: Australian: Commission on Safety and Quality in Health Care, 2008 [Google Scholar]
- 17.Kalkman CJ. Handover in the perioperative care process. Curr Opin Anaesthesiol 2010;23:749–53 [DOI] [PubMed] [Google Scholar]
- 18.Manser T, Foster S. Effective handover communication: an overview of research and improvement efforts. Best Pract Res Clin Anaesthesiol 2011;25:181–91 [DOI] [PubMed] [Google Scholar]
- 19.Welter ER, Reiff PA. Transferring patients from the OR: what the postanesthesia room nurse needs to know. AORN J 1989;50:1248–52 [DOI] [PubMed] [Google Scholar]
- 20.Zavalkoff SR, Razack SI, Lavoie J, Dancea AB. Handover after pediatric heart surgery: a simple tool improves information exchange. Pediatr Crit Care Med 2011;12:309–13 [DOI] [PubMed] [Google Scholar]
- 21.Joy BF, Elliott E, Hardy C, Sullivan C, Backer CL, Kane JM. Standardized multidisciplinary protocol improves handover of cardiac surgery patients to the intensive care unit. Pediatr Crit Care Med 2011;12:304–8 [DOI] [PubMed] [Google Scholar]
- 22.Mistry K, Jaggers J, Lodge A, Alton M, Mericle J, Frush K, Meliones J. Using Six Sigma® methodology to improve hand-off communication in high-risk patients In: Advances in Patient Safety: New Directions and Alternative Approaches. Rockville, MD: Agency for Healthcare Research and Quality, 2008 [PubMed] [Google Scholar]
- 23.Anwari JS. Quality of handover to the postanaesthesia care unit nurse. Anaesthesia 2002;57:488–93 [DOI] [PubMed] [Google Scholar]
- 24.Smith AF, Pope C, Goodwin D, Mort M. Interprofessional handover and patient safety in anaesthesia: observational study of handovers in the recovery room. Br J Anaesth 2008;101:332–7 [DOI] [PubMed] [Google Scholar]
- 25.Nagpal K, Arora S, Abboudi M, Vats A, Wong HW, Manchanda C, Vincent C, Moorthy K. Postoperative handover: problems, pitfalls, and prevention of error. Ann Surg 2010; 252:171–6 [DOI] [PubMed] [Google Scholar]
- 26.Nagpal K, Vats A, Ahmed K, Smith AB, Sevdalis N, Jonannsson H, Vincent C, Moorthy K. A systematic quantitative assessment of risks associated with poor communication in surgical care. Arch Surg 2010;145:582–8 [DOI] [PubMed] [Google Scholar]
- 27.Nagpal K, Vats A, Ahmed K, Vincent C, Moorthy K. An evaluation of information transfer through the continuum of surgical care: a feasibility study. Ann Surg 2010;252:402–7 [DOI] [PubMed] [Google Scholar]
- 28.Entin EB, Lai F, Barach P Training teams for the perioperative environment: a research agenda. Surg Innov 2006;13:170–8 [DOI] [PubMed] [Google Scholar]
- 29.Joy BF, Elliott E, Hardy C, Sullivan C, Backer CL, Kane JM. Standardized multidisciplinary protocol improves handover of cardiac surgery patients to the intensive care unit. Pediatr Crit Care Med 2011;12:304–8 [DOI] [PubMed] [Google Scholar]
- 30.Chen JG, Wright MC, Smith PB, Jaggers J, Mistry KP. Adaptation of a postoperative handoff communication process for children with heart disease: a quantitative study. Am J Med Qual 2011;26:380–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith AF, Mishra K. Interaction between anaesthetists, their patients, and the anaesthesia team. Br J Anaesth 2010;105:60–8 [DOI] [PubMed] [Google Scholar]
- 32.Manser T, Foster S, Gisin S, Jaeckel D, Ummenhofer W. Assessing the quality of patient handoffs at care transitions. Qual Saf Health Care 2010;19:e44. [DOI] [PubMed] [Google Scholar]
- 33.Kim SW, Maturo S, Dwyer D, Monash B, Yager PH, Zanger K, Hartnick CJ Interdisciplinary development and implementation of communication checklist for postoperative management of pediatric airway patients. Otolaryngol Head Neck Surg 2012;146:129–34 [DOI] [PubMed] [Google Scholar]
- 34.Pronovost P Interventions to decrease catheter-related bloodstream infections in the ICU: the Keystone Intensive Care Unit Project. Am J Infect Control 2008;36:S171.e1–5 [DOI] [PubMed] [Google Scholar]
- 35.Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, Herbosa T, Joseph S, Kibatala PL, Lapitan MC, Merry AF, Moorthy K, Reznick RK, Taylor B, Gawande AA; Safe Surgery Saves Lives Study Group. A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 2009;360:491–9 [DOI] [PubMed] [Google Scholar]
- 36.Mann S, Marcus R, Sachs B. Lessons from the cockpit: how team training can reduce errors on L&D. Contemp Ob Gyn, January 2006:1–7 [Google Scholar]
- 37.Neily J, Mills PD, Young-Xu Y. Association between implementation of a medical team training program and surgical mortality. JAMA 2010;304:1693–700 [DOI] [PubMed] [Google Scholar]
- 38.Bhabra G, Mackeith S, Monteiro P, Pothier DD. An experimental comparison of handover methods. Ann R Coll Surg Engl 2007;89:298–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pothier D, Monteiro P, Mooktiar M, Shaw A. Pilot study to show the loss of important data in nursing handover. Br J Nurs 2005;14:1090–3 [DOI] [PubMed] [Google Scholar]
- 40.Cheah LP, Amott DH, Pollard J, Watters DAK. Electronic medical handover: towards safer medical care. Med J Aust 2005;183:369–72 [DOI] [PubMed] [Google Scholar]
- 41.Petersen L, Orav E, Teich J, O’Neil A, Brennan T Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv 1998;24:77–87 [DOI] [PubMed] [Google Scholar]
- 42.Van Eaton EG, Horvath KD, Lober WB, Rossini AJ, Pellegrini CA. A randomized, controlled trial evaluating the impact of a computerized rounding and sign-out system on continuity of care and resident work hours. J Am Coll Surg 2005;200:538–45 [DOI] [PubMed] [Google Scholar]
- 43.Hertzum M, Simonsen J. Positive effects of electronic patient records on three clinical activities. Int J Med Inform 2008;77:809–17 [DOI] [PubMed] [Google Scholar]
- 44.Raptis DA, Fernandes C, Chua W, Boulos PB. Electronic software significantly improves quality of handover in a London teaching hospital. Health Informatics J 2009;15:191–8 [DOI] [PubMed] [Google Scholar]
- 45.Meyer-Bender A, Spitz R, Pollwein B. The anaesthetic report: custom-made printouts from anaesthesia-information-management-systems using extensible stylesheet language transformation. J Clin Monit Comput 2010;24:51–60 [DOI] [PubMed] [Google Scholar]
- 46.Pronovost PJ, Goeschel CA, Colantuoni E, Watson S, Lubomski LH, Berenholtz SM, Thompson DA, Sinopoli DJ, Cosgrove S, Sexton JB, Marsteller JA, Hyzy RC, Welsh R, Posa P, Schumacher K, Needham D. Sustaining reductions in catheter related bloodstream infections in Michigan intensive care units: observational study. BMJ 2010;340:c309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bauer MS. A review of quantitative studies of adherence to mental health clinical practice guidelines. Harv Rev Psychiatry 2002;10:138–53 [DOI] [PubMed] [Google Scholar]
- 48.Grol R, Wensing M, Eccles M. Improving Patient Care: The Implementation of Change in Clinical Practice. Oxford, UK: Elsevier, 2005 [Google Scholar]
- 49.Ware JH, Hamel MB. Pragmatic trials: guides to better patient care? N Engl J Med 2011;364:1685–7 [DOI] [PubMed] [Google Scholar]
- 50.Berkenstadt H, Haviv Y, Tuval A, Shemesh Y, Megrill A, Perry A, Rubin O, Ziv A Improving handoff communications in critical care: utilizing simulation-based training toward process improvement in managing patient risk. Chest 2008;134:158–62 [DOI] [PubMed] [Google Scholar]
- 51.Bogenstatter Y, Tschan F, Semmer N, Spychiger M, Breuer M, Marsch S. How accurate is information transmitted to medical professionals joining a medical emergency? A simulator study. Hum Factors 2009;51:115–25 [DOI] [PubMed] [Google Scholar]
- 52.Currey J, Browne J, Botti M Haemodynamic instability after cardiac surgery: nurses’ perceptions of clinical decisionmaking. J Clin Nurs 2006;15:1081–90 [DOI] [PubMed] [Google Scholar]
- 53.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care 2004;13:i85–i90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Amato-Vealey E, Barba M, Vealey R. Hand-off communication: a requisite for perioperative patient safety. AORN J 2008;88:763–74 [DOI] [PubMed] [Google Scholar]
- 55.Botti M, Bucknall T, Cameron P, Johnstone MJ, Redley B, Evans S, Jeffcott S. Examining communication and team performance during clinical handover in a complex environment: the private sector post-anaesthetic care unit. Med J Aust 2009; 190:S157–60 [DOI] [PubMed] [Google Scholar]
- 56.Catchpole K, Sellers R, Goldman A, McCulloch P, Hignett S. Patient handovers within the hospital: translating knowledge from motor racing to healthcare. Qual Saf Health Care 2010;19:318–22 [DOI] [PubMed] [Google Scholar]
- 57.Chen JG, Mistry KP, Wright MC, Turner DA. Postoperative handoff communication: a simulation-based training method. Simul Healthc 2010;5:242–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McQueen-Shadfar L, Taekman J. Say what you mean to say: improving patient handoffs in the operating room and beyond. Simul Healthc 2010;5:248–53 [DOI] [PubMed] [Google Scholar]
- 59.Nestel D, Kneebone R, Barnet A. Teaching communication skills for handover: perioperative specialist practitioners. Med Educ 2005;39:1157. [DOI] [PubMed] [Google Scholar]