Abstract
Introduction:
Adequate sleep duration and quality are protective against many adverse health outcomes. Many individual-level predictors of poor sleep have been examined, but few studies have examined neighborhood-level influences. Despite known associations between neighborhood green space and sleep influencing factors (e.g. physical activity, mental health), few studies have examined green space and sleep’s relationship. Further, little work has examined the relationship between the magnitude and type of neighborhood sounds and sleep.
Study Methods:
We analyzed data from the Survey of the Health of Wisconsin (SHOW) database (n=2,712) for 2008–2013, a representative sample of Wisconsin residents, ages 21–74. Outcomes included weekday and weekend sleep duration and self-rated sleep quality. Primary predictors were the proportion tree canopy (National Land Cover Database) and mean decibel levels of outdoor sound (US National Park Service) at the census block group (CBG) level. Survey regression analysis was used to examine statistical associations, controlling for individual and neighborhood-level covariates.
Results:
Models suggest a significant relationship (p<0.05) between weekday sleep duration and green space, and between weekend/day sleep duration and human-made and total neighborhood sound. Increased percent tree canopy in a CBG was associated with lower odds of short weekday sleep (<6h) (OR 0.76 [0.58, 0.98]). Increased human made and total mean decibel levels were associated with increased instances of short weekend and weekday sleep (OR 1.05 [1.01, 1.08] and 1.03 [1.01, 1.06] respectively).
Conclusions:
Neighborhood tree canopy and sound levels may influence sleep duration, and are potential targets for neighborhood level interventions to improve sleep.
Keywords: neighborhood, green space, sleep, sound, geography
Introduction
Few studies have considered neighborhood level influences on sleep beyond neighborhood socioeconomic status, despite observed spatial patterning of insufficient sleep, including across counties of the contiguous United States.1 Most studies of neighborhood factors and sleep outcomes that have reached beyond socioeconomic factors have focused on physical and social disorder. Studies have shown that people who feel safer from crime and violence in their neighborhoods have better sleep outcomes.2,3 Further examinations have shown associations between low perceived neighborhood quality and low self-rated health, of which, both have associations with adverse sleep outcomes, and neighborhood social environment inadequacy has been correlated with short sleep duration.2,4,5 Studies have also shown that small improvements to inadequate living facilities can improve the sleep quality among residents.6 Neighborhood population composition has also been explored, with the potential pathway linking neighborhood composition to sleep has been suggested to be psychological distress diminishing protective psychological resources.7 These findings have suggested that low quality sleep may be part of the link between poor neighborhood quality and poor health.5 Altogether, literature to date that focuses on neighborhood influences on sleep has considered only a small number of neighborhood characteristics, with a significant emphasis on neighborhood perceptions, socioeconomic status, housing infrastructure quality, and crime. Less emphasis has been placed on natural environmental features of neighborhoods, which have been found to be associated with related outcomes and may also promote sleep.
One element of the neighborhood environment that has received relatively little attention in sleep research is green space. Green space has been positively related to many health outcomes, including some with established relationships to sleep and sleep quality such as improved mental health. The positive impacts of green space include enhanced health promoting behaviors, such as physical activity and social engagement.8–10 Green space can also protect from air pollution, extreme temperature, and noise pollution.8 Additionally, as previously mentioned, mental health benefits such as stress reduction and mental fatigue reduction – potentially via attention restoration – are positively associated with exposure to green space including tree cover and other forms of vegetation.8,11 Depression and anxiety reductions, too, may be attributable to neighborhood green space.12
However, to our knowledge, only two studies have examined the role for neighborhood green space in impacting sleep outcomes. The first showed that reduced green space was associated with reduced sleep duration among >44 year old Australian adults.9 A second study, which analyzed US citizens at a county level, showed those exhibiting 21–29 days per month of insufficient sleep had lower odds of green space access than those who reported less than 1 week of insufficient sleep per month.13 Additional work is needed to determine if sleep duration and quality are associated with green space and whether findings are consistent across multiple populations and contexts.
Beyond green space, other aspects of the neighborhood built environment, including noise (unwanted sound), have been shown to affect sleep outcomes. Notably, neighborhood sound levels – while intuitively related to sleep quality and quantity – have received little attention in empirical research; this is of interest given that noise is thought to impact sleep, green space is protective against noise pollution, and total sound affecting an individual may include both human made and natural sounds.8,14 Previous research has assessed the associations between neighborhood noise and sleep outcomes. Residents in neighborhoods with high perceived noise levels report poorer physical health that is mediated by low sleep quality.15 Neighborhoods with high human made sound (from traffic, neighbors, and crowding) may prevent residents from initiating and maintaining sleep.15 Decibel levels associated with adverse outcomes have been proposed; among European populations, exposure to sound of <40 dB has been determined to have no significant negative biological effects; 40–55 dB causes a sharp increase in negative health effects, especially in vulnerable populations; >55 dB causes annoyances in most of the population and is associated with a high frequency of adverse outcomes (e.g., CVD).16 Few population based studies have examined these associations in the United States.
For a complete understanding of sleep, it must be conceptualized as a construct that includes both sleep quality and quantity, while controlling for objective demographic and socioeconomic measures.17–19 Excess sleep (>9 hours/night), habitual short sleep duration (<6 hours/night) and low sleep quality have been independently associated with negative health outcomes.5,20–27 In the present investigation, neighborhood levels of green space and sound, and three sleep outcomes—duration (weekday, weekend) and quality—are studied. We hypothesize that, after controlling for confounders, individuals living in areas with higher levels of neighborhood green space and lower levels of sound will experience significantly better sleep, including higher sleep quality and more adequate sleep durations (7–8 hours).
Methods
Survey of the Health of Wisconsin
This analysis uses data from the Survey of the Health of Wisconsin (SHOW). SHOW is an ongoing survey that began in 2008, which is modeled after National Health and Nutrition Examination Survey (NHANES) and designed to collect information from a representative sample of Wisconsin residents. The information included in the SHOW database includes surveys, physical exams, and biospecimens.8 All participant records are geocoded to address and census block group level to enable the linkage of SHOW data with other sources of neighborhood level information.28
Study Participants
Participants are non-institutionalized and non-active duty, adult (21–74-years-old) civilians from randomly selected households. Random selection includes a two-stage probability-based cluster sampling approach, stratified by region and poverty level.28 Since the start of the program in 2008, sample sizes have increased from 400 to over 1000 participants per year.8,29 The present study uses data from 2008–2013, including a total sample size of 2,712 adults with complete data for both exposures and outcomes of interest.
Outcome Measures
Sleep Duration and Sleep Quality
Sleep duration was assessed for respondents who were employed, in school, or had a varying sleep schedule by self-reported number of hours of sleep they achieved per night on an average weekday and weekend. Retired and unemployed persons without a varying sleep schedule were asked how many hours per night on average they slept. Sleep quality was assessed by asking respondents, “Over the past month, how would you rate your sleep quality overall?” Responses were scaled (excellent, very good, good, fair, and poor).
Neighborhood Green Space and Sound Level
US census block groups (defined on average having 600–3000 people) were used as the sampling units for SHOW data collection and adopted as the neighborhood definition in this study. Neighborhood greenspace was measured as the percent tree canopy per block group, using information from the National Land Cover Database (NLCD). The NLCD is the most recent data available on the Wisconsin tree canopy (2011) that can be used to delineate trees as a source of greenness, compared to other sources such as agriculture or other types of vegetation. We opted for a tree canopy based measure, as percent tree canopy has a clear implication for neighborhood-level interventions (e.g. the planting of trees).
Sound levels were also assessed, via data from the US National Park Service (USNPS), which created a georeferenced map of sound levels across the US, using the Random Forest models done by Breiman.14 The Random Forest models are the basis for the mapping of expected sound levels in existing conditions and with no human activity. A map of the sound produced solely by human activity was also derived by the USNPS by deriving the difference between nature’s sounds and actual sound level of the US with human presence.14 This map was established to understand relationships between sound and other variables in nature. Sound levels were measured in decibels exceeded half of the time on an average summer day in the geographic area being measured (L50 dBA sound pressure level, dBA re 20μPa).
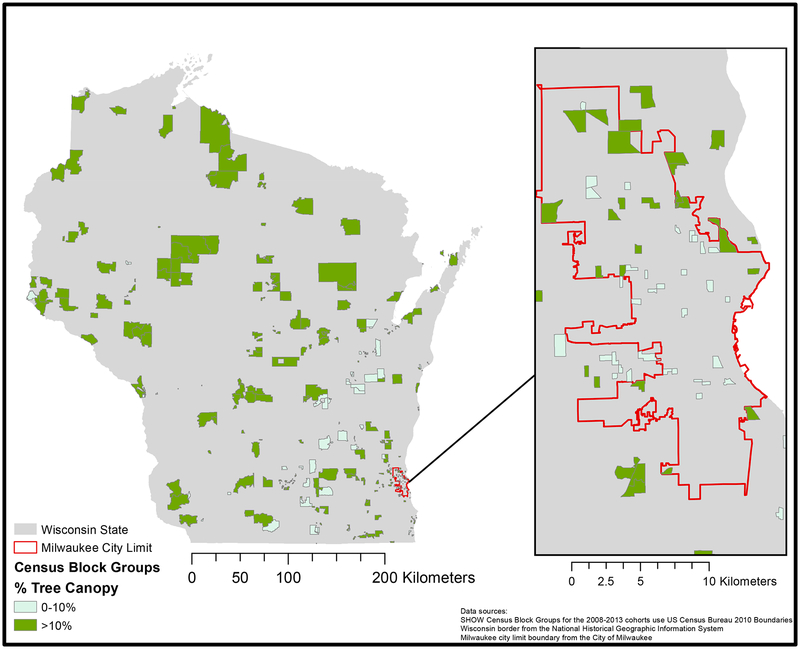
Figure 1 displays census block groups and whether their proportion tree canopy (from the National Land Cover Database) is above (green) or below (blue) 10%. The figure shows urban areas (i.e. Southcentral, Southeast, and Northeast Wisconsin) having lower proportions of tree canopy.
Figure 1:
2011 Proportion Tree Canopy (NLCD) and SHOW Block Groups
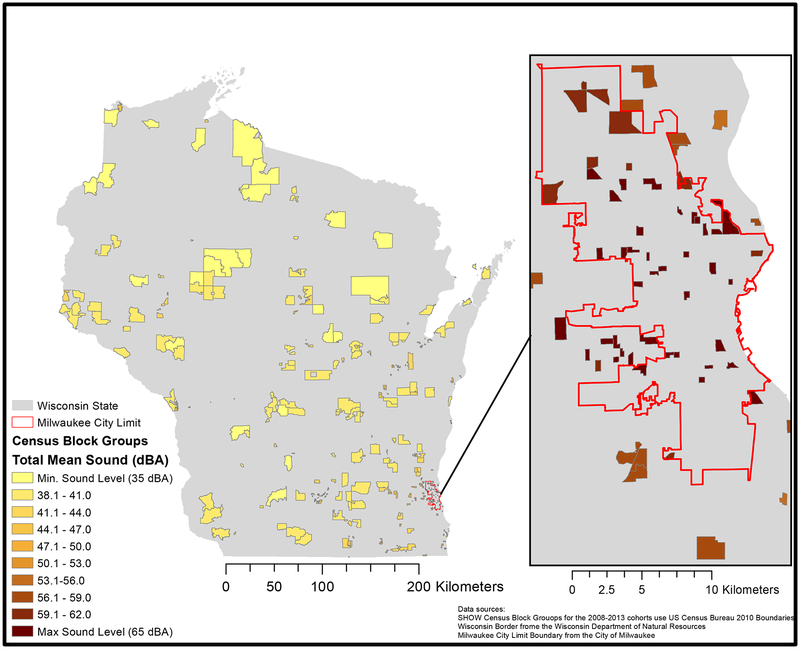
Figure 2 displays census block groups and total sound (from the US National Park Service). Total sound level includes nature sound and human synthesized sound. The figure shows urban CBGs having higher decibel levels (>50 dBA) than those with lower populations.
Figure 2:
2015 Total Sound (US-NPS) and SHOW Census Block Groups
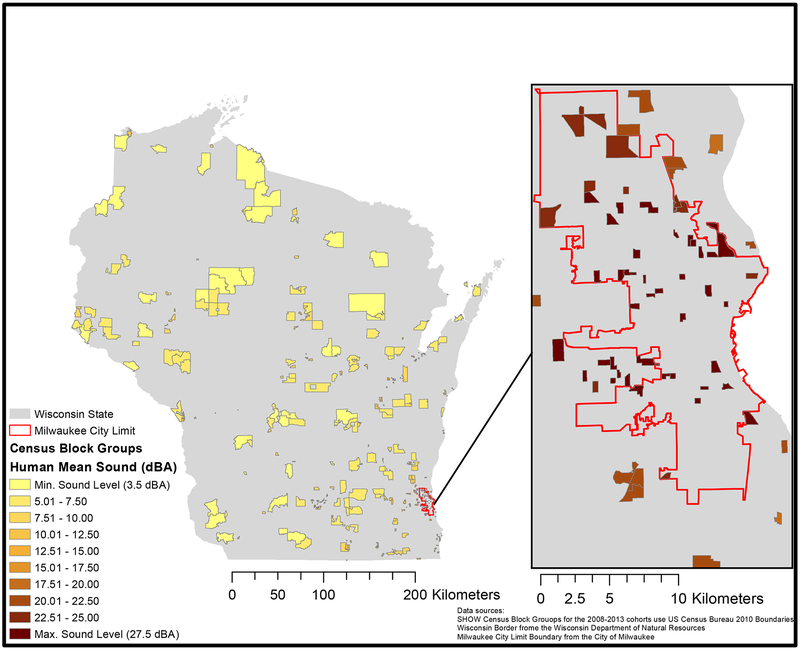
Figure 3 displays census block groups and human only sound (from the US National Park Service). Human only sound level excludes nature’s sound to make it a measure of only human synthesized sound. The figure shows urban CBGs having higher decibel levels (>15 dBA) than those with lower populations.
Figure 3:
2015 Human Only Sound (US-NPS) and SHOW Census Block Groups
Control Variables
Analyses controlled for several individual-level variables including sex (female, male), race/ethnicity (non-Hispanic white, non-Hispanic black/African American, Hispanic, other), age (21–34, 35–44, 45–54, 55–64, 65–74), length of residence (less than 1 year, 1–2 years, more than 2 but less than 5 years, more than 5 but less than 10 years, more than 10 but less than 20 years, more than 20 years but less than 40 years, >40 years), number of people in the household (lives alone, 1 other member, 2–4 other members, >4 other members), and marital status (never married, married/living with a partner, separated/ divorced/ widowed).
Individual socio-economic status was controlled by including measures of education level (less than high school, high school degree, some college/associates degree, bachelor’s degree, above bachelors or professional degree), annual household income (<$20,000, $20,000–$34,999, $35,000–$49,999, $50,000–$74,999, ≥$75,000), and occupational status (working at a job or business, with a job or business but not at work—vacation or sick leave, not working but looking for work, not working at a job or business and not looking for work).
Rural and Urban Communicating Area (RUCA) codes for 2003 (the most recent year) were used to control for neighborhood level urbanicity/rurality.30
Statistical Analysis
Neighborhood level predictors were assessed and mapped, and descriptive statistics for the sample population were calculated. Unadjusted and fully adjusted survey regression models, accounting for the clustering of individuals within block groups, were used to assess associations between daytime sleepiness, sleep quality, and sleep duration with neighborhood green space, and sound levels. Statistical analyses were undertaken in Stata 12.0, and neighborhood variable calculations and mapping were undertaken in ArcGIS.
Results and Discussion
Sample Characteristics
Sample characteristics are displayed in Table 1. The length of residence among SHOW participants ranged from <1 to >20 years. The majority (89%) of participants reported non-Hispanic white race/ethnicity. Most participants were married (72%), employed (68%), and lived in a metropolitan area (68%). Over 37% of individuals reported an income greater than $75,000 per year, and most were well-educated, with 76% of participants reporting at least some college. One third of participants lived in census block groups with less than 10% tree canopy cover. The average total sound level was nearly 46 dB, with an average estimated human contributed sound level of 12dB.
Table 1:
Sample Characteristics
| Variables | Percent (n=2,712) |
|---|---|
| Length of residence (yrs.) | |
| <1 year | 18% |
| ≥1 & ≤2 years | 13% |
| >2 & ≤5 years | 16% |
| >5 & ≤10 years | 18% |
| >10 & ≥20 years | 18% |
| >20 & ≤40 years | 15% |
| > 40 years | 3% |
| Age | |
| <35 | 24% |
| 35–44 | 19% |
| 45–54 | 26% |
| 55–64 | 19% |
| 65–74 | 11% |
| Gender | |
| Male | 51% |
| Female | 49% |
| Race/Ethnicity | |
| Non-Hispanic white | 89% |
| Non-Hispanic black/African American | 4% |
| Hispanic | 3% |
| Other | 4% |
| Educational Attainment | |
| < High school | 6% |
| High school/GED | 19% |
| Some college | 39% |
| Bachelor’s degree | 25% |
| Post-grad work | 12% |
| Household income | |
| <$20,000 | 12% |
| $20,000–34,999 | 15% |
| $35,000–49,999 | 14% |
| $50,000–74,999 | 23% |
| >$75,000 | 37% |
| Marital status | |
| Never married | 15% |
| Married or living with partner | 72% |
| Divorced/separated/widowed | 13% |
| Occupational status | |
| Working | 68% |
| With a job or business, but not at work | 4% |
| Not working, but looking for work | 6% |
| Not working and not looking for work | 21% |
| RUCA (Rural and Urban Commuting Areas) | |
| Metropolitan | 68% |
| Micropolitan | 14% |
| Small town | 10% |
| Rural | 9% |
| Block Group Percent tree canopy | |
| <10% | 33% |
| ≥10% | 67% |
| Continuous variables | Mean, 95%CI |
| Block group mean total sound (decibels) | 45.7 [45.1, 46.4] |
| Block group mean human sound (decibels) | 12.1 [11.4, 12.7] |
Models
Unadjusted regression models revealed many statistically significant associations, some of which were attenuated when adjusted for all control variables. Tree canopy was associated with short sleep on both weekdays and weekends, but the association persisted only for short weekday sleep in fully adjusted models (OR=0.76 [0.58, 0.98]). Total sound levels were associated with short weekday and weekend sleep and poor sleep quality in unadjusted analyses, but only associations with short sleep durations remained in adjusted models (OR=1.03 [1.01, 1.06] on weekdays; OR=1.05 [1.01, 1.08] on weekends); we observed a similar pattern for human-generated sound, indicating that human sources of sound are likely the primary driver of associations with sleep outcomes.
Control variables include: length of residence, age, gender, race/ethnicity, educational attainment, household income, marital status, occupational status, occupational status, and rural and urban commuting areas (RUCA)
Table 2:
Models Linking Neighborhood Green Space to Sleep Outcomes (Odds Ratios)
| Model 1: Unadjusted | Model 2: Adjusted | |
|---|---|---|
| Odds Ratio [95% CI] | Odds Ratio [95% CI] | |
| Short Weekday Sleep | ||
| tree canopy (>10%) | 0.72 [0.55, 0.93]* | 0.76 [0.58, 0.98]* |
| total sound (dBA) | 1.03 [1.01, 1.06]** | 1.03 [1.01, 1.06]* |
| human sound (dBA) | 1.04 [1.02, 1.06]** | 1.03 [1.01, 1.06]* |
| Short Weekend Sleep | ||
| tree canopy | 0.65 [0.46, 0.92]* | 0.86 [0.59, 1.24] |
| total sound | 1.08 [1.06, 1.10]** | 1.05 [1.01, 1.08]** |
| human sound | 1.08 [1.06, 1.10]** | 1.04 [1.01, 1.08]* |
| Poor Sleep Quality | ||
| tree canopy | 0.92 [0.72, 1.18] | 1.01 [0.79, 1.29] |
| total sound | 1.03 [1.01, 1.05]** | 1.02 [1.00, 1.05] |
| human sound | 1.03 [1.01, 1.05]** | 1.02 [0.99, 1.04] |
p<0.05,
p<0.01
Discussion
Few studies have examined relationships between levels of neighborhood green space and sound, and sleep outcomes. Our analyses indicate potential relationships between green space and sleep duration, and between sound levels and sleep duration in both unadjusted and control models. While sleep quality and sound associations were significant for unadjusted models, they did not persist in controls.
The association between higher levels of green space and decreased odds of short sleep provide evidence that green space may have a role in health outcomes. If higher levels of green space and lower levels of sound contribute to sleep outcomes, neighborhood level modifications to reduce sound levels from traffic, industry, and other sources – including through the enhancement of urban greenery – may have important implications for sleep patterns as well as conditions affected by sleep quality and quantity, including metabolic effects, cognitive impairment, endocrine dysfunction, physical inactivity, mortality, disease, obesity, and appetite stimulation).20–24 Further research is warranted to determine if there is causality of these associations. Establishing causality would provide implications for public health policy and urban planning in climates similar to that in Wisconsin.
Findings complement and extend findings of the two previous studies examining sleep outcomes and green space.9,13 Our study was able to look beyond the >44 years old Australian population that Astell-Burt’s study analyzed. We were also able to contextualize a U.S. neighborhood in more accurate way than the U.S. green space and sleep study could, as census block groups are much smaller in size than counties. Finally, our study looked at multiple sleep modalities (sleep duration and quality), while the others examined one sleep outcome each.
While associations were seen with sleep duration, sleep quality associations were not significant in adjusted analyses. The relationship between quality and duration is unclear, but it is recognized that both adequate quality and duration are uniquely protective for different health outcomes, supporting research that considers both sleep quantity and quality.31–35 Sleep research more commonly looks at quantity as a measure of sleep outcomes. Sleep quantity has correlations with physical activity, metabolic effects, cognitive impairment, endocrine dysfunction, physical inactivity, mortality, disease, obesity, and appetite.20,21,23,24 This evidence indicates that research findings specific to either sleep quality or quantity can be useful in informing health policy.
While this study identified relationships between sound, green space and sleep, it did not consider the potential mechanisms by which sound or green space may contribute to sleep patterns. Behavioral factors such as mental health status and levels of physical activity, which have been linked to green space, are also known to be related to sleep. For instance, insomnias or hypersomnias are key features of depression. Additionally, exercise has been shown to be an effective adjunct to medication to help treat symptoms of depression.36 Exercise has also been shown to be an alternative treatment of insomnia, with the exact mechanism still unclear.37 Although physical activity is higher in areas with green space, research has thus far been unable to attribute positive health effects entirely to the increase in exercise.38,39 This suggests a possibility that green space helps in the interplay of exercise, mental health, and sleep duration. Another proposed mechanisms of green space’s influence on sleep duration is through its relationship to social cohesion. Social cohesion can decrease psychological distress.7 This, in turn, is related to additional social determinants of a neighborhood (e.g. crime levels), which have effects on sleep outcomes.2,4,5
Socioeconomic and demographic factors influence sleep as well. Populations with lower education levels are more likely to experience habitually short sleep, specifically if working long hours, multiple jobs, or rotating/night shifts.17–19 The proportion of low income and lower educated is higher among some racial and ethnic minority populations making likely an unequal burden of additional noise by race and ethnicity as well. Differences in demographic distributions by urbanicity, as people living in inner cities have increased short sleep and decreased long sleep, are also important factors to consider.19 Thus, these findings may also be attributed to other factors often associated with urban neighborhoods, (e.g. higher levels of crime, sound, light, and pollution). Finally, in-home factors related to low income status (e.g. sound and light pollution, HVAC control, and non-private uncomfortable sleeping areas) produce challenging sleep environments which were not included in the current study.6,17
Despite this complexity and the potential interplay of these associations, a holistic analysis of green space could help to mitigate the negative impacts of these other social and environmental factors in a cost-effective population level intervention, increasing the value of the existing research. Associations between green space and positive health outcomes appear to be multifactorial, requiring additional research for each outcome. Furthermore, our finding that decreased total and human-made sound resulted in longer weekday and weekend sleep duration should be explored to examine sound levels in concert with green space levels, as green space is known to help in reducing noise pollution,8 and thus may provide both direct and indirect effects. Future work should consider mediating influences linking neighborhood level attributes, such as green space, to sleep outcomes.
Context is an additional factor to consider in neighborhood studies such as this.40 The context of SHOW makes this study both impactful and unique. SHOW is a statewide representative sample made up of approximately one-third rural block groups. Tree cover, sound and sleep are likely differentially related in urban and rural context. Despite adjustment for urbanicity, we did not stratify analyses to explore more specifically in high sound areas whether green space influenced or had positive associations with sleep.
The strengths of this study include a representative population-based sample, the use of objective, detailed green space and sound measures, a reliable database for the extraction of data, and the inclusion of many covariates to control confounding, including length of residence in the neighborhood. To our knowledge, this is the first study to examine green space in concert with several measures of sleep quantity and quality, and one of the first to examine objectively measured neighborhood attributes with sleep outcomes. More work in this area is needed.
However, the study is subject to some limitations. For one, SHOW used census block groups to measure neighborhoods, which may not exactly represent a neighborhood. SHOW also used self-reported health measures, which may be limited by recall bias. Another important limitation is the cross-sectional study design, which precludes the inference of causality. Further, with regard to sleep quality, future work may employ a more comprehensive assessment of sleep quality, as opposed to one scaled question to generalize overall sleep quality.
In conclusion, this study showed that neighborhood features correlate with sleep outcomes. Tree canopy of >10% was associated with lower odds of weekday short sleep duration (OR=0.76), and higher sound decibel levels were associated with higher odds of weekend (OR=1.05) and weekday (OR=1.03) short sleep duration. Further studies should examine associations between neighborhood green space, sleep outcomes, potential mediators, and other health related outcomes to determine whether greening of neighborhoods may be a viable method to improve population sleep and related health outcomes.
Acknowledgments:
The authors thank all the staff and researchers with the Survey of the Health of Wisconsin (SHOW) program and participants as well as the UW Survey Center without whom this research would not be possible. Funding for this project was supported by the National Institute on Aging (T35AG-29793), the National Heart Lung and Blood Institute (1 RC2 HL101468), the National Institutes of Health’s Clinical and Translational Science Award (5UL 1RR025011), the University of Wisconsin’s (UW) Wisconsin Partnership Program PERC Award (233PRJ25DJ), the Advancing a Healthier Wisconsin Endowment at the Medical College of Wisconsin, and a core grant to the Center for Demography and Ecology at the University of Wisconsin-Madison (P2C HD047873). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or other funders. We would like to thank all members of the SHOW administrative, field, and scientific staff for their significant and meaningful contributions to this project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
There are no conflicts of interest.
Sources
- 1.Grandner MA, Smith TE, Jackson N, Jackson T, Burgard S, Branas C. Geographic distribution of insufficient sleep across the United States: A county-level hotspot analysis. Sleep Heal. 2015;1(3):158–165. doi: 10.1016/j.sleh.2015.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hill TD, Trinh HN, Wen M, Hale L. Perceived neighborhood safety and sleep quality: A global analysis of six countries. Sleep Med. 2016;18:56–60. doi: 10.1016/j.sleep.2014.12.003 [DOI] [PubMed] [Google Scholar]
- 3.Johnson DA, Brown DL, Morgenstern LB, Meurer WJ, Lisabeth LD. The association of neighborhood characteristics with sleep duration and daytime sleepiness. Sleep Heal. 2015;1(3):148–155. doi: 10.1016/j.sleh.2015.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeSantis AS, Diez Roux AV, Moore K, Baron KG, Mujahid MS, Nieto FJ. Associations of Neighborhood Characteristics with Sleep Timing and Quality: The Multi-Ethnic Study of Atherosclerosis. Sleep. 2013;36(10):1543–1551. doi: 10.5665/sleep.3054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hale L, Hill TD, Friedman E, et al. Perceived neighborhood quality, sleep quality, and health status: Evidence from the Survey of the Health of Wisconsin. Soc Sci Med. 2013;79:16–22. doi: 10.1016/j.socscimed.2012.07.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simonelli G, Leanza Y, Boilard A, et al. Sleep and quality of life in urban poverty: the effect of a slum housing upgrading program. Sleep. 2013;36(11):1669–1676. doi: 10.5665/sleep.3124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hill TD, Burdette AM, Hale L. Neighborhood disorder, sleep quality, and psychological distress: Testing a model of structural amplification. Heal Place. 2009;15(4):1006–1013. doi: 10.1016/j.healthplace.2009.04.001 [DOI] [PubMed] [Google Scholar]
- 8.Beyer KMM, Kaltenbach A, Szabo A, Bogar S, Javier Nieto F, Malecki KM. Exposure to neighborhood green space and mental health: Evidence from the survey of the health of wisconsin. Int J Environ Res Public Health. 2014;11(3):3453–3472. doi: 10.3390/ijerph110303453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Astell-Burt T, Feng X, Kolt GS. Does access to neighbourhood green space promote a healthy duration of sleep? Novel findings from a cross-sectional study of 259 319 Australians. BMJ Open. 2013;3(8). doi: 10.1136/bmjopen-2013-003094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mitchell R, Popham F. Effect of exposure to natural environment on health inequalities: an observational population study. Lancet. 2008;372(9650):1655–1660. doi: 10.1016/S0140-6736(08)61689-X [DOI] [PubMed] [Google Scholar]
- 11.Faber Taylor A, Kuo FE. Children with attention deficits concentrate better after walk in the park. J Atten Disord. 2009;12(5):402–409. doi: 10.1177/1087054708323000 [DOI] [PubMed] [Google Scholar]
- 12.Miles R, Coutts C, Mohamadi A. Neighborhood urban form, social environment, and depression. J Urban Heal. 2012;89(1):1–18. doi: 10.1007/s11524-011-9621-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grigsby-Toussaint DS, Turi KN, Krupa M, Williams NJ, Pandi-Perumal SR, Jean-Louis G. Sleep insufficiency and the natural environment: Results from the US Behavioral Risk Factor Surveillance System survey. Prev Med (Baltim). 2015;78:78–84. doi: 10.1016/j.ypmed.2015.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mapping Sound - Natural Sounds (U.S. National Park Service). https://www.nps.gov/subjects/sound/soundmap.htm. Accessed May 16, 2016.
- 15.Hale L, Hill TD, Burdette AM. Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Prev Med (Baltim). 2010;51(3–4):275–278. doi: 10.1016/j.ypmed.2010.06.017 [DOI] [PubMed] [Google Scholar]
- 16.Kim R, Berg M den. Summary of night noise guidelines for Europe. Noise Heal. 2010;12(47):61. doi: 10.4103/1463-1741.63204 [DOI] [PubMed] [Google Scholar]
- 17.Stamatakis KA, Kaplan GA, Roberts RE. Short Sleep Duration Across Income, Education, and Race/Ethnic Groups: Population Prevalence and Growing Disparities During 34 Years of Follow-Up. Ann Epidemiol. 2007;17(12):948–955. doi: 10.1016/j.annepidem.2007.07.096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Givens ML, Malecki KC, Peppard PE, et al. Shiftwork, sleep habits, and metabolic disparities: Results from the Survey of the Health of Wisconsin. Sleep Heal. 2015;1(2):115–120. doi: 10.1016/j.sleh.2015.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep. 2007;30(9):1096–1103. doi: 10.1093/sleep/30.9.1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gildner TE, Liebert MA, Kowal P, Chatterji S, Snodgrass JJ. Associations between sleep duration, sleep quality, and cognitive test performance among older adults from six middle income countries: Results from the study on global ageing and adult health (SAGE). J Clin Sleep Med. 2014;10(6):613–621. doi: 10.5664/jcsm.3782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Magee CA, Iverson DC, Caputi P. Factors associated with short and long sleep. Prev Med (Baltim). 2009;49(6):461–467. doi: 10.1016/j.ypmed.2009.10.006 [DOI] [PubMed] [Google Scholar]
- 22.Martin S, Engleman H, Deary I, Douglas J. The effect of sleep fragmentation on daytime function. Am J Respir Crit Care Med. 1996;154(4):1328–1332. doi: 10.1164/ajrccm.155.5.9154863 [DOI] [PubMed] [Google Scholar]
- 23.Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007;11(3):163–178. doi: 10.1016/j.smrv.2007.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Cauter E, Spiegel K, Tasali E, Leproult R. Metabolic consequences of sleep and sleep loss. Sleep Med. 2008;9 Suppl 1:S23–8. doi:S1389–9457(08)70013–3 [pii]\r 10.1016/S1389-9457(08)70013-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Daglar G, Pinar SE, Sabanciogullari S, Kav S. Sleep quality in the elderly either living at home or in a nursing home. Aust J Adv Nurs. 2014;31(4):6–13. [Google Scholar]
- 26.St George RJ, Delbaere K, Williams P, Lord SR. Sleep quality and falls in older people living in self- and assisted-care villages. Gerontology. 2009;55(2):162–168. doi: 10.1159/000146786 [DOI] [PubMed] [Google Scholar]
- 27.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-Analysis of Quantitative Sleep Parameters From Childhood to Old Age in Healthy Individuals: Developing Normative Sleep Values Across the Human Lifespan. Sleep. 2004;27(7):1255–1273. doi: 10.1093/sleep/27.7.1255 [DOI] [PubMed] [Google Scholar]
- 28.Nieto FJ, Peppard PE, Engelman CD, et al. The Survey of the Health of Wisconsin (SHOW), a novel infrastructure for population health research: Rationale and methods. BMC Public Health. 2010;10. doi: 10.1186/1471-2458-10-785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Survey of the Health of Wisconsin (SHOW), University of Wisconsin School of Medicine and Public Health. University of Wisconsin Madison School of Medicine and Public Health. http://www.med.wisc.edu/show/survey-of-the-health-of-wisconsin/35828. Published 2016. Accessed May 16, 2016.
- 30.USDA ERS - Rural-Urban Commuting Area Codes. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/. Accessed August 10, 2017. [Google Scholar]
- 31.Kronholm E, Härmä M, Hublin C, Aro AR, Partonen T. Self-reported sleep duration in Finnish general population. J Sleep Res. 2006;15(3):276–290. doi: 10.1111/j.1365-2869.2006.00543.x [DOI] [PubMed] [Google Scholar]
- 32.Mesas AE, López-García E, León-Muñoz LM, Graciani A, Guallar-Castillón P, Rodríguez-Artalejo F. The association between habitual sleep duration and sleep quality in older adults according to health status. Age Ageing. 2011;40(3):318–323. doi: 10.1093/ageing/afr004 [DOI] [PubMed] [Google Scholar]
- 33.Bixler EO, Vgontzas a N, Lin H-M, Calhoun SL, Vela-Bueno a, Kales a. Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab. 2005;90(8):4510–4515. doi: 10.1210/jc.2005-0035 [DOI] [PubMed] [Google Scholar]
- 34.Goldman SE, Ancoli-Israel S, Boudreau R, et al. Sleep problems and associated daytime fatigue in community-dwelling older individuals. Journals Gerontol Ser A Biol Sci Med Sci. 2008;63A(10):1069–1075. http://search.ebscohost.com/login.aspx?direct=true&db=gnh&AN=125593&lang=zhtw&site=ehost-live. [DOI] [PubMed] [Google Scholar]
- 35.Ohayon MM. Nocturnal awakenings and comorbid disorders in the American general population. J Psychiatr Res. 2008;43(1):48–54. doi: 10.1016/j.jpsychires.2008.02.001 [DOI] [PubMed] [Google Scholar]
- 36.Kryger MH. b, Roth T. d e, Dement WC. Principles and Practice of Sleep Medicine.; 2005. http://www.scopus.com/inward/record.url?eid=2-s2.0-84882866343&partnerID=40&md5=7efc6850e9d80a0c58db18a369e0e8a6.
- 37.Danielson L, Noras AM, Carlsson J. Exercise in the treatment of major depression: A systematic review grading the quality ofevidence. Physiother Theory Pract. 2013;29(8):573–585. http://web.b.ebscohost.com.proxy.lib.mcw.edu/ehost/pdfviewer/pdfviewer?sid=f6c03f62-3608-4613-b31d-10b2e3f5600c%40sessionmgr103&vid=1&hid=123. Accessed April 27, 2017. [DOI] [PubMed] [Google Scholar]
- 38.Richardson EA, Pearce J, Mitchell R, Kingham S. Role of physical activity in the relationship between urban green space and health. Public Health. 2013;127(4):318–324. doi: 10.1016/j.puhe.2013.01.004 [DOI] [PubMed] [Google Scholar]
- 39.Mytton OT, Townsend N, Rutter H, Foster C. Green space and physical activity: An observational study using Health Survey for England data. Health Place. 2012;18(5):1034–1041. doi: 10.1016/j.healthplace.2012.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Diez Roux AV, Mair C, Roux AVD, Mair C, Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186(1):125–145. doi: 10.1111/j.1749-6632.2009.05333.x [DOI] [PubMed] [Google Scholar]