Abstract
Autoantibodies against end products of lipid peroxidation have unexpected effects on atherosclerosis in systemic lupus erythematosus (SLE).
The discovery of their effects could lead to new theories about the role of the adaptive immune system in SLE.
Systemic lupus erythematosus (SLE) is a disease characterized by the formation of pathogenic autoantibodies. Many of these autoantibodies, such as those specific for double-stranded DNA, SSA/Ro and cardiolipin, are believed to act as markers of disease activity and also contribute directly to disease pathogenesis. Current therapeutic options for SLE are mainly focused on reducing or eliminating pathogenic autoantibody formation, usually through dampening immune responses (glucocorticoids and hydroxychloroquine), nonspecific targeting of immune cells (mycophenolate mofetil), or directly targeting antibody-producing B cells (rituximab and belimumab). Patients with SLE are also known to have a greatly increased risk for cardiovascular disease; however, the exact role of autoantibodies in the pathogenesis of atherosclerosis in SLE is less clear. Rahman et al.1 recently reported that autoantibodies against malondialdehyde (MDA) and phosphorylcholine (PC) are negatively associated with the prevalence of atherosclerotic plaques in patients with SLE.
Although the concept of autoantibody- driven diseases suggests that all auto-anti bodies are inherently pathogenic, accumulating evidence shows that some autoantibodies are, in fact, protective. Inducing autoantibody formation through oral tolerance to self-peptides is known to delay or prevent SLE-like disease in rodents2. Translating these successes into treatments for human autoimmunity, however, has proven elusive.
‘Natural’ IgM autoantibodies that arise spontaneously without antigenic or microbial stimuli have also been described. These IgM autoantibodies are present in the circulation from birth, recognize oxidized epitopes on lipoproteins and phospholipid-containing cell membranes exposed during the process of apoptosis, and have immunoregulatory functions in cardiovascular disease3,4. Previous data suggest that the induction of these antibodies are not reliant on interactions between B cells and T cells5,6.
Protective IgM autoantibodies, therefore, might be of particular interest in both atherosclerosis and SLE. Increased levels of IgM that recognize modified PC, a component of oxidized LDL, have been reported to correlate with lower disease activity and damage scores, reduced presence of carotid artery plaques, and reduced frequency of cardiovascular events in patients with SLE4,7. The concept of ‘protective autoimmunity,’ which has been described in diseases of the central nervous system8, could also apply to autoimmune diseases. Thus, protective autoantibodies could represent a novel mechanism of ‘checks and balances’ in autoimmunity.
Indeed, data from the study by Rahman et al.1 suggest that IgM antibodies against PC and the lipid-related epitope MDA seem to protect against atherosclerosis, but that serum anti-MDA antibody levels are negatively associated with SLE. Low levels of IgM anti-MDA were also associated with the presence of atherosclerosis; individuals with SLE in the lowest tertile for anti-MDA IgM levels had a nearly threefold higher adjusted odds ratio for the presence of carotid plaques. This finding complements previous work by the same group that suggested anti-PC antibodies are protective against plaque development in SLE7. Similarly, in their current study Rahman et al.1 found that when levels of both anti-MDA and anti-PC antibodies were in the top tertile, patients with SLE were protected against the development of plaques. These findings mirror the group’s previous observations that combinations of anti-MDA and anti-PC IgM are negatively associated with stroke risk in the general population and with progression of carotid artery intima-media thickness in patients with hypertension9,10.
Unexpectedly, Rahman et al.1 demonstrated that production of anti-PC and anti-MDA antibodies requires physical interactions between B cells and T cells in a manner dependent on CD40 and MHC class II. Although the kind of T cell help required is unclear, these data suggest the novel hypothesis that protective autoantibodies against potentially harmful endogenous epitopes, such as those created by protein oxidation, could be generated by the adaptive immune system.
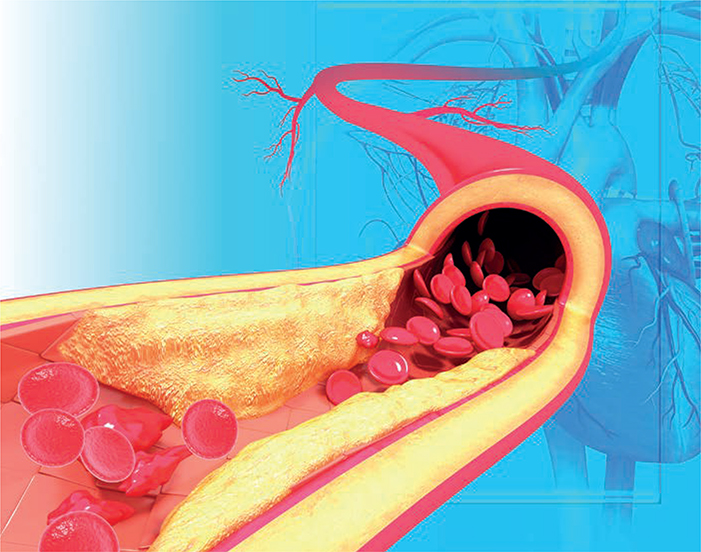
IgM anti-MDA and anti-PC antibodies also seem to be involved in the clearance of apoptotic cells. Rahman et al.1 found that anti-PC and anti-MDA antibodies increased macrophage phagocytosis of apoptotic Jurkat cells. This observation confirms previous in vivo and in vitro work6. Given that dysregulation of apoptosis in SLE promotes inflammation, the deficiency of these antibodies in SLE could provide insights into other pathogenic mechanisms. Furthermore, apoptotic cells are known to accumulate in atherosclerotic lesions, and they can further drive plaque formation and inflammation through endothelial cell activation and monocyte recruitment. The oxidized-PC-specific autoantibody E06 has been shown to inhibit this process6. Patients with SLE are at high risk of developing atherosclerosis, with the risk in young women with SLE being up to 50 times higher than in their age-matched healthy counterparts. Thus, identification of novel biomarkers for atherosclerosis, such as low levels of autoantibodies against PC or MDA or other SLE-specific alterations, is essential to identify and treat at-risk patients.
The data presented by Rahman et al.1 suggest new avenues for future research. The aetiology of the decreased levels of IgM anti-MDA and anti-PC antibodies in patients with SLE is unclear. One possibility is that a higher burden of apoptotic cells in patients with SLE leads to increased consumption of anti-PC and anti-MDA autoantibodies. Alternatively, patients with SLE might have an as-yet unidentified primary deficiency that leads to decreased production of these protective autoantibodies. The relationship of IgM anti-MDA and anti-PC antibodies to other potentially pathogenic autoantibodies, such as anti-cardiolipin antibodies, is also unclear. Moreover, the effect of SLE-targeted therapies on anti-PC and anti-MDA antibodies is unknown, particularly for frequently used treatments that specifically target B cells. Finally, the intriguing finding that autoantibodies against mediators of cardiovascular disease are generated by the adaptive immune system (through a mechanism involving T-cell help) suggests that a certain level of ‘protective autoimmunity’ is tolerated in healthy individuals but that this process becomes dysregulated in patients with SLE who have atherosclerosis. Further studies are required to determine the contributions of the adaptive and innate immune systems, the mechanisms of protective autoantibody generation and maintenance, and the effects of current and future therapies on the levels and functionality of protective autoantibodies in SLE.
Science Photo Library/Alamy Stock Photo
Acknowledgements
The authors are supported by NIH National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) grants R01AR063754–01A1 (M.M.) and K01-AR-059095 (B.S.).
Footnotes
Competing interests statement
The authors declare no competing interests.
Contributor Information
Maureen McMahon, Division of Rheumatology, David Geffen School of Medicine, University of California, Los Angeles, 32–59 Rehab Center, 1000 Veteran Avenue, Los Angeles, California 90095, USA.
Brian Skaggs, Division of Rheumatology, David Geffen School of Medicine, University of California, Los Angeles, 32–59 Rehab Center, 1000 Veteran Avenue, Los Angeles, California 90095, USA.
References
- 1.Rahman M et al. IgM antibodies against malondialdehyde and phosphorylcholine are together strong protection markers for atherosclerosis in systemic lupus erythematosus: regulation and underlying mechanisms. Clin. Immunol 166–167, 27–37 (2016). [DOI] [PubMed] [Google Scholar]
- 2.Sthoeger Z, Sharabi A & Mozes E Novel approaches to the development of targeted therapeutic agents for systemic lupus erythematosus. J. Autoimmun 54, 60–71 (2014). [DOI] [PubMed] [Google Scholar]
- 3.Gronwall C et al. IgM autoantibodies to distinct apoptosis-associated antigens correlate with protection from cardiovascular events and renal disease in patients with SLE. Clin. Immunol 142, 390–398 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gronwall C & Silverman GJ Natural IgM: beneficial autoantibodies for the control of inflammatory and autoimmune disease. J. Clin. Immunol 34, S12–S21 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chou MY et al. Oxidation-specific epitopes are dominant targets of innate natural antibodies in mice and humans. J. Clin. Invest 119, 1335–1349 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elkon KB & Silverman GJ Naturally occurring autoantibodies to apoptotic cells. Adv. Exp. Med. Biol 750, 14–26 (2012). [DOI] [PubMed] [Google Scholar]
- 7.Anania C et al. Increased prevalence of vulnerable atherosclerotic plaques and low levels of natural IgM antibodies against phosphorylcholine in patients with systemic lupus erythematosus. Arthritis Res. Ther 12, R214 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwartz M & Raposo C Protective autoimmunity: a unifying model for the immune network involved in CNS repair. Neuroscientist 20, 343–358 (2014). [DOI] [PubMed] [Google Scholar]
- 9.Fiskesund R et al. Low levels of antibodies against phosphorylcholine predict development of stroke in a population-based study from Northern Sweden. Stroke 41, 607–612 (2010). [DOI] [PubMed] [Google Scholar]
- 10.Fiskesund R et al. IgM phosphorylcholine antibodies inhibit cell death and constitute a strong protection marker for atherosclerosis development, particularly in combination with other auto-antibodies against modified LDL. Results Immunol. 2, 13–18 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]