Abstract
Aims
Using 90% of final height as a benchmark, we sought to develop a quick, quantitative and reproducible method of estimating skeletal maturity based on topographical changes in the distal femoral physis.
Patients and Methods
Serial radiographs of the distal femoral physis three years prior to, during, and two years following the chronological age associated with 90% of final height were analyzed in 81 healthy children. The distance from the tip of the central peak of the distal femoral physis to a line drawn across the physis was normalized to the physeal width.
Results
A total of 389 radiographs of the distal femur with corresponding Greulich and Pyle bone ages and known chronological ages were measured. Children reached 90% of final height at a mean age of 11.3 years (SD 0.8) for girls and 13.2 years (SD 0.6) for boys. Linear regression analysis showed higher correlation coefficent in predicting the true age at 90% of final height using chronological age + gender + central peak value (R2 = 0.900) than chronological age + gender (R2 = 0.879) and Greulich and Pyle bone age + gender (R2 = 0.878).
Conclusion
Chronological age + gender + central peak value provides more accurate prediction of 90% of final height compared with chronological age + gender and Greulich and Pyle bone age + gender.
The accurate estimation of skeletal maturity is important in several orthopaedic conditions, most notably in the assessment of leg-length discrepancy and scoliosis.1 Currently the methods which are used for estimating skeletal maturity include the Greulich and Pyle bone age atlas,2 the modified Sauvegrain method,3 Tanner– Whitehouse staging4 or simply using chronological age. Radiological staging using the Greulich and Pyle atlas, and Tanner–Whitehouse staging vary widely due to the subjective nature of interpretation,1 limiting their use and leading some to favour chronological age. However, based on different rates of growth in children, there are significant limitations to using chronological age.
Recently, Sanders et al5 compared the timing of the adolescent growth spurt’s peak height velocity (PHV) with normalized heights and three methods of measuring the skeletal maturity of the hand (Greulich and Pyle, the Fels 6 and Sander simplified methods7). Using two prospective longitudinal study populations of healthy children from North America, the Bolton-Brush Study Collection and the Berkleley Growth Study, the authors found consistent patterns of growth in both genders following the initiation of the growth spurt. The timing of PHV was found to correspond to 90% of the final height, although the latter was a more reliable and rapid method of quantifying the degree of skeletal maturity in individual children with full growth data.
During skeletal maturation, the topographical anatomy of the distal femoral physis has three major undulations, central peak, lateral ridge, and medial peak, that change with increasing age.8,9 Importantly, the central ridge decreases linearly in height relative to a line connecting the medial and lateral aspects of the physis.9 This anatomical parameter represents a potential landmark, easily identified on routine radiographs of the knee, that could be used to estimate skeletal maturity.
The purpose of this investigation was to determine if there is a quick, quantitative, and reproducible method for estimating skeletal maturity using readily available patient information including chronological age and gender and radiographic measures of the distal femoral central peak. We used 90% of final adult height as a benchmark and analyzed radiographs from the same historical collection that was used to establish the Greulich and Pyle atlas. Moreover, we sought to compare how using chronological age + gender + central peak value estimated the true age at 90% of final height to chronological age + gender, and Greulich and Pyle bone age + gender, both of which are commonly used in current practice. We hypothesized that this new methodology would predict the true age at 90% of final height better.
Patients and Methods
Radiological collection.
Anteroposterior (AP) radiographs of the left distal femur from 81 healthy children, 42 girls and 39 boys, were obtained from the Bolton-Brush Study Centre. This databank of successive radiographs of children growing up in Cleveland, Ohio between 1929 and 1942 involves healthy, almost exclusively Caucasian, middle- to upper-class children based on family income who were enrolled in the Brush Foundation Growth Study. All radiographs were digitized to allow enhancement and ease of organization.
Data collection.
Using the final height of each child, we calculated the chronological age associated with 90% of final height using the chronological timepoints above and below 90% of the final height. The chronological age at the time of 90% of final height was then calculated assuming linear growth between timepoints. Annual radiographs of the left knee taken three years prior to the chronological age at 90% of final height, at 90% of the final height and two years following the 90% mark were analyzed. For example, in a child reaching 90% of final height at age 12, radiographs from between the ages of 9 and 14 were analyzed.
For each radiograph, a digital horizontal line was first drawn along the distal femoral physis, connecting its medial and lateral borders, known as the physeal length, using Image J software (v1.49, National Institutes of Health, Bethesda, Maryland) (Fig. 1, yellow line). At each end we chose the midpoint between the most prominent portions of the metaphysis and epiphysis. The most superior aspect of the central peak on the metaphyseal side was then identified and the perpendicular distance from the peak to the physeal line was measured, to obtain the central peak height (Fig. 1, red line). We defined a positive value when the central peak was inferior to the physeal length line. We then divided the central peak height by the physeal line to obtain a standardized value, known as the central peak value. Radiographs of the hand and wrist from the children at the same chronological ages were used to calculate the Greulich and Pyle bone ages by a fellowship-trained pediatric endocrinologist expert (DRW) in the technique, using standard methodology.2
Fig. 1.
The distance from the central peak to a line between the medial and lateral aspects of the distal femoral physis (red line) was divided by the width of the physis (yellow line) to obtain the standardized central peak value, as measured in a 12-year-old girl on an anteroposterior radiograph. The physeal length line is drawn from points halfway between the ends of the metaphysis and epiphysis. The central peak height is drawn from this line to the edge of the metaphyseal side of the physis.
Radiographs were excluded if they were of poor quality, preventing reliable measurements of the central peak or the Greulich and Pyle bone age. Measurements of the central peak value were tested for intraclass correlation coefficient (ICC) in four children (24 radiographs) by two authors (DMK, RWL). An ICC of < 0.4 was considered poor, between 0.4 and 0.75 good and > 0.75 excellent.10,11
Statistical analysis.
The true age at 90% of final height was compared to estimates obtained using five methods: 1) chronological age + gender; 2) Greulich and Pyle bone age + gender; 3) chronological age + gender + central peak value; 4) Greulich and Pyle bone age + chronological age + gender; and 5) Greulich and Pyle bone age + chronological age + gender + central peak value. For each method, linear regression analysis was used to derive an equation to predict the years off from 90% of final height for both girls and boys, where girls were given value of 1 and boys a value of 0 (Table I) This was done to avoid an unfair advantage towards central peak value, which had to be mathematically optimized to the data set as it is a new parameter. By using the same linear regression approach for each parameter, all competing methods were mathematically optimized to the data set for fair comparison.
Table I.
Derived equations to predict years from 90% from final height
| Known variables | Equation |
|---|---|
| Chronological age, gender: | 2.002 + (0.843 × chronological age) + (−0.342 × gender) |
| Greulich and Pyle bone age, gender | 3.193 + (0.776 × Greulich and Pyle bone age) + (−0.903 × gender) |
| Chronological age, gender, central peak value | 3.495 + (15.409 × central peak value) + (0.658 × chronological age) + (−0.661 × gender) |
| Greulich and Pyle bone age, chronological age, gender | 1.92 + (0.453 × chronological age) + (0.41 × Greulich and Pyle bone age) + (−0.535 × gender) |
| Greulich and Pyle bone age, chronological age, gender, central peak value | 2.692 + (7.836 × central peak value) + (0.419 × chronological age) + (0.347 × Greulich and Pyle bone age) + (−0.668 × gender) |
Using each equation, we examined how well the estimated age at 90% of final height compared with the true age at 90% of final height. The mean discrepancy from the true age at 90% of final height was calculated, along with the percentage of radiographs in which the estimated age at 90% of final height was greater than one year off from the true age at 90% of final height. Repeated measures analysis of variance was performed to examine the differences in estimated age at 90% of final height in each method when compared with chronological age + gender + central peak value. Statistical analysis was performed using SPSS version 23 (IBM, Armonk, New York). A p-value of less than 0.5 was used to determine statistical significance.
Results
A total of 389 AP radiographs of the left distal femur from the 81 children meeting the inclusion criteria were measured to determine the central peak value (Table II). Similarly, 389 AP radiographs of the left wrist and hand from the same timepoints as the distal femoral radiographs were used to determine the Greulich and Pyle bone ages. Patients reached 90% of final height at a mean age of 11.3 years (SD 0.8) for girls and 13.2 years (SD 0.6) for boys. The mean number of radiographs per child was 4.8 (SD 1.2, 1 to 6) with 52 (65%) having > five radiographs and 12 (15%) having < three. A total of 62 radiographs (16%) had skeletal ages which were more than one year off from chronological age, while 70 radiographs (18%) had a skeletal age which was more than one year off from true skeletal age based on 90% of final height.
Table II.
Characteristics of the children
| Patients, n | Radiographs, n | Mean radiographs per patient (SD) | |
|---|---|---|---|
| Boys | 39 | 195 | 4.6 (1.5) |
| Girls | 42 | 194 | 5.0 (0.9) |
| Total | 81 | 389 | 4.8 (1.2) |
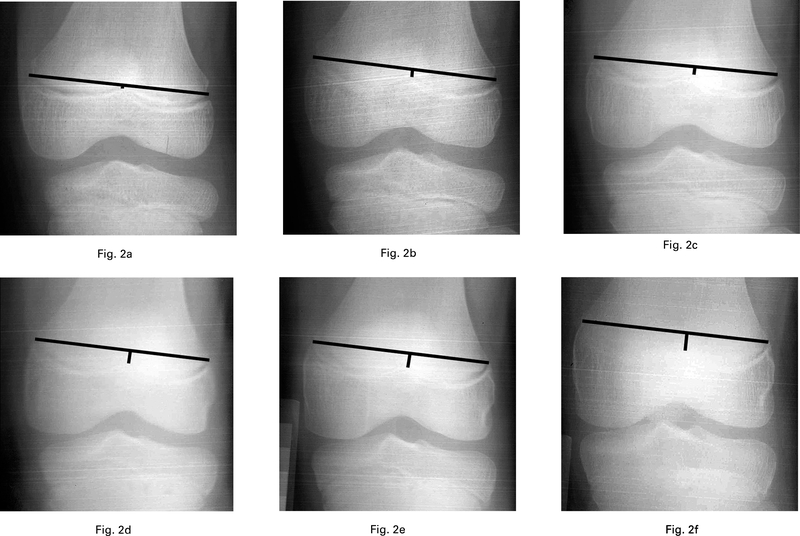
The overall mean central peak value at 90% of final height was 0.064 (SD 0.01), corresponding to a Greulich and Pyle bone age of 12.3 years (SD 1.1), while the central peak value increased for both boys and girls with increasing chronological age (Fig. 2, Table III). The ICC was 0.944 for central peak values, indicating excellent inter-relator reliability. The age of 90% of final height estimates using chronological age + gender + central peak value yielded a significantly lower mean discrepancy in years when compared with chronological age + gender (p < 0.001) while providing comparable values with Greulich Pyle bone age + gender (p = 0.72) (Table IV). However, estimates using Greulich and Pyle bone age + chronological age + gender, and Greulich and Pyle bone age + chronological age + gender + central peak value yielded higher correlation values, statistically significantly so for Greulich and Pyle bone age + chronological age + gender + central peak value. The percentage of radiographs in which the estimated age at 90% of final height was more than one year off from the true age at 90% of final height was lower using chronological age + gender + central peak value (10% of radiographs) compared with chronological age + gender (12%) and Greulich Pyle bone age + gender (13%). R2 values followed the same pattern, as shown in Table IV.
Fig. 2.
Serial anteroposterior radiographs showing increasing central peak height relative to the physeal line with increasing age in a boy when aged a) eight, b) nine, c) ten, d) 11, e) 12, and f) 13 years.
Table III.
Mean central peak value based on years from 90% of final height
| Years from 90% of final height | ||||||
|---|---|---|---|---|---|---|
| −3 | −2 | −1 | 0 | 1 | 2 | |
| Mean central peak value, mm (SD) | ||||||
| Boys | 0.023 (0.02) | 0.036 (0.02) | 0.048 (0.02) | 0.064 (0.01) | 0.080 (0.01) | 0.090 (0.02) |
| Girls | 0.017 (0.02) | 0.036 (0.02) | 0.049 (0.02) | 0.064 (0.01) | 0.074 (0.02) | 0.088 (0.02) |
| Boys and girls | 0.020 (0.02) | 0.036 (0.02) | 0.049 (0.02) | 0.064 (0.01) | 0.077 (0.02) | 0.089 (0.02) |
| Mean Greulich and Pyle bone age, yrs (SD) | ||||||
| Boys | 10.3 (0.2) | 11.3 (0.2) | 12.3 (0.2) | 13.3 (0.2) | 14.3 (0.2) | 15.2 (0.2) |
| Girls | 8.3 (0.2) | 9.3 (0.4) | 10.3 (0.4) | 11.3 (0.4) | 12.3 (0.4) | 13.4 (0.2) |
| Boys and girls | 9.4 (1.0) | 10.3 (1.0) | 11.3 (1.1) | 12.3 (1.1) | 13.2 (1.0) | 14.3 (1.0) |
Table IV.
Comparison between predicted versus true age at 90% of final height
| Chron. age + gender |
G&P + gender | CPV + chron. age + gender |
G&P + chron. age + gender |
G&P + chron. age + gender + CPV |
|
|---|---|---|---|---|---|
| Mean discrepancy from true age at 90% of final height, yrs (SD) | 0.53 (0.40) | 0.51 (0.43) | 0.48 (0.37) | 0.43 (0.33) | 0.33 (0.23) |
| p-value compared with CPV + gender + chron. age* | < 0.001 | 0.72 | N/A | 0.04 | < 0.001 |
| ANOVA | < 0.001 | 0.96 | N/A | 0.38 | < 0.001 |
| % of radiographs > 1 yr off | 13% | 12% | 10% | 7% | 1% |
| R2 | 0.879 | 0.878 | 0.900 | 0.919 | 0.924 |
chron., chronological; G&P, Greulich and Pyle bone age; CPV, central peak value; ANOVA, anaylsis of variance
Discussion
The assessment of skeletal maturity is important in paediatric patients, in order to evaluate the amount of remaining growth. Such information is relevant for preoperative planning prior to surgery for conditions in which the degree of skeletal maturity is pertinent, such as anterior cruciate ligament (ACL) reconstruction and the treatment of leg-length discrepancy and scoliosis. Currently, qualitative radiographic methods represent the benchmark for determining skeletal maturation. These traditional methods have the disadvantage of being less practical, as they are complex and time-intensive.1 The findings by Sanders et al5 of the coincidence of PHV with 90% of final height in boys and girls offers a new standard for quantifying skeletal maturity. Using these data, with measurements of the distal femoral physis, to calculate the central peak value represents a quick, quantitative and easy way of measuring remaining growth. When used with chronological age and gender, this method provided better estimation of skeletal maturity than Greulich and Pyle bone age, the current method considered to be the benchmark.
The distal femoral physis is the fastest growing physis in the body with a rate of 1.0 cm/year.12 Previous investigations into its topographical anatomy have revealed a distinctive pattern that changes with increasing age.8,9 A study by Ngyuen et al8 involving 36 cadaveric femora in children aged between three and 18 years found that, with increasing age, there was a decrease in the radiographic height of the central peak’s position relative to a line connecting the medial and lateral aspects of the physis (R2 = 0.75), identical to the physeal line used in this study. They noted that identifying the central peak on lateral radiographs was more difficult with correlations for the central peak being less consistent (ICC = 0.62). Changes in the topographical anatomy of the distal femoral physis, specifically the central peak, thus reflect skeletal maturation in the growing child and are best seen on anteroposterior images.
The Greulich and Pyle bone age relies on the assessment of radiographs of the wrist and hand with comparison to standard templates that best match the radiograph.1 This assessment has high interobserver variability.1 Other authors have also pointed to the lack of representation of skeletal ages in the atlas, specifically 11.5 and 12.5 years in girls and 14.5 years in boys, and the difficulty in assessing radiographs in girls between 11 and 13 years, and boys between 13 and 15 years of skeletal age,13 age ranges that are highly clinically relevant. The authors also found that the use of the Greulich and Pyle bone age provided estimates that were comparable to those provided using only chronological age.
We found, in this study, that the true age of 90% of final height was more accurately predicted using properly performed Greulich and Pyle bone age + gender when compared with chronological age + gender. Furthermore, estimates of the true age at 90% of final height using chronological age + gender + central peak value were more accurate compared with chronological age + gender, while being comparable to those obtained using Greulich and Pyle bone age + gender, suggesting that our more simple and quantitative system may be as effective in estimating skeletal maturity as the current standard of Greulich and Pyle. The practical ease of measuring the central peak value, compared with the many complicated morphologies required for the Greulich and Pyle bone age, points to a benefit in using the central peak value in the clinical setting.
On the other hand, using a combination of methods, such as Greulich and Pyle bone age + chronological age + gender, or Greulich and Pyle bone age + chronological age + gender + central peak value, yields even more accurate estimates, suggesting that the Greulich and Pyle itself can be further optimized by incorporating chronological age, and further still by adding the central peak value. The central peak value method proposed in this study represents, to our knowledge, the first purely quantitative method for estimating skeletal maturity. By offering a purely quantitative system with two quick and simple linear measurements, this distal femoral system represents a practical alternative for grading skeletal maturity. In contrast, the Greulich and Pyle atlas has significant limitations given the need for specialized knowledge of the system and the longer time of grading, both of which can significantly limit its use. It is important to note that our Greulich and Pyle measurements were made by an endocrinologist with no time pressures, which is different to the practical reality of how the bone age is often assessed clinically from radiographs of the left hand. We are therefore reluctant to recommend the combination of skeletal age grading using the maturity of the knee and Greulich and Pyle atlases in combination, despite the fact that this provided better accuracy in our study. Our short-term objective was, however, to determine whether the Greulich and Pyle system may be replaced in clinical situations where the distal femur has been imaged, and our long-term aim is to identify additional practical grading systems of skeletal maturity that may be used with the distal femoral system.
The importance of gender in the development of bone has been well documented. Girls traditionally have advanced bone ages compared with boys of the same chronological age, becoming more pronounced following the onset of puberty.2,14 However, the reasons behind these discrepancies is not known.15 The Greulich and Pyle bone age atlas takes these differences into consideration by using separate series of templates for girls and boys. We elected to include gender in our regression analysis for these reasons.
The amount of remaining growth in paediatric patients requires consideration for procedures in which the amount of remaining growth is crucial. Being able to estimate the amount of remaining growth may dictate the type of reconstruction performed in children with rupture of the anterior cruciate ligament16 and prediction of final height in those with leg length discrepancy.13,17 Use of the distal femur to grade skeletal maturity is particularly attractive in these conditions as radiographs of the knee are routinely undertaken.
The study had important limitations. Firstly, we were limited by the fact that the collection included only radiographs of the left femur and we were unable to correlate our measurements to those of the right distal femoral physis. However, the Brush Foundation had strict inclusion criteria and we would not anticipate a great deal of bilateral asymmetry due to the healthy nature of each child. Secondly, we assume a selection bias to be present as the children were all healthy, almost entirely Caucasian, and from middle- to upper-income families. The measurements may not have been the same in children with different ethnic backgrounds, who have different rates of skeletal maturity compared with those from the Brush Foundation.18 Moreover, due to anatomical changes that may occur in the distal femoral physis, the measurements may not be the same in children suffering from a previous fracture, infection or tumour affecting the distal femoral physis,19–21 nor those with congenital limb deficiency. Lastly, all radiographs used in this study had been taken more than 70 years before the analysis was undertaken. There may have been subtle anatomical changes during this time and it is not known whether these measurements may be applicable to children today, and this warrants further investigation.
In conclusion, we found that 90% of ultimate adult height is a better predictor of true skeletal maturity compared with PHV, and its use as a new benchmark allows for the development of an improved grading system of skeletal maturity. Calculation of the mean discrepancy in years from the true age at 90% of final height showed that chronological age + gender + central peak value provides more accurate estimates compared with chronological age + gender, and comparable values to those obtained using Greulich and Pyle bone age + gender. To our knowledge, the central peak height represents the first purely quantitative parameter for estimating skeletal maturity, and offers a practical methodology that can may improve treatment in conditions in which skeletal maturity is an important factor.
Take home message:
-
–
90% of ultimate adult height is a better predictor of true skeletal maturity when compared to peak height velocity.
-
–
Use of chronological age + gender + central peak value provide more accurate estimates of 90% of final height compared to Greulich and Pyle Bone Age estimates.
-
–
This investigation demonstrates the first purely quantitative parameterfor estimating skeletal maturity.
Acknowledgements:
This study was supported by a grant provided by the Pediatric Orthopaedic Society of North America and the Case Western Reserve University Department of Orthopaedic Surgery.
Funding statement:
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Contributor Information
D. M. Knapik, University Hospitals Cleveland Medical Center, Cleveland, Ohio, USA and Rainbow Babies and Children’s Hospital at Case Western Reserve University, Cleveland, Ohio, USA..
J. O. Sanders, University of Rochester, Rochester, New York, USA.and Rainbow Babies and Children’s Hospital at Case Western Reserve University, Cleveland, Ohio, USA.
A. Gilmore, University Hospitals Cleveland Medical Center, Cleveland, Ohio, USA and Rainbow Babies and Children’s Hospital at Case Western Reserve University, Cleveland, Ohio, USA..
D. R. Weber, Division of Endocrinology and Diabetes, University of Rochester School of Medicine and Dentistry, Rochester, New York, USA.and Rainbow Babies and Children’s Hospital at Case Western Reserve University, Cleveland, Ohio, USA..
D. R. Cooperman, Department of Orthopaedics and Rehabilitation, Yale University, New Haven, Connecticut, USA.and Rainbow Babies and Children’s Hospital at Case Western Reserve University, Cleveland, Ohio, USA..
R. W. Liu, University Hospitals Cleveland Medical Center, Cleveland, Ohio, USA and Rainbow Babies and Children’s Hospital at Case Western Reserve University, Cleveland, Ohio, USA..
References
- 1.De Sanctis V, Di Maio S, Soliman AT, et al. Hand X-ray in pediatric endocrinology: skeletal age assessment and beyond. Indian J Endocrinol Metab 2014;18(Suppl 1):S63–S71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greulich WW, Pyle SI. Radiographic Atlas of Skeletal Development of the Hand and Wrist. Second ed. California: Stanford University Press, 1959. [Google Scholar]
- 3.Diméglio A, Charles YP, Daures JP, de Rosa V, Kaboré B. Accuracy of the Sauvegrain method in determining skeletal age during puberty. J Bone Joint Surg [Am] 2005;87-A:1689–1696. [DOI] [PubMed] [Google Scholar]
- 4.Tanner JM, Whitehouse RH, Marshall WA, Carter BS. Prediction of adult height from height, bone age, and occurrence of menarche, at ages 4 to 16 with allowance for midparent height. Arch Dis Child 1975;50:14–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanders JO, Qiu X, Lu X L, et al. The Uniform Pattern of Growth and Skeletal Maturation during the Human Adolescent Growth Spurt. Sci Rep 2017;7:16705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roche AF, Chumlea WC, Thissen D. Assessing the skeletal maturity of the handwrist: FELS method. Springfield, Illinois: Charles C. Thomas, 1988. [Google Scholar]
- 7.Sanders JO, Khoury JG, Kishan S, et al. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg [Am] 2008;90-A:540–553. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen CV, Greene JD, Cooperman DR, Liu RW. A radiographic study of the distal femoral epiphysis. J Child Orthop 2015;9:235–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu RW, Armstrong DG, Levine AD, et al. An anatomic study of the distal femoral epiphysis. J Pediatr Orthop 2013;33:743–749. [DOI] [PubMed] [Google Scholar]
- 10.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979;86:420–428. [DOI] [PubMed] [Google Scholar]
- 11.Fleiss JL. The Design and Analysis of Clinical Experiments. New York: WileyBlackwell, 1986. [Google Scholar]
- 12.Anderson M, Messner MB, Green WT. Distribution of lengths of the normal femur and tibia in children from one to eighteen years of age. J Bone Joint Surg [Am] 1964;46-A:1197–1202. [PubMed] [Google Scholar]
- 13.Canavese F, Charles YP, Dimeglio A. Skeletal age assessment from elbow radiographs. Review of the literature. Chir Organi Mov 2008;92:1–6. [DOI] [PubMed] [Google Scholar]
- 14.Mora S, Boechat MI, Pietka E, Huang HK, Gilsanz V. Skeletal age determinations in children of European and African descent: applicability of the Greulich and Pyle standards. Pediatr Res 2001;50:624–628. [DOI] [PubMed] [Google Scholar]
- 15.Gilsanz V Pediatric assessment of skeletal growth. Rev Esp Endocrinol Pediatr 2010;1 (Suppl):11–18. [Google Scholar]
- 16.Nawabi DH, Jones KJ, Lurie B, et al. All-inside, physeal-sparing anterior cruciate ligament reconstruction does not significantly compromise the physis in skeletally immature athletes: a postoperative physeal magnetic resonance imaging analysis. Am J Sports Med 2014;42:2933–2940. [DOI] [PubMed] [Google Scholar]
- 17.Cundy P, Paterson D, Morris L, Foster B. Skeletal age estimation in leg length discrepancy. J Pediatr Orthop 1988;8:513–515. [DOI] [PubMed] [Google Scholar]
- 18.Koc A, Karaoglanoglu M, Erdogan M, Kosecik M, Cesur Y. Assessment of bone ages: Is the Greulich-Pyle method sufficient for Turkish boys? Pediatr Int 2001;43:662–665. [DOI] [PubMed] [Google Scholar]
- 19.Arkader A, Warner WC Jr, Horn BD, Shaw RN, Wells L. Predicting the outcome of physeal fractures of the distal femur. J Pediatr Orthop 2007;27:703–708. [DOI] [PubMed] [Google Scholar]
- 20.Graham JM, Gross RH. Distal femoral physeal problem fractures. Clin Orthop Relat Res 1990;255:51–53. [PubMed] [Google Scholar]
- 21.Wall EJ, May MM. Growth plate fractures of the distal femur. J Pediatr Orthop 2012;32(Suppl 1):S40–S46. [DOI] [PubMed] [Google Scholar]