Abstract
Background
Catastrophizing, a coping style characterized by an exaggerated negative affect when experiencing or anticipating pain, is an important factor that adversely affects surgical outcomes. Various interventions have been attempted with the goal of reducing catastrophizing and, by extension, improving treatment outcomes. We performed a systematic review to determine whether catastrophizing can be altered in surgical patients and to present evidence for interventions aimed at reducing catastrophizing in this population.
Methods
Using a scoping design, we performed a systematic search of MEDLINE and Embase. Studies reporting original research measuring catastrophizing, before and after an intervention, on the Pain Catastrophizing Scale (PCS) or Coping Strategies Questionnaire (CSQ) were selected. Studies were assessed for quality, the nature of the intervention and the magnitude of the effect observed.
Results
We identified 47 studies that measured the change in catastrophizing score following a broad range of interventions in surgical patients, including surgery, patient education, physiotherapy, cognitive behavioural therapy, psychologist-directed therapy, nursing-directed therapy and pharmacological treatments. The mean change in catastrophizing score as assessed with the PCS ranged from 0 to −19, and that with the CSQ, from +0.07 to −13. Clinically important changes in catastrophizing were observed in 7 studies (15%).
Conclusion
Catastrophizing was observed to be modifiable with an intervention in a variety of surgical patient populations. Some interventions produced greater reductions than others, which will help direct future research in the improvement of surgical outcomes.
Abstract
Contexte
Le catastrophisme est un mode d’adaptation caractérisé par un affect démesurément négatif chez la personne qui éprouve ou s’attend à éprouver de la douleur et c’est un facteur important qui peut influer négativement sur les résultats chirurgicaux. Diverses interventions ont été tentées pour atténuer le catastrophisme et par extension, améliorer les résultats des traitements. Nous avons procédé à une revue systématique afin de déterminer s’il est possible de modifier le catastrophisme chez les patients de chirurgie et présenter des données probantes concernant les interventions visant à atténuer le catastrophisme chez cette population.
Méthodes
En utilisant un plan de délimitation de la portée, nous avons procédé à une interrogation systématique de bases de données MEDLINE et Embase. Les études portant sur des recherches originales d’évaluation du catastrophisme, avant et après une intervention, au moyen de l’échelle PCS (Pain Catastrophizing Scale) ou du questionnaire CSQ (Coping Strategies Questionnaire) ont été sélectionnées et elles ont été évaluées aux plans de la qualité, de la nature des interventions et de l’ampleur de l’effet observé.
Résultats
Nous avons recensé 47 études qui ont mesuré un changement au score du catastrophisme après un vaste éventail d’interventions chez des patients de chirurgie, notamment : chirurgie, enseignement au patient, physiothérapie, thérapie cognitivocomportementales, thérapie sous la supervision d’un psychologue, thérapie sous la supervision du personnel infirmier et traitements pharmacologiques. Le changement moyen au score du catastrophisme évalué à l’aide de l’échelle PCS était de 0 à –19, et à l’aide du questionnaire CSQ, de 0,07 à –13. Des changements cliniquement importants du catastrophisme ont été observés dans 7 études (15 %).
Conclusion
Le catastrophisme s’est révélé modifiable à l’aide d’interventions chez divers types de patients de chirurgie. Certaines interventions ont généré des réductions plus marquées, ce qui guidera la recherche future pour améliorer les résultats chirurgicaux.
Pain catastrophizing refers to a coping style characterized by an exaggerated negative affect when experiencing or anticipating pain. It includes components of rumination, magnification and helplessness.1 Catastrophizing is a common coping strategy in surgical patient populations.2,3 Levels of catastrophizing and its components vary among patients. High levels of preoperative catastrophizing are associated with greater postoperative pain, poorer patient-reported surgical outcomes and poorer overall patient satisfaction following surgery.4–7 The adverse effects of catastrophizing on surgical outcomes may also lead to increased use of health care services and higher costs to the health care system.8 In principle, if catastrophizing could be reduced, the potential to improve surgical outcomes exists.9–15 There is debate as to whether catastrophizing represents a fixed trait.16,17 It is also not clear which interventions are effective in reducing catastrophizing in surgical patients.12,18,19 The purposes of this review were to determine whether catastrophizing can be altered in surgical patients and to present the evidence regarding interventions that have been evaluated for their ability to reduce catastrophizing in this population.
Methods
Search strategy
We performed this scoping review in accordance with the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines for the reporting of observational studies. 20 We identified all potentially relevant articles by searching MEDLINE (1946 through May 2017) and Embase (1980 through May 2017) using 3 search themes:
Theme 1: The first search was done with the use of the Boolean operator “OR” to explode and map the medical subject headings “catastrophization” or the Emtree terms “catastrophization,” or the text words “catastrophiz*” or “catastrophis*” or “cope” or “coping.”
Theme 2: The second search was performed with the use of the Boolean operator “OR” to explode and map the medical subject headings “pain,” “pain management” or “pain perception,” the Emtree terms “pain” or “postoperative pain,” or the text word “pain.”
Theme 3: The third search was performed with the use of the Boolean operator “OR” to explode and map the Emtree term “surgical patient” or the text words “orthop?edic*” or “surg*.”
We combined the results of the 3 searches using the Boolean operator “AND” and “NOT” the text words “p?ediatric*” or “child*” or “adolescen*.” This produced a list of potentially relevant abstracts for further review.
The search was enhanced by a hand search of the references of articles identified for the study. There were no date restrictions, but articles unavailable in English were excluded.
Study selection
We included all studies (full-text and conference abstracts) that reported original research that measured catastrophizing tendency at more than 1 time point during the study period using a validated instrument (Pain Catastrophizing Scale [PCS]1 or Coping Strategies Questionnaire,21 Catastrophizing subscale [CSQ-C]). The range of possible scores for the PCS and CSQ-C is 0–52 and 0–36, respectively. Studies were excluded if they did not involve an intervention for the management of catastrophizing, they measured catastrophizing at only 1 time point, they were purely synthesis/review papers, or the full text was not available and the relevant information could not be gleaned from the abstract. Both authors screened all identified titles and abstracts for eligibility, and studies selected by either author were included in a full-text review. If the title or abstract provided insufficient information to determine eligibility, the full-text article or published conference abstract was reviewed for inclusion. Disagreements regarding study inclusion following full-text review were resolved by consensus.
Data extraction and quality assessment
Data extraction was done independently by both authors for each of the studies selected for inclusion in the review. The following parameters were extracted: author, publication year, geographic location, sample size, study population, survey/instrument used to measure catastrophizing, initial and final catastrophizing scores (mean and standard deviation, and median), change in catastrophizing score, length of study period, type of catastrophizing-reduction intervention tested and mode of intervention. The primary outcome was change in catastrophizing score over the study period.
Study quality assessment focused on the research questions. Each study was assessed for study design, explicit statement of the research question, description of study sample and demographic characteristics, uniform application of inclusion/exclusion criteria, description of the intervention and statement of catastrophizing outcome (change). For each of these 6 criteria, study quality was assessed to be good (1) or fair/poor (0). The level of evidence was assessed according to published criteria.22
We collected and managed study data using REDCap (Research Electronic Data Capture) electronic data-capture tools. REDCap is a secure, Web-based application designed to support data capture for research studies.23
Data analysis
We identified or calculated the quantitative change in catastrophizing score for each included study. For studies using the PCS to measure catastrophizing, we evaluated the magnitude of change in catastrophizing score to determine whether it met or exceeded the minimal clinically important difference, which is known to be 9.1.24 The minimal clinically important difference for the CSQ was unavailable at the time of analysis.24
Results
Study selection
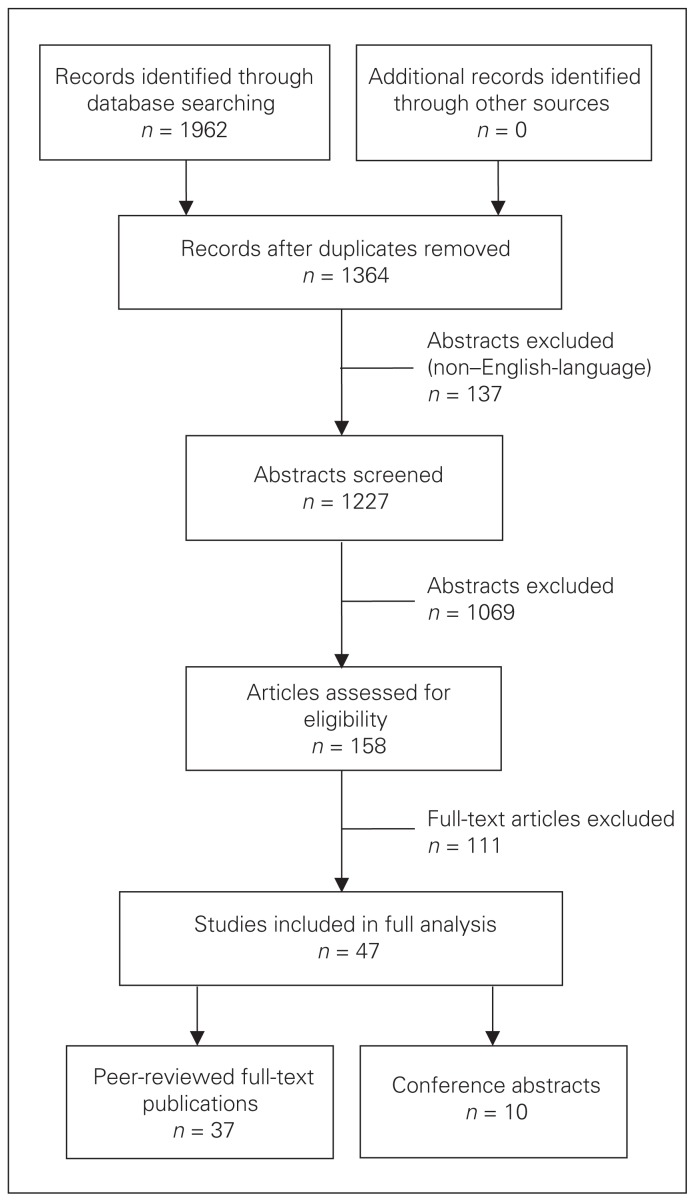
Fig. 1 outlines the process of study selection. Forty-seven studies (37 peer-reviewed publications and 10 conference abstracts) that evaluated a change in catastrophizing following an intervention were identified and were selected for inclusion and data extraction.8,25–69 Cohen’s κ of statistical agreement between the reviewers was 0.907 (p = 0.04). The final data set consisted of 5808 patients, with study sizes ranging from 1 to 1442 (mean 121). Table 1 shows the patient populations and number of patients for the included studies. Study designs included prospective cohort studies (15 studies), randomized controlled trials (14), prospective case series (7), case–control studies, (2) a retrospective cohort study (1), a retrospective case series (1) and a quasi-experimental design (1); in 6 studies, the study design was not described. Fig. 2 shows the geographic distribution of the included studies.
Fig. 1.
Flow diagram showing study selection.
Table 1.
Characteristics of included studies
| Patient population | No. of patients | Study |
|---|---|---|
| Chronic low back pain | 1609 | Barker et al.,27 Kovacs et al.,44 van Hooff et al.63 |
| Spine (operative) | 936 | Abbott et al.,25 Johansson et al.,41,42 Louw et al.,47,48 Monticone et al.,51 Ostelo et al.,52 Rolving et al.,57 Wibault et al.67,68 |
| Neuropathic pain | 789 | Bostick et al.29 |
| Total knee arthroplasty | 618 | Edwards et al.,11 Forsythe et al.,38 Hand et al.,39 Hirakawa et al.,40 Høvik et al.,5 Lluch et al.,46 Riddle et al.,56 Trost et al.,62 Wade et al.66 |
| Knee osteoarthritis | 358 | Broderick et al.,30 Therrien et al.60 |
| Herniorrhaphy | 275 | Powell et al.56,57 |
| Trauma | 184 | Vranceanu et al.66,67 |
| Cancer | 167 | Baudic et al.,28 Darnall et al.,33 Miyazaki et al.50 |
| Anterior cruciate ligament reconstruction | 148 | Chmielewski et al.,31,32 Tichonova et al.61 |
| Cardiac surgery | 116 | Khan et al.,6 Martorella et al.49 |
| Other surgical | 106 | Peters,53 Wideman et al.69 |
| Lateral epicondylitis | 91 | Lee et al.45 |
| Total hip arthroplasty | 90 | Farooq et al.37 |
| Chronic pain | 67 | Alappattu,24 Day et al.,35 Eyer et al.,36 Tetsunaga et al.59 |
| Noncardiac surgery | 44 | Clarke et al.33 |
Fig. 2.
Geographic distribution of included studies. The number in each bubble refers to the number of studies conducted in a given region.
Interventions
The review identified a broad range of interventions to reduce catastrophizing among surgical patients, including surgery, patient education, physiotherapy, cognitive behavioural therapy (CBT), psychologist-directed therapy, nursing-directed therapy and pharmacological treatments. A summary of the study-specific changes in catastrophizing score is shown in Table 2 (PCS) and Table 3 (CSQ-C). The change in mean catastrophizing score ranged from 0 to −19.6 in studies using the PCS and from +0.07 to −13 in studies using the CSQ-C. Clinically important changes in catastrophizing were observed in at least 7 studies (15%).
Table 2.
Measurement of changes in catastrophizing in studies using the Pain Catastrophizing Scale*
| Study | Mean score | Change | Study period | |
|---|---|---|---|---|
| Initial | Final | |||
| Alappattu26 | 18 | 8 | −10.0 | NR |
| Barker et al.27 | 19.6 | 18 | −1.6 | 3 wk |
| Baudic et al.28 | 14.6 | 21.5 | +6.9 | 1 yr |
| Bostick et al.29 | 22.2 | 17.8 | −4.4 | 6 mo |
| Chmielewski et al.31 | 3.7 | 2.5 | −1.2 | 9 wk |
| Chmielewski et al.32 | 11.2 | 4 | −7.2 | 12 wk |
| Clarke et al.33 | 19.5 | 13.0 | −6.5 | 2 h after drug administration |
| Eyer et al.36 | NR | NR | −11.8 | 12 mo |
| Forsythe et al.38 | 9.8 | 9.8 | 0.0 | 2 yr |
| Hirakawa et al.40 | 13 | 9.3 | −3.7 | 3 wk |
| Høvik et al.5 | 18.2 | 7.6† | −10.6† | |
| Khan et al.6 | 11.69 | 10.84 | −0.59 | 48 h |
| Lee et al.45 | 28.1 | 12.7 | −15.4 | 12 mo |
| Lluch et al.46 | 22.6 | 6 | −16.6 | 5 mo |
| Louw et al.47 | 23 | 13 | −10 | 1 d |
| Martorella et al.49 | 1.04 | 1.19 | +0.15 | 7 d |
| Miyazaki et al.50 | 24.2 | 7.1 | −14.1 | 3 mo |
| Monticone et al.51 | 24.8 | 12.6 | −12.2 | 1 yr |
| Ostelo et al.52 | 16.9 | NR | −7.3 | 1 yr |
| Riddle et al.56 | 29.7 | 10.1 | −19.6 | 2 mo |
| Tetsunaga et al.58 | 34.4 | 28 | −5.4 | 6 mo |
| Tetsunaga et al.59 | 33.7 | 28.9 | −4.8 | 6 mo |
| Tichonova et al.61 | 5.2 | 3.8 | −1.4 | Unclear (“after rehabilitation complete”) |
| Vranceanu et al.65 | 14.8 | 3.8 | −11.0 | 4–6 wk |
| Wade et al.66 | 14 | 7.32 | −6.68 | 6 mo |
| Wideman et al.69 | 25.4 | 17.45 | −7.95 | NR |
NR = not reported.
Only studies in which the study period was reported are included.
Median.
Table 3.
Measurement of changes in catastrophizing in studies using the Coping Strategies Questionnaire*
| Study | Mean score | Change | Study period | |
|---|---|---|---|---|
| Initial | Final | |||
| Abbott et al.25 | 15.5 | 11.0 | −4.5 | 2 yr |
| Broderick et al.30 | 7.17 | 7.24 | +0.07 | NR |
| Edwards et al.11 | 3.8 | 3.8 | 0.0 | 12 mo |
| Johansson et al.42 | 16 | 3.8 | −12.2 | 3 mo |
| Johansson et al.41 | 14† | 8† | −6† | 12 mo |
| Rolving et al.57 | NR | NR | −5 | 1 yr |
| Wibault et al.67 | 13 | 5 | −8 | 6 mo |
NR = not reported.
Only studies in which the study period was reported are included.
Median.
Surgery
In 18 studies,11,28,32,37–43,51,56,57,62,67–69 catastrophizing was measured pre- and postoperatively, which made surgery the intervention. These studies included a diverse set of surgical populations including patients undergoing total knee arthroplasty, total hip arthroplasty, spine surgery and reconstruction of the anterior cruciate ligament, surgery for cancer, herniorrhaphy and cardiac surgery. The mean change in catastrophizing score as assessed with the PCS ranged from 0 to −19.6, with 4 studies showing clinically important reductions (> 9.1 points). The mean change in catastrophizing score reported with the CSQ ranged from 0 to −13. Some of the surgical interventions studied were combined with interventions such as physiotherapy,51,67,69 small classroom group sessions57 and telephone counselling. 56 Of the 4 studies with clinically important reductions in catastrophizing, 1 used a combination of surgery, physiotherapy and CBT in a patients undergoing spine fusion surgery for lumbar spondylolisthesis and stenosis,51 1 evaluated total knee replacement supplemented with a psychologist-directed intervention,56 and 2 evaluated only the effects of the surgical intervention alone following knee replacement and lumbar disc surgery.5,42
Patient education
Ten studies evaluated the effect of patient education in reducing catastrophizing.8,30,34,36,46–49,57,59,60 These studies included patients presenting for cardiac surgery, knee osteoarthritis, chronic pain, breast cancer, knee replacement and spine surgery. The mean change in catastrophizing score as assessed with the PCS ranged from 0 to −16.6, and that reported with the CSQ ranged from 0 to −5.0. Two studies using the PCS showed clinically important reductions in catastrophizing.46,47 The first study involved a neuroscience pain-education intervention supplemented with physiotherapy.46 Educational material concerned the pain system, differences between acute and chronic pain, nervous system plasticity, emotions, stress and pain behaviours. The control group received standard care, and the treatment and control groups followed the same physiotherapy protocol postoperatively. The second study consisted of a one-on-one session with a physical therapist, focusing on pain reconceptualization and the teaching of cognitive nerve desensitization techniques.47 With both interventions, supplemental print materials were used.11,36
Physiotherapy
Nine studies used physiotherapy interventions to reduce catastrophizing.8,25,31,46,51,52,58,59,67,68 These studies were performed in patients with operative spinal disease, chronic low-back pain and chronic pain, and those presenting for knee replacement and reconstruction of the anterior cruciate ligament. The mean change in catastrophizing score ranged from −2.5 to −16.6 (PCS) and −6.5 to −8.0 (CSQ). Two studies using the PCS showed clinically important improvements in catastrophizing.46,51 One intervention combined surgery, physiotherapy and CBT.51 The physiotherapy component consisted of active range of motion, stretching and postural control, aimed at improving motor control of the spine and pelvis in patients presenting with lumbar radiculopathy. The other intervention, in patients with knee osteoarthritis, involved knee joint mobilization using pain as a guide, supplemented with neuroscience patient education.46
Psychologist-directed interventions and cognitive behavioural therapy
Twelve studies used CBT interventions.8,25,35,36,51,56–59,63,65,67 They included patients presenting with operative spine disease, chronic low-back pain, chronic pain and orthopedic trauma, and those undergoing knee replacement and spine surgery. The mean change in catastrophizing score as assessed with the CSQ ranged from −5 to −8. The mean change in catastrophizing score reported with the PCS ranged from −1.5 to −19.6, with 3 studies showing clinically important changes.51,56,65 In 1 study, the investigators used surgery, physiotherapy and CBT, including preoperative explanation of the fear-avoidance model and training, in patients undergoing surgical lumbar fusion to ensure a gradual psychological response to catastrophizing behaviours. 51 The second study used CBT and relaxation response exercises focusing on cognitive restructuring of pain sensation and breathing control/progressive muscle relaxation in patients with orthopedic trauma.65 Both studies included participation in 4 or more 1-hour sessions with a psychologist. The third study supplemented knee replacement surgery with training in pain-coping skills provided during 6 telephone sessions and 2 face-to-face sessions with a trained psychologist, spread evenly over the perioperative period.56 The cohort was compared to a historical data set of patients who had undergone knee replacement and had completed the PCS preoperatively. Clinically important reductions in catastrophizing were observed in both the intervention and control groups. The historical cohort did not receive any intervention but did show a clinically important decrease in catastrophizing scores (mean −9.3). This suggests that the effect of surgery may have been greater than that of the intervention.
Nursing-directed interventions
Three studies in patients with osteoarthritis, chronic pain and chronic low-back pain evaluated a nursing-directed intervention to reduce catastrophizing.8,30,58,59 The interventions were nursing-directed training in pain-coping skills,30 patient-specific treatment at a “liaison clinic” for intractable chronic pain58,59 and patient-specific care from a transitional pain service.8 The mean change in catastrophizing score reported with the PCS ranged from −2.5 to −5.4. One study that used the CSQ showed mean changes in catastrophizing score of +0.07 and −1.36 in the control and experimental groups, respectively.30 None of the studies resulted in a clinically important reduction in catastrophizing.
Pharmacological interventions
Two studies involved pharmacological interventions.8,33,50 One included a broad range of surgical patients (except those undergoing cardiac surgery),33 and the other included patients undergoing surgical treatment for lung cancer.50 The mean change in catastrophizing score as assessed with the CSQ ranged from −6.5 to −14.1, and that with the PCS ranged from −5.2 to −14.1. In 1 study, a standardized dosage of pregabalin was administered immediately postoperatively, and a clinically important reduction in catastrophizing was observed.50 In the other study, the pharmacologic intervention consisted of administration of 1200 mg of gabapentin immediately postoperatively, but this did not produce a clinically significant result.8,33
Quality assessment and levels of evidence
Of the 47 studies, 8 had level I evidence, 16 had level II evidence, 11 had level II evidence, 8 had level IV evidence, and 3 had level V evidence; in 1 case, the level of evidence was unclear. The results of the quality assessment are presented in Appendix 1 (available at canjsurg.ca/015417-a1). Quality scores ranged from 0 to 6 (mean 4.3 [standard deviation 1.9], median 5).
Discussion
We observed that, following a range of interventions, catastrophizing scores decreased in the 47 studies identified, with 7 studies (15%) showing a clinically important reduction. This suggests that catastrophizing is not a fixed trait but, rather, one that can be modified in surgical patients.
If catastrophizing tendencies can be reduced, direct interventions for surgical patients may be a means to improve overall outcomes. It is also be important for surgeons to remember that the very act of treating a disease with surgery may allow catastrophizing to decrease over time. Our review shows that interventions to decrease catastrophizing is a topic of interest around the world, and many teams in multiple surgical disciplines are approaching this topic from several patient, cultural and systemic perspectives. Thematically similar work conducted in different environments enhances the ability to apply and translate such work broadly.
There was considerable variation in effect within a given category of catastrophizing-reduction intervention. For example, not all educational or psychological interventions produced a clinically important change in catastrophizing. There are at least 2 factors contributing to this. First, there was inevitably variation in the patients in each sample, and some variation in response to an intervention is expected. Second, the specific details of the individual interventions may be critical to their success or failure, and this remains important for researchers to consider when designing future interventions or translating the results of these studies.
The first step has been achieved toward the ultimate goal of improving surgical outcomes through coherent management of factors such as pain catastrophizing. There exist interventions that appear to be able to produce clinically important reductions in catastrophizing in surgical patients. The first important knowledge gap relates to the generalizability and reproducibility of the effective interventions and their results. Studying the same protocols in other groups of patients at the same centres and in other centres would provide important insight as to whether an intervention is worthy of broader application for this purpose. Comparison of different interventions will also help indicate which interventions provide the most benefit.
The second knowledge gap relates to the ability to favourably change disease-specific outcomes in addition to reducing levels of catastrophizing by means of the interventions identified. It is also not clear how long the reduction in catastrophizing lasts after the intervention. Ideally, 1 intervention would produce long-term changes in patient coping styles, but it is possible that a given intervention may be required before every surgical procedure in those at risk.
A third knowledge gap involves the economics of these interventions. Some of the most successful interventions also required the most patient and system resources. To justify the adoption of these catastrophizing-reduction interventions into routine care, the benefits must outweigh the costs, and the resources need to be available to provide these interventions on an ongoing basis to everyone who would benefit.
Finally, further research is needed into whether a “one-size-fits-all” approach to catastrophizing-reduction interventions in surgical patients is appropriate. Patients undergoing a range of surgical procedures, coming from various life situations, may require disease-specific interventions customized to their circumstances.
Limitations
Because of the diversity manifest in the included studies, pooling the data for meta-analysis was not appropriate or feasible. Differences in interventions in the same category, differences in study design and differences in how catastrophizing outcomes were reported all contribute to this. Our ability to draw conclusions about the relative effectiveness of the interventions was also limited by the fact that none of the studies directly compared interventions, and some combined interventions.
Conclusion
Pain catastrophizing is a recognized negative prognostic factor for patient-reported surgical outcomes. It appears that catastrophizing can be substantially reduced through a range of interventions such as surgery, physiotherapy, CBT and even pharmacotherapy. It remains to be determined which catastrophizing-reduction interventions are the most effective and whether such improvements will result in overall better surgical and general patient health outcomes.
Acknowledgements
The authors acknowledge Alberta Health Services and the Surgery Strategic Clinical Network for studentship funding and support of this project.
Footnotes
Competing interests: None declared.
Contributors: Both authors designed the study, acquired and analyzed the data, wrote and reviewed the article, and approved the final version for publication.
References
- 1.Sullivan MJL. The Pain Catastrophizing Scale. User manual. [accessed 2017 June 27]. Available: http://sullivan-painresearch.mcgill.ca/pdf/pcs/PCSManual_English.pdf.
- 2.Craner JR, Gilliam WP, Sperry JA. Rumination, magnification, and helplessness: How do different aspects of pain catastrophizing relate to pain severity and functioning? Clin J Pain. 2016;32:1028–35. doi: 10.1097/AJP.0000000000000355. [DOI] [PubMed] [Google Scholar]
- 3.Jackson T, Tian P, Wang Y, et al. Toward identifying moderators of associations between presurgery emotional distress and postoperative pain outcomes: a meta-analysis of longitudinal studies. J Pain. 2016;17:874–88. doi: 10.1016/j.jpain.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 4.Pinto PR, McIntyre T, Ferrero R, et al. Predictors of acute postsurgical pain and anxiety following primary total hip and knee arthroplasty. J Pain. 2013;14:502–15. doi: 10.1016/j.jpain.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 5.Høvik LH, Winther SB, Foss OA, et al. Preoperative pain catastrophizing and postoperative pain after total knee arthroplasty: a prospective cohort study with one year follow-up. BMC Musculoskelet Disord. 2016;17:214. doi: 10.1186/s12891-016-1073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan RS, Ahmed K, Blakeway E, et al. Catastrophizing: a predictive factor for postoperative pain. Am J Surg. 2011;201:122–31. doi: 10.1016/j.amjsurg.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 7.Teunis T, Bot AG, Thornton ER, et al. Catastrophic thinking is associated with finger stiffness after distal radius fracture surgery. J Orthop Trauma. 2015;29:e414–20. doi: 10.1097/BOT.0000000000000342. [DOI] [PubMed] [Google Scholar]
- 8.Katz J, Weinrib A, Fashler SR, et al. The Toronto General Hospital Transitional Pain Service: development and implementation of a multidisciplinary program to prevent chronic postsurgical pain. J Pain Res. 2015;8:695–702. doi: 10.2147/JPR.S91924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alodaibi FA, Minick KI, Fritz JM. Do preoperative fear avoidance model factors predict outcomes after lumbar disc herniation surgery? A systematic review. Chiropr Man Therap. 2013;21:40. doi: 10.1186/2045-709X-21-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bot AG, Doornberg JN, Lindenhovius AL, et al. Long-term outcomes of fractures of both bones of the forearm. J Bone Joint Surg Am. 2011;93:527–32. doi: 10.2106/JBJS.J.00581. [DOI] [PubMed] [Google Scholar]
- 11.Edwards RR, Haythornthwaite JA, Smith MT, et al. Catastrophizing and depressive symptoms as prospective predictors of outcomes following total knee replacement. Pain Res Manag. 2009;14:307–11. doi: 10.1155/2009/273783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim HJ, Park JW, Chang BS, et al. The influence of catastrophising on treatment outcomes after surgery for lumbar spinal stenosis. Bone Joint J. 2015;97-B:1546–54. doi: 10.1302/0301-620X.97B11.36016. [DOI] [PubMed] [Google Scholar]
- 13.Papaioannou M, Skapinakis P, Damigos D, et al. The role of catastrophizing in the prediction of postoperative pain. Pain Med. 2009;10:1452–9. doi: 10.1111/j.1526-4637.2009.00730.x. [DOI] [PubMed] [Google Scholar]
- 14.Ponsford J, Hill B, Karamitsios M, et al. Factors influencing outcome after orthopedic trauma. J Trauma. 2008;64:1001–9. doi: 10.1097/TA.0b013e31809fec16. [DOI] [PubMed] [Google Scholar]
- 15.Sullivan M, Tanzer M, Stanish W, et al. Psychological determinants of problematic outcomes following total knee arthroplasty. Pain. 2009;143:123–9. doi: 10.1016/j.pain.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 16.Darnall BD, Sturgeon JA, Kao MC, et al. From catastrophizing to recovery: a pilot study of a single-session treatment for pain catastrophizing. J Pain Res. 2014;7:219–26. doi: 10.2147/JPR.S62329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Domenech J, Sanchis-Alfonso V, Espejo B. Changes in catastrophizing and kinesiophobia are predictive of changes in disability and pain after treatment in patients with anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 2014;22:2295–300. doi: 10.1007/s00167-014-2968-7. [DOI] [PubMed] [Google Scholar]
- 18.Kroska EB. A meta-analysis of fear-avoidance and pain intensity: the paradox of chronic pain. Scand J Pain. 2016;13:43–58. doi: 10.1016/j.sjpain.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 19.Wertli MM, Burgstaller JM, Weiser S, et al. Influence of catastrophizing on treatment outcome in patients with nonspecific low back pain: a systematic review. Spine (Phila Pa 1976) 2014;39:263–73. doi: 10.1097/BRS.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 20.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 21.Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- 22.Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85-A:1–3. [PubMed] [Google Scholar]
- 23.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) — a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.George SZ, Valencia C, Beneciuk JM. A psychometric investigation of fear-avoidance model measures in patients with chronic low back pain. J Orthop Sports Phys Ther. 2010;40:197–205. doi: 10.2519/jospt.2010.3298. [DOI] [PubMed] [Google Scholar]
- 25.Abbott AD, Tyni-Lenne R, Hedlund R. Early rehabilitation targeting cognition, behavior, and motor function after lumbar fusion: a randomized controlled trial. Spine (Phila Pa 1976) 2010;35:848–57. doi: 10.1097/BRS.0b013e3181d1049f. [DOI] [PubMed] [Google Scholar]
- 26.Alappattu MJ. Pain and psychological outcomes after rehabilitative treatment for a woman with chronic pelvic pain with stage III cervical cancer: a case report. J Womens Health Phys Therap. 2013;37:97–102. doi: 10.1097/JWH.0000000000000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barker KL, Elliott CJ, Sackley CM, et al. Treatment of chronic back pain by sensory discrimination training. A phase I RCT of a novel device (FairMed) vs. TENS. BMC Musculoskelet Disord. 2008;9:97. doi: 10.1186/1471-2474-9-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baudic S, Jayr C, Albi-Feldzer A, et al. Effect of alexithymia and emotional repression on postsurgical pain in women with breast cancer: a prospective longitudinal 12-month study. J Pain. 2016;17:90–100. doi: 10.1016/j.jpain.2015.10.001. [DOI] [PubMed] [Google Scholar]
- 29.Bostick GP, Kamper SJ, Haanstra TM, et al. Pain expectations in neuropathic pain: Is it best to be optimistic? Eur J Pain. 2017;21:605–13. doi: 10.1002/ejp.962. [DOI] [PubMed] [Google Scholar]
- 30.Broderick JE, Keefe FJ, Bruckenthal P, et al. Nurse practitioners can effectively deliver pain coping skills training to osteoarthritis patients with chronic pain: a randomized, controlled trial. Pain. 2014;155:1743–54. doi: 10.1016/j.pain.2014.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chmielewski TL, George SZ, Tillman SM, et al. Low-versus high-intensity plyometric exercise during rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:609–17. doi: 10.1177/0363546515620583. [DOI] [PubMed] [Google Scholar]
- 32.Chmielewski TL, Zeppieri G, Jr, Lentz TA, et al. Longitudinal changes in psychosocial factors and their association with knee pain and function after anterior cruciate ligament reconstruction. Phys Ther. 2011;91:1355–66. doi: 10.2522/ptj.20100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Clarke H, Kirkham K, Orser BA, et al. Gabapentin reduces preoperative anxiety and pain catastrophizing scores prior to major surgery in highly anxious patients. Pain Res Manag. 2012;17:195. doi: 10.1007/s12630-013-9890-1. [DOI] [PubMed] [Google Scholar]
- 34.Darnall B, Wheeler A, Taub C, et al. An internet-based perioperative pain psychology treatment program: results of a randomized controlled trial in breast oncology surgery patients. J Pain. 2016;17( 4 Suppl):S106. [Google Scholar]
- 35.Day M, Thorn B, Ward L, et al. Preliminary findings of a cognitive-behavioral pain trial among rural minorities and non-minorities. J Pain. 2010;11(4 Suppl):S56. [Google Scholar]
- 36.Eyer J, Day M, Thorn B. A case study of response to group CBT or a potent pain education group for minority patients with chronic pain. J Pain. 2015;16(4 Suppl):S102. [Google Scholar]
- 37.Farooq A, Farooq D, Chaudhury S. Preoperative pain catastrophisation predicts higher pain and analgesia use during primary hip arthroplasty. Int J Surg. 2014;12(Suppl 3):S65. [Google Scholar]
- 38.Forsythe ME, Dunbar MJ, Hennigar AW, et al. Prospective relation between catastrophizing and residual pain following knee arthroplasty: two-year follow-up. Pain Res Manag. 2008;13:335–41. doi: 10.1155/2008/730951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hand M, Pejsa M, Pawar S, et al. Decreases in catastrophizing precede reductions in pain following total knee replacement. J Pain. 2015;16(4 Suppl):S97. [Google Scholar]
- 40.Hirakawa Y, Hara M, Fujiwara A, et al. The relationship among psychological factors, neglect-like symptoms and postoperative pain after total knee arthroplasty. Pain Res Manag. 2014;19:251–6. doi: 10.1155/2014/471529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Johansson AC, Linton SJ, Rosenblad A, et al. A prospective study of cognitive behavioural factors as predictors of pain, disability and quality of life one year after lumbar disc surgery. Disabil Rehabil. 2010;32:521–9. doi: 10.3109/09638280903177243. [DOI] [PubMed] [Google Scholar]
- 42.Johansson AC, Ohrvik J, Soderlund A. Associations among pain, disability and psychosocial factors and the predictive value of expectations on returning to work in patients who undergo lumbar disc surgery. Eur Spine J. 2016;25:296–303. doi: 10.1007/s00586-015-3820-6. [DOI] [PubMed] [Google Scholar]
- 43.Khan RS, Skapinakis P, Ahmed K, et al. The association between preoperative pain catastrophizing and postoperative pain intensity in cardiac surgery patients. Pain Med. 2012;13:820–7. doi: 10.1111/j.1526-4637.2012.01386.x. [DOI] [PubMed] [Google Scholar]
- 44.Kovacs FM, Seco J, Royuela A, et al. Spanish Back Pain Research Network. The prognostic value of catastrophizing for predicting the clinical evolution of low back pain patients: a study in routine clinical practice within the Spanish National Health Service. Spine J. 2012;12:545–55. doi: 10.1016/j.spinee.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 45.Lee DO, Gong HS, Kim JH, et al. The relationship between positive or negative phrasing and patients’ coping with lateral epicondylitis. J Shoulder Elbow Surg. 2014;23:567–72. doi: 10.1016/j.jse.2014.01.020. [DOI] [PubMed] [Google Scholar]
- 46.Lluch E, Duenas L, Falla D, et al. Preoperative pain neuroscience education combined with knee joint mobilization for knee osteoarthritis: a randomized controlled trial. Clin J Pain. 2018;34:44–52. doi: 10.1097/AJP.0000000000000511. [DOI] [PubMed] [Google Scholar]
- 47.Louw A, Diener I, Puentedura EJ. The short term effects of preoperative neuroscience education for lumbar radiculopathy: a case series. Int J Spine Surg. 2015;9:11. doi: 10.14444/2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Louw A, Puentedura EJ, Diener I, et al. Preoperative therapeutic neuroscience education for lumbar radiculopathy: a single-case fMRI report. Physiother Theory Pract. 2015;31:496–508. doi: 10.3109/09593985.2015.1038374. [DOI] [PubMed] [Google Scholar]
- 49.Martorella G, CÔté J, Racine M, et al. Web-based nursing intervention for self-management of pain after cardiac surgery: pilot randomized controlled trial. J Med Internet Res. 2012;14:e177. doi: 10.2196/jmir.2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miyazaki T, Sakai T, Sato S, et al. Is early postoperative administration of pregabalin beneficial for patients with lung cancer? Randomized control trial. J Thorac Dis. 2016;8:3572–9. doi: 10.21037/jtd.2016.12.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Monticone M, Ferrante S, Teli M, et al. Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial. Eur Spine J. 2014;23:87–95. doi: 10.1007/s00586-013-2889-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ostelo RWJG, de Vet HCW, Vlaeyen JWS, et al. Behavioral graded activity following first-time lumbar disc surgery: 1-year results of a randomized clinical trial. Spine (Phila Pa 1976) 2003;28:1757–65. doi: 10.1097/01.brs.0000083317.62258.e6. [DOI] [PubMed] [Google Scholar]
- 53.Peters M. Optimism as a resiliency for chronic pain. Eur J Pain. 2009;13:S7. [Google Scholar]
- 54.Powell R, Johnston M, Smith WC, et al. Psychological risk factors for chronic post-surgical pain after inguinal hernia repair surgery: a prospective cohort study. Eur J Pain. 2012;16:600–10. doi: 10.1016/j.ejpain.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 55.Powell R, Johnston M, Smith WC, et al. Rehabilitation following surgery: clinical and psychological predictors of activity limitations. Rehabil Psychol. 2013;58:350–60. doi: 10.1037/a0034660. [DOI] [PubMed] [Google Scholar]
- 56.Riddle DL, Keefe FJ, Nay WT, et al. Pain coping skills training for patients with elevated pain catastrophizing who are scheduled for knee arthroplasty: a quasi-experimental study. Arch Phys Med Rehabil. 2011;92:859–65. doi: 10.1016/j.apmr.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rolving N, Nielsen CV, Christensen FB, et al. Does a preoperative cognitive-behavioral intervention affect disability, pain behavior, pain, and return to work the first year after lumbar spinal fusion surgery? Spine (Phila Pa 1976) 2015;40:593–600. doi: 10.1097/BRS.0000000000000843. [DOI] [PubMed] [Google Scholar]
- 58.Tetsunaga T, Tetsunaga T, Nishida K, et al. Short-term outcomes of patients being treated for chronic intractable pain at a liaison clinic and exacerbating factors of prolonged pain after treatment. J Orthop Sci. 2017;22:554–9. doi: 10.1016/j.jos.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 59.Tetsunaga T, Tetsunaga T, Nishie H, et al. Establishment of a liaison clinic for patients with intractable chronic pain. J Orthop Sci. 2015;20:907–13. doi: 10.1007/s00776-015-0748-y. [DOI] [PubMed] [Google Scholar]
- 60.Therrien M, Fuentes A, Landry P, et al. Real-world clinical result from a multimodal management program for knee osteoarthritis. Osteoarthritis Cartilage. 2016;24(Suppl 1):S431. [Google Scholar]
- 61.Tichonova A, Rimdeikiene I, Petruseviciene D, et al. The relationship between pain catastrophizing, kinesiophobia and subjective knee function during rehabilitation following anterior cruciate ligament reconstruction and meniscectomy: a pilot study. Medicina (Kaunas) 2016;52:229–37. doi: 10.1016/j.medici.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 62.Trost Z, Niederstrasser N, Harrison J, et al. Predicting pain catastrophizing following total knee arthroplasty. J Pain. 2013;14(4 Suppl):S93. [Google Scholar]
- 63.van Hooff M, van Lankveld W, O’Dowd J, et al. Patients with longstanding low back pain improve on cognitive behavioral variables after a short, intensive pain management program. Eur J Pain Suppl. 2011;5:158. [Google Scholar]
- 64.Vranceanu AM, Bachoura A, Weening A, et al. Psychological factors predict disability and pain intensity after skeletal trauma. J Bone Joint Surg Am. 2014;96:e20. doi: 10.2106/JBJS.L.00479. [DOI] [PubMed] [Google Scholar]
- 65.Vranceanu AM, Hageman M, Strooker J, et al. A preliminary RCT of a mind body skills based intervention addressing mood and coping strategies in patients with acute orthopaedic trauma. Injury. 2015;46:552–7. doi: 10.1016/j.injury.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 66.Wade JB, Riddle DL, Thacker LR. Is pain catastrophizing a stable trait or dynamic state in patients scheduled for knee arthroplasty? Clin J Pain. 2012;28:122–8. doi: 10.1097/AJP.0b013e318226c3e2. [DOI] [PubMed] [Google Scholar]
- 67.Wibault J, Öberg B, Dedering A, et al. Neck-related physical function, self-efficacy, and coping strategies in patients with cervical radiculopathy: a randomized clinical trial of postoperative physiotherapy. J Manipulative Physiol Ther. 2017;40:330–9. doi: 10.1016/j.jmpt.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 68.Wibault J, Öberg B, Dedering A, et al. Structured rehabilitation in primary health care after surgery for cervical radiculopathy: treatment mediators in a randomized clinical trial. J Neurosurg Spine. 2018;28:1–9. doi: 10.3171/2017.5.SPINE16736. [DOI] [PubMed] [Google Scholar]
- 69.Wideman TH, Scott W, Martel MO, et al. Recovery from depressive symptoms over the course of physical therapy: a prospective cohort study of individuals with work-related orthopaedic injuries and symptoms of depression. J Orthop Sports Phys Ther. 2012;42:957–67. doi: 10.2519/jospt.2012.4182. [DOI] [PubMed] [Google Scholar]