Abstract
Objective
Community paramedicine (CP) is a model of community‐based health care being used around the world. Our objective was to study the patient perspective and valuation of this type of program to understand its potential value for primary care innovation in the future.
Study Setting
The EPIC community paramedicine program is a partnership between primary care physicians and specially trained community paramedics, designed to provide in‐home support for complex chronic disease patients in Ontario, Canada.
Study Design
As part of an ongoing clinical trial we designed an embedded qualitative evaluation using constructionist grounded theory methodology.
Data Collection Methods
Data collection included in‐depth interviews with 30 patients and/or family members and 60 hours of observation.
Principal Findings
The health care needs of this complex population are largely attributes that impact a patient's quality of life—including recognition of their vulnerability, providing a safety‐net in times of exacerbation and health education and accountability. This seems to be facilitated by a relationship with a dedicated provider that increases continuity of care.
Conclusions
Home‐based community paramedicine programs like EPIC appear to be able to create a patient‐centered, safe, responsive therapeutic relationship that is often not possible within the standard primary health care system.
Keywords: Community paramedicine, patient‐centered care, primary care, chronic disease qualitative
Almost a quarter (21.4 percent) of the population of Canada older than 20 has at least one major chronic condition (includes diabetes mellitus, cardiovascular disease, and chronic respiratory diseases) (Government of Canada 2017). However, the existing health care system in Canada, comprised of individual hospitals, primary care providers, and community‐based care initiatives, has been limited in its ability to successfully integrate different levels of care into an effective approach to disease management. As a result, individuals living with chronic disease are currently relying on the 911 system for care and accessing hospitals as the first point of contact for disease‐related exacerbations and symptomatology (McLeod et al. 2016). The three most common chronic diseases in Canada, diabetes mellitus (DM), congestive heart failure (CHF), and chronic obstructive pulmonary disease (COPD) are on the rise and cost the Canadian health care system billions of dollars every year, including the cost of 911 system utilization, emergency department (ED) visits, and hospitalizations (Elmslie 2012). The current structure of the health care system does not have the capacity to effectively care for complex chronic disease patients now or in the future. Accordingly, initiatives aimed at improving health care access, quality, and value have become a system priority.
One such strategy is the development of community‐based paramedic outreach programs in partnership with primary care, hospital emergency departments and long‐term care homes, and integrated with community resources. These programs are active in several regions of North America and Europe as a potential innovation that may reduce inappropriate use of emergency systems and improve health outcomes for vulnerable patients through redirection of existing resources and a modest investment in expanding paramedic scope of practice. Paramedics are well positioned to take on additional non‐emergency‐based roles given their experience working with physicians (sometimes under a delegation of medical acts model) to assess and treat people with acute and chronic illnesses. Research from the United Kingdom, the United States, and Canada assessing the value of community paramedics in primary care settings has demonstrated that paramedics with additional training can effectively and safely practice in different roles, and can independently perform specialized assessments and treatments that improve patient care (Mason et al. 2007; Abrashkin et al. 2016; Agarwal et al. 2017).
While these studies have looked at the quantitative impact of community‐based paramedic outreach programs in a variety of primary care settings, the impact of this model of care for different patient populations cannot be known from quantitative results alone. The dearth of qualitative studies (Martin, O'Meara, and Farmer 2016) has left understudied questions about patient and family experiences and changes in the roles, relationships, and routines that occur within health systems to accommodate this significant change in care delivery. To contribute to this gap in our understanding about the impact of community paramedicine as a model for chronic disease management, we sought to understand the experiences and perspectives of patients and families involved with the Expanding Paramedicine in the Community (EPIC) randomized trial in Ontario, Canada, as well as the ways in which such a model is shaped and enabled according to the needs and interests of program participants.
Method
Study Design
We conducted a qualitative substudy with patients and families participating in the EPIC program in two regions of southwestern Ontario (York Region and Grey County). Data analysis and the representation of our findings followed a modified constructionist grounded theory approach as described by Charmaz (2014) to support our goal of developing a conceptual model of the impact of community paramedicine. One of the strengths of grounded theory is the method's ability to theoretically examine what is actually going on in the substantive area of interest, rather than just describe what is happening (Glaser and Strauss 1967). Community paramedicine is a decidedly “patient‐centered” innovation and we chose this analytic approach in order to “center,” or give interpretive precedence to, what is important to patients and family members while participating in this alternative type of care delivery program.
The EPIC Model of Community Paramedicine
The Expanding Paramedicine in the Community (EPIC) program is a regional, community‐based chronic disease management strategy aimed at reducing hospital admission rates, emergency department visits, and 911 calls for patients living with three major chronic diseases: diabetes mellitus (DM), congestive heart failure (CHF), and chronic obstructive pulmonary disease (COPD). A full description of the EPIC model and study methods has been previously published elsewhere (Drennan et al. 2014). The primary study (a randomized control trial) was conducted in partnership with two paramedic services and four family health care teams and funded through a special funding allocation from the Ontario Ministry of Health and Long‐Term Care. Patients from the family health teams identified as high risk by their primary care physicians were approached to be enrolled in the program and randomized to the active (receive visits from a community paramedic) or control (usual primary care) groups. Each paramedic service dedicated four senior paramedics to be trained as full‐time community paramedics. Following a 6‐week intensive training course in chronic disease management (provided by Centennial College), they are connected with identified patients to conduct scheduled home visits at 3‐month intervals, as well as follow‐up and emergency home visits (on a 24 × 7 basis) to assess and treat patients under a medical delegation of the patients' primary care physicians. EPIC community paramedics address patient needs in their homes, identify and treat disease‐related symptoms before they escalate to emergency health problems, and refer patients to their primary care physician when necessary. Information and data collected during the EPIC visits are entered directly into the patient's EMR at the family health team to ensure consistent charting and communication within the health care team. Physicians were also available to paramedics by phone during normal business hours. At the discretion of the primary care physician, EPIC community paramedics also perform point of care testing for blood, urine, and ECGs with the goal of improving chronic disease management and reducing the rate of acute care hospitalization. Since 2013, 239 patients have received active treatment (community paramedicine visits) and there are eight community paramedics and 32 primary care physicians from four family health teams involved with the program.
Participant Recruitment
Patients of the participating family health teams who were receiving treatment from EPIC community paramedics (active group) were invited to voluntarily participate in the ethnographic observation and interview process for the qualitative study. We employed purposive sampling and sought participants who were most likely to contribute appropriate data in terms of relevance, range of perspectives, and depth (Patton 2002). Therefore, we included patients who had received at least three scheduled visits from the EPIC community paramedics and represented a range of characteristics (including gender, age, chronic condition, social economic status, and geography) and experiences with the program (including high and low total number of visits, and different types of visits, such as scheduled, follow up, and exacerbation visits). Patients randomized to the control group were not recruited as we were interested in patient's perspectives on the community paramedic care delivery model. The EPIC community paramedics contacted eligible patients by telephone and asked “if they would be willing to let a researcher observe their next regularly scheduled EPIC appointment and conduct a short in‐person interview afterwards.” Those who agreed were included in the sample. In addition, all eight of the EPIC community paramedics were included in the ethnographic observations for this study.
Research ethics approval was obtained from St. Michael's Hospital Research Ethics Board. Verbal consent was obtained from patients and the community paramedics for the observations, and written consent was obtained from patients and family members for the interviews.
Data Collection
Data from participant observation and in‐depth interviews were collected in York Region, Ontario, between October 2014 and January 2015, and in Grey County, Ontario, in October and November 2015. All data were collected by MBS, a medical sociologist, and trained qualitative researcher. Approximately 60 hours of participant observation were conducted during ride‐along with the EPIC community paramedic teams during scheduled in‐home patient appointments. Observation sessions lasted between 3 and 6 hours. Observations occurred immediately prior to, during, and following patient appointments and were focused on interactions and activities between the community paramedics and patients and their family members in the patients' homes. During the observation sessions, the researcher took detailed field notes and conducted informal or conversational interviews with the patients and their family members, as well as with the paramedics, to discuss activities, probe emerging issues, and ask questions in a naturalistic manner. The notes were later expanded to include the researcher's reflections on the data collected and preliminary analytic insights.
Single in‐depth interviews were also conducted with 40 individuals (30 patients and 10 family members). These were conducted in the home following the EPIC appointment and did not include the community paramedics. A semi‐structured interview guide developed by the study team and based on the literature, input of experts in Emergency Medicine, paramedicine, and qualitative research, and informed by the objectives of this study (Appendix SA2), was used to provide broad topic areas to guide the discussion. Interviews were conducted until the authors felt we had reached thematic saturation and that no new insights would be gleaned from talking with further participants (Francis et al. 2010). Our team collaboratively determined that saturation had been achieved through extensive team meetings and transcript review.
The average recorded interview with patients and their family members was 35 minutes in length (range 10–90 minutes). All interviews were scheduled in advance, conducted in‐person by a single researcher (MBS), digitally recorded, and transcribed verbatim by an external transcription service for analysis.
Data Analysis
Data analysis was carried out using a constant comparative approach to continuously monitor emerging themes and identify areas for further exploration (Charmaz 2014). Initial analysis of the first five interviews was carried out independently by two of the authors (KND and MBS). Through an ongoing series of meetings, an iterative process was undertaken, in which new transcripts were read and the coding framework evolved, with careful attention to the use of language in both participants' accounts and how our codes were named (Webster et al. 2013). The interview guide was iteratively refined to explore developing concepts in subsequent interviews.
Initial coding was carried out by attaching descriptive codes to segments of the text in each transcript. The descriptive codes were then grouped into broad topic‐oriented categories and all text segments belonging to the same category were compared (Corbin and Strauss 2008). Versions of the analysis were reviewed with the research team at regular intervals. We also looked for negative or nonconforming responses, to ensure we considered the range of variations in developing the thematic concepts. Ultimately, the topic‐oriented categories were further refined and formulated into fewer analytic categories through an inductive, iterative process, and triangulated with the field notes from the observation data. The analytic framework was discussed among the research team members (all authors) and we reached consensus on its validity and applicability.
Results
We observed and interviewed 40 EPIC participants (30 patients and 10 family members) for this study. The mean age of patients at the time of observation and interview was 72 years (range 42–95). A slight majority of the patients were male (57 percent) and most lived in an urban environment (70 percent). Most of the patients had a primary diagnosis of diabetes mellitus or chronic obstructive pulmonary disease and some had combinations of multiple chronic conditions The characteristics of patients who participated in the qualitative study are presented in Table 1 and were closely representative of the entire EPIC patient population.
Table 1.
Characteristics of EPIC Patient Study Participants (N = 30)
| Interviewed (n = 30) | |
|---|---|
| Age, mean (range) | 72 (42–95) |
| Male | 17 (57%) |
| Female | 13 (43%) |
| Geographic location (n = 30) | |
| Urban (York region) | 21 (70%) |
| Rural (Grey County) | 9 (30%) |
| Disease category (n = 30) | |
| DM | 15 (50%) |
| DM & COPD | 4 (13%) |
| COPD | 5 (16%) |
| CHF | 2 (1%) |
| DM & CHF; COPD & CHF; DM & COPD & CHF | 4 (13%) |
The study participants had overwhelmingly positive feedback about the EPIC program and about the EPIC community paramedics in particular. However, our findings, more important, center on a core theme of how a program like EPIC addresses patient vulnerability by providing a “safety‐net,” a source of health education and accountability, and the foundational relationship that is built between the community paramedics and the patients.
Patient Vulnerability
The complex chronic disease patients in this study were selected to participate in the EPIC program because of their high risk of hospitalization, and as such are seen by their primary care physicians as intrinsically vulnerable. Many are of advanced age and know that their health issues and supportive care needs are only going to increase. The participants explained to us that their social needs are changing too. They are facing or have already experienced the loss of a spouse, siblings, longtime friends, and other members of their support networks.
Living with a complex chronic disease means that health is experienced as a precarious state of being for many of the patients we spoke to. They shared that disease exacerbations are stressful, frightening, and difficult for them and their family members to deal with. We repeatedly heard stories about delaying seeking treatment for disease exacerbations until things were quite serious because of the hassle, inconvenience, and stress of trying to get help (e.g., get an appointment with their busy family doctors or receive treatment in a timely manner at an Emergency Department). EMS activation (i.e. calling 911) and hospitalization are also very stressful experiences for patients and their family members because they told us they have little control and sometimes very poor understanding about the care that is being provided.
You can call 911, but that's very scary, especially for someone like [my husband], because he doesn't know what's happening. When the [EPIC community paramedics] come in, they take the time to explain to him everything that they're doing, and it makes a big difference. Because as soon as the upset is there, the chest is worse, because it affects all the breathing and everything too …, It's a very scary scenario for him. [GCPT_1]
Many of the interview participants explained that their precarious health status at the time they were enrolled in the EPIC program was not the result of indifference about their health and well‐being. For this reason, many described to us examples of measurable positive health gains since being in the EPIC program and during observation sessions, we repeatedly heard the community paramedics remark about improvements that patients had made in managing their health.
Continuing Health Education and Accountability
A second major theme that emerged from our analysis is that the EPIC community paramedics were seen as a source of continuing health education and accountability for program participants. The patients told us that that they learn new information about health maintenance and chronic disease management from their conversations with the paramedics, information that they had not received elsewhere.
He [the CP] tells me things about diabetes that I had never learned anywhere else, you know. They talk to you about having your blood sugar taken, but nobody has ever told me that your blood reading is going to be the highest two hours after eating … and he personalizes it so it's meaningful to me. You can read a lot of medical stuff and it's just gibberish going over your head. But when he says this causes that and you should do this, it makes it so much better. [Patient 6]
This important relationship that the patients seem to form with the paramedics is a source of inspiration and motivation to the patients to make or keep up with positive lifestyle and behavior changes and be proactive about disease management. The patients shared that they believe the paramedics genuinely care about them and their well‐being, and they perceive the paramedics to be deeply invested in the relationship with them, in addition to being a reliable and resourceful source of knowledge, health coaching, and care. As a result, several participants told us that the paramedics help “keep them in line” with managing their disease. Many interview participants told us that because of the good relationship with the paramedics, they feel accountable to them for their health.
[The EPIC community paramedics] check everything for you and they teach you a whole lot about what you should and should not do. And if you're smart enough, you can incorporate what they tell you into your daily routine …. For me, EPIC is fantastic. And you end up with a fairly close relationship with the paramedics because you tell them about your family, your life and that sort of thing. And they can take that I presume and incorporate it into their working with you so they know what you do, what you want, and use that as a motivator to get you where you want. [EPICQ_P5]
EPIC as a “Safety Net”
Many of the patients in the study described the EPIC model as a “safety net” (their language). They explained that they believe the community paramedics provide them with thorough care when and where they need it and therefore keep them safe from harm. The patients said that they trust the community paramedics implicitly and openly discuss their health issues and lives with them. Furthermore, both the patients and their family members reported feeling well cared for and reassured about their health status because they are in the EPIC program.
I feel safe. I feel that I'm sort of protected, and that I could call any time, because you don't know what more is going to happen. A lot of people, they don't have anybody to turn to, and I feel that I do. Like, not just my family, I've only got a son and his wife — but I just feel like I'm protected, like I'm safe …. But then, you never know what's ahead, you know? [EPICQ_P17]
Patients and family members also told us they feel more secure knowing they can call EPIC paramedics rather than 911 during a disease exacerbation or health emergency.
It's very comforting to me, to know that I have that support, and even if I'm not having to say to the guys, I need you here, I know that if I have a question, I can call one of them. And they're not going to brush me off, or I'm not going to have to wait for an appointment, they're going to get back to me as soon as they can, or they'll pop up just to make sure everything is OK. [GCPT_1]
Patient Bond with Paramedics
Many patients and their family members reported developing a very unique relationship with their EPIC community paramedics; they have come to see the paramedics as important, trusted, essential members of their health care team who have helped and supported them through stressful and scary health crises, that is, at their most vulnerable moments.
My sister was sick, and [EPIC paramedic] just happened to call, and he came over, and I had to rush back from work. He's actually the one who took care of her and took her to the hospital. And that's how dependable these guys are. She was sick, but on the other hand, he was taking care of my father, who was shaken up because my sister was sick. Because of these two, I mean, they have prevented a lot of things happening to us …, I'm so comfortable with them, I can tell them, I can talk to them, I can tell them whatever I feel like …, These guys are like angels. [EPICQ_P10, 11, 12]
Patients also value the strong connection the program has to their primary care physicians and more integrated health care options. They know the community paramedics are in constant contact with their physician through the family health team EMR and appreciate being able to take printouts of blood work and other tests performed by EPIC paramedics to physician and specialist appointments. Participants explained during interviews that they will bring up things to the community paramedic that they do not have the time or remember to communicate with their primary care physician. They also appreciate that the community paramedics will refer them to their physician as necessary, as well as to other community‐based health care resources, and will advocate on their behalf (e.g., calling the primary care physician to schedule an appointment). The primary care physicians were also available by phone to the Community Paramedics during regular office hours and took calls for immediate consultation whenever necessary, for example, if something of concern showed up in the blood work or assessment during the home visit.
Our doctor has a more continuing sense of what's going on with us. There is excellent communication between our family doctor and this program. So, we are definitely much better monitored. [EPICQ_P7]
Several interview participants described situations where the community paramedics greatly exceeded their expectations and went “beyond the call of duty” to take care of them at a time when they were experiencing a disease exacerbation and feeling particularly vulnerable. For example, during one of the observation sessions, a patient shared that on a previous visit, the community paramedic had realized that she was quite ill, needed to go to hospital immediately, and had activated 911 emergency health services. Because the patient lives alone and was unable to prepare for the trip to hospital, the community paramedic agreed to stay behind in her home after the EMS paramedics had transported her to hospital, tidy up the house, pack the patient an overnight bag, and deliver it off at the hospital. It was clear that for the patient, who described herself as accustomed to receiving less personal care from other health care providers, such actions were remarkable and extraordinary. These kinds of experiences garnered a tremendous level of trust and faith in the community paramedics.
Discussion
Community paramedicine programs are predicated on the idea of helping patients get the appropriate care they need in their communities, while reducing unnecessary emergency room visits and hospital admissions. Appropriate care has often been conceptualized in very practical terms—care, that is, efficient, cost‐effective, and achieves desired clinical outcomes (Fuchs 2011). However, our findings illuminate that “appropriate care” and health care needs are much deeper concepts, which include attributes that impact a patient's quality of life—including recognition of their vulnerability, providing a safety net in times of exacerbation, and source of health education and accountability. This tends to be facilitated by the creation of a relationship with a dedicated health care provider that increases the continuity of care. Furthermore, it is about more than convenient, nice‐to‐have care that only aims to reduce the access burden but rather addressing unmet needs within the organization of the primary care system that may leave patients vulnerable.
Based on our findings, participants in a home visit‐based community paramedicine program feel that it provides several components of care that are often overlooked and that a consistent relationship with a health care provider brings a more holistic perspective to their care. From the viewpoint of the patients, the community paramedics are able to incorporate how they experience their disease day to day as part of their care planning by meeting them where they are and taking into account all the things that contribute to their health, including knowledge, home life, and communication with their primary care provider. The lived experience of having a complex chronic disease is a tenuous state of being that involves various interactions with the health care system, changes to home life, and increased vulnerability. Rather than applying a biomedical framework (Annandale 1998) to chronic disease management, the EPIC‐type community program espouses a more bio‐psychosocial approach, which accounts for understanding the patient's subjective experience as an essential contributor to more appropriate and holistic care and ultimately better health outcomes.
Our findings are also not independent concepts but rather the relationship between each of the main themes forms the basis for a theory or framework for home visit‐based community paramedicine from the participant perspective. The impact of EPIC appears to function via the interconnectedness of the concepts of reducing vulnerability, which include safety, accountability, continuing education, and psychosocial awareness, all resting on the foundation of a consistent and trusting patient–paramedic relationship (Figure 1). The patient's ability to feel safe is connected to the knowledge the paramedics provide, their ability to come to the home, and their understanding of each patient and family's unique psychosocial situation. Patients feel they are able to comply with their treatments and necessary lifestyle choices because the paramedics explain things to them, take time with them, and are there at regular intervals to hold them accountable. And all of this is possible because there is a trusting patient–paramedic relationship and a direct relationship between the paramedic, the patient, and the primary care provider. Brydges, Denton, and Agarwal (2016) reported similar concepts in their exploratory, qualitative study of a community paramedicine clinic program held in one high‐risk residential building. We posit that further qualitative research with other home visit‐based community paramedic programs could strengthen our understanding of how this model functions in different scenarios and/or evolves over time.
Figure 1.
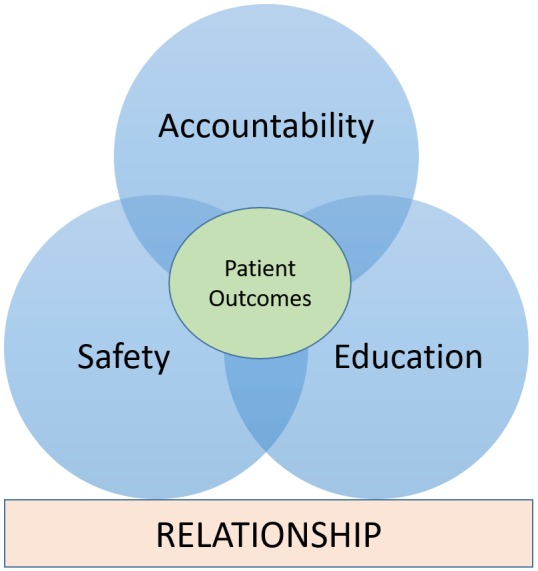
Proposed Framework for Community Paramedicine Programs [Color figure can be viewed at http://wileyonlinelibrary.com]
An increasing number of people around the world are living with advanced chronic diseases or struggle to navigate the health care system appropriately. These individuals have complex medical and social needs, but their care is often fragmented, resulting in adverse health outcomes, avoidable emergency department visits and hospitalizations, and premature admission to long‐term care. Our study provides insight regarding what it takes to provide appropriate and valuable care for these vulnerable patients. Moreover, the study helps us to understand the social and organizational considerations that come with improving the quality of primary patient care.
As with all research, this study is not without limitations. First, the study reported here was specifically designed to understand patient perspectives on the community paramedicine intervention rather than to compare it to other models of care. The specific context of this project may not be generalizable; however, the framework that has been developed from our findings should be conceptually informative to the design of similar care delivery models. Secondly, although the sample is small, it represents several types of patients involved in the program and all of the community paramedics, so we feel it is highly representative, which is the major goal of qualitative sampling. There are other important actors within this delivery model and other sources of data that can be examined with further research.
Health care systems around the world have entered a period of rapid innovation and implementation with a focus on improving quality—including new care practices, care delivery models, and payment methods. We strongly encourage health system decision makers to take heed of the more nuanced patient‐oriented impacts such as those reported here alongside quantitative outcome data to fully appreciate the potential benefits of these kinds of programs for patients and families.
Supporting information
Appendix SA1: Author Matrix.
Appendix SA2: Interview Guide (Patients and Family Members).
Acknowledgments
The authors would like to acknowledge the EPIC patients and their families and the EPIC Paramedics (York Region Paramedic Service and Grey County Paramedic Service) for so willingly participating in this work and sharing their stories with us.
Joint Acknowledgment/Disclosure Statement: The authors state that financial and material support for this project was provided by the Li Ka Shing Knowledge Institute and St. Michael's Hospital as employers of the researcher (KND) and research coordinator (MBS). No grant funding was obtained for this project specifically. We acknowledge the support of this work by the Paramedic Services and Family Health Teams involved in the project and the time given by patients, families, and providers to participate in the interviews.
Disclosures: None.
Disclaimer: None.
Ethics Approval and Consent to Participate: Research ethics approval for this study was obtained from St. Michael's Hospital Research Ethics Board. Verbal consent was obtained from patients and the community paramedics for the observations and recorded in the field notes, and written consent was obtained from patients and family members for the interviews.
Consent to Publish: No individual or personal data are reported in this manuscript.
Availability of Data and Materials: Due to the sensitive and confidential nature of qualitative data, original data will not be made available.
Funding: This research was part of the lead author's overall program of research and did not require separate funding.
Authors' Contributions: KND conceived of and designed the study, conducted the analysis, and drafted the manuscript. She is the guarantor. MBS collected the data, conducted the analysis, and edited the manuscript. ID and LJM reviewed the analysis and edited the manuscript.
References
- Abrashkin, K. A. , Washko J., Zhang J., Poku A., Kim H., and Smith K. L.. 2016. “Providing Acute Care at Home: Community Paramedics Enhance an Advanced Illness Management Program‐Preliminary Data.” Journal of the American Geriatric Society 64 (12): 2572–6. [DOI] [PubMed] [Google Scholar]
- Agarwal, G. , Angeles R., Pirrie M., Marzanek F., McLeod B., Parascandalo J., and Dolovich L.. 2017. Effectiveness of a Community Paramedic‐led Health Assessment and Education Initiative in a Seniors' Residence Building: The Community Health Assessment Program Through Emergency Medical Services (CHAP‐EMS). BMC Emergency Medicine 17 (1): 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annandale, E. 1998. The Sociology of Health and Medicine: A Critical Introduction. Cambridge, UK: Polity Press. [Google Scholar]
- Brydges, M. , Denton M., and Agarwal G.. 2016. “The CHAP‐EMS Health Promotion Program: A Qualitative Study on Participants' Views of the Role of Paramedics.” BMC Health Services Research 16 (1): 435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charmaz, K. 2014. Constructing Grounded Theory. London: Sage. [Google Scholar]
- Corbin, J. , and Strauss A.. 2008. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory, 3rd Edition Thousand Oaks, CA: Sage. [Google Scholar]
- Drennan, I. R. , Dainty K. N., Hoogeveen P., Atzema C. L., Barrette N., Hawker G., Hoch J. S., Isaranuwatchai W., Philpott J., Spearen C., Tavares W., Turner L., Farrell M., Filosa T., Kane J., Kiss A., and Morrison L. J.. 2014. “Expanding Paramedicine in the Community (EPIC): Study Protocol for a Randomized Controlled Trial.” Trials 2 (15): 473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmslie, K. 2012. Against the Growing Burden of Disease. Ottawa, ON: Public Health Agency of Canada; [accessed on June 23, 2017]. Available at http://www.ccgh-csih.ca/assets/Elmslie.pdf. [Google Scholar]
- Francis, J. J. , Johnston M., Robertson C., Glidewell L., Entwistle V., Eccles M. P., and Grimshaw J. M.. 2010. “What Is an Adequate Sample Size? Operationalizing Data Saturation for Theory‐based Interview Studies.” Psychology & Health 25: 1229–45. [DOI] [PubMed] [Google Scholar]
- Fuchs, V. R. 2011. “The Doctor's Dilemma–What Is “Appropriate” Care?”New England Journal of Medicine 365 (7): 585–7. [DOI] [PubMed] [Google Scholar]
- Glaser, B. G. , and Strauss A. L.. 1967. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine. [Google Scholar]
- Government of Canada .(2017) “How Health are Canadians: A Trend Analysis of the Health of Canadians from a Healthy Living and Chronic Disease Perspective” [accessed on May 5, 2017]. Available at https://www.canada.ca/en/publichealth/services/publications/healthy-living/how-healthy-canadians.html?=undefined&wbdisable=true
- Martin, A. , O'Meara P., and Farmer J.. 2016. “Consumer Perspectives of a Community Paramedicine Program in Rural Ontario.” Australian Journal of Rural Health 24 (4): 278–83. [DOI] [PubMed] [Google Scholar]
- Mason, S. , Knowles E., Colwell B., Dixon S., Wardrope J., Gorringe R., Snooks H., Perrin J., and Nicholl J.. 2007. “Effectiveness of Paramedic Practitioners in Attending 999 Calls from Elderly People in the Community: Cluster Randomized Controlled Trial.” British Medical Journal 335 (7626): 919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod, B. , Angeles R., Guenter D., Howard M., Stosic A., and Agarwal G.. 2016. “Why Frequent Users of EMS Services Call 911: A Knowledge‐to‐Action Approach.” Final Research Report Submission to Ontario Association of Paramedic Chiefs/Ontario Paramedic Research Consortium
- Patton, M. 2002. Qualitative Research and Evaluation Methods. Thousand Oaks, CA: Sage. [Google Scholar]
- Webster, F. , Perruccio A. V., Jenkinson R., Jaglal S., Schemitsch E., Waddell J. P., Bremner S., Mobilio M. H., Venkataramanan V., Davis A. M.. 2013. “Where Is the Patient in Models of Patient‐centered Care: A Grounded Theory Study of Total Joint Replacement Patients.” BMC Health Services Research 13: 531. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Interview Guide (Patients and Family Members).


